Evaluating the Cost-Effectiveness of Air Pollution Mitigation Strategies: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Study Selection
2.3. Data Extraction
2.4. Synthesis of the Results
2.5. Quality Assessment
3. Results
3.1. Study Selection
3.2. Study Identification
3.3. Characteristics of Health Economic Evaluations
3.4. Results of Health Economic Evaluations
3.5. Results Quality Assessment
4. Discussion
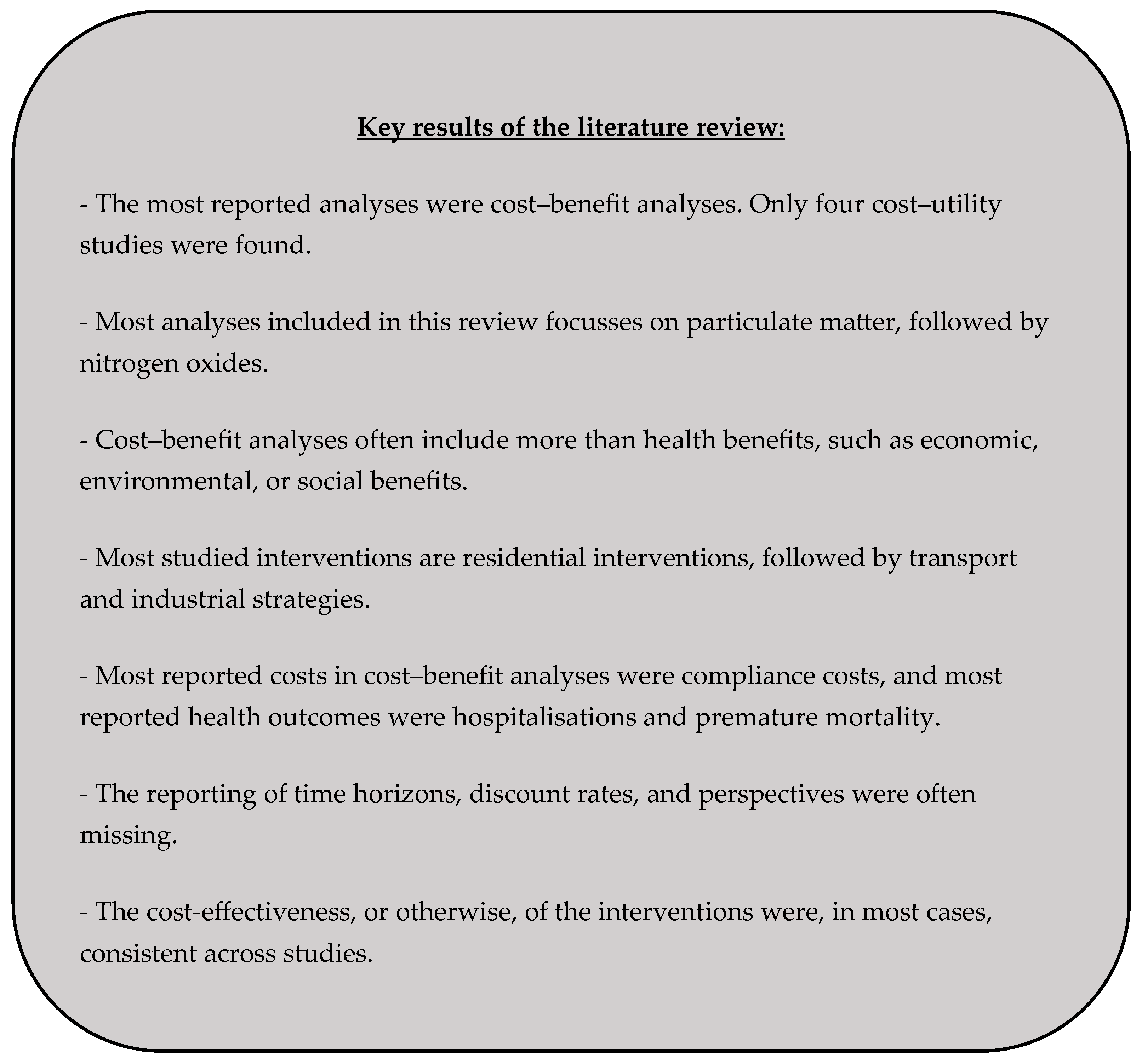
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| CBA | Cost–benefit analysis |
| CBR | Cost–benefit ratio |
| CHEERS | Consolidated Health Economic Evaluation Reporting Standards |
| COI | Cost of illness |
| COPD | Chronic obstructive pulmonary disease |
| CUA | Cost–utility analysis |
| DALY | Disability-adjusted life year |
| IAM | Integrated assessment model |
| ICER | Incremental cost-effectiveness ratio |
| ICS | Improved cooking stoves |
| ICUR | Incremental cost–utility ratio |
| LPG | Liquid petroleum gas |
| MeSH | Medical Subject Heading |
| NB | Net benefits |
| QALY | Quality-adjusted life year |
| UK | United Kingdom |
| USA | United States of America |
| VSL | Value of statistical life |
| WHO | World Health Organization |
| WTP | Willingness to pay |
Appendix A
| Residential | ||
| Author (Publication Year) | Intervention | Comparator |
| Adibi et al. (2023) [70] | Air purification: types of government reimbursement for air purifiers for residents with asthma. | Base case: the provincial government reimburses 100% of the cost of air purifiers for residents with asthma. |
| Aunan et al. (2013) [38] | Heating: replacement of biomass stoves with improved systems (implementation in individual households (1) or in the community (2) in households with (a) a chimney and without (b)). | Situation prior to the intervention. |
| Cansino et al. (2019) [62] | Implementation of solar panels and storage systems. | Business as usual: traditional wood-burning stoves. |
| Feng et al. (2021) [41] | Implementation of gas and electricity for heating. | Basic scenario without clean heating. |
| Fisk et al. (2017) [43] | Different methods to purify air with air purifiers (i1–i6). | Two basic scenarios:
|
| Fisk et al. (2017a) [42] | Different methods to purify air with air purifiers (i1–i6). | Idem Fisk et al. (2017) [43]. |
| Irfan et al. (2021) [45] | Implementation of stoves based on liquefied petroleum gases, gas, biogas, electricity, or improved cooking systems. | Not mentioned. |
| Jeuland et al. (2016) [32] | Improved wood-burning stoves, improved charcoal-burning stoves, implementation of stoves based on liquefied petroleum gases or electric stoves. | Business as usual: traditional wood-burning stoves. |
| Liu Y. et al. (2021) [47] | Different scenarios of air purification: S1: PM2.5 target = 35 µg/m3; S2: PM2.5 target = 25 µg/m3; S3: PM2.5 target = 15 µg/m3; S4: PM2.5 target = 10 µg/m3. | Base case: no air purifier. |
| Mardones et al. (2021) [33] | Implementation of kerosene heating with ventilation (1), pellet stove (2), certified wood-burning stove (4). | Most common method of heating prior to the intervention: wood. |
| Meng et al. (2023) [34] | Heating with electricity (1), gas (2), a combination of these two (3), coal in highly efficient stoves (4), pellet stove with gasifier (5). | Base case: Stated Policy Scenario. |
| Meng et al. (2023b) [49] | Heating with clean energy (not specified). | Base scenario without clean heating. |
| Ramirez et al. (2024) [69] | Two improved (biomass-improved cookstove tier 2 and tier 3) and three clean (LPG, biogas, and electricity induction). | Traditional cooking. |
| Yang et al. (2024) [36] | Air purifiers in different residential spaces: bedroom (1), kitchen (2), both (3), bedroom + living room (4), (4) + (2) (5), classroom (6). | Base scenario: no air purifier. |
| Zhang et al. (2023) [56] | Air purification with different target concentrations: S1–S4 → 5–15–25–35 µg/m3. | Base scenario, not specified. |
| Industrial | ||
| Author (publication year) | Intervention | Comparator |
| Buonocore et al. (2016) [73] | Policy scenario similar to ‘Clean Power Plan’. | Business as usual, reference scenario. |
| Chen et al. (2015) [39] | Different environmental policy scenarios (FS: strict policy measure; FR: less strict policy measure). | Base case: development without implementation of environmental policy scenarios. |
| Cropper et al. (2017) [63] | Implementation of flue gas desulphurisation to reduce SO2. | No desulphurisation. |
| Gao et al. (2016) [44] | Policy scenario of coal savings, ‘end-of-pipe’ treatments, or an integrated scenario. | Base case: no coal savings, no emission reduction (counterfactual scenario). |
| Guo et al. (2023) [64] | Implementation of clean energy transition: early retirement of coal-fired units after 20 years of operation. | Base case: normal retirement of all energy facilities after 30 years. |
| Levy et al. (2017) [46] | Advanced-technology combined heat and power biomass system. | Counterfactual scenario: conventional configuration. |
| Liu K et al. (2024) [67] | (1) Ultralow APCDs (upgrading air pollutant control devices); (2) natural retirement of coal-fired industrial boilers (CFIBs); (3) early retirement of CFIBs; (4) enhanced retirement of CFIBs; (5) biomass replacement; (6) gas replacement. | Baseline scenario (2020). |
| Thompson et al. (2016) [52] | Two subnational carbon policy scenarios: ‘clean energy standard’, in which a fraction of electricity must be generated by clean energy, and ‘cap-and-trade method’ for emissions. | Base case: no carbon constraints. |
| Wan et al. (2023) [54] | Emission reduction strategies: dismantling small units, renovating existing units, promoting clean energy, building new units. | Not mentioned. |
| Wiser et al. (2017) [55] | Standards for renewable portfolio and its expansion. | ‘Renewable Portfolio Standards’ purchase obligations were eliminated after 2014. |
| Zhang et al. (2015) [57] | Multipollutant strategy and gradual pollutant strategy. | No baseline scenario; both interventions are directly compared. |
| Zhang et al. (2019) [58] | Action Plan for Air Pollution Prevention and Control. | Not mentioned. |
| Transport | ||
| Author (publication year) | Intervention | Comparator |
| Ballinger et al. (2016) [76] | Different measures to reduce transport emissions (e.g., low-emission zones, road closures, impact of noise barriers, etc.). | Scenario prior to the intervention. |
| Evans et al. (2021) [40] | Retrofitting heavy-duty commercial vehicles in use: diesel oxidation catalysts; diesel particulate filters. | Base case, not specified. |
| Lomas et al. (2016) [14] | Implementation of low-emission zones. | ‘Do nothing’ scenario. |
| Lopez-Aparicio et al. (2020) [48] | Implementation of speed limits: Scenario 1, speed limit analysed with observed speeds; Scenario 2, speed limits analysed with maximum speeds. | Base case: no speed limit. |
| Whitehurst et al. (2021) [66] | Different scenarios for the expansion of cycling infrastructure: no increase, moderate increase, and significant increase in cyclists. | Base case, reference year. |
