A Longitudinal Ecologic Analysis of Neighborhood-Level Social Inequalities in Health in Texas
Abstract
1. Introduction
1.1. Neighborhood Poverty and Health
1.2. Neighborhood Racial/Ethnic Composition and Health
1.3. History of Social Inequality in Texas: A Snapshot
1.4. Study Purpose
2. Materials and Methods
2.1. Data
2.2. Measures
2.3. Analytical Plan
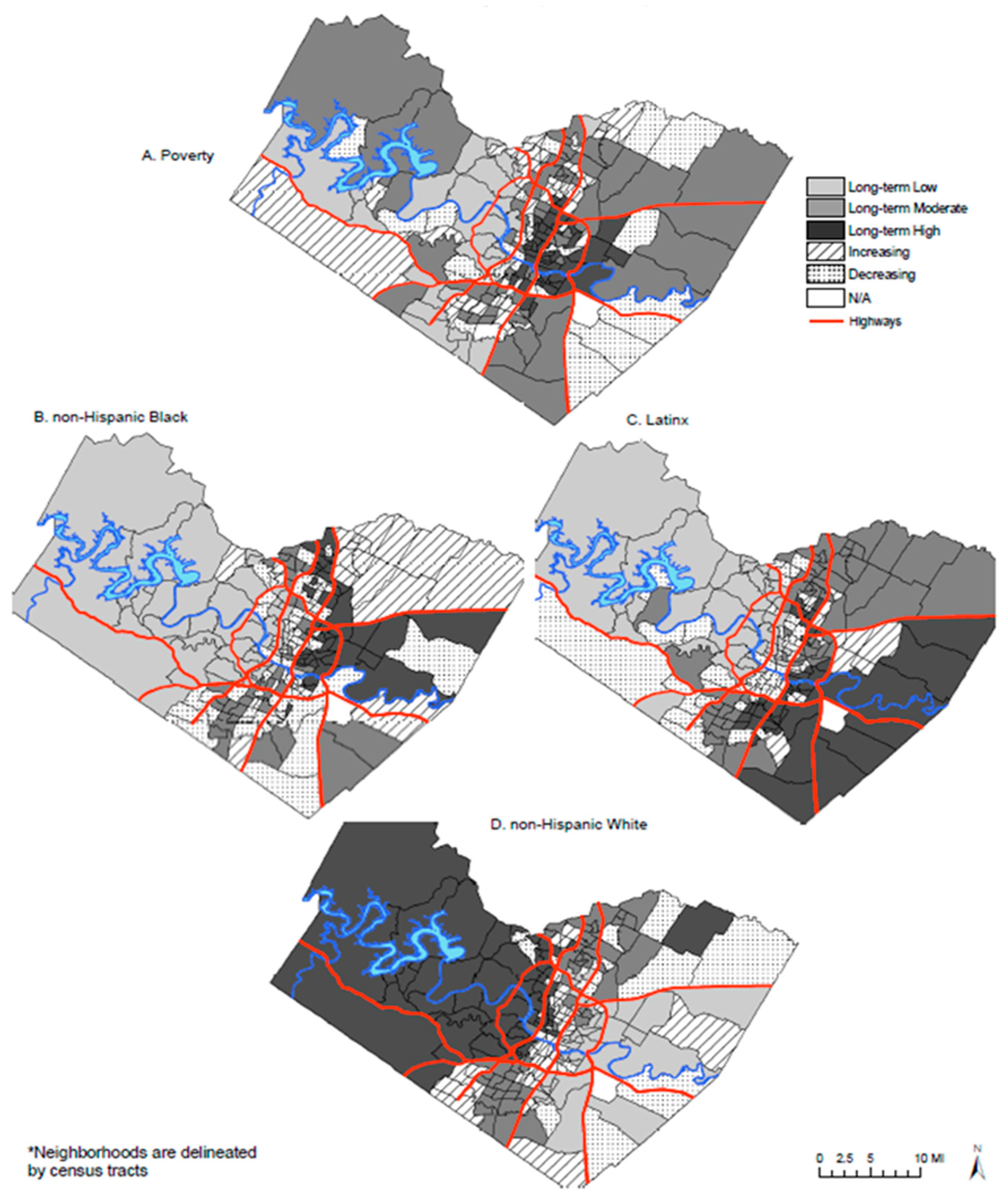
3. Results
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cubbin, C.; Hadden, W.C.; Winkleby, M.A. Neighborhood Context and Cardiovascular Disease Risk Factors: The Contribution of Material Deprivation. Ethn. Dis. 2001, 11, 687–700. Available online: https://www.jstor.org/stable/45410317 (accessed on 4 July 2025).
- De la Roca, J.; Ellen, I.G.; O’Regan, K.M. Race and Neighborhoods in the 21st Century: What Does Segregation Mean Today? Reg. Sci. Urban Econ. 2014, 47, 138–151. [Google Scholar] [CrossRef]
- Reardon, S.F.; Fox, L.; Townsend, J. Neighborhood Income Composition by Household Race and Income, 1990–2009. Ann. Am. Acad. Political Soc. Sci. 2015, 660, 78–97. [Google Scholar] [CrossRef]
- Overview of Race and Hispanic Origin. 2010. Available online: https://www.census.gov/content/dam/Census/library/publications/2011/dec/c2010br-02.pdf (accessed on 29 May 2025).
