Content Analysis of Assessment Tools Used in Post-Stroke Rehabilitation: A Scoping Review with Linkage to the International Classification of Functioning
Abstract
1. Introduction
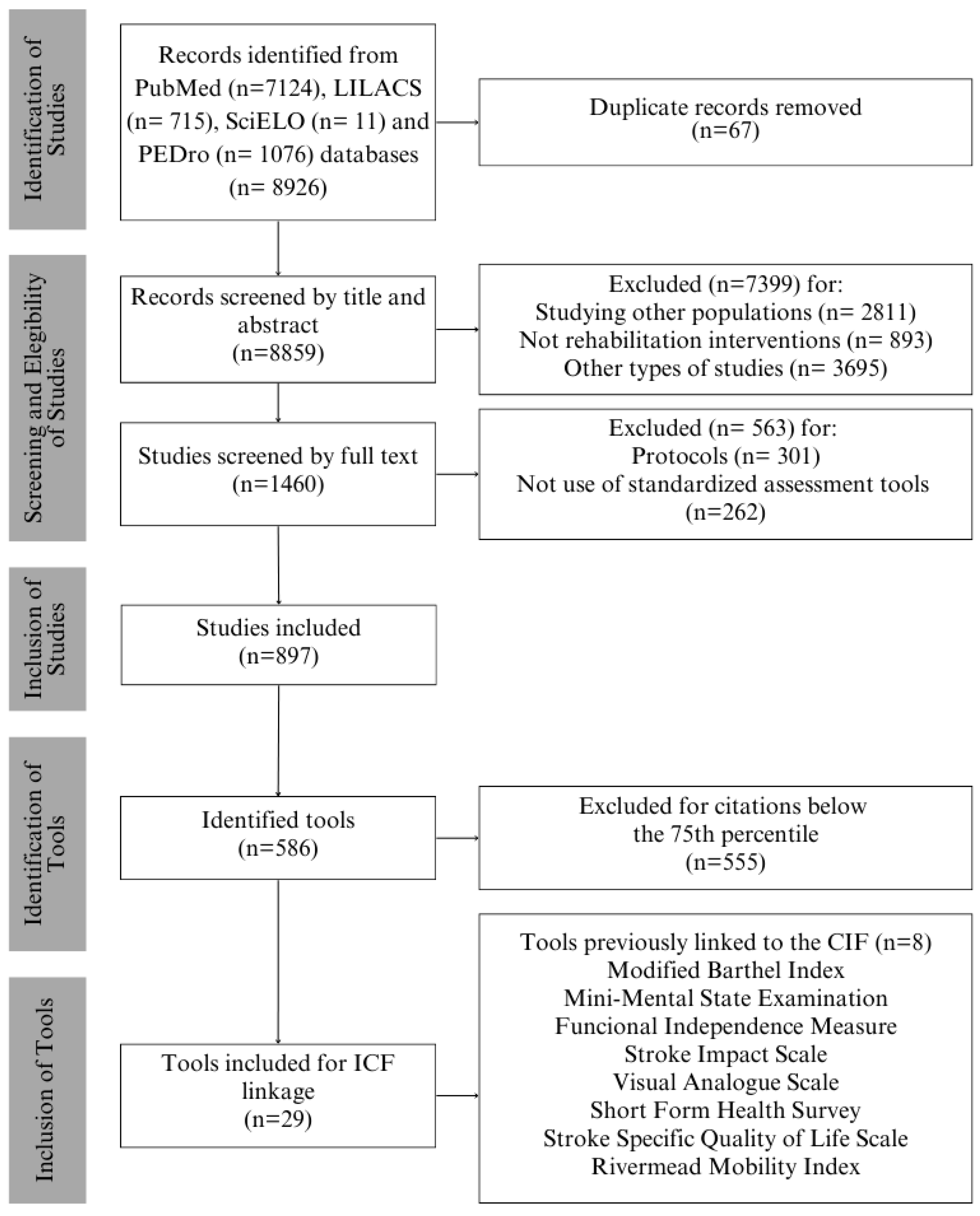
2. Materials and Methods
2.1. Scoping Review
2.2. Linking Process
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Minelli, C.; Bazan, R.; Pedatella, M.T.A.; Neves, L.d.O.; Cacho, R.d.O.; Magalhães, S.C.S.A.; Luvizutto, G.J.; Moro, C.H.C.; Lange, M.C.; Modolo, G.P.; et al. Brazilian Academy of Neurology practice guidelines for stroke rehabilitation: Part I. Arq. Neuro-Psiquiatr. 2022, 80, 634–652. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, P.; Furie, K.L.; Davis, S.M.; Donnan, G.A.; Norrving, B. World stroke organization global stroke services guidelines and action plan. Int. J. Stroke 2014, 9, 4–13. [Google Scholar] [CrossRef]
- Carvalho, M.R.d.S.; Miranda, N.M.S.S.; Lustosa, V.R.; Silva, B.G.S.; Rodrigues, V.E.S.; Oliveira, F.G.L.; Amorim Júnior, J.d.S.; dos Santos, R.S.; de Sousa, J.R. Cuidados de Enfermagem ao Paciente acometido por Acidente Vascular Cerebral: Revisão Integrativa. Rev. Multidiscip. Psicol. 2019, 13, 198–207. [Google Scholar]
- Majersik, J.J.; Woo, D. The enormous financial impact of stroke disability. Neurology 2020, 94, 377–378. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.L.; Boden-Albala, B.; Langa, K.M.; Lisabeth, L.D.; Fair, M.; Smith, M.A.; Sacco, R.L.; Morgenstern, L.B. Projected costs of ischemic stroke in the United States. Neurology 2006, 67, 1390–1395. [Google Scholar] [CrossRef]
- Kumar, A.; Adhikari, D.; Karmarkar, A.; Freburger, J.; Gozalo, P.; Mor, V.; Resnik, L. Variation in hospital-based rehabilitation services among patients with ischemic stroke in the United States. Phys. Ther. 2019, 99, 494–506. [Google Scholar] [CrossRef]
- Minelli, C.; Luvizutto, G.J.; Cacho Rde, O.; Neves Lde, O.; Magalhães, S.C.S.A.; Pedatella, M.T.A.; de Mendonça, L.I.Z. Diretrizes brasileiras para reabilitação no acidente vascular cerebral: Parte II. Arq. Neuropsiquiatr. 2022, 80, 741–758. [Google Scholar]
- dos Santos, H.M.; de Oliveira, L.C.; Bonifácio, S.R.; Brandão, T.C.P.; Silva, W.P.; Pereira, G.S. Use of the International Classification of Functioning, Disability and Health (ICF) to expand and standardize the assessment of quality-of-life following a stroke: Proposal for the use of codes and qualifiers. Disabil. Rehabil. 2022, 44, 7449–7454. [Google Scholar] [CrossRef]
- Heiss, W.D.; Brainin, M.; Bornstein, N.M.; Tuomilehto, J.; Hong, Z. Cerebrolysin in patients with acute ischemic stroke in Asia: Results of a double-blind, placebo-controlled randomized trial. Stroke 2012, 43, 630–636. [Google Scholar] [CrossRef]
- Giardini, A.; Vitacca, M.; Pedretti, R.; Nardone, A.; Chiovato, L.; Spanevello, A. Misure di valutazione e abbinamento dei codici ICF in medicina riabilitativa: La sfida del passaggio dalla teoria alla pratica. G. Ital. Med. Lav. Erg. 2019, 2, 78–104. [Google Scholar]
