Using Machine Learning to Predict Resilience Among Nurses in a South African Setting
Abstract
1. Introduction
2. The Present Study
3. Materials and Methods
3.1. Setting and Sample
3.2. Predictors and Outcome Metric
3.3. Statistical Analysis
3.4. Ethical Considerations
4. Results
4.1. Demographics
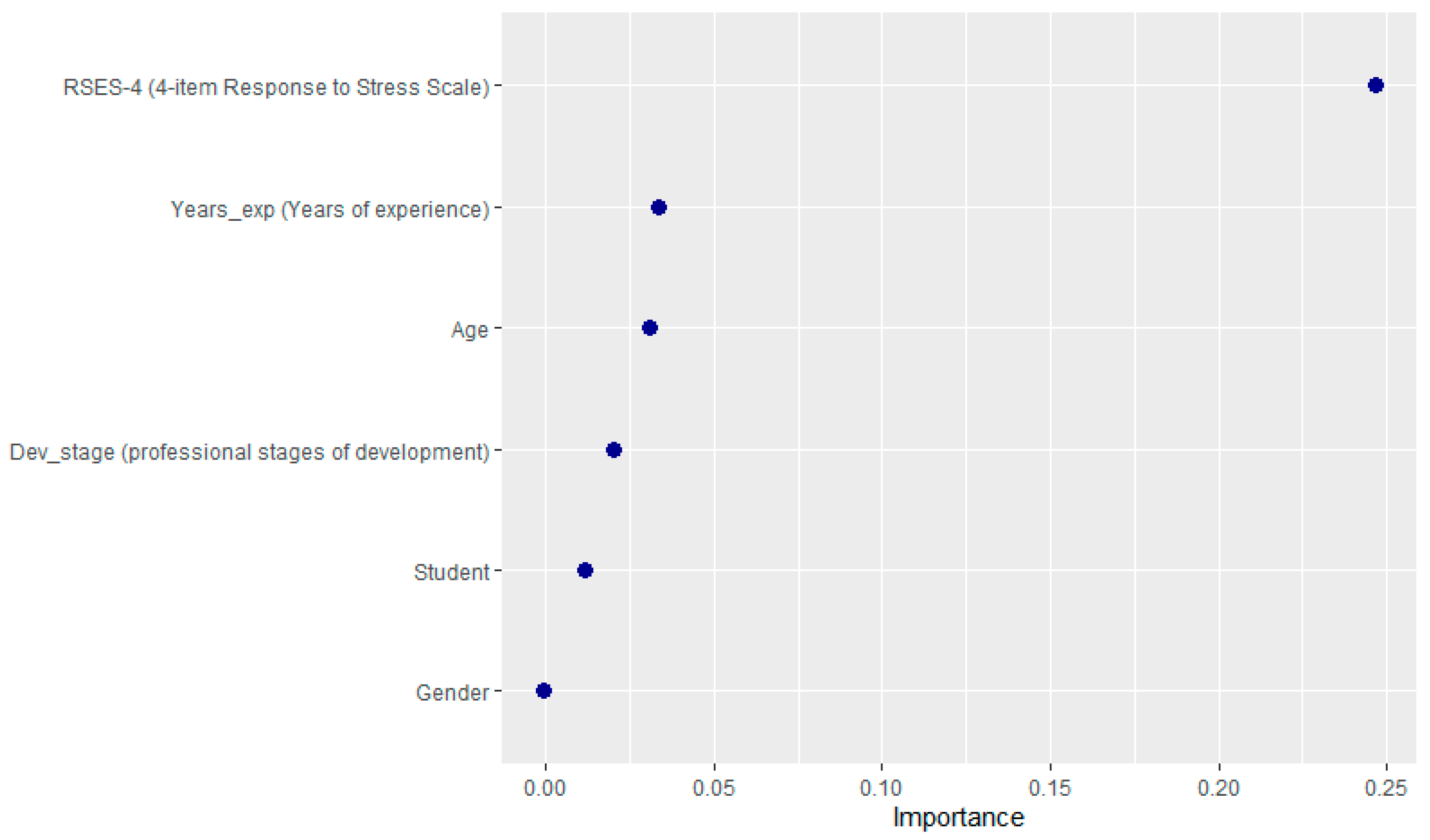
4.2. Key Predictors
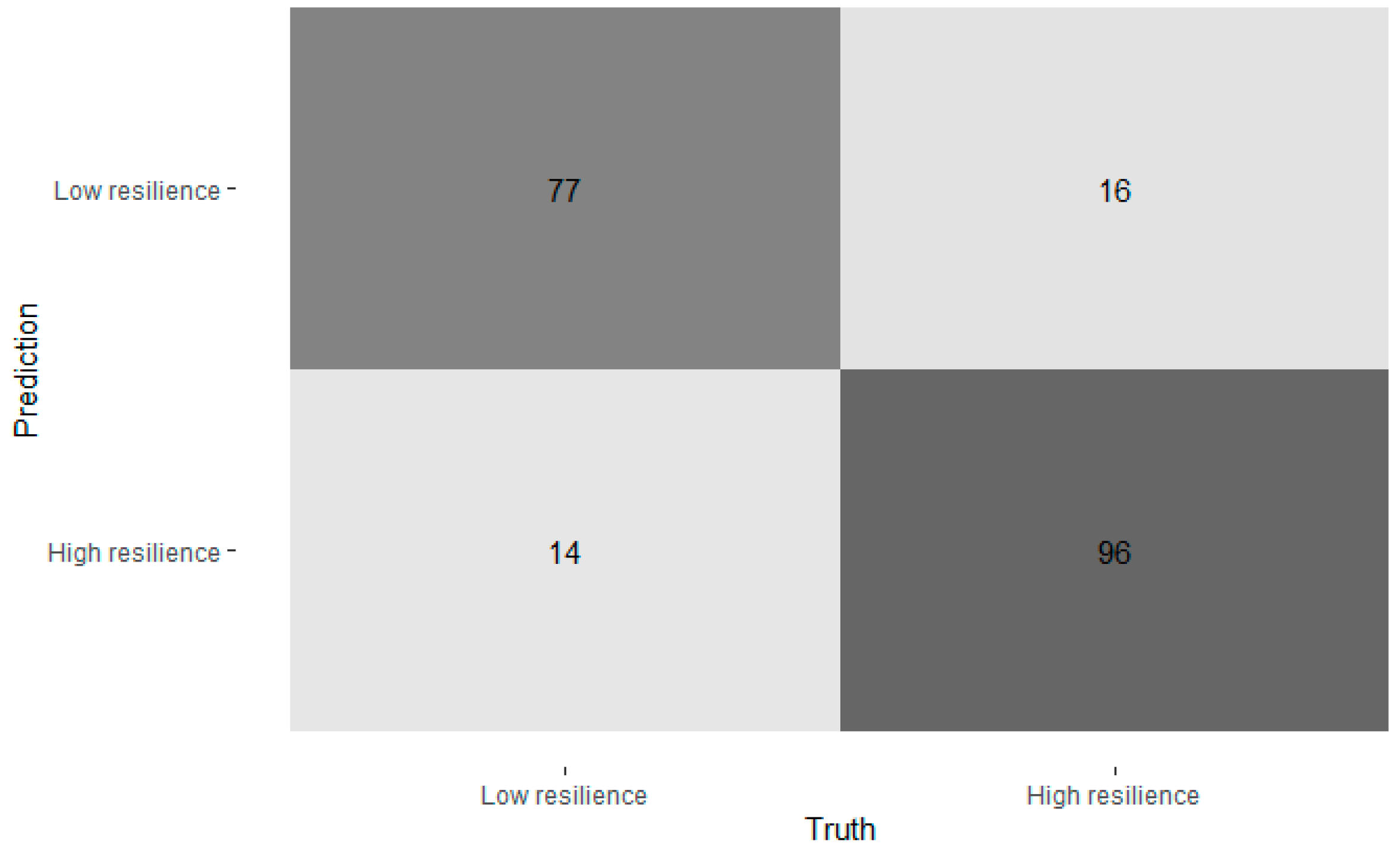
4.3. Accuracy
4.4. Random Forest Classification Predicting Resilience Levels
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bobbio, A.; Manganelli, A.M. Antecedents of hospital nurses’ intention to leave the organization: A cross sectional survey. Int. J. Nurs. Stud. 2015, 52, 1180–1192. [Google Scholar] [CrossRef] [PubMed]
- Khamisa, N.; Oldenburg, B.; Peltzer, K.; Ilic, D. Work Related Stress, Burnout, Job Satisfaction and General Health of Nurses. Int. J. Environ. Res. Public Health 2015, 12, 652–666. [Google Scholar] [CrossRef] [PubMed]
- Khamisa, N.; Peltzer, K.; Ilic, D.; Oldenburg, B. Work related stress, burnout, job satisfaction and general health of nurses: A follow-up study. Int. J. Nurs. Pract. 2016, 22, 538–545. [Google Scholar] [CrossRef] [PubMed]
- Young, T.; Dickinson, N.; Yau, H.L.O.; Watson, B. ‘An emotional roller coaster’: Fertility nurses’ stressors, wellbeing, burnout and work engagement through a mixed methods investigation. Aust. J. Adv. Nurs. 2025, 42, 40–52. [Google Scholar] [CrossRef]
- Xavier, T.; Hittle, B.M.; Rojas-Guyler, L.; Lee, R.C. Resilience in Intensive Care Unit Nurses: An Integrative Review. Crit. Care Nurse 2024, 44, 52–63. [Google Scholar] [CrossRef]
- Manomenidis, G.; Panagopoulou, E.; Montgomery, A. Resilience in nursing: The role of internal and external factors. J. Nurs. Manag. 2019, 27, 172–178. [Google Scholar] [CrossRef]