| Zhou et al. (2019) [60] | Replacement of labelled vehicles. | Base case: no policy. |
| Zhou et al. (2022) [61] | Limitations for high-emission vehicles. | Base case: the amount of current high-emission-vehicle-restricted areas without the policy. |
| Agricultural | ||
| Author (publication year) | Intervention | Comparator |
| Giannadaki et al. (2018) [74] | (1) Implementation of low-nitrogen feed; (2) low-emission animal housing; (3) fertiliser storage capacity; (4) techniques to reduce fertiliser emissions. | Not mentioned. |
| Giannakis et al. (2019) [30] | (1) Implementation of low-nitrogen feed; (2) manure storage capacity; (3) low-emission animal housing; (4) replacement or improvement of urea fertiliser. | Control simulation, not further specified. |
| Liu M. et al. (2019) [75] | Reduction in NH3 and SO2 emissions (not specified). | Emissieniveaus in 2015. |
| Wagner et al. (2015) [35] | (1) Calcium ammonium nitrate instead of urea fertiliser; (2) reduced tillage; (3) low-protein feed for pigs and poultry; (4) covering techniques for manure storage; (5) techniques for manure spreading; (6) air purification systems for exhaust gases. | Base case: estimated emissions under current conditions. |
| Wagner et al. (2017) [53] | Scenario where emission reduction strategies are implemented on every farm. | Reference scenario: estimated emissions under current reduction measures. |
| Zhang et al. (2020) [37] | Change in diet, optimal nitrogen use, and less agricultural waste through better recycling of animal manure, crop residues, and human waste. | Base case: current policy measures and plans. |
| Intersectoral | ||
| Author (publication year) | Intervention | Comparator |
| Lavee et al. (2018) [65] | Twenty different policy measures in the energy, industry, transport, and household sectors. | Baseline scenario: current policy measures led by IMoEP and other relevant government departments. |
| Miranda et al. (2016) [50] | Reduction in emissions through a combination of the following interventions: (1) HYB, replacement of 10% of vehicles under EURO3 with hybrid cars; (2) LEZ, low emission zone in Porto; (3) FIR, replacement/conversion of 50% of conventional open fireplaces with more efficient equipment; (4) IND, application of environmentally friendly technology that causes a 10% reduction in PM10 emissions in production processes and industrial combustion. | Reference scenario where the emissions reflect the already implemented measures. |
| Schucht et al. (2018) [51] | Different measures in the energy, transport, industrial, and household sectors. | Not mentioned. |
| Zhao et al. (2022) [59] | Introduction of local and national action plans to reduce air pollution. | Current air pollution level. |
| No real intervention | ||
| Author (publication year) | Intervention | Comparator |
| Amann et al. (2017) [77] | Different emission standards | Not reported. |
| Holland et al. (2014) [78] | Maximum Technically Feasible Reduction (MTFR) scenario and a series of intermediate scenarios for 2025 and 2030: These scenarios vary in the ambition levels set for mortality linked to PM2.5 exposure, ozone, and eutrophication. | Scenario with current legislation. |
| Howard et al. (2019) [31] | Three different scenarios:
| Base case, not specified. |
| Kim et al. (2020) [71] | Two scenarios (no real intervention):
|
|
| Liu Z et al. (2023) [68] | Nox-only, Nox-AVOC-A, Nox-AVOC-B | Not specified. |
| Schmitt et al. (2016) [72] | A hypothetical scenario of an immediate reduction of 1 µg/m3 in the average ambient concentration of PM2.5. | No intervention. |
| Srinivasan et al. (2018) [79] | Different emission standards | Not reported. |
Appendix B
| Adibi et al. (2023) [70] | Aunan et al. (2013) [77] | Buonocore et al. (2016) [73] | Cansino et al. (2019) [62] | Chen et al. (2015) [39] | Cropper et al. (2017) [63] | Evans et al. (2021) [40] | Feng et al. (2021) [41] | Fisk et al. (2017) [43] | Fisk et al. (2017a) [42] | Gao et al. (2016) [44] | Giannadaki et al. (2018) [74] | Giannakis et al. (2019) [30] | Guo et al. (2023) [64] | Howard et al. (2019) [31] | Irfan et al. (2021) [45] | Jeuland et al. (2016) [32] | Kim et al. (2021) [71] | Lavee et al. (2018) [65] | Levy et al. (2017) [46] | Liu K et al. (2024) [67] | Liu M. et al. (2019) [75] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Title | ✔ | ✔ | ± | x | ± | ✔ | ± | ± | ✔ | ✔ | ± | x | ✔ | ± | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ± | ± |
| (2) Abstract | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ± | ✔ | ✔ | ± |
| (3) Background and objectives | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (4) Health economic analysis plan | ✔ | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| (5) Study population | ✔ | ✔ | x | x | x | x | ✔ | x | x | x | x | x | ✔ | x | x | x | x | x | x | x | x | x |
| (6) Setting and location | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (7) Comparators | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (8) Perspective | ✔ | x | x | x | x | x | x | ✔ | ✔ | x | ✔ | ✔ | x | x | x | x | ✔ | ✔ | x | x | x | x |
| (9) Time horizon | ✔ | x | x | x | x | ✔ | x | ✔ | x | x | ✔ | x | x | x | x | ✔ | ✔ | ✔ | x | ✔ | ✔ | x |
| (10) Discount rate | ✔ | ✔ | ✔ | x | ✔ | ✔ | ✔ | x | x | x | ✔ | x | x | x | x | ✔ | ✔ | ✔ | x | ✔ | x | x |
| (11) Selection of outcomes | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (12) Measurement of outcomes | ✔ | ✔ | ✔ | ✔ | x | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (13) Valuation of outcomes | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | x | x | ✔ |
| (14) Measurement and valuation of resources and costs | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | x | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (15) Currency, price date, and conversion | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | x | x | x | x | ✔ | x | x | ✔ | ✔ | ✔ | x | ✔ | x | x | ✔ | x |
| (16) Rationale and description of model | ✔ | x | ✔ | x | ✔ | ✔ | x | NA | NA | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | x | x | ✔ | ✔ | ✔ | ✔ | ✔ |
| (17) Analytics and assumptions | ✔ | x | ✔ | x | ✔ | x | ✔ | NA | NA | x | ✔ | ✔ | ✔ | ✔ | ✔ | x | ✔ | ✔ | x | ✔ | ✔ | ✔ |
| (18) Characterising heterogeneity | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| (19) Characterising distributional effects | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| (20) Characterising uncertainty | ✔ | ✔ | x | x | x | ✔ | ✔ | x | x | ✔ | ✔ | ✔ | x | ✔ | ✔ | ✔ | ✔ | ✔ | x | x | x | x |
| (21) Approach to engagement with patients and others affected by the study | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| (22) Study parameters | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (23) Summary of the main results | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (24) Effect of uncertainty | ✔ | ✔ | x | x | x | ✔ | ✔ | x | x | ✔ | ✔ | ✔ | x | ✔ | ✔ | ✔ | ✔ | ✔ | x | x | x | x |