- Leonardi, M.; Lee, H.; Kostanjsek, N.; Fornari, A.; Raggi, A.; Martinuzzi, A.; Yáñez, M.; Almborg, A.-H.; Fresk, M.; Besstrashnova, Y.; et al. 20 Years of ICF—International Classification of Functioning, Disability and Health: Uses and Applications around the World. Int. J. Environ. Res. Public Health 2022, 19, 11321. [Google Scholar] [CrossRef]
- Cerniauskaite, M.; Quintas, R.; Boldt, C.; Raggi, A.; Cieza, A.; Bickenbach, J.E.; Leonardi, M. Systematic literature review on ICF from 2001 to 2009: Its use, implementation and operationalisation. Disabil. Rehabil. 2011, 33, 281–309. [Google Scholar] [CrossRef] [PubMed]
- Geyh, S.; Cieza, A.; Schouten, J.; Dickson, H.; Frommelt, P.; Omar, Z.; Kostanjsek, N.; Ring, H.; Stucki, G. ICF Core Sets for stroke. J. Rehabil. Med. Suppl. 2004, 36, 135–141. [Google Scholar] [CrossRef]
- Viktorisson, A.; Reinholdsson, M.; Danielsson, A.; Palstam, A.; Sunnerhagen, K.S. Pre-Stroke Physical Activity In Relation To Post-Stroke Outcomes Linked To The International Classification Of Functioning, Disability And Health: A Scoping Review. J. Rehabil. Med. Med. J. Swed. AB 2022, 54, jrm00251. [Google Scholar] [CrossRef] [PubMed]
- Castaneda, L.; Bergmann, A.; Bahia, L. A Classificação Internacional de Funcionalidade, Incapacidade e Saúde: Uma revisão sistemática de estudos observacionais. Rev. Bras. Epidemiol. 2014, 17, 437–451. [Google Scholar] [CrossRef]
- Alt Murphy, M.; Rafsten, L.; Lin, F.; Feng, C.; Jiang, Z.-L.; Sun, M.-X. Simplified Post-stroke Functioning Assessment Based on ICF via Dichotomous Mokken Scale Analysis and Rasch Modeling. Front. Neurol. 2022, 1, 827247. [Google Scholar]
- Biz, M.C.P.; Chun, R.Y.S. Operationalization of the international classification of functioning, disability and health, ICF, in a specialized rehabilitation center. CODAS 2020, 32, e20190046. [Google Scholar] [CrossRef]
- de Paula, M.L.; Jorge, M.S.B.; de Morais, J.B. The health research process and obstacles to the use of research findings by health professionals. Interface Commun Health Educ. 2019, 23, 1–15. [Google Scholar]
- Rajala, C.; Waterhouse, C.; Evans, E.; Erler, K.S.; Bergin, M.J.; Bannon, S.M.; Slavin, M.D.; Kazis, L.E. Conceptualization of Participation: A Qualitative Synthesis of Brain Injury Stakeholder Perspectives. Front. Rehabil. Sci. 2022, 3, 908615. [Google Scholar] [CrossRef]
- Cieza, A.; Fayed, N.; Bickenbach, J.; Prodinger, B. Refinements of the ICF Linking Rules to strengthen their potential for establishing comparability of health information. Disabil. Rehabil. 2016, 41, 574–583. [Google Scholar] [CrossRef]
- Grou, T.C.; Castro SSde Leite, C.F.; Carvalho, M.T.; Patrizzi, L.J. Validação da versão brasileira do World Health Organization Disability Assessment Schedule 2.0 em idosos institucionalizados. Fisioter E Pesqui. 2021, 28, 77–87. [Google Scholar] [CrossRef]