- Margerison-Zilko, C.; Cubbin, C.; Jun, J.; Marchi, K.; Fingar, K.; Braveman, P. Beyond the Cross-Sectional: Neighborhood Poverty Histories and Preterm Birth. Am. J. Public Health 2015, 105, 1174–1180. [Google Scholar] [CrossRef] [PubMed]
- Macintyre, S.; Ellaway, A.; Cummins, S. Place Effects on Health: How Can We Conceptualise, Operationalise and Measure Them? Soc. Sci. Med. 2002, 55, 125–139. [Google Scholar] [CrossRef] [PubMed]
- Diez Roux, A.V. The Study of Group-Level Factors in Epidemiology: Rethinking Variables, Study Designs, and Analytical Approaches. Epidemiol. Rev. 2004, 26, 104–111. [Google Scholar] [CrossRef]
- Yang, T.-C.; South, S.J. Neighborhood Poverty and Physical Health at Midlife: The Role of Life-Course Exposure. J. Urban Health 2020, 97, 486–501. [Google Scholar] [CrossRef]
- Lippert, A.M.; Evans, C.R.; Razak, F.; Subramanian, S.V. Associations of Continuity and Change in Early Neighborhood Poverty With Adult Cardiometabolic Biomarkers in the United States: Results From the National Longitudinal Study of Adolescent to Adult Health, 1995–2008. Am. J. Epidemiol. 2017, 185, 765–776. [Google Scholar] [CrossRef]
- Huang, Y.; Sparks, P.J. Longitudinal Exposure to Neighborhood Poverty and Obesity Risk in Emerging Adulthood. Soc. Sci. Res. 2023, 111, 102796. [Google Scholar] [CrossRef]
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.J.; Taylor, S.; Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- Morrissey, T.W.; Oellerich, D.; Meade, E.; Simms, J.; Stock, A. Neighborhood Poverty and Children’s Food Insecurity. Child. Youth Serv. Rev. 2016, 66, 85–93. [Google Scholar] [CrossRef]
- Chamberlain, A.W.; Hipp, J.R. It’s All Relative: Concentrated Disadvantage within and across Neighborhoods and Communities, and the Consequences for Neighborhood Crime. J. Crim. Justice 2015, 43, 431–443. [Google Scholar] [CrossRef]
- Haley, D.F.; Linton, S.; Luo, R.; Hunter-Jones, J.; Adimora, A.A.; Wingood, G.M.; Bonney, L.; Ross, Z.; Cooper, H.L.F. Public Housing Relocations and Relationships of Changes in Neighborhood Disadvantage and Transportation Access to Unmet Need for Medical Care. J. Health Care Poor Underserved 2017, 28, 315–328. [Google Scholar] [CrossRef]
- Moore, L.V.; Diez Roux, A.V. Associations of Neighborhood Characteristics With the Location and Type of Food Stores. Am. J. Public Health 2006, 96, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.V.; Diez Roux, A.V.; Nettleton, J.A.; Jacobs, D.R., Jr. Associations of the Local Food Environment with Diet Quality—A Comparison of Assessments Based on Surveys and Geographic Information Systems: The Multi-Ethnic Study of Atherosclerosis. Am. J. Epidemiol. 2008, 167, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Morland, K.; Wing, S.; Diez Roux, A.; Poole, C. Neighborhood Characteristics Associated with the Location of Food Stores and Food Service Places. Am. J. Prev. Med. 2002, 22, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Pearce, J.; Blakely, T.; Witten, K.; Bartie, P. Neighborhood Deprivation and Access to Fast-Food Retailing: A National Study. Am. J. Prev. Med. 2007, 32, 375–382. [Google Scholar] [CrossRef]
- Larson, N.I.; Story, M.T.; Nelson, M.C. Neighborhood Environments: Disparities in Access to Healthy Foods in the U.S. Am. J. Prev. Med. 2009, 36, 74–81.e10. [Google Scholar] [CrossRef]
- Richardson, A.S.; Meyer, K.A.; Howard, A.G.; Boone-Heinonen, J.; Popkin, B.M.; Evenson, K.R.; Kiefe, C.I.; Lewis, C.E.; Gordon-Larsen, P. Neighborhood Socioeconomic Status and Food Environment: A 20-Year Longitudinal Latent Class Analysis among CARDIA Participants. Health Place 2014, 30, 145–153. [Google Scholar] [CrossRef]
- Massey, D.S. American Apartheid: Segregation and the Making of the Underclass. Am. J. Sociol. 1990, 96, 329–357. [Google Scholar] [CrossRef]
- Sharifi, V.; Dimitropoulos, G.; Williams, J.V.A.; Rao, S.; Pedram, P.; Bulloch, A.G.M.; Patten, S.B. Neighborhood Material versus Social Deprivation in Canada: Different Patterns of Associations with Child and Adolescent Mental Health Problems. Soc. Psychiatry Psychiatr. Epidemiol. 2025, 60, 823–836. [Google Scholar] [CrossRef] [PubMed]
- Pereira, N.; Zhu, X. Neighborhood Socioeconomic Contexts Mediate the Association between Adverse Childhood Experiences and Social Risk and Health Outcomes in Adulthood. SSM Popul. Health 2025, 30, 101802. [Google Scholar] [CrossRef]
- Liu, M.; Patel, V.R.; Salas, R.N.; Rice, M.B.; Kazi, D.S.; Zheng, Z.; Wadhera, R.K. Neighborhood Environmental Burden and Cardiovascular Health in the US. JAMA Cardiol. 2024, 9, 153–163. [Google Scholar] [CrossRef]
- Diez Roux, A.-V. Neighborhoods and Health: Where Are We and Were Do We Go from Here? Rev. D’épidémiologie Santé Publique 2007, 55, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Diez Roux, A.V.; Mair, C. Neighborhoods and Health. Ann. N. Y. Acad. Sci. 2010, 1186, 125–145. [Google Scholar] [CrossRef]