| (25) Effect of engagement with patients and others affected by the study | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| (26) Study findings, limitations, generalizability, and current knowledge | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | x | ✔ | ✔ | ✔ |
| (27) Source of funding | x | ✔ | x | ✔ | x | x | x | ✔ | ✔ | ✔ | ✔ | x | ✔ | x | x | x | x | ✔ | x | ✔ | ✔ | ✔ |
| (28) Conflict of interest | x | x | x | ✔ | x | x | x | ✔ | ✔ | ✔ | x | ✔ | ✔ | ✔ | x | x | x | ✔ | ✔ | x | ✔ | x |
| TOTAL/28 | 22 | 18 | 15.5 | 14 | 14.5 | 18 | 16.5 | 15.5 | 15 | 17 | 20.5 | 16 | 17 | 17.5 | 17 | 17 | 18 | 22 | 12.5 | 16 | 16.5 | 14 |
| Liu Y. et al. (2021) [47] | Liu Z et al. (2023) [68] | Lomas et al. (2016) [14] | Lopez-Aparicio et al. (2020) [48] | Mardones et al. (2021) [33] | Meng et al. (2023) [34] | Meng et al. (2023) [49] | Miranda et al. (2016) [50] | Ramirez et al. (2024) [69] | Schmitt L.H.M. (2016) [72] | Schucht et al. (2018) [51] | Thompson et al. (2016) [52] | Wagner et al. (2015) [35] | Wagner et al. (2017) [53] | Wan et al. (2023) [54] | Whitehurst et al. (2021) [66] | Wiser et al. (2017) [55] | Yang et al. (2024) [36] | Zhang et al. (2015) [57] | Zhang et al. (2019) [58] | Zhang et al. (2021) [37] | Zhang et al. (2023) [56] | Zhao et al. (2022) [59] | Zhou et al. (2019) [60] | Zhou et al. (2022) [61] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Title | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ± | ✔ | ✔ | ✔ | ± | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ± | ✔ | ✔ | ✔ | x | ✔ | ✔ |
| (2) Abstract | ✔ | ± | ✔ | ✔ | ✔ | ± | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ± | ✔ | ± | ✔ | ✔ | ± | ✔ |
| (3) Background and objectives | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (4) Health economic analysis plan | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| (5) Study population | x | x | ✔ | x | ✔ | ✔ | x | x | x | ✔ | x | x | x | x | x | x | x | x | x | x | x | ✔ | x | x | x |
| (6) Setting and location | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (7) Comparators | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (8) Perspective | x | ✔ | ✔ | x | x | x | x | x | ✔ | x | x | x | ✔ | ✔ | x | ✔ | x | x | x | ✔ | x | x | x | ✔ | ✔ |
| (9) Time horizon | x | ✔ | ✔ | x | x | x | x | x | ✔ | ✔ | x | x | x | ✔ | x | ✔ | ✔ | x | ✔ | ✔ | ✔ | x | ✔ | ✔ | ✔ |
| (10) Discount rate | x | x | ✔ | x | ✔ | ✔ | ✔ | x | ✔ | ✔ | x | x | x | ✔ | x | ✔ | ✔ | x | ✔ | x | ✔ | x | x | ✔ | ✔ |
| (11) Selection of outcomes | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | x | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (12) Measurement of outcomes | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (13) Valuation of outcomes | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | x | ✔ | ✔ | x | x | ✔ | x | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (14) Measurement and valuation of resources and costs | ✔ | ✔ | x | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | x | ✔ | ± | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | x | ✔ | ✔ |
| (15) Currency, price date, and conversion | x | ✔ | x | ✔ | x | ✔ | ✔ | ✔ | ✔ | ✔ | x | ✔ | x | ✔ | ✔ | ✔ | x | x | x | ✔ | ✔ | x | x | ✔ | ✔ |
| (16) Rationale and description of model | ✔ | ✔ | x | ✔ | NA | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | x | ✔ | ✔ | NA | ✔ | ✔ |
| (17) Analytics and assumptions | ✔ | ✔ | x | x | NA | ✔ | x | ✔ | ✔ | ✔ | x | x | ✔ | x | ✔ | ✔ | ✔ | ✔ | x | x | ✔ | x | NA | ✔ | ✔ |
| (18) Characterising heterogeneity | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| (19) Characterising distributional effects | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| (20) Characterising uncertainty | ✔ | x | x | ✔ | ✔ | ✔ | ✔ | x | x | ✔ | x | ✔ | x | ✔ | x | ✔ | ✔ | ✔ | ✔ | x | x | ✔ | x | x | x |
| (21) Approach to engagement with patients and others affected by the study | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| (22) Study parameters | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (23) Summary of the main results | ✔ | x | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| (24) Effect of uncertainty | ✔ | x | x | ✔ | ✔ | ✔ | ✔ | x | x | ✔ | x | x | ✔ | ✔ | x | ✔ | x | x | ✔ | x | x | ✔ | x | x | x |
| (25) Effect of engagement with patients and others affected by the study | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| (26) Study findings, limitations, generalizability, and current knowledge | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ± | ✔ | ✔ | ✔ | ✔ |
| (27) Source of funding | ✔ | ✔ | ✔ | ✔ | x | x | ✔ | ✔ | x | x | ✔ | ✔ | x | ✔ | ✔ | ✔ | ✔ | x | ✔ | x | x | ✔ | ✔ | ✔ | ✔ |
| (28) Conflict of interest | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | x | ✔ | x | ✔ | x | x | x | ✔ | ✔ | x | ✔ | x | x | ✔ | ✔ | ✔ | x | ✔ |
| TOTAL/28 | 18 | 18.5 | 17 | 18 | 17 | 19.5 | 19 | 15.5 | 19 | 20 | 14 | 15.5 | 13.5 | 20 | 17 | 21 | 17 | 16 | 16 | 15 | 17 | 18 | 13 | 18.5 | 20 |
| Amann et al. (2017) [77] | Ballinger et al. (2016) [76] | Holland et al. (2014) [78] | Srinivasan et al. (2018) [79] | |
|---|---|---|---|---|
| (1) Title | ✔ | ± | ✔ | ✔ |
| (2) Abstract | ± | ✔ | ✔ | ✔ |
| (3) Background and objectives | ✔ | ✔ | ✔ | ✔ |
| (4) Health economic analysis plan | x | x | x | x |
| (5) Study population | x | x | x | x |
| (6) Setting and location | ✔ | ✔ | ✔ | ✔ |
| (7) Comparators | x | ✔ | ✔ | x |
| (8) Perspective | ✔ | ✔ | x | x |
| (9) Time horizon | ✔ | ✔ | ✔ | ✔ |
| (10) Discount rate | x | ✔ | x | ✔ |
| (11) Selection of outcomes | ✔ | ✔ | ✔ | ✔ |
| (12) Measurement of outcomes | ✔ | ✔ | ✔ | ✔ |
| (13) Valuation of outcomes | ✔ | ✔ | ✔ | ✔ |
| (14) Measurement and valuation of resources and costs | ✔ | ✔ | ✔ | ✔ |
| (15) Currency, price date, and conversion | ✔ | ± | ✔ | ✔ |
| (16) Rationale and description of model | x | ✔ | ✔ | ✔ |
| (17) Analytics and assumptions | x | ✔ | ✔ | ✔ |
| (18) Characterising heterogeneity | x | x | x | x |
| (19) Characterising distributional effects | x | x | x | x |
| (20) Characterising uncertainty | ✔ | ✔ | x | x |
| (21) Approach to engagement with patients and others affected by the study | x | x | x | x |
| (22) Study parameters | ✔ | ✔ | ✔ | ✔ |
| (23) Summary of the main results | ✔ | ✔ | ✔ | ✔ |
| (24) Effect of uncertainty | ✔ | x | ✔ | x |
| (25) Effect of engagement with patients and others affected by the study | x | x | x | x |
| (26) Study findings, limitations, generalizability, and current knowledge | ✔ | ✔ | ✔ | ✔ |
| (27) Source of funding | x | ✔ | ✔ | ✔ |
| (28) Conflict of interest | x | x | x | x |
| TOTAL/28 | 15.5 | 19 | 18 | 17 |
References
- Gautam, D.; Bolia, N.B. Air pollution: Impact and interventions. Air Qual. Atmos. Health 2020, 13, 209–223. [Google Scholar] [CrossRef]
- Viana, M.; de Leeuw, F.; Bartonova, A.; Castell, N.; Ozturk, E.; Gonzalez Ortiz, A. Air quality mitigation in European cities: Status and challenges ahead. Environ. Int. 2020, 143, 105907. [Google Scholar] [CrossRef]
- World Health Organization. Air Pollution. Available online: https://www.who.int/health-topics/air-pollution#tab=tab_1 (accessed on 11 December 2023).
