Satisfaction with Health Facility Personnel Among Older People with Disabilities in Chile: An Observational Study Based on the 2024 DISCA Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
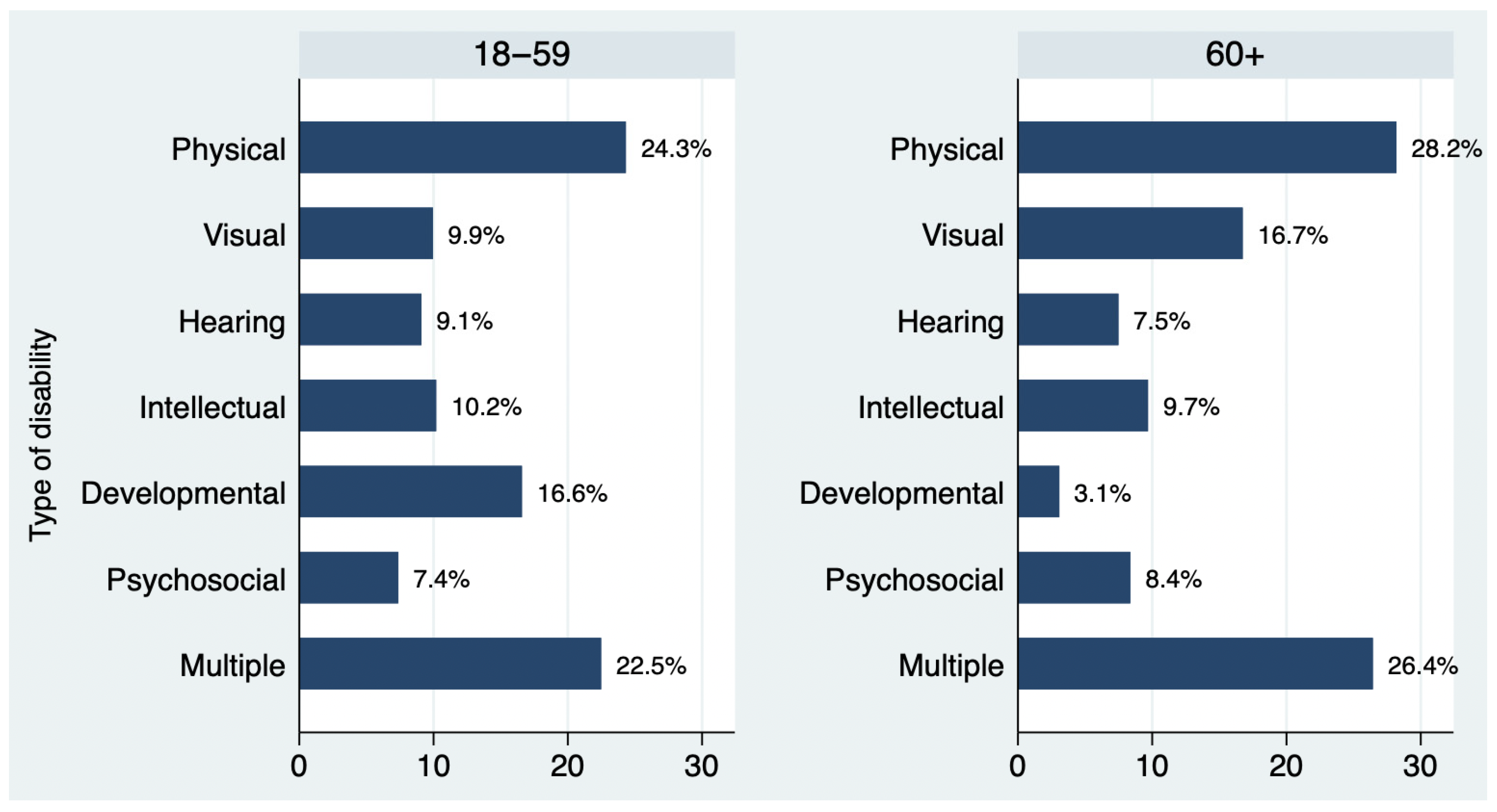
2.2. Variables
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIC | Akaike information criterion |
| BIC | Bayesian information criterion |
| DISCA | Disability and citizenship |
| FONASA | National health fund |
| ISAPRE | Health insurance institutions |
| CRPD | Convention on the Rights of Persons with Disabilities |
| WHO | World Health Organization |
References
- World Health Organization. Global Report on Health Equity for Persons with Disabilities; World Health Organization: Geneva, Switzerland, 2022.
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015.