- Côté-Lussier, C.; Barnett, T.A.; Kestens, Y.; Tu, M.T.; Séguin, L. The Role of the Residential Neighborhood in Linking Youths’ Family Poverty Trajectory to Decreased Feelings of Safety at School. J. Youth Adolesc. 2015, 44, 1194–1207. [Google Scholar] [CrossRef]
- Kivimäki, M.; Batty, G.D.; Pentti, J.; Nyberg, S.T.; Lindbohm, J.V.; Ervasti, J.; Gonzales-Inca, C.; Suominen, S.B.; Stenholm, S.; Sipilä, P.N.; et al. Modifications to residential neighbourhood characteristics and risk of 79 common health conditions: A prospective cohort study. Lancet Public Health 2021, 6, e396–e407. [Google Scholar] [CrossRef]
- Cubbin, C.; Kim, Y.; Vohra-Gupta, S.; Margerison, C. Longitudinal Measures of Neighborhood Poverty and Income Inequality Are Associated with Adverse Birth Outcomes in Texas. Soc. Sci. Med. 2020, 245, 112665. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, C.; Powers, D.; Margerison-Zilko, C.; McDevitt, T.; Cubbin, C. Historical Neighborhood Poverty Trajectories and Child Sleep. Sleep Health 2018, 4, 127–134. [Google Scholar] [CrossRef]
- Acolin, A.; Crowder, K.; Decter-Frain, A.; Hajat, A.; Hall, M.; Homandberg, L.; Hurvitz, P.M.; Woyczynski, L. Gentrification Yields Racial And Ethnic Disparities In Exposure To Contextual Determinants Of Health. Health Aff. 2024, 43, 172–180. [Google Scholar] [CrossRef]
- Xiao, Q.; Myott, E.; Schlundt, D.G.; Stancil, W. Association of Neighborhood Economic Trajectories With Changes in Weight Status Among Black and White Adults in the Southeastern US. JAMA Netw. Open 2022, 5, e2230697. [Google Scholar] [CrossRef] [PubMed]
- Chrisinger, B.W.; Springfield, S.; Whitsel, E.A.; Shadyab, A.H.; Krok-Schoen, J.L.; Garcia, L.; Sealy-Jefferson, S.; Stefanick, M.L. The Association of Neighborhood Changes with Health-Related Quality of Life in the Women’s Health Initiative. Int. J. Environ. Res. Public Health 2022, 19, 5309. [Google Scholar] [CrossRef]
- Booth, J.M.; Teixeira, S.; Zuberi, A.; Wallace, J.M. Barrios, Ghettos, and Residential Racial Composition: Examining the Racial Makeup of Neighborhood Profiles and Their Relationship to Self-Rated Health. Soc. Sci. Res. 2018, 69, 19–33. [Google Scholar] [CrossRef]
- Osypuk, T.L.; Schmidt, N.M.; Kehm, R.D.; Tchetgen Tchetgen, E.J.; Glymour, M.M. The Price of Admission: Does Moving to a Low-Poverty Neighborhood Increase Discriminatory Experiences and Influence Mental Health? Soc. Psychiatry Psychiatr. Epidemiol. 2019, 54, 181–190. [Google Scholar] [CrossRef]
- English, D.; Lambert, S.F.; Evans, M.K.; Zonderman, A.B. Neighborhood Racial Composition, Racial Discrimination, and Depressive Symptoms in African Americans. Am. J. Community Psychol. 2014, 54, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Vohra-Gupta, S.; Margerison, C.E.; Cubbin, C. Neighborhood Racial/Ethnic Composition Trajectories and Black-White Differences in Preterm Birth among Women in Texas. J Urban Health 2020, 97, 37–51. [Google Scholar] [CrossRef]
- The Changing Face of Texas: Population Projections and Implications. Available online: https://ideas.repec.org/b/fip/feddmo/2005tcfoppa.html (accessed on 20 May 2025).
- Fastest Growing Group in Texas: Asian Americans. Available online: https://www.texastribune.org/2024/06/26/texas-asian-american-growth-census/ (accessed on 23 June 2025).
- Martin, J.A.; Hamilton, B.E.; Ventura, S.J.; Osterman, M.J.; Wilson, E.C.; Mathews, T.J. Births: Final data for 2010. In National Vital Statistics Reports; National Center for Health Statistics: Hyattsville, MD, USA, 2012; Volume 61. [Google Scholar]
- Braveman, P.A.; Cubbin, C.; Egerter, S.; Chideya, S.; Marchi, K.S.; Metzler, M.; Posner, S. Socioeconomic Status in Health Research: One Size Does Not Fit All. JAMA 2005, 294, 2879–2888. [Google Scholar] [CrossRef] [PubMed]
- Gaskin, D.J.; Thorpe, R.J.; McGinty, E.E.; Bower, K.; Rohde, C.; Young, J.H.; LaVeist, T.A.; Dubay, L. Disparities in Diabetes: The Nexus of Race, Poverty, and Place. Am. J. Public Health 2014, 104, 2147–2155. [Google Scholar] [CrossRef]
- Montgomery, L.E.; Kiely, J.L.; Pappas, G. The Effects of Poverty, Race, and Family Structure on US Children’s Health: Data from the NHIS, 1978 through 1980 and 1989 through 1991. Am. J. Public Health 1996, 86, 1401–1405. [Google Scholar] [CrossRef]
- Greenlund, K.J.; Lu, H.; Wang, Y.; Matthews, K.A.; LeClercq, J.M.; Lee, B.; Carlson, S.A. PLACES: Local Data for Better Health. Prev. Chronic Dis. 2022, 19, E31. [Google Scholar] [CrossRef]
- Tatian, P.A. Neighborhood Change Database (NCDB) 1970–2000 Tract Data: Data User’s Guide Long Form Release; The Urban Institute: Washington, DC, USA, 2003; Available online: https://geolytics.com/media/pdf/NCDB-final-LF-version.pdf (accessed on 4 July 2025).