- Cooper, A.L.; Brown, J.A.; Rees, C.S.; Leslie, G.D. Nurse resilience: A concept analysis. Int. J. Ment. Health Nurs. 2020, 29, 553–575. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Brewin, C.R.; Kaniasty, K.; Greca, A.M.L. Weighing the Costs of Disaster: Consequences, Risks, and Resilience in Individuals, Families, and Communities. Psychol. Sci. Public Interest 2010, 11, 1–49. [Google Scholar] [CrossRef]
- Johnson, D.C.; Polusny, M.A.; Erbes, C.R.; King, D.; King, L.; Litz, B.T.; Schnurr, P.P.; Friedman, M.; Pietrzak, R.H.; Southwick, S.M. Development and Initial Validation of the Response to Stressful Experiences Scale. Mil. Med. 2011, 176, 161–169. [Google Scholar] [CrossRef]
- Yu, F.; Raphael, D.; Mackay, L.; Smith, M.; King, A. Personal and work-related factors associated with nurse resilience: A systematic review. J. Nurs. Stud. 2019, 93, 129–140. [Google Scholar] [CrossRef]
- Shandhi, M.M.H.; Dunn, J.P. AI in medicine: Where are we now and where are we going? Cell Rep. Med. 2022, 3, 100861. [Google Scholar] [CrossRef] [PubMed]
- Jiesisibieke, Z.L.; Ye, M.; Xu, W.; Chuang, Y.C.; Liou, J.J.; Tung, T.H.; Chien, C.W. Academic resilience of nursing students during COVID-19: An analysis using machine learning methods. Nurs. Open 2024, 11, e70018. [Google Scholar] [CrossRef]
- Van Zyl-Cillié, M.M.; Bührmann, J.H.; Blignaut, A.J.; Demirtas, D.; Coetzee, S.K. A machine learning model to predict the risk factors causing feelings of burnout and emotional exhaustion amongst nursing staff in South Africa. BMC Health Serv. Res. 2024, 24, 1665. [Google Scholar] [CrossRef]
- Tsai, E.R.; Demirtas, D.; Hoogendijk, N.; Tintu, A.N.; Boucherie, R.J. Turnaround time prediction for clinical chemistry samples using machine learning. Clin. Chem. Lab. Med. 2022, 60, 1902–1910. [Google Scholar] [CrossRef]
- De La Rosa, G.M.; Webb-Murphy, J.A.; Johnston, S.L. Development and Validation of a Brief Measure of Psychological Resilience: An Adaptation of the Response to Stressful Experiences Scale. Mil. Med. 2016, 181, 202–208. [Google Scholar] [CrossRef]