- Da Silva, J.B., Jr.; Rowe, J.W.; Jauregui, J.R. Healthy aging in the Americas. Rev. Panam. Salud Publica 2021, 45, e116. [Google Scholar] [CrossRef] [PubMed]
- Economic Commission for Latin America and the Caribbean (ECLAC). Ageing in Latin America and the Caribbean: Inclusion and Rights of Older Persons; ECLAC: Santiago, Chile, 2022.
- Ferreira, D.C.; Vieira, I.; Pedro, M.I.; Caldas, P.; Varela, M. Patient satisfaction with healthcare services and the techniques used for its assessment: A systematic literature review and a bibliometric analysis. Healthcare 2023, 11, 639. [Google Scholar] [CrossRef] [PubMed]
- Friedel, A.L.; Siegel, S.; Kirstein, C.F.; Gerigk, M.; Bingel, U.; Diehl, A.; Steidle, O.; Haupeltshofer, S.; Andermahr, B.; Chmielewski, W.; et al. Measuring patient experience and patient satisfaction—How are we doing it and why does it matter? A comparison of European and U.S. American approaches. Healthcare 2023, 11, 797. [Google Scholar] [CrossRef]
- Batbaatar, E.; Dorjdagva, J.; Luvsannyam, A.; Savino, M.M.; Amenta, P. Determinants of patient satisfaction: A systematic review. Perspect. Public Health 2017, 137, 89–101. [Google Scholar] [CrossRef]
- Iezzoni, L.I.; Davis, R.B.; Soukup, J.; O’Day, B. Quality dimensions that most concern people with physical and sensory disabilities. Arch. Intern. Med. 2003, 163, 2085–2092. [Google Scholar] [CrossRef]
- Bright, T.; Kuper, H. A systematic review of access to general healthcare services for people with disabilities in low and middle income countries. Int. J. Environ. Res. Public Health 2018, 15, 1879. [Google Scholar] [CrossRef]
- Rotarou, E.S.; Sakellariou, D. Neoliberal reforms in health systems and the construction of long-lasting inequalities in health care: A case study from Chile. Health Policy 2017, 121, 495–503. [Google Scholar] [CrossRef]
- Krahn, G.L.; Walker, D.K.; Correa-De-Araujo, R. Persons with disabilities as an unrecognized health disparity population. Am. J. Public Health 2015, 105, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Kuper, H.; Rotenberg, S.; Azizatunnisa’, L.; Banks, L.M.; Smythe, T. The association between disability and mortality: A mixed-methods study. Lancet Public Health 2024, 9, e306–e315. [Google Scholar] [CrossRef]
- Meade, M.A.; Mahmoudi, E.; Lee, S.Y. The intersection of disability and healthcare disparities: A conceptual framework. Disabil. Rehabil. 2015, 37, 632–641. [Google Scholar] [CrossRef]
- Floud, S.; Barnes, I.; Verfürden, M.; Kuper, H.; Gathani, T.; Blanks, R.G.; Alison, R.; Patnick, J.; Beral, V.; Green, J.; et al. Disability and participation in breast and bowel cancer screening in England: A large prospective study. Br. J. Cancer 2017, 117, 1711–1714. [Google Scholar] [CrossRef]
- Sakellariou, D.; Rotarou, E.S. The effects of neoliberal policies on access to healthcare for people with disabilities. Int. J. Equity Health 2017, 16, 199. [Google Scholar] [CrossRef] [PubMed]
- Llewellyn, G.; Balandin, S.; Poulos, A.; McCarthy, L. Disability and mammography screening: Intangible barriers to participation. Disabil. Rehabil. 2011, 33, 1755–1767. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.Y.; Clark, M.A. Breast and cervical cancer screening practices among disabled women aged 40–75: Does quality of the experience matter? J. Womens Health 2008, 17, 1321–1329. [Google Scholar] [CrossRef]
- Marusic, M. Fonasa incorporó más de 600 mil nuevos afiliados en 2023: Más de la mitad provino desde las Isapres. In La Tercera; HighBridge: Minneapolis, MN, USA, 2024. [Google Scholar]
- Rodríguez Gatta, D.; Gutiérrez Monclus, P.; Wilbur, J.; Hanefeld, J.; Banks, L.M.; Kuper, H. Inclusion of people with disabilities in Chilean health policy: A policy analysis. Int. J. Equity Health 2024, 23, 174. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Interior. Public Service Satisfaction Survey: Fonasa Results; Ministry of Interior: Santiago, Chile, 2022.