- de Wind, A.; Donker-Cools, B.H.P.M.; Jansen, L.; Luymes, C.H.; van der Burg-Vermeulen, S.J.; Oomens, S.; Anema, J.R.; Schaafsma, F.G. Development of the core of an ICF-based instrument for the assessment of work capacity and guidance in return to work of employees on sick leave: A multidisciplinary modified Delphi study. BMC Public Health 2022, 22, 2449. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, E.; Gustafsson, J. Validation of the International Classification of Functioning, Disability and Health (ICF) core sets from 2001 to 2019—A scoping review. Disabil. Rehabil. 2022, 44, 3736–3748. [Google Scholar] [CrossRef]
- Algurén, B.; Lundgren-Nilsson, Å.; Sunnerhagen, K.S. Functioning of stroke survivors—A validation of the ICF core set for stroke in Sweden. Disabil. Rehabil. 2010, 32, 551–559. [Google Scholar] [CrossRef]
- Prodinger, B.; O’Connor, R.; Stucki, G.; Tennant, A. Establishing score equivalence of the functional independence measure motor scale and the barthel index, utilising the international classification of functioning, disability and health and rasch measurement theory. J. Rehabil. Med. 2017, 49, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Perin, C.; Bolis, M.; Limonta, M.; Meroni, R.; Ostasiewicz, K.; Cornaggia, C.M.; Alouche, S.R.; Matuti, G.d.S.; Cerri, C.G.; Piscitelli, D. Differences in Rehabilitation Needs after Stroke: A Similarity Analysis on the ICF Core Set for Stroke. Int. J. Environ. Res. Public Health 2020, 17, 4291. [Google Scholar] [CrossRef]
- Moriello, C.; Byrne, K.; Cieza, A.; Nash, C.; Stolee, P.; Mayo, N. Mapping the Stroke Impact Scale (SIS-16) to the International Classification of Functioning, Disability and Health. J. Rehabil. Med. 2008, 40, 102–106. [Google Scholar] [CrossRef]
- Kohler, F.; Connolly, C.; Sakaria, A.; Stendara, K.; Buhagiar, M.; Mojaddidi, M. Can the ICF be used as a rehabilitation outcome measure? A study looking at the inter- and intra-rater reliability of ICF categories derived from an ADL assessment tool. J. Rehabil. Med. 2013, 45, 881–887. [Google Scholar] [CrossRef] [PubMed]
- Bernardelli, R.S.; Santos, B.C.; Scharan, K.O.; Corrêa, K.P.; Silveira, M.I.B.; Moser, A.D.d.L. Application of the refinements of ICF linking rules to the Visual Analogue Scale, Roland Morris questionnaire and SF-36. Cienc E Saude Coletiva. 2021, 26, 1137–1152. [Google Scholar] [CrossRef]
- Silva, S.M.; Brandão, T.C.P.; Da Silva, F.P.; Buchalla, C.M. Identification of categories of the International Classification of Functioning, Disability and Health in functional assessment measures for stroke survivors: A systematic review. Disabil. Rehabil. 2020, 42, 156–162. [Google Scholar] [CrossRef]
- Han, K.Y.; Kim, H.J.; Bang, H.J. Feasibility of Applying the Extended ICF Core Set for Stroke to Clinical Settings in Rehabilitation: A Preliminary Study. Ann. Rehabil. Med. 2015, 39, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Tarvonen-Schröder, S.; Hurme, S.; Laimi, K. The world health organization disability assessment schedule (WHODAS 2.0) and the WHO minimal generic set of domains of functioning and health versus conventional instruments in subacute stroke. J. Rehabil. Med. 2019, 51, 675–682. [Google Scholar] [CrossRef]