- Cantrell, J.; Anesetti-Rothermel, A.; Pearson, J.L.; Xiao, H.; Vallone, D.; Kirchner, T.R. The Impact of the Tobacco Retail Outlet Environment on Adult Cessation and Differences by Neighborhood Poverty. Addiction 2015, 110, 152–161. [Google Scholar] [CrossRef]
- Li, Q.; Douglas, J.A.; Subica, A.M. Examining Neighbourhood-Level Disparities in Black, Latina/o, Asian, and White Physical Health, Mental Health, Chronic Conditions, and Social Disadvantage in California. Glob. Public Health 2023, 18, 2273425. [Google Scholar] [CrossRef]
- Sheehan, C.M.; Cantu, P.A.; Powers, D.A.; Margerison-Zilko, C.E.; Cubbin, C. Long-Term Neighborhood Poverty Trajectories and Obesity in a Sample of California Mothers. Health Place 2017, 46, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N.; Waterman, P.D.; Subramanian, S.V. Monitoring Socioeconomic Inequalities in Sexually Transmitted Infections, Tuberculosis, and Violence: Geocoding and Choice of Area-Based Socioeconomic Measures—The Public Health Disparities Geocoding Project (US). Public Health Rep. 2003, 118, 240–260. [Google Scholar] [CrossRef]
- Kim, Y.; Cubbin, C.; Oh, S. A systematic review of neighbourhood economic context on child obesity and obesity-related behaviours. Obes. Rev. 2019, 3, 420–431. [Google Scholar] [CrossRef] [PubMed]
- Do, D.P.; Dubowitz, T.; Bird, C.E.; Lurie, N.; Escarce, J.J.; Finch, B.K. Neighborhood Context and Ethnicity Differences in Body Mass Index: A Multilevel Analysis Using the NHANES III Survey (1988–1994). Econ. Hum. Biol. 2007, 5, 179–203. [Google Scholar] [CrossRef]
- Fuller-Rowell, T.E.; Curtis, D.S.; Klebanov, P.K.; Brooks-Gunn, J.; Evans, G.W. Racial Disparities in Blood Pressure Trajectories of Preterm Children: The Role of Family and Neighborhood Socioeconomic Status. Am. J. Epidemiol. 2017, 185, 888–897. [Google Scholar] [CrossRef] [PubMed]
- Mujahid, S.M.; Diez-Roux, A.V.; Cooper, R.; Shea, S.; Ni, H. Neighborhood Walkability and Access to Healthy Foods are Related to Hypertension in a Multiethnic Sample. Am. J. Epidemiol. 2006, 163 (Suppl. S11), S253. [Google Scholar] [CrossRef]
- Merkin, S.S.; Diez Roux, A.V.; Coresh, J.; Fried, L.F.; Jackson, S.A.; Powe, N.R. Individual and Neighborhood Socioeconomic Status and Progressive Chronic Kidney Disease in an Elderly Population: The Cardiovascular Health Study. Soc. Sci. Med. 2007, 65, 809–821. [Google Scholar] [CrossRef]
- Cantu, P.; Kim, Y.; Sheehan, C.; Powers, D.; Margerison, C.E.; Cubbin, C. Downward Neighborhood Poverty Mobility during Childhood Is Associated with Child Asthma: Evidence from the Geographic Research on Wellbeing (GROW) Survey. J. Urban Health 2019, 96, 558–569. [Google Scholar] [CrossRef]
- Jivraj, S.; Murray, E.T.; Norman, P.; Nicholas, O. The impact of life course exposures to neighbourhood deprivation on health and well-being: A review of the long-term neighbourhood effects literature. Eur. J. Public Health 2020, 30, 922–928. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mair, C.; Roux, A.V.D.; Galea, S. Are Neighbourhood Characteristics Associated with Depressive Symptoms? A Review of Evidence. J. Epidemiol. Community Health 2008, 62, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.S.; Breakstone, H.; Dean, L.T.; Thorpe, R.J., Jr. Impacts of Gentrification on Health in the US: A Systematic Review of the Literature. J. Urban Health 2020, 97, 845–856. [Google Scholar] [CrossRef] [PubMed]
- Vohra-Gupta, S.; Wood, B.M.; Kim, Y.; La Frinere-Sandoval, Q.N.; Widen, E.M.; Cubbin, C. Neighborhood Diversity Is Good for Your Health: An Example of Racial/Ethnic Integration and Preterm Birth in Texas. J. Racial Ethn. Health Disparities 2024. [CrossRef] [PubMed]
- Maps Show Visible Racial Divides in Major Texas Cities. Available online: https://www.houstonchronicle.com/news/houston-texas/article/Highways-interstates-reinforce-divides-in-Texas-6399606.php (accessed on 28 May 2025).
