A Quasi-Experimental Pre-Post Assessment of Hand Hygiene Practices and Hand Dirtiness Following a School-Based Educational Campaign
Abstract
1. Introduction
2. Materials and Methods
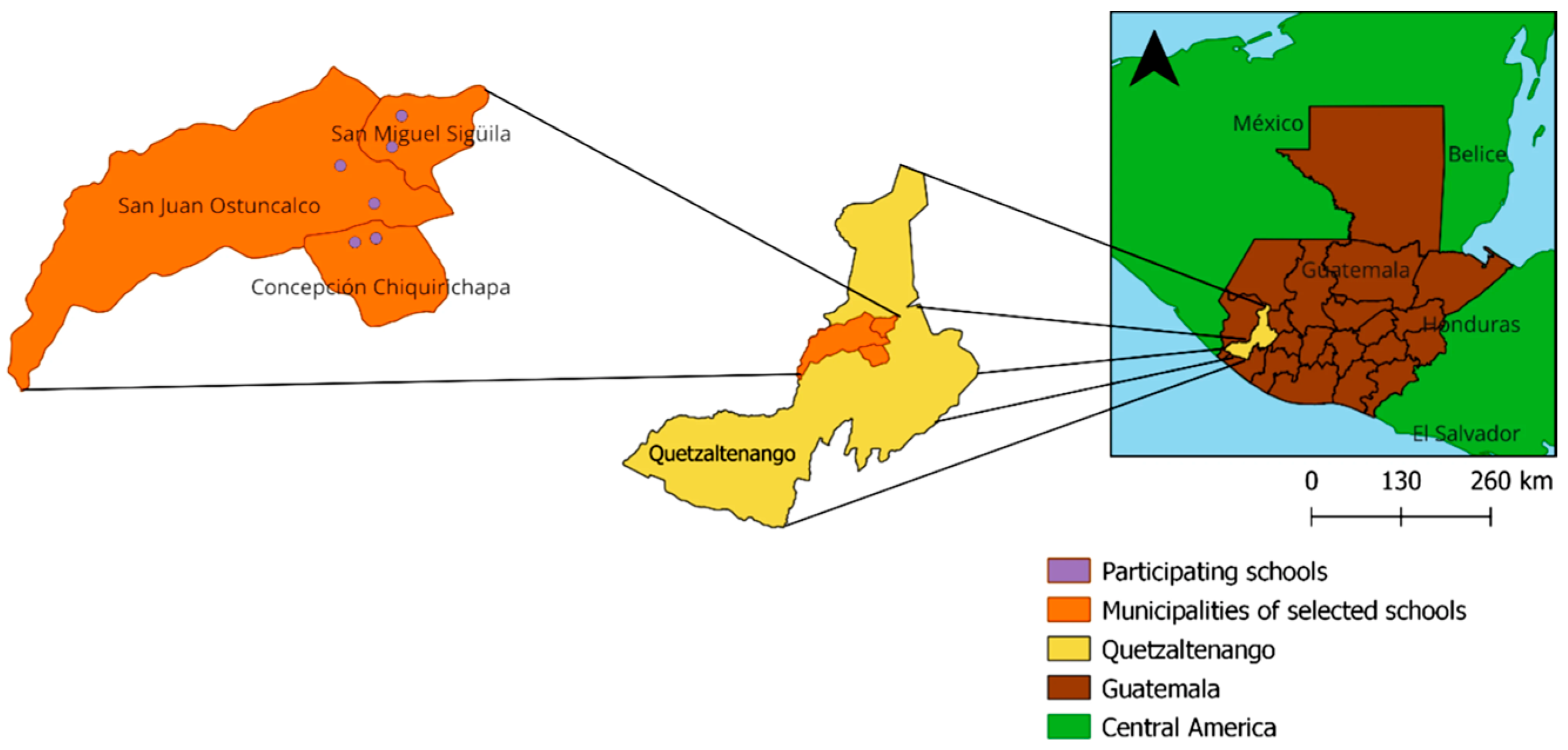
2.1. Study Setting
2.2. Intervention
2.3. Procedures
2.3.1. Hand Hygiene Observations Methods
2.3.2. Hand Dirtiness Evaluation Methods
2.4. Data Analysis
2.5. Ethics Statement
3. Results
3.1. Hand Hygiene Observations
3.2. Hand Dirtiness Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ABHR | Alcohol based hand rub |
| HH | Hand hygiene |
| WHO | World Health Organization |
| WASH | Water, sanitation and hygiene |
| UVG | Universidad del Valle de Guatemala |
| qPHAT | Quantitative Personal Hygiene Assessment Tool |
| CDC | US Centers for Disease Control and Prevention |
References
- Mbakaya, B.C.; Lee, P.H.; Lee, R.L.T. Hand Hygiene Intervention Strategies to Reduce Diarrhoea and Respiratory Infections among Schoolchildren in Developing Countries: A Systematic Review. Int. J. Environ. Res. Public Health 2017, 14, 371. [Google Scholar] [CrossRef] [PubMed]
- Effectiveness of Hand Hygiene Interventions in Reducing Illness Absence Among Children in Educational Settings: A Systematic Review and Meta-Analysis|Archives of Disease in Childhood. Available online: https://adc.bmj.com/content/101/1/42 (accessed on 9 April 2024).