- Burns, J.; Boogaard, H.; Polus, S.; Pfadenhauer, L.M.; Rohwer, A.C.; van Erp, A.M.; Turley, R.; Rehfuess, E.A. Interventions to reduce ambient air pollution and their effects on health: An abridged Cochrane systematic review. Environ. Int. 2020, 135, 105400. [Google Scholar] [CrossRef] [PubMed]
- Farmer, S.A.; Nelin, T.D.; Falvo, M.J.; Wold, L.E. Ambient and household air pollution: Complex triggers of disease. Am. J. Physiol. Heart Circ. Physiol. 2014, 307, H467–H476. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Household Air Pollution. Available online: https://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health (accessed on 12 December 2023).
- Fuller, R.; Landrigan, P.J.; Balakrishnan, K.; Bathan, G.; Bose-O’Reilly, S.; Brauer, M.; Caravanos, J.; Chiles, T.; Cohen, A.; Corra, L.; et al. Pollution and health: A progress update. Lancet Planet Health 2022, 6, e535–e547. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Air Quality Guidelines. Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. Executive Summary; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Cohen, A.J.; Brauer, M.; Burnett, R.; Anderson, H.R.; Frostad, J.; Estep, K.; Balakrishnan, K.; Brunekreef, B.; Dandona, L.; Dandona, R.; et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017, 389, 1907–1918. [Google Scholar] [CrossRef]
- Miraglia, S.G.E.; Gouveia, N. Costs of air pollution in Brazilian metropolitan regions. Cienc. Saude Coletiva 2014, 19, 4141–4147. [Google Scholar] [CrossRef]
- Shamsi, H.; Munshed, M.; Tran, M.K.; Lee, Y.; Walker, S.; The, J.; Raahemifar, K.; Fowler, M. Health Cost Estimation of Traffic-Related Air Pollution and Assessing the Pollution Reduction Potential of Zero-Emission Vehicles in Toronto, Canada. Energies 2021, 14, 4956. [Google Scholar] [CrossRef]
- Devos, S.; Cox, B.; Dhondt, S.; Nawrot, T.; Putman, K. Cost saving potential in cardiovascular hospital costs due to reduction in air pollution. Sci. Total Environ. 2015, 527, 413–419. [Google Scholar] [CrossRef]
- Hutton, G. Economic Evaluation of Environmental Health Interventions to Support Decision Making. Environ. Health Insights 2008, 2, 137–155. [Google Scholar] [CrossRef]
- Lomas, J.; Schmitt, L.; Jones, S.; McGeorge, M.; Bates, E.; Holland, M.; Cooper, D.; Crowther, R.; Ashmore, M.; Rojas-Rueda, D.; et al. A pharmacoeconomic approach to assessing the costs and benefits of air quality interventions that improve health: A case study. BMJ Open 2016, 6, e010686. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Guo, C.; Wu, Y.; Huang, C.; Lu, K.; Zhang, Y.; Duan, L.; Cheng, M.; Chai, F.; Mei, F.; et al. Evaluating cost and benefit of air pollution control policies in China: A systematic review. J. Environ. Sci. 2023, 123, 140–155. [Google Scholar] [CrossRef]
- Wang, S.; Song, R.; Xu, Z.; Chen, M.; Di Tanna, G.L.; Downey, L.; Jan, S.; Si, L. The costs, health and economic impact of air pollution control strategies: A systematic review. Glob. Health Res. Policy 2024, 9, 30. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- van Mastrigt, G.A.; Hiligsmann, M.; Arts, J.J.; Broos, P.H.; Kleijnen, J.; Evers, S.M.; Majoie, M.H. How to prepare a systematic review of economic evaluations for informing evidence-based healthcare decisions: A five-step approach (part 1/3). Expert Rev. Pharmacoecon Outcomes Res. 2016, 16, 689–704. [Google Scholar] [CrossRef]
- Thielen, F.W.; Van Mastrigt, G.; Burgers, L.T.; Bramer, W.M.; Majoie, H.; Evers, S.; Kleijnen, J. How to prepare a systematic review of economic evaluations for clinical practice guidelines: Database selection and search strategy development (part 2/3). Expert Rev. Pharmacoecon Outcomes Res. 2016, 16, 705–721. [Google Scholar] [CrossRef] [PubMed]
- Wijnen, B.; Van Mastrigt, G.; Redekop, W.K.; Majoie, H.; De Kinderen, R.; Evers, S. How to prepare a systematic review of economic evaluations for informing evidence-based healthcare decisions: Data extraction, risk of bias, and transferability (part 3/3). Expert Rev. Pharmacoecon Outcomes Res. 2016, 16, 723–732. [Google Scholar] [CrossRef]
- Werbrouck, A.; Schmidt, M.; Putman, K.; Benhalima, K.; Verhaeghe, N.; Annemans, L.; Simoens, S. A systematic review on costs and cost-effectiveness of screening and prevention of type 2 diabetes in women with prior gestational diabetes: Exploring uncharted territory. Diabetes Res. Clin. Pract. 2019, 147, 138–148. [Google Scholar] [CrossRef]
- Ge, X.; Cui, K.; Ma, H.; Zhao, S.; Meng, W.; Wang, W. Cost-effectiveness of comprehensive preventive measures for coal workers’ pneumoconiosis in China. BMC Health Serv. Res. 2022, 22, 266. [Google Scholar] [CrossRef]
- Huang, L.; Cheng, H.; Ma, S.; He, R.; Gong, J.; Li, G.; An, T. The exposures and health effects of benzene, toluene and naphthalene for Chinese chefs in multiple cooking styles of kitchens. Environ. Int. 2021, 156, 106721. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Mandrik, O.; Severens, J.L.; Bardach, A.; Ghabri, S.; Hamel, C.; Mathes, T.; Vale, L.; Wisløff, T.; Goldhaber-Fiebert, J.D. Critical Appraisal of Systematic Reviews With Costs and Cost-Effectiveness Outcomes: An ISPOR Good Practices Task Force Report. Value Health 2021, 24, 463–472. [Google Scholar] [CrossRef] [PubMed]
- Guerriero, C. Chapter 1—The key steps in cost–benefit analysis of environmental health interventions. In Cost-Benefit Analysis of Environmental Health Interventions; Guerriero, C., Ed.; Academic Press: Cambridge, MA, USA, 2020; pp. 1–19. [Google Scholar]
- EPPI. CCEMG—EPPI-Centre Cost Converter. Available online: https://eppi.ioe.ac.uk/costconversion/ (accessed on 26 February 2025).