- Mehra, R.; Boyd, L.M.; Ickovics, J.R. Racial Residential Segregation and Adverse Birth Outcomes: A Systematic Review and Meta-Analysis. Soc. Sci. Med. 2017, 191, 237–250. [Google Scholar] [CrossRef]
- Kershaw, K.N.; Osypuk, T.L.; Do, D.P.; De Chavez, P.J.; Diez Roux, A.V. Neighborhood-Level Racial/Ethnic Residential Segregation and Incident Cardiovascular Disease. Circulation 2015, 131, 141–148. [Google Scholar] [CrossRef]
- Reardon, S.F.; Bischoff, K. Income Inequality and Income Segregation. Am. J. Sociol. 2011, 116, 1092–1153. [Google Scholar] [CrossRef]
- Williams, D.R.; Collins, C. Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Rep. 2001, 116, 404–416. [Google Scholar] [CrossRef]
- Schulz, A.J.; Zenk, S.N.; Israel, B.A.; Mentz, G.; Stokes, C.; Galea, S. Do Neighborhood Economic Characteristics, Racial Composition, and Residential Stability Predict Perceptions of Stress Associated with the Physical and Social Environment? Findings from a Multilevel Analysis in Detroit. J. Urban Health 2008, 85, 642–661. [Google Scholar] [CrossRef]
- Krueger, P.M.; Reither, E.N. Mind the Gap: Race/Ethnic and Socioeconomic Disparities in Obesity. Curr. Diabetes Rep. 2015, 15, 95. [Google Scholar] [CrossRef]
- Zenk, S.N.; Schulz, A.J.; Israel, B.A.; James, S.A.; Bao, S.; Wilson, M.L. Neighborhood Racial Composition, Neighborhood Poverty, and the Spatial Accessibility of Supermarkets in Metropolitan Detroit. Am. J. Public Health 2005, 95, 660–667. [Google Scholar] [CrossRef]
- Bower, K.M.; Thorpe, R.J.; Rohde, C.; Gaskin, D.J. The Intersection of Neighborhood Racial Segregation, Poverty, and Urbanicity and Its Impact on Food Store Availability in the United States. Prev. Med. 2014, 58, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Gordon-Larsen, P.; Nelson, M.C.; Page, P.; Popkin, B.M. Inequality in the Built Environment Underlies Key Health Disparities in Physical Activity and Obesity. Pediatrics 2006, 117, 417–424. [Google Scholar] [CrossRef] [PubMed]
| Median (Range) or % of Total | |
|---|---|
| Social Determinants of Health | |
| Distance to the nearest emergency department (miles) | 4.6 (0.1–51.6) |
| Distance to the nearest obstetrics department (miles) | 3.2 (0.0–45.6) |
| Median home value ($) | 113,500 (9999–1,000,001) |
| Rented occupied housing units (%) | 32.5 (0.0–100) |
| Crowded housing (%) | 3.6 (0.0–39.8) |
| Gini index of income inequality | 0.4 (0.0–0.7) |
| Less than high school (%) | 17.8 (0.0–100) |
| Bachelor’s degree (%) | 13.8 (0.0–61.4) |
| Public assistance income or food stamps/SNAP (%) | 8.5 (0.0–64.8) |
| Unemployed (%) | 6.5 (0.0–59.7) |
| Limited English proficiency (%) | 5.8 (0.0–100) |
| Single-parent households (%) | 29.4 (0.0–100.0) |
| Health Risk and Preventive Behaviors | |
| Insufficient sleep (%) | 34.8 (21.7–49.0) |
| Current smoking (%) | 16.6 (4.5–40.6) |
| No physical activity (%) | 30.4 (13.6–52.2) |
| Hypertension (%) | 29.7 (7.7–62.9) |
| Dental Visit (%) | 57.0 (23.9–85.5) |
| Routine checkup (%) | 66.5 (50.8–86.9) |
| Uninsured (%) | 25.5 (5.8–64.1) |
| Health Status/Outcomes | |
| Cancer (%) | 4.8 (0.7–20.9) |
| Chronic obstructive pulmonary disease (%) | 5.5 (1.3–18.2) |
| Coronary heart disease (%) | 5.4 (0.4–20.9) |
| Diabetes (%) | 10.6 (1.2–29.4) |
| Obesity (%) | 33.1 (15.8–52.3) |
| Poor mental health status (%) | 11.7 (4.8–21.8) |
| Poor physical health status (%) | 12.1 (4.0–30.2) |
| Poverty trajectories (%) | |
| Long-term low | 11.4 |
| Long-term moderate | 30.1 |
| Long-term high | 24.2 |
| Increasing | 20.7 |
| Decreasing | 13.7 |
| White trajectories (%) | |
| Long-term low | 32.0 |
| Long-term moderate | 20.2 |
| Long-term high | 19.0 |
| Increasing | 12.8 |
| Decreasing | 16.1 |