- State of the World’s Hand Hygiene. Pdf. Available online: https://www.unicef.org/media/108356/file/State%20of%20the%20World%E2%80%99s%20Hand%20Hygiene.pdf (accessed on 19 September 2023).
- Chittleborough, C.R.; Nicholson, A.L.; Young, E.; Bell, S.; Campbell, R. Implementation of an educational intervention to improve hand washing in primary schools: Process evaluation within a randomised controlled trial. BMC Public Health 2013, 13, 757. [Google Scholar] [CrossRef] [PubMed]
- WHO. Promoting Health Through Schools: Report of a WHO Expert Committee on Comprehensive School Health Education and Promotion; i–vi; World Health Organization: Geneva, Switzerland, 1997; Volume 870, pp. 1–93. [Google Scholar]
- Younie, S.; Mitchell, C.; Bisson, M.-J.; Crosby, S.; Kukona, A.; Laird, K. Improving young children’s handwashing behaviour and understanding of germs: The impact of A Germ’s Journey educational resources in schools and public spaces. PLoS ONE 2020, 15, e0242134. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.K.; Harris, J.R.; Juliao, P.; Nygren, B.; Were, V.; Kola, S.; Sadumah, I.; Faith, S.H.; Otieno, R.; Obure, A.; et al. Impact of a Hygiene Curriculum and the Installation of Simple Handwashing and Drinking Water Stations in Rural Kenyan Primary Schools on Student Health and Hygiene Practices. Am. J. Trop. Med. Hyg. 2012, 87, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Mosa, A.J.; Hayward, A.S.; Matthews, S.A. Promoting clean hands among children in Uganda: A school-based intervention using ‘tippy-taps’. Public Health 2013, 127, 586–589. [Google Scholar] [CrossRef] [PubMed]
- Arora, A. Progress on Drinking Water, Sanitation and Hygiene in Schools 2015–2023: Special Focus on Menstrual Health. Available online: https://data.unicef.org/resources/jmp-wash-in-schools-2024/ (accessed on 11 November 2024).
- Pieters, M.M.; Fahsen, N.; Quezada, R.; Pratt, C.; Craig, C.; McDavid, K.; Vega Ocasio, D.; Hug, C.; Cordón-Rosales, C.; Lozier, M.J. Assessing hand hygiene knowledge, attitudes, and behaviors among Guatemalan primary school students in the context of the COVID-19 pandemic. BMC Public Health 2023, 23, 2252. [Google Scholar] [CrossRef] [PubMed]
- Arvelo, W.; Hall, A.J.; Henao, O.; Lopez, B.; Bernart, C.; Moir, J.C.; Reyes, L.; Montgomery, S.P.; Morgan, O.; Estevez, A.; et al. Incidence and etiology of infectious diarrhea from a facility-based surveillance system in Guatemala, 2008–2012. BMC Public Health 2019, 19, 1340. [Google Scholar] [CrossRef] [PubMed]
- Pieters, M.M.; Fahsen, N.; Craig, C.; Quezada, R.; Pratt, C.Q.; Gomez, A.; Brown, T.W.; Kossik, A.; McDavid, K.; Vega Ocasio, D.; et al. Assessment of Water, Sanitation, and Hygiene Conditions in Public Elementary Schools in Quetzaltenango, Guatemala, in the Context of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 6914. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Delea, M.G.; Snyder, J.S.; Woreta, M.; Zewudie, K.; Solomon, A.W.; Freeman, M.C. Development and reliability of a quantitative personal hygiene assessment tool. Int. J. Hyg. Environ. Health 2020, 227, 113521. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, W.-P.; Wloch, C.; Biran, A.; Curtis, V. Punam Mangtani Formative Research on the Feasibility of Hygiene Interventions for Influenza Control in UK Primary Schools|BMC Public Health|Full Text. Available online: https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-9-390 (accessed on 29 August 2022).