- Catalá-López, F.; Ridao, M.; Alonso-Arroyo, A.; García-Altés, A.; Cameron, C.; González-Bermejo, D.; Aleixandre-Benavent, R.; Bernal-Delgado, E.; Peiró, S.; Tabarés-Seisdedos, R.; et al. The quality of reporting methods and results of cost-effectiveness analyses in Spain: A methodological systematic review. Syst. Rev. 2016, 5, 6. [Google Scholar] [CrossRef]
- Husereau, D.; Drummond, M.; Augustovski, F.; de Bekker-Grob, E.; Briggs, A.H.; Carswell, C.; Caulley, L.; Chaiyakunapruk, N.; Greenberg, D.; Loder, E.; et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) Statement: Updated Reporting Guidance for Health Economic Evaluations. Value Health 2022, 25, 3–9. [Google Scholar] [CrossRef]
- Giannakis, E.; Kushta, J.; Bruggeman, A.; Lelieveld, J. Costs and benefits of agricultural ammonia emission abatement options for compliance with European air quality regulations. Environ. Sci. Eur. 2019, 31, 93. [Google Scholar] [CrossRef]
- Howard, D.B.; Thé, J.; Soria, R.; Fann, N.; Schaeffer, R.; Saphores, J.-D.M. Health benefits and control costs of tightening particulate matter emissions standards for coal power plants—The case of Northeast Brazil. Environ. Int. 2019, 124, 420–430. [Google Scholar] [CrossRef]
- Jeuland, M.; Soo, J.S. Analyzing the Costs and Benefits of Clean and Improved Cooking Solutions; Clean Cooking Alliance: Washington, DC, USA, 2016. [Google Scholar]
- Mardones, C. Ex-post evaluation and cost-benefit analysis of a heater replacement program implemented in southern Chile. Energy 2021, 227, 120484. [Google Scholar] [CrossRef]
- Meng, W.; Kiesewetter, G.; Zhang, S.; Schoepp, W.; Rafaj, P.; Klimont, Z.; Tao, S. Costs and Benefits of Household Fuel Policies and Alternative Strategies in the Jing-Jin-Ji Region. Environ. Sci. Technol. 2023, 57, 21662–21672. [Google Scholar] [CrossRef] [PubMed]
- Wagner, S.; Angenendt, E.; Beletskaya, O.; Zeddies, J. Costs and benefits of ammonia and particulate matter abatement in German agriculture including interactions with greenhouse gas emissions. Agric. Syst. 2015, 141, 58–68. [Google Scholar] [CrossRef]
- Yang, K.; Wang, Y.; Guo, Y.; Liu, N.; Weschler, L.; Wei, J.; Guo, J.; Cao, Y.; Zhang, Y. Cost-effective analysis of different intervention scenarios with air cleaners to reduce the exposure to fine particulate matters in China. J. Build. Eng. 2024, 86, 108827. [Google Scholar] [CrossRef]
- Zhang, X.; Gu, B.; van Grinsven, H.; Lam, S.K.; Liang, X.; Bai, M.; Chen, D. Societal benefits of halving agricultural ammonia emissions in China far exceed the abatement costs. Nat. Commun. 2020, 11, 4357. [Google Scholar] [CrossRef] [PubMed]
- Aunan, K.; Alnes, L.W.H.; Berger, J.; Dong, Z.; Ma, L.; Mestl, H.E.S.; Vennemo, H.; Wang, S.; Zhang, W. Upgrading to cleaner household stoves and reducing chronic obstructive pulmonary disease among women in rural China—A cost-benefit analysis. Energy Sustain. Dev. 2013, 17, 489–496. [Google Scholar] [CrossRef]
- Chen, F.; Yamashita, K.; Kurokawa, J.; Klimont, Z. Cost–Benefit Analysis of Reducing Premature Mortality Caused by Exposure to Ozone and PM2.5 in East Asia in 2020. Water Air Soil Pollut. 2015, 226, 108. [Google Scholar] [CrossRef]
- Evans, J.; Rojas-Bracho, L.; Hammitt, J.; Dockery, D. Mortality Benefits and Control Costs of Improving Air Quality in Mexico City: The Case of Heavy Duty Diesel Vehicles. Risk Anal. 2020, 41, 661–677. [Google Scholar] [CrossRef]
- Feng, T.; Du, H.; Coffman, D.M.; Qu, A.; Dong, Z. Clean heating and heating poverty: A perspective based on cost-benefit analysis. Energy Policy 2021, 152, 112205. [Google Scholar] [CrossRef]
- Fisk, W.J.; Chan, W.R. Effectiveness and cost of reducing particle-related mortality with particle filtration. Indoor Air 2017, 27, 909–920. [Google Scholar] [CrossRef] [PubMed]
- Fisk, W.J.; Chan, W.R. Health benefits and costs of filtration interventions that reduce indoor exposure to PM2.5 during wildfires. Indoor Air 2017, 27, 191–204. [Google Scholar] [CrossRef]
- Gao, J.; Yuan, Z.; Liu, X.; Xia, X.; Huang, X.; Dong, Z. Improving air pollution control policy in China—A perspective based on cost–benefit analysis. Sci. Total Environ. 2016, 543, 307–314. [Google Scholar] [CrossRef]
- Irfan, M.; Cameron, M.P.; Hassan, G. Interventions to mitigate indoor air pollution: A cost-benefit analysis. PLoS ONE 2021, 16, e0257543. [Google Scholar] [CrossRef]
- Levy, J.I.; Biton, L.; Hopke, P.K.; Zhang, K.M.; Rector, L. A cost-benefit analysis of a pellet boiler with electrostatic precipitator versus conventional biomass technology: A case study of an institutional boiler in Syracuse, New York. Environ. Res. 2017, 156, 312–319. [Google Scholar] [CrossRef]
- Liu, Y.; Zhou, B.; Wang, J.; Zhao, B. Health benefits and cost of using air purifiers to reduce exposure to ambient fine particulate pollution in China. J. Hazard. Mater. 2021, 414, 125540. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Aparicio, S.; Grythe, H.; Thorne, R.; Vogt, M. Costs and benefits of implementing an Environmental Speed Limit in a Nordic city. Sci. Total Environ. 2020, 70, 137577. [Google Scholar] [CrossRef]
- Meng, W.; Zhu, L.; Liang, Z.; Xu, H.; Zhang, W.; Li, J.; Zhang, Y.; Luo, Z.; Shen, G.; Shen, H.; et al. Significant but Inequitable Cost-Effective Benefits of a Clean Heating Campaign in Northern China. Environ. Sci. Technol. 2023, 57, 8467–8475. [Google Scholar] [CrossRef] [PubMed]
- Miranda, A.I.; Ferreira, J.; Silveira, C.; Relvas, H.; Duque, L.; Roebeling, P.; Lopes, M.; Costa, S.; Monteiro, A.; Gama, C.; et al. A cost-efficiency and health benefit approach to improve urban air quality. Sci. Total Environ. 2016, 569–570, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Schucht, S.; Real, E.; Couvidat, F.; Rouil, L.; Brignon, J.-M.; Allemand, N.; Clercq, G.; Fayolle, D. Analyse économique des impacts sanitaires dans le cadre de l’élaboration du PREPA. Environ. Risques Santé 2018, 17, 393–400. [Google Scholar]
- Thompson, T.; Rausch, S.; Saari, R.; Selin, N. Air Quality Co-Benefits of Sub-National Carbon Policies. J. Air Waste Manag. Assoc. 2016, 66, 988–1002. [Google Scholar] [CrossRef]
- Wagner, S.; Angenendt, E.; Beletskaya, O.; Zeddies, J. Assessing ammonia emission abatement measures in agriculture: Farmers’ costs and society’s benefits—Case study for Lower Saxony, Germany. Agric. Syst. 2017, 157, 70–80. [Google Scholar] [CrossRef]
- Wan, R.; Tang, L.; Guo, J.; Zhai, W.; Li, L.; Xie, Y.; Bo, X.; Wu, J. Cost-benefits analysis of ultra-low emissions standard on air quality and health impact in thermal power plants in China. J. Environ. Manag. 2023, 345, 118731. [Google Scholar] [CrossRef]
- Wiser, R.; Mai, T.; Millstein, D.; Barbose, G.; Bird, L.; Heeter, J.; Keyser, D.; Krishnan, V.; Macknick, J. Assessing the costs and benefits of US renewable portfolio standards. Environ. Res. Lett. 2017, 12, 094023. [Google Scholar] [CrossRef]
- Zhang, A.; Liu, Y.; Ji, J.S.; Zhao, B. Air Purifier Intervention to Remove Indoor PM(2.5) in Urban China: A Cost-Effectiveness and Health Inequality Impact Study. Environ. Sci. Technol. 2023, 57, 4492–4503. [Google Scholar] [CrossRef]
- Zhang, H.; Zhang, B.; Bi, J. More efforts, more benefits: Air pollutant control of coal-fired power plants in China. Energy 2015, 80, 1–9. [Google Scholar] [CrossRef]
- Zhang, J.; Jiang, H.; Zhang, W.; Ma, G.; Wang, Y.; Lu, Y.; Hu, X.; Zhou, J.; Peng, F.; Bi, J.; et al. Cost-benefit analysis of China’s Action Plan for Air Pollution Prevention and Control. Front. Eng. Manag. 2019, 6, 524–537. [Google Scholar] [CrossRef]
- Zhao, N.; Elshareef, H.; Li, B.; Wang, B.; Jia, Z.; Zhou, L.; Liu, Y.; Sultan, M.; Dong, R.; Zhou, Y. The efforts of China to combat air pollution during the period of 2015–2018: A case study assessing the environmental, health and economic benefits in the Beijing-Tianjin-Hebei and surrounding “2 + 26” regions. Sci. Total Environ. 2022, 853, 158437. [Google Scholar] [CrossRef]