- Kossi, O.; Amanzonwe, E.R.; Thonnard, J.-L.; Batcho, C.S. Applicability of International Classification of Functioning, Disability and Health-based participation measures in stroke survivors in Africa: A systematic review. Int. J. Rehabil. Res. 2020, 43, 3–11. [Google Scholar] [CrossRef]
- Cramer, S.C.; Richards, L.G.; Bernhardt, J.; Duncan, P. Cognitive Deficits After Stroke. Stroke 2023, 54, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Schwade, M.; Smith, Y.; Wood, R.; Young, L. Exercise-based interventions for post-stroke social participation: A systematic review and network meta-analysis. Int. J. Nurs. Stud. 2020, 111, 103738. [Google Scholar] [CrossRef]
- Zhou, X.; Du, M.; Dai, X.; Zhu, S.; Zhou, L.; Li, X. Intervention patterns and preliminary effectiveness on Social Participation following stroke: A scoping review. BMC Neurol. 2023, 23, 275. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.; Khalil, H. Chapter 11: Scoping reviews. In JBI Manual for Evidence Synthesis; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2019; pp. 407–452. [Google Scholar]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Aromataris, E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Database Syst. Rev. Implement Rep. 2019, 18, 2127–2133. [Google Scholar] [CrossRef]
- Aromataris, E.; Lokwood, C.; Porritt, K.; Pilla, B.; Jordan, Z. JBI Manual for Evidence Synthesis; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2024. [Google Scholar]
- Cieza, A.; Brockow, T.; Ewert, T.; Amman, E.; Kollerits, B.; Chatterji, S.; Üstün, T.B.; Stucki, G. Linking health-status measurements to the International Classification of Functioning, Disability and Health. J. Rehabil. Med. 2002, 34, 205–210. [Google Scholar] [CrossRef]
- Fayed, N.; Cieza, A.; Bickenbach, J.E. Linking health and health-related information to the ICF: A systematic review of the literature from 2001 to 2008. Disabil. Rehabil. 2011, 33, 1941–1951. [Google Scholar] [CrossRef]
- Cieza, A.; Geyh, S.; Chatterji, S.; Kostanjsek, N.; Üstün, B.; Stucki, G. ICF linking rules: An update based on lessons learned. J. Rehabil. Med. 2005, 37, 212–218. [Google Scholar] [CrossRef]
- Berzina, G.; Sveen, U.; Paanalahti, M.; Sunnerhagen, K.S. Analyzing the modified rankin scale using concepts of the international classification of functioning, disability and health. Eur. J. Phys. Rehabil. Med. 2016, 52, 203–213. [Google Scholar] [PubMed]
- De Vriendt, P.; Gorus, E.; Bautmans, I.; Mets, T. Conversion of the mini-mental state examination to the international classification of functioning, disability and health terminology and scoring system. Gerontology 2012, 58, 112–119. [Google Scholar] [CrossRef]
