Abstract
Travestis and transgender women in Brazil face a disproportionate burden of mental health conditions, exacerbated by structural discrimination, violence, and social exclusion. This narrative review synthesizes evidence on the prevalence of depression, anxiety, suicidality, and substance use among travestis and transgender women in Brazil, and examines intersecting social and health disparities. We searched PubMed, Embase, and PsycINFO in April 2025, identifying peer-reviewed studies in English or Portuguese reporting mental health outcomes or associated social determinants of health in this population. Thirty-one studies across twelve different cities (n = 7683) were included and grouped into two thematic domains. Reported prevalence ranged from 16–70.1% for depression, 24.8–26.5% for anxiety, and 25–47.3% for suicidality. Substance use was also highly prevalent, with studies reporting high rates of alcohol (21.5–72.7%), tobacco (56.6–61.6%), cannabis (19–68.9%), and cocaine/crack (6–59.8%) use. Discrimination, violence, economic hardship, and HIV were consistently associated with psychological distress and barriers to care. These findings underscore the urgent need to integrate mental health, gender-affirming care, and HIV services into Brazil’s Unified Health System (Sistema Único de Saúde–SUS), strengthen anti-discrimination and violence-prevention policies, and adopt inclusive public health strategies that prioritize the leadership and lived experiences of transgender, nonbinary, and gender diverse people, particularly amid rising political threats to gender-affirming care.
1. Introduction
Transgender, nonbinary, and gender diverse people across the globe experience a disproportionate burden of mental health conditions due to pervasive societal stigma, discrimination, and structural inequities [1,2,3]. In Brazil, an estimated 2% of the adult population—nearly three million people—identify as transgender, nonbinary, and gender diverse people [4]. These communities face health disparities that are further compounded by widespread social exclusion and violence [5]. Notably, Brazil has accounted for approximately one-third of all reported global murders of transgender, nonbinary, and gender diverse people over the past 17 years [6,7]. In parallel, HIV prevalence among travestis—a culturally specific gender identity within the transfeminine spectrum in Latin America [8]—and transgender women in Brazil remains alarmingly high, ranging from 24% to 54%, underscoring the urgent need for inclusive, equity-oriented public health strategies [9,10,11,12].
Evidence consistently shows that transgender, nonbinary, and gender diverse people are at elevated risk for depression, anxiety, and suicidality compared to cisgender populations [13,14,15]. A meta-analysis reported pooled prevalence rates of 50% for lifetime suicidal ideation and 29% for lifetime suicide attempts among transgender, nonbinary, and gender diverse people [16]. In another study involving over 600 transgender, nonbinary, and gender diverse adults, 72.2% had received a lifetime diagnosis of depression, and 73% had received a lifetime diagnosis of anxiety [17]. These disparities are often explained through the minority stress model, which posits that chronic exposure to structural and interpersonal discrimination contributes to sustained psychological distress [18,19]. Studies across multiple settings have further demonstrated associations between societal stigma and increased risk of poor mental health outcomes and barriers to healthcare access [20,21,22].
In Brazil, these mental health risks are exacerbated by systemic barriers within the public healthcare system [23]. The Brazilian Unified Health System (Sistema Único de Saúde–SUS), founded on principles of universality, integrality, and equity, offers free and universal healthcare [24]. However, the implementation of gender-affirming care and mental health services for transgender, nonbinary, and gender diverse people remains limited and unevenly distributed across regions [25]. Although gender-affirming care, including hormone therapies and gender-affirming surgeries, is formally recognized within SUS, access is largely concentrated in a small number of specialized urban centers with long waitlists [26]. In addition, mental health services tailored to this marginalized population are rarely integrated into primary care or HIV prevention and treatment programs, despite the syndemic overlap between HIV, psychological distress, and structural vulnerability [5]. Inadequate provider training, discrimination in healthcare settings, and logistical barriers further restrict access to care and reinforce existing inequities [5].
Despite increasing global recognition of the health disparities affecting transgender, nonbinary, and gender diverse communities [27], there remains a lack of consolidated evidence in Brazil that synthesizes mental health outcomes and their intersecting social determinants. Many existing reviews examined mental health across broader LGBTQIA+ communities but they have not focused specifically on travestis and transgender women [5,26,28,29,30], or they examined only HIV-related outcomes [31,32]. To address this gap, we conducted a narrative review to: (1) provide an overview of the prevalence of depression, anxiety, suicidality, and substance use among travestis and transgender women in Brazil, focusing on these communities given the predominance of existing studies; (2) examine intersecting social and health disparities, including discrimination, violence, economic exclusion, and HIV and other health outcomes; and (3) propose public health policy strategies grounded in equity, integration, and expanded access to mental health and gender-affirming care within SUS for this highly marginalized population.
2. Materials and Methods
2.1. Search Strategy
We conducted a narrative review of articles reporting on mental health outcomes among travestis and transgender women in Brazil. The search was carried out across three databases—PubMed, Embase, and PsycINFO—without date restrictions. We developed search terms to capture a broad range of mental health outcomes and used combinations of terms related to gender identity (e.g., “travesti,” “transgender,” “transgender woman,” “transgender women,” “trans woman,” “trans women,” “gender diverse”) and mental health (e.g., “depression,” “anxiety,” “suicidality,” “suicidal,” “suicide,” “substance,” “substance-related disorder,” “substance use disorder,” “alcohol,” “tobacco,” “cannabis,” “marijuana,” “cocaine,” “crack,” “amphetamine,” “methamphetamine,” “opioid,” “heroin,” “inhalant,” “ecstasy,” “polysubstance” “mental disorder,” “mental health”), along with “Brazil.” The search was first conducted in December 2023 and updated in April 2025.
2.2. Eligibility Criteria
We included studies that met the following criteria: (1) included travestis or transgender women; (2) examined mental health outcomes, including depression, anxiety, suicidality, and/or substance use; or reported on social determinants of health, including discrimination, physical, psychological, and sexual violence, economic hardship, and HIV and other health outcomes; (3) presented prevalence estimates for mental health outcomes and effect measures for social determinants of health; (4) were peer-reviewed; and (5) were published in English or Portuguese. We excluded case reports, case series, qualitative-only studies, abstracts, protocols, and studies where outcomes were reported alongside transgender men and nonbinary people and could not be extracted separately for travestis and transgender women.
2.3. Study Selection and Data Extraction
All records were screened by title and abstract, followed by full-text review of potentially eligible articles. Discrepancies were resolved through discussion and consensus. A standardized data extraction form was used to collect the following information: author(s), year of publication, study location(s), sample size, participant characteristics, mental health outcomes and/or social determinants of health assessed, and key prevalence or association estimates (e.g., odds ratios [OR], risk ratios [RR], prevalence rates [PR]).
2.4. Data Synthesis
Given the heterogeneity in study design, measurement tools, and outcome definitions, a narrative synthesis approach was adopted. Results were grouped into two main domains: (1) mental health outcomes, including depression, anxiety, suicidality, and substance use, and (2) intersecting social and health disparities, including discrimination, physical, psychological, and sexual violence, economic hardship, and HIV and other health outcomes. When different publications reported distinct outcomes from the same study cohort, we included each publication separately and noted the overlapping cohorts. Outcomes were reported as described in the original studies, which varied in timeframe (e.g., lifetime vs. recent) and in operationalization. In some cases, studies reported the presence of any symptom or substance use, while others used standardized scales with defined cutoffs or severity categories. This variability was preserved to reflect the methodological diversity across the included literature. For ease of reference, studies were organized alphabetically by first author’s name in both summary tables. Key findings were summarized in tabular format, and effect estimates were reported as ranges where applicable. No quantitative meta-analysis was conducted due to the narrative nature of the review and substantial heterogeneity across studies.