- Rodríguez Gatta, D.; Rotarou, E.S.; Banks, L.M.; Kuper, H. Healthcare access among people with and without disabilities: A cross-sectional analysis of the National Socioeconomic Survey of Chile. Public Health 2025, 241, 144–150. [Google Scholar] [CrossRef]
- Jara-Rosales, S.; Rotarou, E.S. Cervical cancer screening uptake among women with disabilities: Findings from a cross-sectional study in Chile. Int. J. Environ. Res. Public Health 2024, 21, 1578. [Google Scholar] [CrossRef]
- Rotarou, E.S.; Sakellariou, D. Inequalities in access to health care for people with disabilities in Chile: The limits of universal health coverage. Crit. Public Health 2017, 27, 604–616. [Google Scholar] [CrossRef]
- Rotarou, E.S.; Sakellariou, D. Determinants of utilisation rates of preventive health services: Evidence from Chile. BMC Public Health 2018, 18, 839. [Google Scholar] [CrossRef]
- Rodríguez Gatta, D.; Piriz Tapia, C.; Tagle Schmidt, E.; Luna Benavides, J.; Vivar Jara, D.; Moreno Celis, R.; Tobar Carrizo, G.; Vilaró Cáceres, J.; Heydt, P.; Banks, L.M.; et al. Inclusive health for people with disabilities in Chile: A national health system assessment. Health Res. Policy Syst. 2025, 23, 22. [Google Scholar] [CrossRef]
- Elliott, M.N.; Beckett, M.K.; Cohea, C.; Lehrman, W.G.; Russ, C.; Cleary, P.D.; Giordano, L.A.; Goldstein, E.; Saliba, D. The hospital care experiences of older patients compared to younger patients. J. Am. Geriatr. Soc. 2022, 70, 3570–3577. [Google Scholar] [CrossRef]
- Katz, E.; Edelstein, B.; Turiano, N.A. Age as a moderator of health outcomes and trust in physicians. J. Aging Health 2024, 36, 308–319. [Google Scholar] [CrossRef]
- Bjertnaes, O.A.; Sjetne, I.S.; Iversen, H.H. Overall patient satisfaction with hospitals: Effects of patient-reported experiences and fulfilment of expectations. BMJ Qual. Saf. 2012, 21, 39–46. [Google Scholar] [CrossRef]
- Ministry of Health. National Health Strategy for the Health Objectives Until 2030; Ministry of Health: Santiago, Chile, 2022.
- General Secretary of the Presidency. Law 19828: Creation of National Service of the Elderly; Library of the National Congress of Chile: Santiago, Chile, 2002.
- Agency for Healthcare Research and Quality. What Is Patient Experience? Agency for Healthcare Research and Quality: Rockville, MD, USA, 2025.
- United Nations. Convention on the Rights of Persons with Disabilities (CRPD) 2007. Available online: https://www.un.org/disabilities/documents/convention/convoptprot-e.pdf (accessed on 18 February 2025).
- Allison, P. Listwise Deletion: It’s not Evil; Statistical Horizons: Ardmore, PA, USA, 2014. [Google Scholar]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Br. Med. J. 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- Danielsen, K.; Garratt, A.M.; Bjertnaes, Ø.A.; Pettersen, K.I. Patient experiences in relation to respondent and health service delivery characteristics: A survey of 26,938 patients attending 62 hospitals throughout Norway. Scand. J. Public Health 2007, 35, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Rahmqvist, M.; Bara, A.C. Patient characteristics and quality dimensions related to patient satisfaction. Int. J. Qual. Health Care 2010, 22, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Young, G.J.; Meterko, M.; Desai, K.R. Patient satisfaction with hospital care: Effects of demographic and institutional characteristics. Med. Care 2000, 38, 325–334. [Google Scholar] [CrossRef]
- Harp, B.; de Riese, C.; de Riese, W.T.W. Association of age and patient satisfaction scores: A systematic review. Urol. Pract. 2024, 11, 906–914. [Google Scholar] [CrossRef]
- Peck, B.M. Age-related differences in doctor—Patient interaction and patient satisfaction. Curr. Gerontol. Geriatr. Res. 2011, 2011, 137492. [Google Scholar] [CrossRef]
- Ministry of Health; Ministry of Social Development and Family. Mental Health Strategy for the Elderly; Ministry of Health: Santiago, Chile; Ministry of Social Development and Family: Santiago, Chile, 2020.