- Teixeira-Salmela, L.F.; Neto, M.G.; Magalhães, L.C.; Lima, R.C.; Faria, C.D.C.M. Content comparisons of stroke-specific quality of life based upon the international classification of functioning, disability, and health. Qual. Life Res. 2009, 18, 765–773. [Google Scholar] [CrossRef]
- Amatya, B.D.; Mukaino, M.; Stucki, G.; Selb, M.M.; Khan, F.A. Content comparison of multidimensional functional outcome measures in rehabilitation and the ICF clinical functioning information tool: A scoping literature review. J. Int. Soc. Phys. Rehabil. Med. 2024, 7, 144–159. [Google Scholar] [CrossRef]
- Wong, M.N.-K.; Cheung, M.K.-T.; Ng, Y.-M.; Yuan, H.-L.; Lam, B.Y.-H.; Fu, S.N.; Chan, C.C.H. International Classification of Functioning, Disability, and Health-based rehabilitation program promotes activity and participation of post-stroke patients. Front. Neurol. 2023, 14, 1235500. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Blázquez, C.; Damián, J.; Andrés-Prado, M.J.; Almazán-Isla, J.; Alcalde-Cabero, E.; Forjaz, M.J.; Castellote, J.M.; González-Enríquez, J.; Martínez-Martín, P.; Comín, M.; et al. Associations between chronic conditions, body functions, activity limitations and participation restrictions: A cross-sectional approach in Spanish non-clinical populations. BMJ Open 2016, 6, e010446. [Google Scholar] [CrossRef] [PubMed]
- Irrgang, S.; Himmelhaus, S.; Allek, K.; Debecker, I.; Gemperli, A.; Kynast, K.; von Reumont, A.; Scheel-Sailer, A. Assessments and interventions on body functions, structures and activity to prepare adults with acute spinal cord injury or disease for participation: A scoping review. Front. Rehabil. Sci. 2024, 5, 1272682. [Google Scholar] [CrossRef]
- Foley, E.L.; Nicholas, M.L.; Baum, C.M.; Connor, L.T. Influence of environmental factors on social participation post-stroke. Behav. Neurol. 2019, 2019, 2606039. [Google Scholar] [CrossRef]
- Darzins, S.; Imms, C.; Di Stefano, M.; Taylor, N.F.; Pallant, J.F. Evaluation of the internal construct validity of the Personal Care Participation Assessment and Resource Tool (PC-PART) using Rasch analysis. BMC Health Serv. Res. 2014, 14, 543. [Google Scholar] [CrossRef]
- Daneski, K.; Coshall, C.; Tillingand, K.; Wolfe, C.D.A. Reliability and validity of a postal version of the Reintegration to Normal Living Index, modified for use with stroke patients. Clin. Rehabil. 2003, 17, 835–839. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, M.; Maso, I.; Sasaki, A.C.; Neto, N.B.; Filho, J.O.; Pinto, E.B. Validation of the Frenchay activity index on stroke victims. Arq. de Neuro-Psiquiatr. 2017, 75, 167–171. [Google Scholar] [CrossRef]
- Post, M.W.M.; van der Zee, C.H.; Hennink, J.; Schafrat, C.G.; Visser-Meily, J.M.; van Berlekom, S.B. Validity of the utrecht scale for evaluation of rehabilitation-participation. Disabil. Rehabil. 2012, 34, 478–485. [Google Scholar] [CrossRef]
- Wilkie, R.; Peat, G.; Thomas, E.; Croft, P.; Wilkie, R.; Peat, G. Factors Associated with Participation Restriction in Community-Dwelling Adults Aged 50 Years and Over. Qual. Life Res. 2016, 16, 1147–1156. [Google Scholar] [CrossRef]