3. Results
3.1. Overview of Included Studies
We included a total of thirty-one studies (k = 31) [9,10,11,12,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. Ten studies (k = 10) examined mental health outcomes among travestis and transgender women in Brazil [12,33,34,35,36,37,38,39,40,41]. Specifically, six (k = 6) focused on depression [12,33,34,35,36,37], two (k = 2) on anxiety [35,36], four (k = 4) on suicidality [35,36,38,39], and six (k = 6) on substance use [12,35,37,39,40,41]. Twenty-six studies (k = 26) reported on intersecting social and health disparities [9,10,11,12,33,35,38,39,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59], including five (k = 5) on discrimination [42,43,44,45,46], nine (k = 9) on violence [33,35,38,39,42,44,47,48,49], two (k = 2) on economic difficulties [12,43], and fourteen (k = 14) on HIV and health disparities [9,10,11,12,50,51,52,53,54,55,56,57,58,59]. After removing studies that analyzed overlapping cohorts, the total number of unique participants across studies was 7683 travestis and transgender women. The studies were conducted across multiple Brazilian cities: São Paulo (SP) (k = 15) [11,35,37,39,41,43,44,45,47,49,50,51,53,55,56], Salvador (BA) (k = 12) [10,11,33,34,41,43,44,46,47,51,52,55], Rio de Janeiro (RJ) (k = 8) [12,38,42,48,54,57,58,59], Campo Grande (MS) (k = 6) [9,11,41,43,47,55], Porto Alegre (RS) (k = 6) [11,36,41,43,47,55], Manaus (AM) (k = 5) [11,41,43,47,55], Belo Horizonte (MG) (k = 3) [34,44,51], Fortaleza (CE) (k = 3) [10,33,46], Recife (PE) (k = 3) [10,33,46], Goiânia (GO) (k = 1) [40], Itumbiara (GO) (k = 1) [40], and Jataí (GO) (k = 1) [40]. Figure 1 illustrates the geographic distribution of included studies across cities and states in Brazil.

Figure 1.
Geographic distribution of studies on mental health and social determinants among travestis and transgender women across Brazilian cities and states.
3.2. Mental Health Outcomes Among Travestis and Transgender Women in Brazil
Substantial mental health challenges have been documented among travestis and transgender women in Brazil, particularly regarding depression, anxiety, suicidality, and substance use [12,33,34,35,36,37,38,39,40,41]. Table 1 shows these studies on mental health outcomes.

Table 1.
Mental health outcomes among travestis and transgender women in Brazil.
The burden of depression is especially pronounced among Brazilian travestis and transgender women, with studies reporting rates between 16% and 70.1% [12,33,34,35,36,37]. For example, in a multi-city study conducted in Fortaleza, Recife, and Salvador, 70.1% of participants exhibited symptoms of major depressive disorder (MDD) [33]. Similarly, a study across Belo Horizonte, Salvador, and São Paulo found that 69.6% reported depressive symptoms, with 44.6% experiencing severe cases [34]. Other studies found depressive symptoms in 57.8% of participants in Rio de Janeiro [12], 19.1% and 16% in São Paulo [35,37], and 16.6% in Porto Alegre [36]. While prevalence rates vary by region and methodology, they consistently indicate rates well above those observed in the general Brazilian population, where the estimated prevalence of depression is approximately 10.2% [60].
Anxiety and suicidality are also critical public health concerns among travestis and transgender women in Brazil. Anxiety symptoms were reported in 24.8% [36] to 26.5% [35] of participants in studies from São Paulo and Porto Alegre, nearly triple the national prevalence of 9.3% [61]. Suicidality was also particularly alarming, ranging from 25% to 47.25% for suicidal ideation and 27.25% to 39.8% for suicide attempts [35,36,38,39]. For instance, in Rio de Janeiro, 47.25% of participants had experienced suicidal ideation, and 27.25% had attempted suicide [38]. In Porto Alegre, 46.4% had a history of suicidal ideation and 31.2% of suicide attempt [36]. In São Paulo, suicidal ideation was reported by 25% of participants, with 31.2% reporting prior suicide attempts [35], while another study found a 39.8% prevalence of suicide attempts [39].
Substance use is also highly prevalent among Brazilian travestis and transgender women, with reported rates ranging from 1.3% for less common substances like hallucinogens or hypnotics to 72.7% for alcohol [12,35,37,39,40,41]. Notably, only tobacco and alcohol are legal substances in Brazil, and other commonly reported substances, such as cannabis, cocaine, and crack, are illegal for recreational use [62]. However, recent legal changes have decriminalized the possession of small amounts of cannabis for personal use under specific limits, while cannabis-based medications remain permitted in certain medical contexts [62]. Across studies, alcohol use ranged from 21.5% to 72.7% [12,35,37,39,40,41], tobacco from 56.6% to 61.6% [12,40,41], cannabis from 19% to 68.9% [12,35,37,40,41], and cocaine/crack from 6% to 59.8% [12,37,40,41]. For comparison, national estimates in the general population indicate a smoking prevalence of 11.3% [63], heavy episodic drinking at 17.1% [64], cannabis use at 2.1% [65], and crack-cocaine use at 2.2% [66]. Lifetime use of multiple substances, including inhalants, stimulants, and other drugs, was also frequent, with some studies reporting overall illicit or recreational drug use in 46% to 66.4% of participants [35,37,39,41]. Specifically, in a study conducted across Goiânia, Itumbiara, and Jataí, high rates of at-risk substance use were observed: marijuana (68.9%), tobacco (59.8%), cocaine/crack (59.8%), and binge drinking (56.6%) [40]. In São Paulo, alcohol use in the past year was reported by 72.7% of participants, while cannabis (46.8%) and stimulant use (44.4%) were also prevalent [35]. Another São Paulo-based study reported 30% alcohol use and 46% illicit or recreational drug use, including marijuana (19%), cocaine (15%), and crack (6%) [37]. In Rio de Janeiro, problematic use of tobacco (56.6%), cannabis (28.9%), cocaine (23.8%), and alcohol (21.5%) was also documented [12]. In addition, a multi-city study spanning Campo Grande, Manaus, Porto Alegre, Salvador, and São Paulo found high lifetime use of alcohol (65.5%), tobacco (61.6%), marijuana (52%), cocaine (42.6%), inhalants (14.6%), crack (13.9%), amphetamines/ecstasy (11.8%), and other substances, including hypnotics, hallucinogens, and opioids (1.3–13.1%) [41].
Taken together, these studies illustrate a mental health crisis among travestis and transgender women in Brazil. The consistently elevated prevalence rates across multiple indicators—depression, anxiety, suicidality, and substance use—signal a pattern of psychological distress shaped by social exclusion and systemic inequities [12,33,34,35,36,37,38,39,40,41]. Compared to population-level estimates for mental health disorders in Brazil [60,61], these rates are substantially higher, reinforcing the need for focused, culturally responsive mental health interventions for this marginalized community.
3.3. Intersecting Social and Health Disparities Faced by Travestis and Transgender Women in Brazil
In Brazil, the mental health of travestis and transgender women is shaped by a constellation of intersecting social determinants that exacerbate psychological distress and limit access to care. These include discrimination, violence, economic marginalization, and HIV-related disparities [9,10,11,12,33,35,38,39,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. Table 2 shows these studies on intersecting social and health disparities.

Table 2.
Intersecting social and health disparities faced by travestis and transgender women in Brazil.