- Zhou, J.; Wang, J.; Jiang, H.; Cheng, X.; Lu, Y.; Zhang, W.; Bi, J.; Xue, W.; Liu, N. Cost-benefit analysis of yellow-label vehicles scrappage subsidy policy: A case study of Beijing-Tianjin-Hebei region of China. J. Clean. Prod. 2019, 232, 94–103. [Google Scholar] [CrossRef]
- Zhou, J.; Jiang, H.; Cheng, X.; Lu, Y.; Zhang, W.; Dong, Z. Are the Benefits of a High-Emission Vehicle Driving Area Restriction Policy Greater Than the Costs? Int. J. Environ. Res. Public Health 2022, 19, 15789. [Google Scholar] [CrossRef] [PubMed]
- Cansino, J.; Moreno, R.; Quintana, D.; Román-Collado, R. Health and Heating in the City of Temuco (Chile). Monetary Savings of Replacing Biomass with PV System in the Residential Sector. Sustainability 2019, 11, 5205. [Google Scholar] [CrossRef]
- Cropper, M.L.; Guttikunda, S.; Jawahar, P.; Lazri, Z.; Malik, K.; Song, X.P.; Yao, X. Applying Benefit-Cost Analysis to Air Pollution Control in the Indian Power Sector. J. Benefit Cost Anal. 2019, 10, 185–205. [Google Scholar] [CrossRef]
- Guo, Y.; Zhou, M.; Peng, L.; Yang, J.; Li, M.; Chen, L.; Mauzerall, D. Carbon Mitigation and Environmental Co-Benefits of a Clean Energy Transition in China’s Industrial Parks. Environ. Sci. Technol. 2023, 57, 6494–6505. [Google Scholar] [CrossRef]
- Lavee, D. Cost-benefit analysis of implementing policy measures for reducing PM and O3 concentrations: The case of Israel. J. Pollut. Eff. Control. 2017, 5, 683–695. [Google Scholar] [CrossRef]
- Whitehurst, D.G.T.; DeVries, D.N.; Fuller, D.; Winters, M. An economic analysis of the health-related benefits associated with bicycle infrastructure investment in three Canadian cities. PLoS ONE 2021, 16, e0246419. [Google Scholar] [CrossRef]
- Liu, K.; Wang, K.; Jia, S.; Liu, Y.; Liu, S.; Yin, Z.; Zhang, X. Air quality and health benefits for different heating decarbonization pathways in China. Sci. Total Environ. 2024, 919, 170976. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhang, Y.; Wang, Y.; Jiang, F.; Qi, Z.; Cao, W.; Xue, W.; Ni, X.; Zhang, Q.; Wang, J. Cost-Effectiveness of NOX and VOC Co-operative Controls for PM2.5 and O3 Mitigation in the Context of China’s Carbon Neutrality. Environ. Sci. Technol. Lett. 2023, 10, 1109–1116. [Google Scholar] [CrossRef]
- Ramirez, C.; Khavari, B.; Oberholzer, A.; Ghimire, B.R.; Mishra, B.; Sinclair-Lecaros, S.; Mentis, D.; Gurung, A.; Khatiwada, D.; Nerini, F.F. Achieving Nepal’s clean cooking ambitions: An open source and geospatial cost–benefit analysis. Lancet Planet. Health 2024, 8, e754–e765. [Google Scholar] [CrossRef]
- Adibi, A.; Barn, P.; Shellington, E.M.; Harvard, S.; Johnson, K.M.; Carlsten, C. HEPA Air Filters for Preventing Wildfire-Related Asthma Complications, a Cost-effectiveness Study. medRxiv 2023, 2023, 23288697. [Google Scholar] [CrossRef]
- Kim, S.; Xiao, C.; Platt, I.; Zafari, Z.; Bellanger, M.; Muennig, P. Health and economic consequences of applying the United States’ PM2.5 automobile emission standards to other nations: A case study of France and Italy. Public Health 2020, 183, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, L.H.M. QALY gain and health care resource impacts of air pollution control: A Markov modelling approach. Environ. Sci. Policy 2016, 63, 35–43. [Google Scholar] [CrossRef]
- Buonocore, J.J.; Lambert, K.F.; Burtraw, D.; Sekar, S.; Driscoll, C.T. An Analysis of Costs and Health Co-Benefits for a U.S. Power Plant Carbon Standard. PLoS ONE 2016, 11, e0156308. [Google Scholar] [CrossRef]
- Giannadaki, D.; Giannakis, E.; Pozzer, A.; Lelieveld, J. Estimating health and economic benefits of reductions in air pollution from agriculture. Sci. Total Environ. 2018, 622–623, 1304–1316. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Huang, X.; Song, Y.; Tang, J.; Cao, J.; Zhang, X.; Zhang, Q.; Wang, S.; Xu, T.; Kang, L.; et al. Ammonia emission control in China would mitigate haze pollution and nitrogen deposition, but worsen acid rain. Proc. Natl. Acad. Sci. USA 2019, 116, 7760–7765. [Google Scholar] [CrossRef]
- Ballinger, A.; Chowdhury, T.; Chris, S.; Cole, G. Air Pollution: Economic Analysis. Main Report; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- Amann, M.; Holland, M.; Maas, R.; Vandyck, T.; Saveyn, B. Costs, Benefits and Economic Impacts of the EU Clean Air Strategy and Their Implications on Innovation and Competitiveness. IIASA Report; International Institute for Applied Systems Analysis (IIASA): Laxenburg, Austria, 2017. [Google Scholar]
- Holland, M. Cost-Benefit Analysis of Final Policy Scenarios for the EU Clean Air Package; European Maritime Safety Agency: Lisboa, Portugal, 2016. [Google Scholar]
- Srinivasan, S.; Roshna, N.; Guttikunda, S.; Kanudia, A.; Saif, S.; Asundi, J. Benefit Cost Analysis of Emission Standards for Coal-based Thermal Power Plants in India, (CSTEP-Report-2018-06); Shakti Sustainable Energy Foundation: New Delhi, India, 2018. [Google Scholar]
- Bojke, L.; Schmitt, L.; Lomas, J.; Richardson, G.; Weatherly, H. Economic Evaluation of Environmental Interventions: Reflections on Methodological Challenges and Developments. Int. J. Environ. Res. Public Health 2018, 15, 2459. [Google Scholar] [CrossRef]
- Center for Science Education. Effects of Air Pollution. Available online: https://scied.ucar.edu/learning-zone/air-quality/effects-air-pollution (accessed on 26 February 2025).
- Hutton, G.; Rehfuess, E.; World Health Organization. Guidelines for Conducting Cost-Benefit Analysis of Household Energy and Health Interventions/Guy Hutton with Eva Rehfuess; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Turner, H.C.; Archer, R.A.; Downey, L.E.; Isaranuwatchai, W.; Chalkidou, K.; Jit, M.; Teerawattananon, Y. An Introduction to the Main Types of Economic Evaluations Used for Informing Priority Setting and Resource Allocation in Healthcare: Key Features, Uses, and Limitations. Front. Public Health 2021, 9, 722927. [Google Scholar] [CrossRef] [PubMed]
- Tran, V.V.; Park, D.; Lee, Y.C. Indoor Air Pollution, Related Human Diseases, and Recent Trends in the Control and Improvement of Indoor Air Quality. Int. J. Environ. Res. Public Health 2020, 17, 2927. [Google Scholar] [CrossRef]
- Ritchie, H.; Roser, M. Indoor Air Pollution. Available online: https://ourworldindata.org/indoor-air-pollution#:~:text=In%20the%20map%20here,%20we%20see (accessed on 26 February 2025).
- Rentschler, J.; Leonova, N. Global air pollution exposure and poverty. Nat. Commun. 2023, 14, 4432. [Google Scholar] [CrossRef] [PubMed]
- Jonidi Jafari, A.; Charkhloo, E.; Pasalari, H. Urban air pollution control policies and strategies: A systematic review. J. Environ. Health Sci. Eng. 2021, 19, 1911–1940. [Google Scholar] [CrossRef]
- Ferguson, L.; Taylor, J.; Davies, M.; Shrubsole, C.; Symonds, P.; Dimitroulopoulou, S. Exposure to indoor air pollution across socio-economic groups in high-income countries: A scoping review of the literature and a modelling methodology. Environ. Int. 2020, 143, 105748. [Google Scholar] [CrossRef]
- Sofia, D.; Gioiella, F.; Lotrecchiano, N.; Giuliano, A. Mitigation strategies for reducing air pollution. Environ. Sci. Pollut. Res. Int. 2020, 27, 19226–19235. [Google Scholar] [CrossRef]
- State of Global Air. PM2.5. Available online: https://www.stateofglobalair.org/pollution-sources/pm25 (accessed on 26 February 2025).
- United States Environmental Protection Agency. Managing Air Quality—Multi-Pollutant Planning and Control. Available online: https://www.epa.gov/air-quality-management-process/managing-air-quality-multi-pollutant-planning-and-control#:~:text=Some%20control%20technologies%20can%20reduce%20emissions%20of%20multiple,goals%20in%20developing%20an%20air%20pollution%20management%20plan (accessed on 26 February 2025).