| Long-Term Moderate a | Long-Term High a | Increasing a | Decreasing a | Population Density (Quartile 1) b | Population Density (Quartile 2) b | Population Density (Quartile 3) b | R2 | F (p Value) | |
|---|---|---|---|---|---|---|---|---|---|
| beta (se) | beta (se) | beta (se) | beta (se) | beta (se) | beta (se) | beta (se) | |||
| Social Determinants of Health | |||||||||
| Distance to the nearest emergency department c | 0.423 (0.053) * | 0.317 (0.054) * | 0.282 (0.056) * | 0.351 (0.061) * | 1.069 (0.045) * | 0.463 (0.044) * | 0.132 (0.044) | 0.218 | 118.70 (<0.0001) |
| Distance to the nearest obstetrics department c | −0.002 (0.049) | −0.144 (0.051) | −0.006 (0.052) | 0.005 (0.058) | 1.054 (0.042) * | 0.209 (0.041) * | 0.030 (0.041) | 0.234 | 129.82 (<0.0001) |
| Median home value c | −0.489 (0.038) * | −1.010 (0.038) * | −0.555 (0.039) * | −0.524 (0.043) * | −0.190 (0.025) * | −0.066 (0.024) | −0.007 (0.024) | 0.313 | 150.99 (<0.0001) |
| Rented occupied housing units | 15.197 (1.791) * | 27.306 (1.798) * | 20.309 (1.840) * | 12.679 (2.013) * | −24.102 (1.176) * | −11.294 (1.140) * | −8.969 (1.122) * | 0.269 | 122.53 (<0.0001) |
| Crowded housing c | 1.039 (0.082) * | 1.852 (0.082) * | 1.229 (0.084) * | 0.992 (0.092) * | −0.462 (0.054) * | −0.353 (0.052) * | −0.333 (0.051) * | 0.254 | 113.30 (<0.0001) |
| Gini index of income inequality | 0.032 (0.006) * | 0.077 (0.006) * | 0.041 (0.006) * | 0.032 (0.006) * | 0.012 (0.004) * | −0.003 (0.004) | −0.003 (0.003) | 0.124 | 47.50 (<0.0001) |
| Less than high school | 12.390 (1.149) * | 33.433 (1.153) * | 15.462 (1.180) * | 15.045 (1.291) * | −5.220 (0.754) * | −4.599 (0.731) * | −4.538 (0.720) * | 0.408 | 228.48 (<0.0001) |
| Bachelor’s degree | −15.599 (0.799) * | −24.425 (0.802) * | −15.829 (0.821) * | −14.453 (0.898) * | −2.777 (0.525) * | −0.237 (0.509) | 0.863 (0.501) | 0.331 | 163.80 (<0.0001) |
| Public assistance income or food stamps/SNAP | 1.275 (0.069) * | 2.326 (0.069) * | 1.453 (0.071) * | 1.196 (0.078) * | −0.036 (0.045) | −0.083 (0.044) | −0.131 (0.043) | 0.394 | 215.30 (<0.0001) |
| Unemployed | 2.195 (0.365) * | 5.610 (0.366) * | 3.295 (0.375) * | 2.130 (0.410) * | −1.061 (0.240) * | 0.234 (0.232) | 0.141 (0.229) | 0.162 | 64.72 (<0.0001) |
| Limited English proficiency c | 0.698 (0.086) * | 1.621 (0.086) * | 0.997 (0.088) * | 0.741 (0.096) * | −1.135 (0.056) * | −0.605 (0.055) * | −0.466 (0.054) * | 0.321 | 156.48 (<0.0001) |
| Single-parent households | 14.176 (1.396) * | 26.667 (1.400) * | 17.639 (1.434) * | 10.779 (1.569) * | −8.667 (0.917) * | −1.072 (0.888) | −1.644 (0.875) | 0.224 | 95.96 (<0.0001) |
| Health Risk and Preventive Behaviors | |||||||||
| Insufficient sleep | 0.752 (0.287) | 0.743 (0.296) | 0.617 (0.305) | 0.234 (0.337) | 1.982 (0.247) * | 1.601 (0.240) * | 0.930 (0.241) * | 0.026 | 12.14 (<0.0001) |
| Current smoking | 0.469 (0.311) | 0.378 (0.321) | 0.446 (0.330) | 0.210 (0.366) | 1.584 (0.268) * | 1.173 (0.261) * | 0.409 (0.261) | 0.014 | 6.78 (<0.0001) |
| No physical activity | 2.080 (0.526) * | 1.631 (0.543) | 1.916 (0.559) * | 1.695 (0.618) | 2.934 (0.454) * | 3.141 (0.441) * | 1.798 (0.441) * | 0.024 | 11.28 (<0.0001) |
| Hypertension | 2.039 (0.432) * | 2.062 (0.446) * | 1.941 (0.459) * | 1.101 (0.507) | 2.911 (0.372) * | 2.290 (0.362) * | 1.121 (0.362) | 0.030 | 14.24 (<0.0001) |
| Dental visit | −2.232 (0.863) | −0.878 (0.891) | −2.308 (0.917) | −1.387 (1.013) | −2.967 (0.744) * | −3.409 (0.723) * | −1.710 (0.723) | 0.010 | 5.18 (<0.0001) |
| Routine checkup | 0.500 (0.251) | 0.957 (0.259) * | 0.276 (0.266) | 0.118 (0.295) | 1.013 (0.217) * | 0.253 (0.210) | 0.173 (0.211) | 0.013 | 6.54 (<0.0001) |
| Uninsured | 2.575 (0.841) | 0.974 (0.868) | 2.731 (0.893) | 2.536 (0.988) | 2.460 (0.725) * | 3.659 (0.705) * | 2.276 (0.705) | 0.012 | 6.17 (<0.0001) |
| Health Status/Outcomes | |||||||||