Discrimination remains a widespread and compounding structural barrier. In Rio de Janeiro, 96% of participants reported experiencing discrimination, which was significantly associated with increased depressive symptoms [42]. In São Paulo, a study using the Intersectional Discrimination Index found that each unit increase in anticipated discrimination was associated with higher odds of severe psychological distress (adjusted odds ratio [aOR] = 2.13, 95% confidence interval [CI]: 1.57–2.89) and suicidality (aOR = 1.44, 95% CI: 1.08–1.93) [45]. In a multi-site study across Fortaleza, Recife, and Salvador, discrimination was associated with lower odds of seeking medical care (OR = 0.29; 95% CI: 0.14–0.63) and HIV testing (OR = 0.41; 95% CI: 0.22–0.78) [46]. Among adolescent travestis and transgender women (15–19 years) in Belo Horizonte, Salvador, and São Paulo, 50% reported experiencing discrimination six times or more [44]. Similarly, in the national TransOdara study, 85% of participants across Campo Grande, Manaus, Porto Alegre, Salvador, and São Paulo reported some form of discrimination [43]. Alarmingly, in this study, 23% had been arrested, yet fewer than 1% were placed in dedicated LGBTQIA+ detention spaces, highlighting institutional neglect and structural violence [43].
Experiences of violence further compound these disparities. In Rio de Janeiro, 52% of travestis and transgender women reported physical violence, and 42% reported sexual violence—both of which were significantly associated with increased depressive symptoms [42]. Another study from the same city found that physical violence was associated with increased suicidal ideation (adjusted prevalence ratio [aPR] = 1.37; 95% CI: 1.09–1.71) and suicide attempts (aPR = 1.92; 95% CI: 1.28–2.88) [38]. Childhood abuse was also identified as a critical factor in Rio de Janeiro: emotional abuse—defined as experiences such as being insulted or cursed at by parents, or hearing them express regret that the child had been born—was associated with suicide attempts (OR = 9.00; 95% CI: 1.13–71.34) [48]. In the same study, emotional neglect—characterized by not feeling supported or loved, or being special—was associated with self-injurious behavior (OR = 11.64; 95% CI: 2.35–57.5) [48]. In the TransOdara study, which included participants from five Brazilian cities, 14.2% of travestis and transgender women reported having experienced physical violence [47], and 51% reported being forced to have sex [43]. Similarly, high rates were observed in São Paulo, where 45.1% of participants had suffered sexual violence [39]. Another study from the same city reported that 62% had experienced physical violence and 45% sexual violence [49]. In addition, lifetime sexual violence was associated with a 56% reduction in HIV viral suppression (adjusted risk ratio [aRR]: 0.44, 95% CI: 0.24–0.79) in that study [49]. In another analysis from São Paulo, sexual violence was associated with both suicidal ideation and suicide attempts (OR = 1.69; 95% CI: 1.18–2.44) [35], and among adolescent (15–19 years) travestis and transgender women in Belo Horizonte, Salvador, and São Paulo, 45% reported having suffered sexual violence [51]. Lastly, in northeastern cities including Fortaleza, Recife, and Salvador, both physical (OR = 2.09; 95% CI: 1.20–3.67) and sexual violence (OR = 2.06; 95% CI: 1.15–3.68) were associated with mild to moderate symptoms of MDD [33].
Economic hardship is another central factor. In the TransOdara study, 37.6% of travestis and transgender women reported unstable housing, only 8.4% were formally employed, and 57% earned up to one minimum wage [43]. Additionally, 73.7% had engaged in transactional sex, and 21.3% identified sex work as their main income source [43]. In a Rio de Janeiro study, 78.6% of participants reported current or past engagement in sex work, and 62% earning less than USD 10 per day [12].
HIV-related disparities further deepen health inequities. HIV prevalence was reported at 54% in Rio de Janeiro [12], 34% in the TransOdara study across five cities [11], 24.5% in a multicenter study conducted across Fortaleza, Recife, and Salvador [10], and 24% in Campo Grande [9]. Two studies in Salvador found HIV prevalence ranging from 9% to 24.3%, with gender-based discrimination associated with testing positive for HIV (OR = 8.65; 95% CI: 1.45–51.59) [46]. In São Paulo, HIV prevalence was disproportionately high among younger travestis and transgender women (ages 18–24) (RR = 3.85; 95% CI: 1.24–12.93) compared to older peers [53]. Two studies in Rio de Janeiro and São Paulo found that a history of sex work was associated with newly diagnosed HIV cases (OR = 30.7; 95% CI: 3.5–267.3 and RR = 5.90; 95% CI: 1.71–26.62, respectively) [53,54]. Among participants living with HIV in the TransOdara study, 42% had a detectable viral load, despite most being on antiretroviral therapy (ART) [55]. Younger age (PR = 2.26; 95% CI: 1.13–4.51), poor housing (PR = 2.72; 95% CI: 1.30–5.68), and self-rated poor/very poor mental health (PR = 1.70; 95% CI: 1.08–2.66) were associated with unsuppressed viremia [55]. Moreover, discrimination emerged as a key impediment to consistent engagement in HIV care services. A mediation analysis in São Paulo found that anticipated stigma was associated with reluctance to report new symptoms to healthcare providers among travestis and transgender women living with HIV (aOR = 7.42; 95% CI: 1.93–28.5) [56]. Lastly, in terms of health disparities in São Paulo, 36.8% reported current use of nonprescribed hormones due to factors such as financial hardship, with the highest rates among those aged 18–25 (49.1%) [50].
Among those not living with HIV, travestis and transgender women in Rio de Janeiro aged 18–24 had lower knowledge of HIV pre-exposure prophylaxis (PrEP) (OR = 0.5; 95% CI: 0.3–0.8) and HIV post-exposure prophylaxis (PEP) (OR = 0.5; 95% CI: 0.3–0.9), and were more likely to engage in high-risk behaviors, including at-risk substance use (OR = 1.8; 95% CI: 1.1–2.9) and unprotected sex (OR = 1.8; 95% CI: 1.1–3.0) [58]. In a multicenter study across Belo Horizonte, Salvador, and São Paulo, 79.3% of travestis and transgender women aged 15–19 reported condomless anal sex in the past six months [51]. In Rio de Janeiro, a study found higher odds of early loss to follow-up in PrEP care among travestis and transgender women (aOR = 2.8; 95% CI: 1.6–4.8) [59]. In another study from Rio de Janeiro, although 85.4% of participants were retained in care over 48 weeks, only 48.6% had high PrEP adherence based on tenofovir levels in dried blood spots [57]. Specifically, participants aged 18–24 had more missing study visits (aOR: 8.76; 95% CI: 2.09–36.7) compared to those aged 35+, and stimulant use was also associated with missed visits (aOR: 4.99; 95% CI: 1.37–18.1) [57].
Together, these findings demonstrate how structural and interpersonal factors, including discrimination, violence, economic hardship, HIV vulnerability, and health disparities, interact to exacerbate mental health conditions and restrict access to care among travestis and transgender women in Brazil [9,10,11,12,33,35,38,39,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. Compared to the general population, this group faces disproportionate exposure to psychosocial stressors and structural barriers [9,10,11,12,33,35,38,39,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59], underscoring the need for integrated, affirming, and equity-oriented policy interventions.
4. Discussion
This review synthesized evidence concerning mental health outcomes and intersecting social determinants affecting travestis and transgender women in Brazil. Across multiple studies and cities, elevated rates of depression, anxiety, suicidality, and substance use were consistently reported [12,33,34,35,36,37,38,39,40,41], alongside structural disparities including discrimination, violence, economic exclusion, and HIV vulnerability [9,10,11,12,33,35,38,39,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. These findings reveal a syndemic environment driven by systemic inequities and underscore the urgent need for integrated mental health and gender-affirming care strategies. Table 3 outlines key policy recommendations based on this review and their corresponding stakeholders, and Figure 2 provides a visual representation of the main policy areas.

Table 3.
Integrated policy recommendations and key stakeholders for comprehensive transgender mental healthcare in Brazil.