- R Core Team. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Yu, F.; Chu, G.; Yeh, T.; Fernandez, R. Effects of interventions to promote resilience in nurses: A systematic review. J. Nurs. Stud. 2024, 157, 104825. [Google Scholar] [CrossRef]
- Ponder, W.N.; Prosek, E.A.; Sherrill, T. Validation of the Adapted Response to Stressful Experiences Scale (RSES-4) Among First Responders. Prof. Couns. 2021, 11, 300–312. [Google Scholar] [CrossRef]
- Robertson, I.T.; Cooper, C.L.; Sarkar, M.; Curran, T. Resilience training in the workplace from 2003 to 2014: A systematic review. J. Occup. Organ. Psychol. 2015, 88, 533–562. [Google Scholar] [CrossRef]
- Sansó, N.; Vidal-Blanco, G.; Galiana, L. Development and Validation of the Brief Nursing Stress Scale (BNSS) in a Sample of End-of-Life Care Nurses. Nurs. Rep. 2021, 11, 311–319. [Google Scholar] [CrossRef]
- Mallon, A.; Mitchell, G.; Carter, G.; McLaughlin, D.; Wilson, C.B. A rapid review of evaluated interventions to inform the development of a resource to support the resilience of care home nurses. BMC Geriatr. 2023, 23, 275. [Google Scholar] [CrossRef]
- Dailah, H.G.; Koriri, M.; Sabei, A.; Kriry, T.; Zakri, M. Artificial Intelligence in Nursing: Technological Benefits to Nurse’s Mental Health and Patient Care Quality. Healthcare 2024, 12, 2555. [Google Scholar] [CrossRef] [PubMed]
- Inkster, B.; Sarda, S.; Subramanian, V. An Empathy-Driven, Conversational Artificial Intelligence Agent (Wysa) for Digital Mental Well-Being: Real-World Data Evaluation Mixed-Methods Study. JMIR mHealth uHealth 2018, 6, e12106. [Google Scholar] [CrossRef] [PubMed]
- Han, P.; Duan, X.; Jiang, J.; Zeng, L.; Zhang, P.; Zhao, S. Experience in the development of nurses’ personal resilience: A meta-synthesis. Nurs. Open 2023, 10, 2780–2792. [Google Scholar] [CrossRef] [PubMed]