- Wesson, K.; Fann, N.; Morris, M.; Fox, T.; Hubbell, B. A multi–pollutant, risk–based approach to air quality management: Case study for Detroit. Atmos. Pollut. Res. 2010, 1, 296–304. [Google Scholar] [CrossRef]
- Martuzzi, M.; George, F. Chapter 5—Health benefit analysis: Monetization of health impacts and its use in environment and health. In Cost-Benefit Analysis of Environmental Health Interventions; Guerriero, C., Ed.; Academic Press: Cambridge, MA, USA, 2020; pp. 95–109. [Google Scholar]
- Kim, D.D.; Silver, M.C.; Kunst, N.; Cohen, J.T.; Ollendorf, D.A.; Neumann, P.J. Perspective and Costing in Cost-Effectiveness Analysis, 1974-2018. Pharmacoeconomics 2020, 38, 1135–1145. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, T. Cost-Benefit Analysis and the environment: The time horizon is of the essence. Environ. Impact Assess. Rev. 2021, 89, 106587. [Google Scholar] [CrossRef]
- Brouwer, W.B.F.; Niessen, L.W.; Postma, M.J.; Rutten, F.F.H. Need for differential discounting of costs and health effects in cost effectiveness analyses. BMJ 2005, 331, 446. [Google Scholar] [CrossRef]
- Jain, R.; Grabner, M.; Onukwugha, E. Sensitivity Analysis in Cost-Effectiveness Studies. Pharmacoeconomics 2011, 29, 297–314. [Google Scholar] [CrossRef] [PubMed]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Drummond—Methods for the Economic Evaluation of Health Care Programmes; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Williams, I.; Brown, H.; Healy, P. Contextual Factors Influencing Cost and Quality Decisions in Health and Care: A Structured Evidence Review and Narrative Synthesis. Int. J. Health Policy Manag. 2018, 7, 683–695. [Google Scholar] [CrossRef] [PubMed]
- Welte, R.; Feenstra, T.; Jager, H.; Leidl, R. A decision chart for assessing and improving the transferability of economic evaluation results between countries. Pharmacoeconomics 2004, 22, 857–876. [Google Scholar] [CrossRef] [PubMed]
- Mandrik, O.; Knies, S.; Kaló, Z.; Severens, H. Reviewing Transferability in Economic Evaluations Originating from Eastern Europe. Int. J. Technol. Assess. Health Care 2015, 31, 434–441. [Google Scholar] [CrossRef]
- Goeree, R.; Burke, N.; O’Reilly, D.; Manca, A.; Blackhouse, G.; Tarride, J.-E. Transferability of economic evaluations: Approaches and factors to consider when using results from one geographic area for another. Curr. Med. Res. Opin. 2007, 23, 671–682. [Google Scholar] [CrossRef]
- World Health Organization. Considerations in Evaluating the Cost-Effectiveness of Environmental Health Interventions; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]

| Parameter | Inclusion | Exclusion |
|---|---|---|
| Population | General exposure to air pollution | Occupational exposure |
| Intervention | Strategies aimed at reducing or controlling air pollution both indoors and outdoors. | Strategies where the reduction in air pollution occurs as a ‘co-benefit’ |
| Comparator | / | |
| Outcome | Studies that take costs and health outcomes into account to calculate ICER/ICUR/NB/CBR | Only costs, exclusion of health outcomes |
| Study design | Cost-effectiveness analysis, cost–utility analysis, cost–benefit analysis, cost-minimisation analysis, pre–post study designs, (non-)randomised controlled trials | Other study designs (i.e., reviews, meta-analyses) |
| Geography | No limitations | / |
| Language | English, French, Dutch | Other languages |
| Publication date | From 2013 | Before 2013 |
| Cost–Benefit Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author (Publication Year) | Country | Sort of Pollutant | ||||||
| NH3 | PM * | NOx | O3 | SO2 | COx | NS | ||
| Aunan et al. (2013) [38] | China | x | ||||||
| Cansino et al. (2019) [62] | Temuco (Chile) | x | ||||||
| Chen et al. (2015) [39] | East Asia | x | x | |||||
| Cropper et al. (2017) [63] | India | x | x | |||||
| Evans et al. (2021) [40] | Mexico City | x | ||||||
| Feng et al. (2021) [41] | China | x | ||||||
| Fisk et al. (2017) [43] | South California (USA) | x | ||||||
| Fisk et al. (2017a) [42] | USA (Los Angeles CA, Elizabeth NJ, Houston TX) | x | ||||||
| Gao et al. (2016) [44] | China | x | x | x | ||||
| Giannakis et al. (2019) [30] | Europe | x | ||||||
| Guo et al. (2023) [64] | China | x | x | |||||
| Howard et al. (2019) [31] | Northeast Brazil | x | ||||||
| Irfan et al. (2021) [45] | Pakistan | x | ||||||
| Jeuland et al. (2016) [32] | South Asia/global | x | ||||||
| Lavee et al. (2018) [65] | Israël | x | x | |||||
| Levy et al. (2017) [46] | New York | x | ||||||
| Liu K et al. (2024) [67] | China | x | x | x | ||||
| Liu Y. et al. (2021) [47] | China | x | ||||||
| Liu Z et al. (2023) [68] | China | x | x | |||||
| Lopez-Aparicio et al. (2020) [48] | Oslo (Norway) | x | x | x | ||||
| Mardones et al. (2021) [33] | Southern Chile | x | ||||||
| Meng W. et al. (2023) [34] | Jing-Jin-Ji Region (China) | x | ||||||
| Meng W. et al. (2023a) [49] | China | x | ||||||
| Miranda et al. (2016) [50] | Grande Porto area | x | x | |||||
| Ramirez et al. (2024) [69] | Nepal | x | ||||||
| Schucht et al. (2018) [51] | France | x | x | x | ||||
| Thompson et al. (2016) [52] | USA | x | x | |||||
| Wagner et al. (2015) [35] | Germany (German Federal States of Lower Saxony, Brandenburg, Baden-Württemberg) | x | x | |||||
| Wagner et al. (2017) [53] | Germany (Lower Saxony) | x | ||||||
| Wan et al. (2023) [54] | China | x | x | x | ||||
| Whitehurst et al. (2021) [66] | Canada | x | ||||||
| Wiser et al. (2017) [55] | US | x | x | |||||
| Yang et al. (2024) [36] | China (Beijing, Harbin, Shanghai, Guangzhou, Sanya, Kunming) | x | ||||||
| Zhang et al. (2015) [57] | China | x | x | |||||
| Zhang et al. (2019) [58] | China | x | ||||||
| Zhang et al. (2020) [37] | China | x | ||||||
| Zhang et al. (2023) [56] | China | x | ||||||
| Zhao et al. (2022) [59] | China | x | x | x | x | x | ||
| Zhou et al. (2019) [60] | China (BTH region) | x | ||||||
| Zhou et al. (2022) [61] | China (BTH region) | x | ||||||
| Cost–utility analysis | ||||||||
| Adibi et al. (2023) [70] | Canada | x | ||||||
| Kim et al. (2020) [71] | Italy, France | x | ||||||
| Lomas et al. (2016) [14] | UK | x | x | |||||
| Schmitt L.H.M. (2016) [72] | UK | x | ||||||
| Not specified | ||||||||
| Buonocore et al. (2016) [73] | USA | x | ||||||
| Giannadaki et al. (2018) [74] | Europe, America, Asia | x | ||||||
| Liu M. et al. (2019) [75] | China | x | ||||||
| Author (Publication Year) | Study Design | Model | Perspective | Time Horizon | Costs | Valuta | Discount Rate | Reference Year |
|---|---|---|---|---|---|---|---|---|
| Adibi et al. (2023) [70] | CUA | Markov model | Healthcare perspective | 2018–2022 | Healthcare costs, Compliance costs | CAD | Costs: 1.5% Benefits: 1.5% | 2023 |
| Aunan et al. (2013) [38] | CBA | Not specified | / | / | Compliance costs | CNY | Costs: 8% Benefits: 8% | 2010 |
| Buonocore et al. (2016) [73] | Not specified | Combination of Integrated Planning Model + Community Multiscale Air Quality Model + BenMAP CE | / | / | Compliance costs | USD | / | 2013 |
| Cansino et al. (2019) [62] | CBA | Ex post evaluation | / | / | Compliance costs | USD | / | 2013 |
| Chen et al. (2015) [39] | CBA | Combination of CMAQ/REAS + GAINS + arc GIS system models | / | / | Not specified | USD | Costs: 10% Benefits: / | 2020 |
| Cropper et al. (2017) [63] | CBA | Combination of CAMx + IERs | / | / | Compliance costs | USD | Costs: 3% Benefits: 3–8% | 2015 |
| Evans et al. (2021) [40] | BKA | Not specified | / | / | Compliance costs | USD | Costs: 3% Benefits: / | / |
| Feng et al. (2021) [41] | CBA | Ex post evaluation (difference-in-difference modelling) | Costs: governmental perspective Benefits: residents | 2015–2018 | Compliance costs, Regulatory costs | CNY | / | / |
| Fisk et al. (2017) [43] | CBA | Not specified | / | / | Compliance costs | USD | / | 2003 |
| Fisk et al. (2017a) [42,43] | BCA | Not specified | / | / | Compliance costs | USD | / | / |