- Liu, H.; Chen, L.; Zhang, G.; Jiang, Y.; Qu, S.; Liu, S.; Huang, Y.; Chen, J. Scalp Acupuncture Enhances the Functional Connectivity of Visual and Cognitive-Motor Function Network of Patients with Acute Ischemic Stroke. Evid. Based Complement Altern. Med. 2020, 2020, 8836794. [Google Scholar] [CrossRef] [PubMed]
- Eyssen, I.C.; Steultjens, M.P.; Dekker, J.; Terwee, C.B. A systematic review of instruments assessing participation: Challenges in defining participation. Arch. Phys. Med. Rehabil. 2011, 92, 983–997. [Google Scholar] [CrossRef] [PubMed]
- Dadson, D.; Ball, K.; Veal, B.; Meng, H.; Andel, R. Predictors Of Everyday Functioning, Adls/Iadls Among Older Adults Using The Active Study. Innov. Aging 2023, 7, 969. [Google Scholar] [CrossRef]
- Elf, M.; Rasoal, D.; Zingmark, M.; Kylén, M. The importance of context—A qualitative study exploring healthcare practitioners’ experiences of working with patients at home after a stroke. BMC Health Serv. Res. 2023, 23, 733. [Google Scholar] [CrossRef]
- de Rooij, I.J.M.; van de Port, I.G.L.; van der Heijden, L.L.M.; Meijer, J.W.G.; Visser-Meily, J.M.A. Perceived barriers and facilitators for gait-related participation in people after stroke: From a patients’ perspective. Physiother. Theory Pract. 2021, 37, 1337–1345. [Google Scholar] [CrossRef]
- Caro, C.C.; Costa, J.D.; Da Cruz, D.M.C. Burden and Quality of Life of Family Caregivers of Stroke Patients. Occup. Ther. Health Care 2018, 32, 154–171. [Google Scholar] [CrossRef]
- Stucki, G.; Cieza, A. The International Classification of Functioning, Disability and Health (ICF) Core Sets for rheumatoid arthritis: A way to specify functioning. Ann. Rheum. Dis. 2004, 63, ii40–ii45. [Google Scholar] [CrossRef] [PubMed]
- Pathak, A.; Abbott, H.J.; Sharma, S.; Ribeiro, D.C.; Heinemann, A.W. Content validity of the Brief and Comprehensive ICF Core Sets for common disabling conditions in a developing country. Int. J. Rehabil. Res. 2021, 44, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Farias, N.; Buchalla, C.M. A classificação internacional de funcionalidade, incapacidade e saúde da organização mundial da saúde: Conceitos, usos e perspectivas. Rev. Bras. Epidemiol. 2005, 8, 187–193. [Google Scholar] [CrossRef]
- Zhang, T.; Liu, L.; Xie, R.; Peng, Y.; Wang, H.; Chen, Z.; Li, B. Value of using the international classification of functioning, disability, and health for stroke rehabilitation assessment: A multicenter clinical study. Medicine 2018, 97, e12802. [Google Scholar] [CrossRef]
| Tools | Number of Citations |
|---|---|
| Fugl Meyer Assessment (FMA) * | 375 |
| Modified Barthel Index (MBI) [25] | 209 |
| Modified Ashworth scale (MAS) | 206 |
| Mini-Mental State Examination (MMSE) [45] | 158 |
| National Institute of Health Stroke Scale (NHISS) | 128 |
| Berg Balance Scale (BBS) | 120 |