| Cancer | 0.272 (0.103) | 0.354 (0.106) * | 0.245 (0.109) | 0.167 (0.121) | 0.245 (0.089) | 0.084 (0.086) | −0.027 (0.086) | 0.006 | 3.49 (0.001) |
| Chronic obstructive pulmonary disease | 0.551 (0.125) * | 0.429 (0.129) * | 0.477 (0.133) * | 0.325 (0.147) | 0.695 (0.108) * | 0.613 (0.105) * | 0.280 (0.105) | 0.023 | 10.79 (<0.0001) |
| Coronary heart disease | 0.757 (0.131) * | 0.619 (0.135) * | 0.671 (0.139) * | 0.516 (0.153) * | 0.637 (0.113) * | 0.696 (0.109) * | 0.360 (0.110) * | 0.025 | 11.85 (<0.0001) |
| Diabetes | 1.433 (0.280) * | 1.280 (0.290) * | 1.353 (0.298) * | 0.924 (0.329) | 1.234 (0.242) * | 1.515 (0.235) * | 0.868 (0.235) * | 0.021 | 10.24 (<0.0001) |
| Obesity | 1.440 (0.407) * | 1.218 (0.420) | 1.346 (0.43) | 1.227 (0.478) | 2.955 (0.351) * | 2.646 (0.341) * | 1.440 (0.341) * | 0.033 | 15.23 (<0.0001) |
| Poor mental health status | 0.481 (0.191) | 0.169 (0.197) | 0.452 (0.203) | 0.379 (0.224) | 0.657 (0.165) * | 0.732 (0.160) * | 0.446 (0.160) | 0.009 | 5.00 (<0.0001) |
| Poor physical health status | 1.325 (0.282) * | 0.868 (0.291) | 1.202 (0.300) * | 1.015 (0.331) | 1.274 (0.243) * | 1.553 (0.237) * | 0.883 (0.237) * | 0.021 | 10.15 (<0.0001) |
| Long-Term Low a | Long-Term Moderate a | Increasing a | Decreasing a | Population Density (Quartile 1) b | Population Density (Quartile 2) b | Population Density (Quartile 3) b | R2 | F (p Value) | |
|---|---|---|---|---|---|---|---|---|---|
| beta (se) | beta (se) | beta (se) | beta (se) | beta (se) | beta (se) | beta (se) | |||
| Social Determinants of Health | |||||||||
| Distance to the nearest emergency department c | −0.073 (0.062) | −0.110 (0.064) | −0.016 (0.073) | −0.151 (0.071) | 1.035 (0.054) * | 0.473 (0.049) * | 0.138 (0.049) | 0.194 | 80.36 (<0.0001) |
| Distance to the nearest obstetrics department c | −0.053 (0.059) | −0.189 (0.061) | −0.244 (0.070) * | −0.089 (0.067) | 1.090 (0.051) * | 0.217 (0.047) * | 0.044 (0.046) | 0.229 | 98.82 (<0.0001) |
| Median home value c | −0.772 (0.031) * | −0.297 (0.032) * | −0.191 (0.032) * | −0.348 (0.035) * | −0.415 (0.027) * | −0.097 (0.025) * | −0.031 (0.024) | 0.291 | 136.33 (<0.0001) |
| Rented occupied housing units | 10.584 (1.522) * | 7.967 (1.572) * | 10.584 (1.781) * | 7.571 (1.722) * | −23.492 (1.316) * | −12.406 (1.206) * | −9.626 (1.186) * | 0.190 | 78.28 (<0.0001) |
| Crowded housing c | 1.585 (0.064) * | 0.631 (0.066) * | 0.506 (0.075) * | 0.855 (0.072) * | 0.001 (0.055) | −0.281 (0.051) * | −0.276 (0.050) * | 0.298 | 140.62 (<0.0001) |
| Gini index of income inequality | 0.006 (0.005) | −0.006 (0.005) | 0.021 (0.005) * | −0.024 (0.005) * | 0.003 (0.004) | −0.009 (0.004) | −0.005 (0.004) | 0.0455 | 16.42 (<0.0001) |
| Less than high school | 27.690 (0.916) * | 6.355 (0.947) * | 5.722 (1.073) * | 11.855 (1.037) * | 3.076 (0.793) * | −2.989 (0.726) * | −3.286 (0.714) * | 0.422 | 241.19 (<0.0001) |
| Bachelor’s degree | −16.850 (0.644) * | −5.614 (0.665) * | −3.087 (0.754) * | −7.127 (0.729) * | −8.099 (0.557) * | −0.853 (0.510) | 0.301 (0.502) | 0.333 | 165.38 (<.0001) |
| Public assistance income or food stamps/SNAP | 1.644 (0.058) * | 0.582 (0.060) * | 0.473 (0.067) * | 0.676 (0.065) * | 0.406 (0.050) * | −0.035 (0.456) | −0.085 (0.045) | 0.351 | 178.89 (<0.0001) |
| Unemployed | 4.625 (0.295)* | 1.319 (0.305) * | 1.443 (0.346) * | 1.950 (0.334) * | 0.037 (0.255) | 0.415 (0.234) | 0.295 (0.230) | 0.157 | 62.58 (<0.0001) |
| Limited English proficiency c | 1.940 (0.063) * | 0.899 (0.065) * | 0.715 (0.073) * | 1.351 (0.071) * | −0.543 (0.054) * | −0.479 (0.050) * | −0.379 (0.049) * | 0.443 | 263.14 (<0.0001) |
| Single-parent households | 16.492 (1.183) * | 7.433 (1.222) * | 8.513 (1.384) * | 7.175 (1.339) * | −5.677 (1.023) * | −1.143 (0.937) | −1.541 (0.922) | 0.144 | 56.45 (<0.0001) |