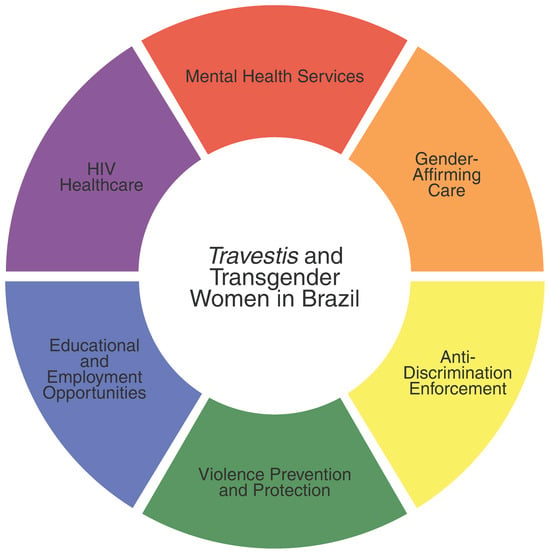
Figure 2.
Key policy areas to improve health equity for travestis and transgender women in Brazil.
A key implication is the need to expand mental health services, including psychotherapy, within Brazil’s public healthcare system. Travestis and transgender women face multiple barriers to care, including stigma, lack of trained providers, and limited access to specialized services [67]. Although full integration within SUS remains a logistical challenge, co-locating mental health support in existing gender-affirming care settings, HIV clinics, and primary care settings offers a feasible and equity-oriented approach. Initiatives such as those implemented by Fundação Oswaldo Cruz (Fiocruz), which offer integrated, community-based services tailored to transgender, nonbinary, and gender diverse people, demonstrate the feasibility and impact of such models in Brazil [12]. Moreover, enhancing referral systems, particularly in underserved regions, and investing in provider training are essential for improving access and retention [68,69].
In parallel, expanding access to gender-affirming care is critical. Although SUS formally recognizes services such as hormone therapies and gender-affirming surgeries, access remains limited and unevenly distributed, with services concentrated in large urban centers and often requiring complex referrals and long wait times [25,26]. These access gaps are exacerbated by recent political efforts to restrict transgender, nonbinary, and gender diverse rights nationally and globally, limiting healthcare protections and threatening progress toward equity and inclusion [70]. Robust evidence shows that gender-affirming care is associated with significant reductions in depression, anxiety, and suicidality, as well as improvements in quality of life and psychological well-being [71,72]. Ensuring that gender-affirming services are not only protected but expanded within SUS is essential to promoting mental health equity and upholding the human rights of travestis and transgender women in Brazil. This is particularly urgent in the context of a global political climate marked by growing hostility toward transgender, nonbinary, and gender diverse communities [70,73]. For example, in countries like the United States, recent legislative rollbacks have restricted access to gender-affirming care [70]. Similarly, Brazil has experienced periods of political regression, including increased anti-gender rhetoric, attempts to dismantle LGBTQIA+ protections, and, more recently, efforts to prohibit the use of pubertal suppression and hormone therapies for transgender, nonbinary, and gender diverse young people [73,74]. Therefore, it is essential to anchor public health strategies in a human rights framework to ensure access to care and to resist the politicization of health.
Structural discrimination must also be directly addressed. While anti-discrimination laws exist in Brazil, enforcement remains inconsistent across healthcare, education, and employment [75]. Strengthening legal protections and establishing accountability mechanisms are critical to preventing mistreatment and denial of care. National data show that travestis and transgender women may be more likely to access Basic Health Units (UBS), yet experiences of discrimination, especially from reception staff, significantly reduce continued service use [76]. This highlights the need for respectful, inclusive clinical environments and ongoing provider training. In addition, public awareness campaigns and digital tools like the Dandarah app, used by over 4000 LGBTQIA+ people to report violence and access psychosocial support [77], illustrate how technology can be leveraged to improve safety and strengthen connections to care, particularly in a context of pervasive violence against transgender, nonbinary, and gender diverse people in Brazil [6,7].
Equally important is addressing socioeconomic exclusion. As detailed in this review, many travestis and transgender women face chronic financial insecurity and rely on sex work as their primary—and often sole—source of income due to limited access to formal employment [12,55]. Advancing education and workforce inclusion is essential to breaking this cycle. Initiatives, such as PreparaNem, a university preparatory program for LGBTQIA+ students, create pathways to higher education and long-term mobility [78]. More recently, affirmative action policies at several Brazilian universities have emerged, following sustained advocacy from organizations such as the Associação Nacional de Travestis e Transexuais (ANTRA) and other LGBTQIA+ civil society groups [73,79]. These efforts should be complemented by inclusive policies at earlier educational levels, including primary and secondary schools, to reduce dropout rates and ensure safer, more supportive learning environments for transgender, nonbinary, and gender diverse young people. Employment programs like TransEmpregos, which connect transgender, nonbinary, and gender diverse people to inclusive job opportunities, also show promise in reducing poverty and improving mental health outcomes [80]. These programs deserve broader support and scale-up through partnerships with government and private employers.
In addition, strengthening HIV prevention and care must remain a national public health priority [81], particularly given the disproportionate burden of HIV among transgender, nonbinary, and gender diverse populations [82]. In addition, depression, substance use, and stigma can all compromise adherence to ART, exacerbating morbidity and inequities [46,52,56,57,58]. Integrating mental health support into HIV care settings and implementing routine mental health screening during HIV testing, prevention, and treatment could significantly improve outcomes. Expanding access to and awareness of PrEP, PEP, and community-based HIV testing is especially urgent among young transgender, nonbinary, and gender diverse people and those engaged in sex work, who face substantial barriers to care [54,57,58]. For example, a recent scoping review further identified low perceived risk, fear of confidentiality breaches, and younger age as key barriers to HIV rapid testing among travestis and transgender women in Brazil, while autonomy and favorable testing environments were cited as facilitators, especially in the context of self-testing [31]. These findings reinforce the value of youth-specific, privacy-preserving, and community-led strategies to improve HIV testing uptake and retention in care.
Ultimately, these policies must place transgender, nonbinary, and gender diverse populations at their core, centering their lived experiences and leadership. Community-based participatory research and inclusive governance, with ANTRA and other LGBTQIA+ groups engaged throughout, enhance relevance and methodological rigor. Funding frameworks must prioritize sustained support for community-driven advocacy and capacity building, while institutionalizing mechanisms for transgender, nonbinary, and gender diverse representation in decision-making bodies. As depicted in Figure 2, this people-centered approach not only upholds human rights and agency but is indispensable for advancing health equity and building an inclusive, resilient public health system.
This review has several strengths. To our knowledge, it is the first national synthesis focused specifically on mental health outcomes among travestis and transgender women in Brazil, integrating mental health data with structural vulnerabilities, such as discrimination, violence, economic exclusion, HIV, and other health disparities. The inclusion of studies from different regions allows for a more comprehensive snapshot of the health needs and lived experiences of this marginalized population. Additionally, the review brings together both epidemiological data and public policy implications, providing an evidence-based foundation for focused mental health and gender-affirming care strategies in the Brazilian context.
However, some limitations should be noted. The included studies varied in methodology, sample size, and outcome measures, limiting comparability. Most relied on cross-sectional data, with few longitudinal analyses. Moreover, many samples were drawn from urban settings and may not fully reflect the experiences of rural or Indigenous transgender, nonbinary, and gender diverse populations. This review was also conducted as a narrative review rather than a systematic or scoping review and focused exclusively on travestis and transgender women, given the predominance of research on this group in Brazil, thereby excluding studies on transgender men and nonbinary people. In addition, qualitative studies were not included, though they offer valuable insight into lived experiences. Future research should prioritize longitudinal and intervention studies to better understand causal pathways between structural violence and mental health outcomes, and to evaluate the effectiveness of integrated service models and policy reforms. Expanding gender identity data collection in national health surveys and improving surveillance systems will also be critical to increasing the visibility of Brazilian travestis and transgender women in health policy and research.
5. Conclusions
The mental health landscape for travestis and transgender women in Brazil presents significant challenges. While the studies included do not encompass all regions, they provide valuable insights and highlight the urgent need for tailored public health policies. It is a call to action for creating an inclusive and equitable environment while ensuring that the health and dignity of travestis and transgender women are not only recognized but are actively championed as a measure of Brazil’s commitment to equality and human rights.