| Timed Up and Go (TUG) | 93 |
| 10-Meter Walk Test (10 MWT) | 89 |
| Modified Rankin Scale (mRS) | 86 |
| Action Research Arm Test (ARAT) | 79 |
| Montreal Cognitive Assessment (MoCA) | 78 |
| Wolf Motor Function Test (WMFT) | 74 |
| 6-Minute Walk Test (6 MWT) | 71 |
| Functional Ambulation Categories (FAC) | 61 |
| Stroke Impact Scale (SIS) [27] | 61 |
| Functional Independence Measure (FIM) [28] | 60 |
| Box and Block (BBT) | 58 |
| Motor Activity Log (MAL) | 45 |
| Visual Analogue Scale (VAS) [29] | 40 |
| Brunnstrom Recovery Stage (BRS) | 38 |
| Medical Research Council (MRC) | 30 |
| Motricity Index (MI) | 30 |
| Short Form-36 Health Survey (SF-36) | 28 |
| Hospital Anxiety and Depression Scale (HADS) | 28 |
| European Quality of Life 5-Dimension (EQ-5D) | 27 |
| Stroke Specific Quality of Life Scale (SSQoL) [46] | 25 |
| Trunk Impairment Scale (TIS) | 23 |
| Borg Rating of Perceived Exertion (RPE) | 22 |
| Rivermead Mobility Index (RMI) [30] | 21 |
| Tool | Body Functions | % | Activities and Participation | % | Environmental Factors | % | Others |
|---|---|---|---|---|---|---|---|
| 10-Meter Walk Test (10 WMT) | 0% | d4500; d465 | 100% | 0% | |||
| Action Research Arm Test (ARAT) | 0% | d4300; d4301; d4400; d4401; d4402; d4453; d4458 | 100% | 0% | |||
| Box and Block Test (BBT) | 0% | d4301; d4400; d4403 | 100% | 0% | |||
| Berg Balance BERG (BERG) | 0% | d4103; d4104; d4105; d4106; d4153; d4154; d4200; d429; d4400 | 100% | 0% | |||
| EuroQol (EQ-5D) | b280 | 11% | d450, d510; d540; d859; d839; d640; d760; d920 | 34% 55% | 0% | nd-gh; nc-hc; pf | |
| Functional Ambulation Categories (FAC) | 0% | d4500; d4502; d4551; d465 | 100% | 0% | |||
| Fugl Meyer Assessment (FMA) | b28016; b260; b265; b7100; b7300; b7500; b7600; b7602; b7651 | 64% | d4106; d4153; d4154; d4400; d4401 | 36% | 0% | ||
| Motor Activity Log (MAL) | b7600 | 5% | d170; d2100; d2101; d4104; d4300; d4301; d4402; d4450; d4451; d4453; d5100; d5102; d5200; d5201; d5202; d5402; d5403; d550; d6402 | 90% 5% | 0% | ||
| Motricity Index (MI) | b7300 | 50% | d4400 | 50% | 0% | ||
| Modified Ashworth Scale (MAS) | b735 | 100% | 0% | 0% | |||
| Montreal Cognitive Assessment (MoCA) | b1400; b1440; b1441; b1442; b1560; b1561; b1565; b164; b1640; b167; b16700; b16710; b1720 | 100% | 0% | 0% | |||
| Medical Research Council (MRC) * | b1670; b7300; b7600 | 75% | d210 | 25% | 0% | ||
| National Institutes of Health Stroke Scale (NIHSS) | b1100; b1140; b11420; b156; b167; b1670; b2101; b2703; b320; b3300; b7300; b7301; b7401; b7600; b7602 | 88% | d210 | 6% | 0% | ||
| 6-Minute Walk Test (6 MWT) | b4202; b455 | 67% | d4500 | 33% | 0% | ||
| Time Up and Go (TUG) | 0% | d4103; d4104; d4108; d4500 | 100% | 0% | |||
| Wolf Motor Function Test (WFMT) | b7301; b7600; b7602 | 75% | d4300; d4301; d4400; d4401; d4402; d4450; d4451; d4452; d4453 | 25% | 0% | ||
| Functional Independence Measure (FIM) | b144; b525; b620 | 18% | d175; d310; d330; d410; d4500; d4551; d465; d510; d520; d530; d540; d550; d560; d710 | 76% 6% | 0% | ||