- Ghasempour, S.; Abbasi, A.; Basirinezhad, M.H.; Dadgari, A.; Ebrahimi, H. Relationship between resilience and self-efficacy among Iranian nurses: A cross-sectional study during the post-Corona era. BMC Nurs. 2024, 23, 243. [Google Scholar] [CrossRef]
- Martinez, H.; Obod, M. Personal Optimism, Self-Efficacy and Resilience among nurses in a private medical centre amidst COVID-19 pandemic. Psychol. Appl. Trends 2023, 631–635. [Google Scholar] [CrossRef]
- Hampton, D.; Melander, S.; Rayens, M.K.; Langley, T. The relationship between resilience, self-efficacy, and job satisfaction among NPs and the impact of experience and education. Nurse Pract. 2025, 50, 22–30. [Google Scholar] [CrossRef]
- Zhang, D.; Du, L.; Wang, W.; Zhu, Q.; Bi, J.; Scovronick, N.; Naidoo, M.; Garland, R.M.; Liu, Y. A machine learning model to estimate ambient PM2.5 concentrations in industrialized highveld region of South Africa. Remote Sens. Environ. 2021, 266, 112713. [Google Scholar] [CrossRef]
- Chipps, J.; Penelope, M.; Jeffrey, H.; Margaret, W.; Olivia, B.; Fiona, W.; Jarvis, M.A. Evaluation of a digital programme for final year nursing students during COVID-19. Int. J. Afr. Nurs. Sci. 2022, 17, 100455. [Google Scholar] [CrossRef]
- Jarvis, M.A.; Martin, P.; Williams, M.; Walters, F.; Baloyi, O.B.; Hoffman, J.; Chipps, J. Stress and coping—Perceptions of final year nursing students returning to clinical practice during the COVID-19 pandemic, South Africa. Health SA Gesondheid 2021, 26, 1641. [Google Scholar] [CrossRef]
| Train | Test | |
|---|---|---|
| ‘Resilient’ (71–88) | 445 | 109 |
| ‘Less resilient’ (0–70) | 378 | 93 |
| Variable | Value |
|---|---|
| Age | |
| Mean age | 31.5 years |
| Range | 18–64 years |
| Gender | |
| Female | 874 (77.1%) |
| Male | 250 (22.0%) |
| Other | 10 (0.9%) |
| Stages of professional development | |
| Student nurses | 557 (49.1%) |
| Novice nurses (0–2 years’ experience) | 70 (6.2%) |
| Early-career nurses (3–5 years’ experience) | 113 (10.0%) |