Author Contributions
D.R.A.C. and S.L.R. conceptualized and designed the study. D.R.A.C. was involved with data acquisition, analysis, and interpretation. D.R.A.C. drafted the original manuscript. A.L.N.F., W.F.V., A.S.K. and S.L.R. revised the manuscript draft. A.S.K. and S.L.R. supervised the study. All authors critically revised the manuscript for important intellectual content, including data interpretation in the broader context. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
A.S.K. declares royalties as editor of a McGraw Hill textbook on transgender and gender diverse health care, and editor of an American Psychiatric Association textbook on gender-affirming psychiatric care. All other authors declare no competing interests.
References
- Beckwith, N.; McDowell, M.J.; Reisner, S.L.; Zaslow, S.; Weiss, R.D.; Mayer, K.H.; Keuroghlian, A.S. Psychiatric Epidemiology of Transgender and Nonbinary Adult Patients at an Urban Health Center. LGBT Health 2019, 6, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Reisner, S.L.; White Hughto, J.M.; Gamarel, K.E.; Keuroghlian, A.S.; Mizock, L.; Pachankis, J. Discriminatory Experiences Associated with Posttraumatic Stress Disorder Symptoms among Transgender Adults. J. Couns. Psychol. 2016, 63, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Pinna, F.; Paribello, P.; Somaini, G.; Corona, A.; Ventriglio, A.; Corrias, C.; Frau, I.; Murgia, R.; El Kacemi, S.; Galeazzi, G.M.; et al. Mental Health in Transgender Individuals: A Systematic Review. Int. Rev. Psychiatry 2022, 34, 292–359. [Google Scholar] [CrossRef] [PubMed]
- Spizzirri, G.; Eufrásio, R.; Lima, M.C.P.; de Carvalho Nunes, H.R.; Kreukels, B.P.C.; Steensma, T.D.; Abdo, C.H.N. Proportion of People Identified as Transgender and Non-Binary Gender in Brazil. Sci. Rep. 2021, 11, 2240. [Google Scholar] [CrossRef]
- Freitas, F.L.S.; Bermúdez, X.P.C.D.; Merchán-Hamann, E.; Dias dos Santos, A.S.; Vieira, V.F. Social and Programmatic Vulnerability in the Context of Transgender People’s Health: A Scoping Review of Scientific Evidence from Brazil. Int. J. Equity Health 2024, 23, 272. [Google Scholar] [CrossRef]
- Trans Murder Monitoring (TMM). TMM Update TDoR 2022; Transgender Europe (TGEU): Berlin, Germany, 2022; Available online: https://transrespect.org/en/tmm-update-tdor-2022/ (accessed on 19 April 2025).
- Benevides BG (Ed.) Dossiê Assassinatos e Violências Contra Travestis e Transexuais Brasileiras em 2021 [Dossier on Murders and Violence Against Brazilian Travestis and Transgender and Gender Diverse People in 2021]; Distrito Drag: Brasília, Brazil, 2023. [Google Scholar]
- Carvalho, M. “Travesti”, “mulher transexual”, “homem trans” e “não binário”: Interseccionalidades de classe e geração na produção de identidades políticas. Cad. Pagu 2018, 52, e185211. [Google Scholar] [CrossRef]
- Cesar, G.A.; do Lago, B.V.; Ortiz Tanaka, T.S.; Zanini, P.B.; Bandeira, L.M.; Puga, M.A.M.; Pires Fernandes, F.R.; Pinto, C.S.; Castro, L.S.; Bertolacci-Rocha, L.G.; et al. Differences in Risky Sexual Behaviors and HIV Prevalence between Men Who Have Sex with Men and Transgender Women in the Midwest Brazil. PLoS Glob. Public Health 2024, 4, e0003061. [Google Scholar] [CrossRef]
- Leite, B.O.; Magno, L.; Bastos, F.I.; Dourado, I. Association between In-Country Migration and HIV Infection among Transgender Women from Northeastern Brazil: A Respondent-Driven Sampling Survey. BMC Public Health 2024, 24, 589. [Google Scholar] [CrossRef]
- Dourado, I.; Magno, L.; Leite, B.O.; Bastos, F.I.; da Mota, J.C.; Veras, M.A.d.S.M. TransOdara Research Group Prevalence of HIV Infection among Transgender Women and Travestis in Brazil: Data from the TransOdara Study. Rev. Bras. Epidemiol. Braz. J. Epidemiol. 2024, 27 (Suppl. S1), e240004.supl.1. [Google Scholar] [CrossRef]
- Ferreira, A.C.G.; Coelho, L.E.; Jalil, E.M.; Luz, P.M.; Friedman, R.K.; Guimarães, M.R.C.; Moreira, R.C.; Eksterman, L.F.; Cardoso, S.W.; Castro, C.V.; et al. Transcendendo: A Cohort Study of HIV-Infected and Uninfected Transgender Women in Rio de Janeiro, Brazil. Transgender Health 2019, 4, 107–117. [Google Scholar] [CrossRef]
- Eccles, H.; Abramovich, A.; Patte, K.A.; Elton-Marshall, T.; Racine, N.; Ferro, M.A.; Edwards, J.; Anderson, K.K.; Afifi, T.O.; Geoffroy, M.-C.; et al. Mental Disorders and Suicidality in Transgender and Gender-Diverse People. JAMA Netw. Open 2024, 7, e2436883. [Google Scholar] [CrossRef] [PubMed]
- Hochheimer, M.; Glick, J.L.; Garrison-Desany, H.; Huhn, A.S. Transgender Individuals Are at Higher Risk for Suicidal Ideation and Preparation than Cisgender Individuals in Substance Use Treatment. Front. Psychiatry 2023, 14, 1225673. [Google Scholar] [CrossRef] [PubMed]
- Kidd, J.D.; Tettamanti, N.A.; Kaczmarkiewicz, R.; Corbeil, T.E.; Dworkin, J.D.; Jackman, K.B.; Hughes, T.L.; Bockting, W.O.; Meyer, I.H. Prevalence of Substance Use and Mental Health Problems among Transgender and Cisgender U.S. Adults: Results from a National Probability Sample. Psychiatry Res. 2023, 326, 115339. [Google Scholar] [CrossRef] [PubMed]
- Kohnepoushi, P.; Nikouei, M.; Cheraghi, M.; Hasanabadi, P.; Rahmani, H.; Moradi, M.; Moradi, G.; Moradpour, F.; Moradi, Y. Prevalence of Suicidal Thoughts and Attempts in the Transgender Population of the World: A Systematic Review and Meta-Analysis. Ann. Gen. Psychiatry 2023, 22, 28. [Google Scholar] [CrossRef]
- Kattari, S.K.; Kattari, L.; Johnson, I.; Lacombe-Duncan, A.; Misiolek, B.A. Differential Experiences of Mental Health among Trans/Gender Diverse Adults in Michigan. Int. J. Environ. Res. Public Health 2020, 17, 6805. [Google Scholar] [CrossRef]
- Meyer, I.H. Minority Stress and Mental Health in Gay Men. J. Health Soc. Behav. 1995, 36, 38–56. [Google Scholar] [CrossRef]
- Meyer, I.H. Prejudice, Social Stress, and Mental Health in Lesbian, Gay, and Bisexual Populations: Conceptual Issues and Research Evidence. Psychol. Bull. 2003, 129, 674–697. [Google Scholar] [CrossRef]