- Jaipaul, C.K.; Rosenthal, G.E. Are older patients more satisfied with hospital care than younger patients? J. Gen. Intern. Med. 2003, 18, 23–30. [Google Scholar] [CrossRef]
- Lima, G.S.; Figueira, A.L.G.; Carvalho, E.C.; Kusumota, L.; Caldeira, S. Resilience in older people: A concept analysis. Healthcare 2023, 11, 2491. [Google Scholar] [CrossRef] [PubMed]
- Besoain-Saldaña, A.; Rebolledo Sanhueza, J.; Manríquez Hizaut, M.; Cortínez Rojas, V.; Huepe Ortega, G.; Aliaga-Castillo, V. Rehabilitación Basada en la Comunidad (RBC) en centros de atención primaria en Chile. Rev. Saude Publica 2020, 54, 38. [Google Scholar] [CrossRef] [PubMed]
- Iezzoni, L.I.; Rao, S.R.; Ressalam, J.; Bolcic-Jankovic, D.; Agaronnik, N.D.; Donelan, K.; Lagu, T.; Campbell, E.G. Physicians’ perceptions of people with disability and their health care. Health Aff. 2021, 40, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Rotenberg, S.; Rodríguez-Gatta, D.; Wahedi, A.; Loo, R.; McFadden, E.; Ryan, S. Disability training for health workers: A global evidence synthesis. Disabil. Health J. 2022, 15, 101260. [Google Scholar] [CrossRef]
- Kuper, H.; Azizatunnisa’, L.; Rodríguez Gatta, R.; Rotenberg, S.; Banks, L.M.; Smythe, T.; Heydt, P. Building disability-inclusive health systems. Lancet Public Health 2024, 9, e316–e325. [Google Scholar] [CrossRef]
- Ministry of Social Development. Convención Interamericana Sobre La Protección De Los Derechos Humanos De Las Personas Mayores; Ministry of Social Development: Santiago, Chile, 2017.
- United Nations. Convention on the Rights of Persons with Disabilities; United Nations: New York, NY, USA, 2006.
- Lum, J.; Morean, W.; Maccarrone, A.; Carpenter, T.P.; Aaberg, V.; Bentley, J.A. Implicit associations related to physical disability among nursing students. Disabil. Health J. 2021, 14, 101150. [Google Scholar] [CrossRef]
- World Health Organization. Policy Brief on Disability-Inclusive Health Systems; World Health Organization: Copenhagen, Denmark, 2021.
- Ankam, N.S.; Bosques, G.; Sauter, C.; Stiens, S.; Therattil, M.; Williams, F.H.; Atkins, C.C.; Mayer, R.S. Competency-based curriculum development to meet the needs of people with disabilities: A call to action. Acad. Med. 2019, 94, 781–788. [Google Scholar] [CrossRef]
- Bowen, C.N.; Havercamp, S.M.; Karpiak Bowen, S.; Nye, G. A call to action: Preparing a disability-competent health care workforce. Disabil. Health J. 2020, 13, 100941. [Google Scholar] [CrossRef]
- World Health Organization. Policy on the Health Workforce 2030: Strengthening Human Resources for Health to Achieve Resilient Health Systems; World Health Organization: Washington, DC, USA, 2023.
- Pizarro-Mena, R.; Rotarou, E.S.; Chavarro-Carvajal, D.; Wachholz, P.A.; López, M.F.; Perdomo Delgado, C.; Parra-Soto, S.; Barrientos-Calvo, I.; Retamal-Walter, F.; Riveros-Basoalto, G. Comprehensive Gerontological Assessment: An update on the concept and its evaluation tools in Latin America and the Caribbean—A literature review. Int. J. Environ. Res. Public Health 2024, 21, 1697. [Google Scholar] [CrossRef]

| Variable | People with Disabilities Aged 18–59 (n = 832, 77.5%) | People with Disabilities Aged 60+ (n = 242, 22.5%) | p |
|---|---|---|---|
| Socioeconomic variables | |||
| Gender | |||
| Men | 303 (36.4%) | 121 (50.0%) | p < 0.001 |
| Women | 529 (63.6%) | 121 (50.0%) | |
| Age (median, IQR) | 36 (28–45) | 68 (64–73) | |
| Zone | |||
| Urban | 685 (82.4%) | 202 (83.5%) | p = 0.707 |
| Rural | 146 (17.6%) | 40 (16.5%) | |
| Education | |||
| Primary | 60 (7.2%) | 53 (21.9%) | p < 0.001 |
| Secondary | 222 (26.7%) | 106 (43.8%) | |
| Tertiary | 496 (59.6%) | 81 (33.5%) | |
| Special | 54 (6.5%) | 2 (0.8%) | |
| Indigeneity | |||
| Not indigenous | 694 (89.1%) | 216 (93.9%) | p = 0.031 |