| Health Risk and Preventive Behaviors | |||||||||
| Insufficient sleep | 0.564 (0.261) | 0.459 (0.274) | 0.209 (0.307) | 1.242 (0.300) * | 2.263 (0.258) * | 1.626 (0.241) * | 0.951 (0.241) * | 0.029 | 13.40 (<0.0001) |
| Current smoking | 0.093 (0.283) | −0.219 (0.298) | 0.260 (0.333) | 0.821 (0.325) | 1.702 (0.280) * | 1.184 (0.262) * | 0.430 (0.262) | 0.017 | 8.17 (<0.0001) |
| No physical activity | 1.080 (0.479) | 0.798 (0.504) | 1.648 (0.464) | 1.834 (0.550) * | 3.393 (0.474) * | 3.143 (0.444) * | 1.822 (0.444) * | 0.023 | 10.89 (<0.0001) |
| Hypertension | 0.653 (0.394) | 0.209 (0.415) | 0.566 (0.464) | 1.078 (0.453) | 3.108 (0.390) * | 2.179 (0.365) * | 1.056 (0.365) | 0.023 | 10.92 (<0.0001) |
| Dental visit | −0.455 (0.785) | −0.567 (0.826) | −1.412 (0.924) | −2.519 (0.902) | −3.329 (0.777) * | −3.367 (0.727) * | −1.701 (0.727) | 0.010 | 5.20 (<0.0001) |
| Routine checkup | 0.365 (0.229) | 0.190 (0.241) | −0.097 (0.270) | 0.191 (0.263) | 1.106 (0.227) * | 0.225 (0.212) | 0.153 (0.212) | 0.008 | 4.33 (<0.0001) |
| Uninsured | 1.454 (0.765) | 1.705 (0.806) | 2.352 (0.902) | 2.904 (0.880) * | 3.191 (0.758) * | 3.724 (0.709) * | 2.335 (0.709) * | 0.011 | 5.74 (<0.0001) |
| Health Status/Outcomes | |||||||||
| Cancer | 0.092 (0.094) | −0.047 (0.099) | 0.101 (0.110) | −0.062 (0.108) | 0.241 (0.093) | 0.063 (0.087) | −0.038 (0.087) | 0.003 | 2.43 (0.02) |
| Chronic obstructive pulmonary disease | 0.179 (0.114) | 0.069 (0.120) | 0.256 (0.134) | 0.319 (0.131) | 0.770 (0.113) * | 0.599 (0.106) * | 0.275 (0.105) | 0.018 | 8.89 (<0.0001) |
| Coronary heart disease | 0.293 (0.119) | 0.224 (0.126) | 0.428 (0.141) | 0.312 (0.137) | 0.725 (0.118) * | 0.669 (0.111) * | 0.346 (0.111) | 0.017 | 8.17 (<0.0001) |
| Diabetes | 0.597 (0.256) | 0.602 (0.269) | 0.654 (0.031) | 0.973 (0.294) * | 1.463 (0.253) * | 1.473 (0.237) * | 0.843 (0.237) * | 0.016 | 7.69 (<0.0001) |
| Obesity | 0.539 (0.370) | 0.580 (0.390) | 0.884 (0.436) | 1.268 (0.425) | 3.223 (0.366) * | 2.601 (0.343) * | 1.415 (0.343) * | 0.031 | 14.66 (<0.0001) |
| Poor mental health status | 0.236 (0.174) | 0.253 (0.183) | 0.406 (0.205) | 0.618 (0.200) | 0.799 (0.172) * | 0.749 (0.161) * | 0.462 (0.161) | 0.009 | 5.32 (<0.0001) |
| Poor physical health status | 0.577 (0.257) | 0.552 (0.271) | 0.922 (0.303) | 0.909 (0.296) | 1.511 (0.255) * | 1.537 (0.238) * | 0.881 (0.238) * | 0.018 | 8.54 (<0.0001) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cubbin, C.; Yirenya-Tawiah, A.; Kim, Y.; Wood, B.; La Frinere-Sandoval, N.Q.N.B.; Vohra-Gupta, S. A Longitudinal Ecologic Analysis of Neighborhood-Level Social Inequalities in Health in Texas. Int. J. Environ. Res. Public Health 2025, 22, 1076. https://doi.org/10.3390/ijerph22071076
Cubbin C, Yirenya-Tawiah A, Kim Y, Wood B, La Frinere-Sandoval NQNB, Vohra-Gupta S. A Longitudinal Ecologic Analysis of Neighborhood-Level Social Inequalities in Health in Texas. International Journal of Environmental Research and Public Health. 2025; 22(7):1076. https://doi.org/10.3390/ijerph22071076
Chicago/Turabian StyleCubbin, Catherine, Abena Yirenya-Tawiah, Yeonwoo Kim, Bethany Wood, Natasha Quynh Nhu Bui La Frinere-Sandoval, and Shetal Vohra-Gupta. 2025. "A Longitudinal Ecologic Analysis of Neighborhood-Level Social Inequalities in Health in Texas" International Journal of Environmental Research and Public Health 22, no. 7: 1076. https://doi.org/10.3390/ijerph22071076
APA StyleCubbin, C., Yirenya-Tawiah, A., Kim, Y., Wood, B., La Frinere-Sandoval, N. Q. N. B., & Vohra-Gupta, S. (2025). A Longitudinal Ecologic Analysis of Neighborhood-Level Social Inequalities in Health in Texas. International Journal of Environmental Research and Public Health, 22(7), 1076. https://doi.org/10.3390/ijerph22071076