- Hajek, A.; König, H.-H.; Buczak-Stec, E.; Blessmann, M.; Grupp, K. Prevalence and Determinants of Depressive and Anxiety Symptoms among Transgender People: Results of a Survey. Healthcare 2023, 11, 705. [Google Scholar] [CrossRef]
- Ramos, N.; Marr, M.C. Traumatic Stress and Resilience Among Transgender and Gender Diverse Youth. Child Adolesc. Psychiatr. Clin. N. Am. 2023, 32, 667–682. [Google Scholar] [CrossRef]
- Sherman, A.D.F.; Higgins, M.K.; Balthazar, M.S.; Hill, M.; Klepper, M.; Schneider, J.S.; Adams, D.; Radix, A.; Mayer, K.H.; Cooney, E.E.; et al. Stigma, Social and Structural Vulnerability, and Mental Health among Transgender Women: A Partial Least Square Path Modeling Analysis. J. Nurs. Scholarsh. Off. Publ. Sigma Theta Tau Int. Honor Soc. Nurs. 2024, 56, 42–59. [Google Scholar] [CrossRef]
- Da Silva, S.A.G.; Miranda-Ribeiro, P.; Noronha, K.V.M.d.S.; Guedes, G.R. Exploring the Complexities and Challenges of Healthcare Access for Transgender People in Minas Gerais State: A Qualitative Study a Decade Following the Implementation of the Transsexualization Process in the Brazilian National Health System. Epidemiol. Serviços Saúde 2024, 33, e2024350. [Google Scholar] [CrossRef]
- Castro, M.C.; Massuda, A.; Almeida, G.; Menezes-Filho, N.A.; Andrade, M.V.; de Souza Noronha, K.V.M.; Rocha, R.; Macinko, J.; Hone, T.; Tasca, R.; et al. Brazil’s Unified Health System: The First 30 Years and Prospects for the Future. Lancet 2019, 394, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Bender, M.S.; Paz, I.; Beranger, K.S.; Garcia, E.L. Access Pathways to the Transsexualizing Process in Brazil: A Scoping Review. Epidemiol. Serviços Saúde 2025, 33, e2024311. [Google Scholar] [CrossRef]
- De Lima, R.R.T.; Flor, T.B.M.; Noro, L.R.A. Systematic Review on Health Care for Transvestites and Transsexuals in Brazil. Rev. Saúde Pública 2023, 57, 19. [Google Scholar] [CrossRef]
- Goldsen, K.I.F.; Romanelli, M.; Hoy-Ellis, C.P.; Jung, H. Health, Economic and Social Disparities among Transgender Women, Transgender Men and Transgender Nonbinary Adults: Results from a Population-Based Study. Prev. Med. 2022, 156, 106988. [Google Scholar] [CrossRef]
- Sales, J.M.R.d.; Lopes, G.d.S. Saúde Mental na Comunidade LGBTQIA+: Uma Revisão Narrativa da Literatura. Rev. Contemp. 2023, 3, 30720–30739. [Google Scholar] [CrossRef]
- Silva, L.S.R.d.; Silva, R.d.T.A.e; Moura, D.T.B.d.; Dias, V.D.M.M.; Araújo, N.F.d.; de Alencar, F.S. Cuidados em Saúde Mental da População LGBTQIAPN+ Frente à Assistência à Saúde: Mental health care of the LGBTQIAPN+ population in the face of health care. Cad. Bras. Saúde Ment. J. Ment. Health 2024, 16, 55–77. [Google Scholar]
- Francisco, L.C.F.d.L.; Barros, A.C.; Pacheco, M.D.S.; Nardi, A.E.; Alves, V.d.M. Ansiedade em minorias sexuais e de gênero: Uma revisão integrativa. J. Bras. Psiquiatr. 2020, 69, 48–56. [Google Scholar] [CrossRef]
- Toledo, L.d.S.G.; Palmieri, P.; Ribeiro, G.d.R.; Silva, A.d.; Bastos, F.I. Barriers and Facilitators for HIV Rapid Testing among Transgender Women and Gay and Other Men Who Have Sex with Men in Brazil: A Scoping Review. Glob. Public Health 2024, 19, 2360982. [Google Scholar] [CrossRef]
- Freitas, C.A.M.; Rossi, T.A.; Dourado, I.; Castellanos, M.E.P.; Guimarães, N.S.; Magno, L. Mapping Evidence on Health Promotion in HIV Testing among Men Who Have Sex with Men and Transgender Women Using the Social-Ecological Model and the Vulnerability Theoretical Framework: A Scoping Review. BMC Public Health 2023, 23, 1946. [Google Scholar] [CrossRef]
- Almeida, M.M.d.; Silva, L.A.V.d.; Bastos, F.I.; Guimarães, M.D.C.; Coutinho, C.; de Brito, A.M.; Cavalcante, S.; Dourado, I. Factors Associated with Symptoms of Major Depression Disorder among Transgender Women in Northeast Brazil. PLoS ONE 2022, 17, e0267795. [Google Scholar] [CrossRef] [PubMed]
- De Medeiros, D.S.; Magno, L.; Crosland Guimarães, M.D.; Grangeiro, A.; Filho, M.E.; Soares, F.; Greco, D.; Westin, M.; Ferraz, D.; Zucchi, E.M.; et al. Violence, Discrimination, and High Levels of Symptoms of Depression Among Adolescent Men Who Have Sex with Men and Transgender Women in Brazil. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2023, 73, S19–S25. [Google Scholar] [CrossRef] [PubMed]
- Reis, A.; Sperandei, S.; de Carvalho, P.G.C.; Pinheiro, T.F.; de Moura, F.D.; Gomez, J.L.; Porchat, P.; Bastos, F.I.; McFarland, W.; Wilson, E.C.; et al. A Cross-Sectional Study of Mental Health and Suicidality among Trans Women in São Paulo, Brazil. BMC Psychiatry 2021, 21, 557. [Google Scholar] [CrossRef] [PubMed]
- Silva, D.C.; Salati, L.R.; Villas-Bôas, A.P.; Schwarz, K.; Fontanari, A.M.; Soll, B.; Costa, A.B.; Hirakata, V.; Schneider, M.; Lobato, M.I.R. Factors Associated with Ruminative Thinking in Individuals with Gender Dysphoria. Front. Psychiatry 2021, 12, 602293. [Google Scholar] [CrossRef]
- Sabino, T.E.; Avelino-Silva, V.I.; Cavalcantte, C.; Goulart, S.P.; Luiz, O.C.; Fonseca, L.A.M.; Casseb, J.S. Adherence to Antiretroviral Treatment and Quality of Life among Transgender Women Living with HIV/AIDS in São Paulo, Brazil. AIDS Care 2021, 33, 31–38. [Google Scholar] [CrossRef]
- Rafael, R.d.M.R.; Jalil, E.M.; Luz, P.M.; de Castro, C.R.V.; Wilson, E.C.; Monteiro, L.; Ramos, M.; Moreira, R.I.; Veloso, V.G.; Grinsztejn, B.G.J.; et al. Prevalence and Factors Associated with Suicidal Behavior among Trans Women in Rio de Janeiro, Brazil. PLoS ONE 2021, 16, e0259074. [Google Scholar] [CrossRef]
- Bassichetto, K.C.; Saggese, G.S.R.; Maschião, L.F.; de Carvalho, P.G.C.; Gilmore, H.; Sevelius, J.; Lippman, S.A.; Veras, M.A.d.S.M. Factors Associated with the Retention of Travestis and Transgender Women Living with HIV in a Peer Navigation Intervention in São Paulo, Brazil. Cad. Saude Publica 2023, 39, e00147522. [Google Scholar] [CrossRef]
- Magalhães, L.S.; Dos Santos, K.C.; Diniz E Silva, B.V.; Filho, G.F.S.; Vaddiparti, K.; Gonzalez, R.I.C.; Pillon, S.C.; Carneiro, M.A.D.S.; Caetano, K.A.A.; Cook, R.L.; et al. Alarming Patterns of Moderate and High-Risk Alcohol Use among Transgender Women in Goiás, Central Brazil. Front. Public Health 2024, 12, 1333767. [Google Scholar] [CrossRef]