| Mid-career nurses (6–15 years’ experience) | 245 (21.6%) |
| Experienced nurses (16–25 years’ experience) | 78 (6.9%) |
| Veterans (26+ years’ experience) | 54 (4.8%) |
| RSES-22 (0–88) | |
| Mean, SD | 69.8 (±15.8) |
| ‘Less resilient’ (0–70) | 519 (45.7%) |
| ‘Resilient’ (71–88) | 614 (54.1%) |
| RSES-4 (0–16) | |
| Mean, SD | 13.1 (±2.9) |
| Metric | Value | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Overall Accuracy | 86.41% | [0.810, 0.908] | <0.001 |
| No-Information Rate | 53.88% | — | — |
| Sensitivity (True Positive Rate) | 83.16% (79/95) | — | — |
| Specificity (True Negative Rate) | 89.19% (99/111) | — | — |
| Positive Predictive Value (PPV) | 86.81% | — | — |
| Negative Predictive Value (NPV) | 86.09% | — | — |
| Cohen’s Kappa (κ) | 0.726 | — | — |
| McNemar’s Test (Symmetry) | — | — | 0.571 |
| Balanced Accuracy | 86.17% | — | — |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chipps, J.; Cromhout, A.; Tokac, U. Using Machine Learning to Predict Resilience Among Nurses in a South African Setting. Int. J. Environ. Res. Public Health 2025, 22, 996. https://doi.org/10.3390/ijerph22070996
Chipps J, Cromhout A, Tokac U. Using Machine Learning to Predict Resilience Among Nurses in a South African Setting. International Journal of Environmental Research and Public Health. 2025; 22(7):996. https://doi.org/10.3390/ijerph22070996
Chicago/Turabian StyleChipps, Jennifer, Amanda Cromhout, and Umit Tokac. 2025. "Using Machine Learning to Predict Resilience Among Nurses in a South African Setting" International Journal of Environmental Research and Public Health 22, no. 7: 996. https://doi.org/10.3390/ijerph22070996
APA StyleChipps, J., Cromhout, A., & Tokac, U. (2025). Using Machine Learning to Predict Resilience Among Nurses in a South African Setting. International Journal of Environmental Research and Public Health, 22(7), 996. https://doi.org/10.3390/ijerph22070996