| Indigenous | 85 (10.9%) | 14 (6.1%) | |
| Health-related variables | |||
| Health self-assessment | |||
| Bad | 124 (14.9%) | 92 (38.0%) | p < 0.001 |
| Neither good nor bad | 335 (40.3%) | 97 (40.1%) | |
| Good | 373 (44.8%) | 53 (21.9%) | |
| Chronic disease | |||
| No | 305 (40.0%) | 22 (9.2%) | p < 0.001 |
| Yes | 458 (60.0%) | 218 (90.8%) | |
| Health insurance | |||
| Public (FONASA) | 676 (84.5%) | 222 (94.9%) | p < 0.001 |
| Private (ISAPRE) | 124 (15.5%) | 12 (5.1%) | |
| Satisfaction with health facility personnel | |||
| With doctors | |||
| Low | 36 (5.3%) | 2 (0.9%) | p < 0.001 |
| Average | 101 (14.8%) | 12 (5.3%) | |
| High | 546 (79.9%) | 214 (93.9%) | |
| With other health professionals | |||
| Low | 23 (4.1%) | 2 (1.3%) | p = 0.001 |
| Average | 71 (12.7%) | 6 (3.8%) | |
| High | 467 (83.2%) | 149 (94.9%) | |
| With paramedical technicians | |||
| Low | 30 (6.3%) | 2 (1.2%) | p < 0.001 |
| Average | 96 (20.3%) | 9 (5.6%) | |
| High | 347 (73.4%) | 151 (93.2%) | |
| With administrative personnel | |||
| Low | 58 (9.8%) | 3 (1.8%) | p < 0.001 |
| Average | 156 (26.4%) | 21 (12.4%) | |
| High | 376 (63.7%) | 145 (85.8%) | |
| With security guards and cleaning personnel | |||
| Low | 16 (3.1%) | 1 (1.0%) | p = 0.038 |
| Average | 95 (18.5%) | 10 (9.7%) | |
| High | 404 (78.5%) | 92 (89.3%) | |
| Dependent Variable | OR | 95% CI | Observations | LR chi2 (p) |
|---|---|---|---|---|
| Satisfaction with doctors | ||||
| Simple regression | 3.864 | 2.181–6.845 | 911 | 28.76 (p < 0.001) |
| Multiple regression | 3.831 | 1.950–7.524 | 790 | 78.27 (p < 0.001) |
| Satisfaction with other health professionals | ||||
| Simple regression | 3.741 | 1.777–7.880 | 718 | 16.49 (p < 0.001) |
| Multiple regression | 4.655 | 1.878–11.541 | 612 | 55.36 (p < 0.001) |
| Satisfaction with paramedical technicians | ||||
| Simple regression | 4.992 | 2.619–9.512 | 635 | 33.71 (p < 0.001) |
| Multiple regression | 4.305 | 2.074–8.936 | 549 | 69.98 (p < 0.001) |
| Satisfaction with administrative personnel | ||||
| Simple regression | 3.504 | 2.208–5.561 | 759 | 34.66 (p < 0.001) |
| Multiple regression | 3.126 | 1.824–5.357 | 651 | 90.06 (p < 0.001) |
| Satisfaction with security guards and cleaning personnel | ||||
| Simple regression | 2.309 | 1.195–4.463 | 618 | 7.33 (p = 0.007) |
| Multiple regression | 1.776 | 0.839–3.758 | 516 | 24.79 (p = 0.010) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rotarou, E.S.; Sakellariou, D.; Pizarro-Mena, R. Satisfaction with Health Facility Personnel Among Older People with Disabilities in Chile: An Observational Study Based on the 2024 DISCA Survey. Int. J. Environ. Res. Public Health 2025, 22, 1103. https://doi.org/10.3390/ijerph22071103
Rotarou ES, Sakellariou D, Pizarro-Mena R. Satisfaction with Health Facility Personnel Among Older People with Disabilities in Chile: An Observational Study Based on the 2024 DISCA Survey. International Journal of Environmental Research and Public Health. 2025; 22(7):1103. https://doi.org/10.3390/ijerph22071103
Chicago/Turabian StyleRotarou, Elena S., Dikaios Sakellariou, and Rafael Pizarro-Mena. 2025. "Satisfaction with Health Facility Personnel Among Older People with Disabilities in Chile: An Observational Study Based on the 2024 DISCA Survey" International Journal of Environmental Research and Public Health 22, no. 7: 1103. https://doi.org/10.3390/ijerph22071103
APA StyleRotarou, E. S., Sakellariou, D., & Pizarro-Mena, R. (2025). Satisfaction with Health Facility Personnel Among Older People with Disabilities in Chile: An Observational Study Based on the 2024 DISCA Survey. International Journal of Environmental Research and Public Health, 22(7), 1103. https://doi.org/10.3390/ijerph22071103