- da Mota, J.C.; Sperandei, S.; De Boni, R.B.; Dourado, I.; Veras, M.A.d.S.M.; Bastos, F.I. Multiple Substance Use and Associated Factors in Transgender Women and Travestis: Findings from the TransOdara Study, Brazil. Rev. Bras. Epidemiol. Braz. J. Epidemiol. 2024, 27 (Suppl. S1), e240011.supl.1. [Google Scholar] [CrossRef]
- Luz, P.M.; Jalil, E.M.; Castilho, J.; Velasque, L.; Ramos, M.; Ferreira, A.C.G.; Ferreira, A.L.; Wilson, E.C.; Veloso, V.G.; Thombs, B.D.; et al. Association of Discrimination, Violence, and Resilience with Depressive Symptoms Among Transgender Women in Rio de Janeiro, Brazil: A Cross-Sectional Analysis. Transgender Health 2022, 7, 101–106. [Google Scholar] [CrossRef]
- Veras, M.A.d.S.M.; Pinheiro, T.F.; Galan, L.; Magno, L.; Leal, A.F.; Knauth, D.R.; Motta-Castro, A.R.C.; de Queiroz, R.S.B.; Mayaud, P.; McCartney, D.J.; et al. TransOdara Study: The Challenge of Integrating Methods, Settings and Procedures during the COVID-19 Pandemic in Brazil. Rev. Bras. Epidemiol. Braz. J. Epidemiol. 2024, 27 (Suppl. S1), e240002.supl.1. [Google Scholar] [CrossRef]
- Ryngelblum, M.; Grangeiro, A.; Zucchi, E.M.; Couto, M.T.; Dourado, I.; Magno, L.; Tupinambás, U.; Peres, M.F.T. Violence, Discrimination, and Sexual Health Practices among Adolescent Men Who Have Sex with Men, Transgender Women and Travestis in Three Cities in Brazil. Cad. Saúde Pública 2023, 39, e00142922. [Google Scholar] [CrossRef] [PubMed]
- Koreitem, A.; Mocello, A.R.; Gomez, J.L.; Saggese, G.; Neilands, T.; de Sousa Mascena Veras, M.A.; Lippman, S.A.; Sevelius, J. Intersectional Discrimination, Mental Health, and Health Care Access among Transgender Women in Brazil. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2025, 44, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Leite, B.O.; de Medeiros, D.S.; Magno, L.; Bastos, F.I.; Coutinho, C.; de Brito, A.M.; Cavalcante, M.S.; Dourado, I. Association between Gender-Based Discrimination and Medical Visits and HIV Testing in a Large Sample of Transgender Women in Northeast Brazil. Int. J. Equity Health 2021, 20, 199. [Google Scholar] [CrossRef]
- Magno, L.; Leite, B.O.; Sperandei, S.; Pereira, M.; Knauth, D.R.; Leal, A.F.; Veras, M.A.d.S.M.; Dourado, I. Discrimination Based on Gender Identity against Transgender Women and Travestis in Brazil: A Latent Class Analysis and Associated Factors. Rev. Bras. Epidemiol. 2024, 27, e240012.supl.1. [Google Scholar] [CrossRef]
- Depret, D.; Rafael, R.d.M.R.; Acioli, S.; Neto, M.; Velasque, L.d.S.; Knupp, V.M.A.d.O. Relationship between Childhood Abuse and Self-Harm among Transvestites and Transgender Women in Rio de Janeiro State 2019–2020. Epidemiol. Serv. Saude Rev. Sist. Unico Saude Bras. 2025, 33, e2024337. [Google Scholar] [CrossRef]
- de Sousa Mascena Veras, M.A.; Menezes, N.P.; Mocello, A.R.; Leddy, A.M.; Saggese, G.S.R.; Bassichetto, K.C.; Gilmore, H.J.; de Carvalho, P.G.C.; Maschião, L.F.; Neilands, T.B.; et al. Correlation between Gender-Based Violence and Poor Treatment Outcomes among Transgender Women Living with HIV in Brazil. BMC Public Health 2024, 24, 791. [Google Scholar] [CrossRef]
- Costa, M.C.B.; McFarland, W.; Wilson, E.C.; Xie, H.; Arayasirikul, S.; Moura, F.D.; Veras, M.A.S.M. Prevalence and Correlates of Nonprescription Hormone Use Among Trans Women in São Paulo, Brazil. LGBT Health 2021, 8, 162–166. [Google Scholar] [CrossRef]
- Rosário, R.; Dourado, I.; Pereira, M.; Dezanet, L.; Greco, D.; Grangeiro, A.; Magno, L. Factors associated with condomless anal sex among adolescent men who have sex with men and transgender women in three Brazilian state capitals: A PrEP1519 study. Rev. Saude Publica 2024, 58, 8s. [Google Scholar] [CrossRef]
- Leite, B.O.; Magno, L.; Soares, F.; MacCarthy, S.; Brignol, S.; Bastos, F.I.; Dourado, I. HIV Prevalence among Transgender Women in Northeast Brazil—Findings from Two Respondent Driven Sampling Studies. BMC Public Health 2022, 22, 2120. [Google Scholar] [CrossRef]
- Amelia de Sousa Mascena Veras, M.; Roza Saggese, G.S.; Gomez Junior, J.L.; Silveira, P.; Paiatto, B.; Ferreira, D.; Alves de Souza, P.; Calado, R.; Castejon, M.J.; Yamashiro, R.; et al. Brief Report: Young Age and Sex Work Are Associated with HIV Seroconversion Among Transgender Women in São Paulo, Brazil. J. Acquir. Immune Defic. Syndr. 1999 2021, 88, e1–e4. [Google Scholar] [CrossRef] [PubMed]
- Grinsztejn, B.; Jalil, E.M.; Monteiro, L.; Velasque, L.; Moreira, R.I.; Garcia, A.C.F.; Castro, C.V.; Krüger, A.; Luz, P.M.; Liu, A.Y.; et al. Unveiling HIV Dynamics among Transgender Women: A Respondent Driven Sampling Study in Rio de Janeiro, Brazil. Lancet HIV 2017, 4, e169–e176. [Google Scholar] [CrossRef] [PubMed]
- Barros, C.R.D.S.; Matsuda, E.M.; Rocha, A.B.M.d.; López-Lopes, G.I.S.; Campos, N.C.; Brígido, L.F.d.M.; Bassichetto, K.C.; Veras, M.A.d.S.M. Factors Associated with HIV Viremia in Transgender Women and Transvestites in Five Brazilian Capitals, 2019-2021: A Multicenter Study. Epidemiol. Serv. Saude Rev. Sist. Unico Saude Bras. 2024, 33, e2024412. [Google Scholar] [CrossRef]
- Amarante, I.C.J.; Lippman, S.A.; Sevelius, J.M.; Saggese, G.S.R.; da Silva, A.A.M.; Veras, M.A.d.S.M. Anticipated Stigma and Social Barriers to Communication Between Transgender Women Newly Diagnosed with HIV and Health Care Providers: A Mediation Analysis. LGBT Health 2023, 11, 229–238. [Google Scholar] [CrossRef]
- Jalil, E.M.; Torres, T.S.; Luz, P.M.; Monteiro, L.; Moreira, R.I.; de Castro, C.R.V.; Leite, I.d.C.; Cunha, M.; de Cássia Elias Estrela, R.; Ramos, M.; et al. Low PrEP Adherence despite High Retention among Transgender Women in Brazil: The PrEParadas Study. J. Int. AIDS Soc. 2022, 25, e25896. [Google Scholar] [CrossRef]
- Wilson, E.C.; Jalil, E.M.; Moreira, R.I.; Velasque, L.; Castro, C.V.; Monteiro, L.; Veloso, V.G.; Grinsztejn, B. High Risk and Low HIV Prevention Behaviours in a New Generation of Young Trans Women in Brazil. AIDS Care 2021, 33, 997–1001. [Google Scholar] [CrossRef]