- Maddux, J.E.; Rogers, R.W. Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. J. Exp. Soc. Psychol. 1983, 19, 469–479. [Google Scholar] [CrossRef]
- A Meta-Analysis of Fear Appeals: Implications for Effective Public Health Campaigns—Kim Witte, Mike Allen. 2000. Available online: https://journals.sagepub.com/doi/abs/10.1177/109019810002700506 (accessed on 27 September 2023).
- Becker: The Health Belief Model and Sick Role Behavior—Google Académico. Available online: https://scholar.google.com/scholar_lookup?title=The+health+belief+model+and+sick+role+behavior&author=M.+H.+Becker&publication_year=1974&pages=409-419&doi=10.1177%2F109019817400200407 (accessed on 27 September 2023).
- WHO Chief Declares End to COVID-19 as a Global Health Emergency|UN News. Available online: https://news.un.org/en/story/2023/05/1136367 (accessed on 27 September 2023).
- Coronavirus en Guatemala|Soy502. Available online: https://www.soy502.com/covid19 (accessed on 29 October 2024).
- Gobierno de Guatemala. CUERDO GUBERNATIVO 19-2023. Available online: https://leyes.infile.com/index.php?id=182&id_publicacion=86475 (accessed on 28 September 2023).
- Arlinghaus, K.R.; Johnston, C.A. Advocating for Behavior Change with Education. Am. J. Lifestyle Med. 2018, 12, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.P.; Barker, M. Why is changing health-related behaviour so difficult? Public Health 2016, 136, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Biran, A.; Schmidt, W.P.; Varadharajan, K.S.; Rajaraman, D.; Kumar, R.; Greenland, K.; Gopalan, B.; Aunger, R.; Curtis, V. Effect of a behaviour-change intervention on handwashing with soap in India (SuperAmma): A cluster-randomised trial. Lancet Glob. Health 2014, 2, e145–e154. [Google Scholar] [CrossRef] [PubMed]
- Curtis, V.A.; Danquah, L.O.; Aunger, R.V. Planned, motivated and habitual hygiene behaviour: An eleven country review. Health Educ. Res. 2009, 24, 655–673. [Google Scholar] [CrossRef] [PubMed]
- Approaches to Promote Handwashing and Sanitation Behaviour Change in Low- and Middle-Income Countries: A Mixed Method Systematic Review—De Buck—2017—Campbell Systematic Reviews—Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/full/10.4073/csr.2017.7 (accessed on 28 September 2023).
- Tzikas, A.; Koulierakis, G. A systematic review of nudges on hand hygiene against the spread of COVID-19. J. Behav. Exp. Econ. 2023, 105, 102046. [Google Scholar] [CrossRef] [PubMed]
- WASH in Schools Network. Using Environmental Nudges to Improve Handwashing with Soap Among School Children—A Resource Guide for Rapidly Deployable Interventions for Use as an Interim Measure During School Reopenings. Available online: https://www.susana.org/en/knowledge-hub/resources-and-publications/library/details/3921# (accessed on 7 December 2022).

| Characteristic | Pre-Intervention n (%) N = 289 | Post-Intervention n (%) N = 275 |
|---|---|---|
| Sex | ||
| Male | 151 (52.3) | 160 (58.2) |
| Female | 138 (47.8) | 115 (41.8) |
| Time | ||
| School entrance | 81 (28.0) | 35 (12.7) |
| After restroom | 84 (29.1) | 120 (43.6) |
| Before eating | 124 (42.9) | 120 (43.6) |
| HH assistant present | ||
| Yes | 129 (44.6) | 27 (10.0) |
| No | 160 (55.4) | 242 (89.9) * |
| School location | ||
| Urban | 93 (32.2) | 100 (36.4) |
| Rural | 196 (67.8) | 175 (63.6) |
| Covariate | Appropriate HH Practices (Pre-Intervention) n (% *) | Appropriate HH Practices (Post-Intervention) n (% *) | Percent Change | p-Value |
|---|---|---|---|---|
| Appropriate HH practices | 148 (51.2) | 91 (33.1) | −18.1 | p < 0.001 |
| HH Time | ||||
| At entrance | 80 (98.8) | 15 (42.9) | −55.9 | p < 0.001 |