| Mini-Mental State Examination (MMSE) | 83% | d210 | 17% | 0% | |||
| Modified Barthel Index (MBI) | 0% | d410; d420; d450; d455; d5; d510; d530; d540; d550; d560 | 100% | 0% | |||
| Modified Rankin Scale (mRS) | b210; b270; b3300; b5105; b75; b755; b760 | 14% | d140; d170; d450; d465; d475; d489; d4608; d5100; d5108; d520; d5201; d5202; d530; d5400; d5401; d550; d599; d640; d6401; d6409; d6060; d860; d6300; d839; d8450; d870; d85; d859; d9; d920; d9200; d9201; d9202; d9203; d9204; d9205; d930; d7500; d760 | 35% 45% | e310, e320; e399 | 6% | nd; nc |
| Short Form-36 Health Survey (SF-36) | b1300; b1263; b1265; b152; b280 | 20% | d230; d4; d4101; d4102; d4105; d430; d4300; d4500; d4501; d4551; d4552; d5; d510; d540; d6402; d6403; d750; d850; d9201; d9205 | 56% 24% | 0% | nd-gh; nd-ph; nd-mh; nc-hc | |
| Stroke Impact Scale (SIS) | b525; b620 | 11% | d410; d4153; d4154; d420; d430; d450; d4508; d4550; d4551; d5101; d530; d5300; d5301; d5400; d6200; d640 | 78% 11% | 0% | ||
| Visual Analogue Scale (VAS) | b280 | 100% | 0% | 0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, M.H.A.; Dantas, T.H.d.M.; Araújo, A.C.d.M.; Dantas, D.d.S.; Dantas, M.I.d.A.; de Lucena, B.C.M.; Moura, I.C.R.R.; Fernandes, A.B.G.S. Content Analysis of Assessment Tools Used in Post-Stroke Rehabilitation: A Scoping Review with Linkage to the International Classification of Functioning. Int. J. Environ. Res. Public Health 2025, 22, 1277. https://doi.org/10.3390/ijerph22081277
Silva MHA, Dantas THdM, Araújo ACdM, Dantas DdS, Dantas MIdA, de Lucena BCM, Moura ICRR, Fernandes ABGS. Content Analysis of Assessment Tools Used in Post-Stroke Rehabilitation: A Scoping Review with Linkage to the International Classification of Functioning. International Journal of Environmental Research and Public Health. 2025; 22(8):1277. https://doi.org/10.3390/ijerph22081277
Chicago/Turabian StyleSilva, Maria Heloiza Araujo, Thaissa Hamana de Macedo Dantas, Ana Cecília de Medeiros Araújo, Diego de Sousa Dantas, Maria Isabelle de Araújo Dantas, Beatriz Cristina Medeiros de Lucena, Isabelly Cristina Rodrigues Regalado Moura, and Aline Braga Galvão Silveira Fernandes. 2025. "Content Analysis of Assessment Tools Used in Post-Stroke Rehabilitation: A Scoping Review with Linkage to the International Classification of Functioning" International Journal of Environmental Research and Public Health 22, no. 8: 1277. https://doi.org/10.3390/ijerph22081277
APA StyleSilva, M. H. A., Dantas, T. H. d. M., Araújo, A. C. d. M., Dantas, D. d. S., Dantas, M. I. d. A., de Lucena, B. C. M., Moura, I. C. R. R., & Fernandes, A. B. G. S. (2025). Content Analysis of Assessment Tools Used in Post-Stroke Rehabilitation: A Scoping Review with Linkage to the International Classification of Functioning. International Journal of Environmental Research and Public Health, 22(8), 1277. https://doi.org/10.3390/ijerph22081277