- Echeverría-Guevara, A.; Coelho, L.E.; Veloso, V.G.; Pimenta, M.C.; Hoagland, B.; Moreira, R.I.; Leite, I.; Jalil, E.M.; Cardoso, S.W.; Torres, T.S.; et al. Travestis, Transgender Women and Young MSM Are at High Risk for PrEP Early Loss to Follow-up in Rio de Janeiro, Brazil. Braz. J. Infect. Dis. Off. Publ. Braz. Soc. Infect. Dis. 2023, 27, 102733. [Google Scholar] [CrossRef]
- Hintz, A.M.; Gomes-Filho, I.S.; Loomer, P.M.; de Sousa Pinho, P.; de Santana Passos-Soares, J.; Trindade, S.C.; Cerqueira, E.d.M.M.; Alves, C.M.C.; Rios, Y.S.S.; Batista, J.E.T.; et al. Depression and Associated Factors among Brazilian Adults: The 2019 National Healthcare Population-Based Study. BMC Psychiatry 2023, 23, 704. [Google Scholar] [CrossRef]
- WHO. Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- da Silva Junior, A.L.S.; Santana, G.M.; Nascimento, M.M.; Cunha, R.L.; Mesquita, P.R.R.; de Jesus, R.M. Illicit Drugs in Brazil: Environmental Consequences and Consumption Patterns. Environ. Sci. Pollut. Res. Int. 2024, 31, 47530–47551. [Google Scholar] [CrossRef]
- Malta, D.C.; Flor, L.S.; Machado, Í.E.; Felisbino-Mendes, M.S.; Brant, L.C.C.; Ribeiro, A.L.P.; Teixeira, R.A.; Macário, E.M.; Reitsma, M.B.; Glenn, S.; et al. Trends in Prevalence and Mortality Burden Attributable to Smoking, Brazil and Federated Units, 1990 and 2017. Popul. Health Metr. 2020, 18, 24. [Google Scholar] [CrossRef]
- da Silva, L.E.S.; Helman, B.; da Luz e Silva, D.C.; de Aquino, É.C.; de Freitas, P.C.; Santos, R.d.O.; Brito, V.C.d.A.; Garcia, L.P.; Sardinha, L.M.V. Prevalence of Heavy Episodic Drinking in the Brazilian Adult Population: National Health Survey 2013 and 2019. Epidemiol. Serviços Saúde Rev. Sist. Unico Saúde Bras. 2022, 31, e2021379. [Google Scholar] [CrossRef]
- Jungerman, F.S.; Menezes, P.R.; Pinsky, I.; Zaleski, M.; Caetano, R.; Laranjeira, R. Prevalence of Cannabis Use in Brazil: Data from the I Brazilian National Alcohol Survey (BNAS). Addict. Behav. 2010, 35, 190–193. [Google Scholar] [CrossRef] [PubMed]
- Abdalla, R.R.; Madruga, C.S.; Ribeiro, M.; Pinsky, I.; Caetano, R.; Laranjeira, R. Prevalence of Cocaine Use in Brazil: Data from the II Brazilian National Alcohol and Drugs Survey (BNADS). Addict. Behav. 2014, 39, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, T.F.; Carvalho, P.G.C.d.; Nolasco, G.; Santos, L.A.D.; Veras, M.A.d.S.M. Difficulties and Advances in Access to and Use of Health Services by Transgender Women and Travestis in Brazil. Rev. Bras. Epidemiol. Braz. J. Epidemiol. 2024, 27 (Suppl. S1), e240007.supl.1. [Google Scholar] [CrossRef] [PubMed]
- Vermeir, E.; Jackson, L.A.; Marshall, E.G. Improving Healthcare Providers’ Interactions with Trans Patients: Recommendations to Promote Cultural Competence. Healthc. Policy 2018, 14, 11–18. [Google Scholar] [CrossRef]
- Yu, H.; Flores, D.D.; Bonett, S.; Bauermeister, J.A. LGBTQ + Cultural Competency Training for Health Professionals: A Systematic Review. BMC Med. Educ. 2023, 23, 558. [Google Scholar] [CrossRef]
- Coelho, D.R.A.; Chen, A.L.; Keuroghlian, A.S. Advancing Transgender Health amid Rising Policy Threats. N. Engl. J. Med. 2025, 392, 1041–1044. [Google Scholar] [CrossRef]
- Coleman, E.; Radix, A.E.; Bouman, W.P.; Brown, G.R.; de Vries, A.L.C.; Deutsch, M.B.; Ettner, R.; Fraser, L.; Goodman, M.; Green, J.; et al. Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. Int. J. Transgender Health 2022, 23, S1–S259. [Google Scholar] [CrossRef]
- Almazan, A.N.; Keuroghlian, A.S. Association Between Gender-Affirming Surgeries and Mental Health Outcomes. JAMA Surg. 2021, 156, 611–618. [Google Scholar] [CrossRef]
- Simpson, K.; Benevides, B. 20 Years of Trans Visibility, from Mourning to Fighting! Epidemiol. Serv. Saude Rev. Sist. Unico Saude Bras. 2024, 33, e2024034. [Google Scholar] [CrossRef]
- Ferreira, L.C. Brazilian Medical Entities Criticize Veto on Trans Youth Therapies. Brasil de Fato. 28 April 2025. Available online: https://www.brasildefato.com.br/2025/04/28/brazilian-medical-entities-criticize-veto-on-trans-youth-therapies/ (accessed on 8 June 2025).
- Fleury, F.M. Estado, direito, transfobia e cissexismo no Brasil. Rev. Videre 2021, 13. [Google Scholar] [CrossRef]
- Borges Romeiro Caetano, B.; Dias Oliveira, D.; Schaffer Ramos, T.; Serra Bavaresco, C.; Luiz Stefanello Busato, A.; Itzel Acosta Moreno Vinholes, J.; Renato Reis de Moura, F. LGBTQIA+ vs. the Brazilian Unified Health System: Basic Health Unit Use and Associated Factors. J. Homosex. 2024, 71, 3362–3380. [Google Scholar] [CrossRef] [PubMed]
- Malta, M.; da Silva, A.B.; da Silva, C.M.F.; LeGrand, S.; Seixas, M.; Benevides, B.; Kalume, C.; Whetten, K. Addressing discrimination and violence against Lesbian, Gay, Bisexual, Transgender, and Queer (LGBTQ) persons from Brazil: A mobile health intervention. BMC Public Health 2023, 23, 2069. [Google Scholar] [CrossRef] [PubMed]
- Benfeitoria. PreparaNem—CasaNem. Benfeitoria, Rio de Janeiro, Brazil. Available online: https://benfeitoria.com/projeto/PreparaNem (accessed on 19 April 2025).
- Cruz, E.P. Unicamp Aprova Cotas Para Pessoas Trans, Travestis ou Não Binárias [Unicamp Approves Quotas for Trans, Travesti, or Nonbinary People]. Agência Brasil. 2 April 2025. Available online: https://agenciabrasil.ebc.com.br/educacao/noticia/2025-04/unicamp-aprova-cotas-para-pessoas-trans-travestis-ou-nao-binarias (accessed on 19 April 2025).
- TransEmpregos. TransEmpregos Platform. TransEmpregos, São Paulo, Brazil. Available online: https://www.transempregos.com.br (accessed on 19 April 2025).
- Grangeiro, A.; Ferraz, D.; Magno, L.; Zucchi, E.M.; Couto, M.T.; Dourado, I. Forty Years of the Brazilian Response to HIV: Reflections on the Need for a Programmatic Shift and Policy as a Common Good. Cad. Saúde Pública 2023, 39, e00199423. [Google Scholar] [CrossRef]
- Stutterheim, S.E.; van Dijk, M.; Wang, H.; Jonas, K.J. The Worldwide Burden of HIV in Transgender Individuals: An Updated Systematic Review and Meta-Analysis. PLoS ONE 2021, 16, e0260063. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).