| After restroom | 36 (42.9) | 30 (25.0) | −17.9 | p < 0.01 |
| Before eating | 32 (25.8) | 46 (38.3) | 12.5 | p < 0.05 |
| Sex | ||||
| Male | 67 (44.4) | 46 (28.8) | −15.6 | p < 0.01 |
| Female | 81 (58.7) | 45 (39.1) | −19.6 | p < 0.001 |
| HH assistant | ||||
| Yes | 97 (75.2) | 27 (100.0) | 24.8 | p < 0.05 |
| No | 51 (31.9) | 64 (26.5) | −5.5 | p < 0.01 |
| School location | ||||
| Urban | 34 (36.6) | 27 (27.0) | −9.6 | p < 0.001 |
| Rural | 114 (58.2) | 64 (36.6) | −21.6 | p < 0.001 |
| OR (95% CI) | p-Value | aOR (95% CI) | p-Value | |
|---|---|---|---|---|
| HH Time | ||||
| At Entrance * | Ref. | Ref. | ||
| After Restroom | 0.15 (0.09–0.26) | <0.0001 | 0.41 (0.20–0.80) | 0.0099 |
| Before Eating | 0.08 (0.04–0.13) | <0.0001 | 0.18 (0.09–0.34) | <0.0001 |
| Sex | ||||
| Female | Ref. | Ref. | ||
| Male | 0.58 (0.41–0.81) | 0.0013 | 0.76 (0.51–1.13) | 0.174 |
| HH Assistance | ||||
| No | Ref. | Ref. | ||
| Yes | 9.67 (6.20–15.09) | <0.0001 | 6.69 (3.74–11.94) | <0.0001 |
| Locality | ||||
| Rural | Ref. | Ref. | ||
| Urban | 0.51 (0.35–0.72) | 0.0002 | 0.42 (0.27–0.65) | 0.0001 |
| Evaluation | ||||
| Pre-intervention | Ref. | Ref. | ||
| Post-intervention | 0.47 (0.34–0.66) | <0.0001 | 0.95 (0.62–1.45) | 0.8025 |
| Characteristic | Pre-intervention (N = 82) n (%) | Post-Intervention (N = 126) n (%) |
|---|---|---|
| Sex | ||
| Male | 41 (50.0) | 78 (61.9) |
| Female | 41 (50.0) | 48 (38.1) |
| Age (years) | ||
| 5–8 | 7 (8.5) | 29 (23.0) |
| 9–12 | 71 (86.6) | 88 (69.8) |
| 13 or older | 4 (4.9) | 9 (7.1) |
| Time | ||
| School entrance | 29 (35.4) | 42 (33.3) |
| After restroom | 26 (31.7) | 42 (33.3) |
| Before eating | 27 (32.9) | 42 (33.3) |
| School location | ||
| Urban | 23 (28.1) | 42 (33.3) |
| Rural | 59 (72.0) | 84 (66.7) |
| qPHAT Score | Pre intervention (N = 82) Median (IQR) | Post intervention (N = 126) Median (IQR) | Difference in Median |
|---|---|---|---|
| Overall | 6 (3) | 8 (3) | 2 |
| Time | |||
| At entrance | 5 (2) | 7 (2) | 2 |
| After restroom | 7 (2) | 9 (2) | 2 |
| Before eating | 5 (3) | 5 (3) | 0 |
| Sex | |||
| Male | 7 (2) | 8 (3) | 1 |
| Female | 5 (2) | 7 (3) | 2 |
| School location | |||
| Rural | 7 (3) | 7 (3) | 0 |
| Urban | 5 (2) | 8 (3) | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pieters, M.M.; Fahsen, N.; Hug, C.; Ishida, K.; Cordon-Rosales, C.; Lozier, M.J. A Quasi-Experimental Pre-Post Assessment of Hand Hygiene Practices and Hand Dirtiness Following a School-Based Educational Campaign. Int. J. Environ. Res. Public Health 2025, 22, 1198. https://doi.org/10.3390/ijerph22081198
Pieters MM, Fahsen N, Hug C, Ishida K, Cordon-Rosales C, Lozier MJ. A Quasi-Experimental Pre-Post Assessment of Hand Hygiene Practices and Hand Dirtiness Following a School-Based Educational Campaign. International Journal of Environmental Research and Public Health. 2025; 22(8):1198. https://doi.org/10.3390/ijerph22081198
Chicago/Turabian StylePieters, Michelle M., Natalie Fahsen, Christiana Hug, Kanako Ishida, Celia Cordon-Rosales, and Matthew J. Lozier. 2025. "A Quasi-Experimental Pre-Post Assessment of Hand Hygiene Practices and Hand Dirtiness Following a School-Based Educational Campaign" International Journal of Environmental Research and Public Health 22, no. 8: 1198. https://doi.org/10.3390/ijerph22081198
APA StylePieters, M. M., Fahsen, N., Hug, C., Ishida, K., Cordon-Rosales, C., & Lozier, M. J. (2025). A Quasi-Experimental Pre-Post Assessment of Hand Hygiene Practices and Hand Dirtiness Following a School-Based Educational Campaign. International Journal of Environmental Research and Public Health, 22(8), 1198. https://doi.org/10.3390/ijerph22081198