| Gao et al. (2016) [44] | CBA | Not specified | Societal perspective | 5 years | Not specified | CNY | Costs: 3% Benefits: / | 2012 |
| Giannadaki et al. (2018) [74] | Not specified | Combination of ‘EMAC global atmospheric chemistry–climate model + health impact function + exposure response function’ | Societal perspective | / | Compliance costs | USD | / | 2010 |
| Giannakis et al. (2019) [30] | CBA | Combination of models: WRF/Chem model | / | / | Not specified | M EUR | / | 2016 |
| Guo et al. (2023) [64] | CBA | Combination of WRF/Chem model + health impact assessment | / | / | Compliance costs | USD | / | 2015 |
| Howard et al. (2019) [31] | CBA | Combination of Plexos + CALPUFF + BenMAP models | / | / | Compliance costs | USD | / | 2015 |
| Irfan et al. (2021) [45] | CBA | Not specified | / | 2014–2024 | Compliance costs | INR, USD | Costs: 3%; 7.5%; 12% Benefits: 3%; 7.5%; 12% | 2014 |
| Jeuland et al. (2016) [32] | CBA | Not specified | Household and societal perspective | 100 | Compliance costs | USD | Private costs: 5–15% Social costs: 1–6% | / |
| Kim et al. (2020) [71] | CUA | Markov model | / | Life time | Compliance costs, Healthcare costs | EUR | Costs: 3% QALYs: 3% | 2018 |
| Lavee et al. (2018) [65] | CBA | Combination of ‘IMoEP air quality forecast models + dose–response functions’ | / | / | Not specified | ILS | / | / |
| Levy et al. (2017) [46] | CBA | Combination of AERMOD + BenMAP models | / | 20 years | Compliance costs | USD | Costs: 3% Benefits: 3% | / |
| Liu K et al. (2024) [67] | CBA | Combination of models: Facility-level emission inventory + CMAQ + GEMM | / | 2020–2060 | Compliance costs Regulatory costs | CNY | / | 2020 |
| Liu M. et al. (2019) [75] | Not specified | Combination of WRF/Chem + GAINS model | / | / | Not specified | USD | / | / |
| Liu Y. et al. (2021) [47] | CBA | Combination of exposure assessment model + health risk assessment model + cost-effectiveness assessment model | / | / | Compliance costs | CNY | / | / |
| Liu Z et al. (2023) [68] | CBA | Combination of DPEC model + RSM | Societal perspective | 2020–2060 | Compliance costs | USD | / | 2020 |
| Lomas et al. (2016) [14] | CUA | Not specified | Healthcare perspective | Life time | Not specified | GBP | Costs: 3.5% Benefits: 3.5% | / |
| Lopez-Aparicio et al. (2020) [48] | CBA | Combination of ‘emission inventory + different atmospheric dispersion models + population exposure’ | / | / | Other costs: private and social costs, health, climate, accidents, noise | NOK | / | 2019 |
| Mardones et al. (2021) [33] | CBA | Ex post evaluation (difference-in-difference modelling) | / | / | Compliance costs, Regulatory costs | CLP | Costs: 6% | / |
| Meng et al. (2023) [34] | CBA | Combination of models: GAINS model | / | 2020–2030 | Compliance costs | CNY | Costs: 4% | 2020 |
| Meng et al. (2023) [49] | CBA | Combination of ‘Energy consumption and emission modelling + WRF/Chem model’ | / | / | Compliance costs | RMB | Costs: 6% Benefits: / | 2021 |
| Miranda et al. (2016) [50] | CBA | Combination of models, not specified, | / | / | Compliance costs | M EUR | / | 2012 |
| Ramirez et al. (2024) [69] | CBA | Open-source clean cooking cost–benefit analysis tool OneStove + multicriteria analysis based on the Energy Access Explorer methods | Societal perspective Private household perspective | 2021–2030 | Compliance costs | USD | / | 2021 |
| Schmitt L.H.M. (2016) [72,80] | CUA | Markov model | / | 60 years | Healthcare costs | GBP | Costs: 3.5% Benefits: 3.5% | 2013 |
| Schucht et al. (2018) [51] | CBA | Combination of CHIMERE ARP-France model | / | / | Not specified | M EUR | / | 2012 |
| Thompson et al. (2016) [52] | CBA | Combination of ‘United Stated Energy Policy + Comprehensive Air quality Model with Extensions + BenMAP + mortality incidence’ | / | / | Regulatory costs | USD | / | 2006 |
| Wagner et al. (2015) [35] | CBA | Combination of EFEM + EcoSense modelling | Costs: farmer’s perspectiveBenefits: societal perspective | / | Not specified (‘reduction cost’) | M EUR | / | 2015 |
| Wagner et al. (2017) [53] | CBA | Combination of economic–ecological farm model + integrated environmental assessment model | Costs: farmer’s perspectiveBenefits: societal perspective | 2015–2050 | Other costs: reduction in gross profit margin due to mitigation measures | EUR | Costs: 3% in 2030 and 2% from 2030 to 2050 Benefits: / | 2015 |
| Wan et al. (2023) [54] | CBA | Combination of ‘China Emissions Accounts for Power Plants database + WRF-CAMx + IMED/HEL + LCOE model’ | / | / | Not specified | CNY | / | 2015 |
| Whitehurst et al. (2021) [66] | CBA | Not specified | Perspective of local government | 10 years | Compliance costs | USD | Costs: 1.5% Benefits: / | 2016 |
| Wiser et al. (2017) [55] | CBA | Combination of models: an electric generation capacity expansion model | / | 2015–2050 | Compliance costs | USD | Costs: 3% Benefits: 1.5% | / |
| Yang et al. (2024) [36] | CBA | Not specified | / | / | Compliance costs | CNY | / | / |
| Zhang et al. (2015) [57] | CBA | Not specified | / | 2006–2015 | Compliance costs | USD | / | 2006 |
| Zhang et al. (2019) [58] | CBA | Ex post evaluation | Societal perspective | / | Not specified | RMB | / | 2013 |
| Zhang et al. (2020) [37] | CBA | Combination of CHANS + GAINS + WRF-CMAQ + exposure response models | / | / | Compliance costs | CNY | Costs: 2% | 2015 |
| Zhang et al. (2023) [56] | CBA | Not specified | / | / | Compliance costs | CNY | / | / |
| Zhao et al. (2022) [59] | CBA | Ex post evaluation | / | 2016–2018 | Not specified | CNY | / | / |
| Zhou et al. (2019) [60] | CBA | Combination of WRF-CMAQ-response functions–economic evaluation model | Societal perspective (government residents, enterprises) | 2008–2015 | Other costs | CNY | Costs: 8% Benefits: 8% | 2015 |
| Zhou et al. (2022) [61] | CBA | Idem Zhou et al. (2019) [60] | Societal perspective | 2008–2016 | Not specified | CNY | Costs: 8% Benefits: 8% | 2015 |
| Author (Publication Year) | Study Design | Model | Perspective | Time Horizon | Costs | Valuta | Discount Rate | Reference Year |
|---|---|---|---|---|---|---|---|---|
| Amann et al. (2017) [77] | CBA | Combination of models: GAINS | Societal perspective | 2005–2030 | Compliance costs, Regulatory costs | EUR | / | 2005 |
| Ballinger et al. (2016) [76] | CBA and CUA | Not specified | Perspective of local government | 30 years | Compliance costs | GBP | Costs: 3.5% Benefits: 3.5% | / |
| Holland et al. (2014) [78] | CBA | Combination of models: GAINS | / | 2010–2030 | Healthcare costs (direct and indirect) | EUR | / | 2005 |
| Srinivasan et al. (2018) [79] | CBA | Combination of models: CAMx | / | 2015–2030 | Compliance costs | INR | Costs: 8% Benefits: 8% | 2015 |
| Author (Publication Year) | Outcome (Valuation Outcome) | Sensitivity Analysis | Incremental Costs (1) Incremental Benefits (2) | Cost-Effectiveness Results | Results of Sensitivity Analysis |
|---|---|---|---|---|---|
| Adibi et al. (2023) [70] | QALYs (EQ-5D) | OWSA, PSA | (1) USD 70.9–86.4 (2) 0.0018–0.0010 QALY | ICERs between USD 38,628 and 85,445 (±) | PSA: 80.2% in KB, 43.6% in Ok, 29.6% in TCS. OWSA: risk ratio of increased salbutamol dispensation and hospitalisation, utility of well-controlled and uncontrolled asthma, and retail price of air filter units are the most influential parameters. |
| Aunan et al. (2013) [38] | Health benefits (VSL) | OWSA Monte Carlo analysis | / | BCR: S1a: 14.7; S1b: 3.3, S2a: 14.5, S2b: 3.7 (+) | OWSA: lifetime of intervention, value of VSL, and baseline COPD prevalence are the most influential parameters. |
| Buonocore et al. (2016) [73] | Health benefits (/) | / | / | NB: −USD 2.3–1.7 billion (+) | / |
| Cansino et al. (2019) [62] | Health and social benefits: less accidents (VSL/HCM) | / | / | Benefits exceed costs (no numbers) (+) | / |
| Chen et al. (2015) [39] | Health benefits (VSL) | / | / | BCR: FS: 9.0–25; FR: 25–68 (+) | / |
| Cropper et al. (2017) [63] | Health benefits (VSL) | OWSA | / | CBR: 0.31–18 NB: −USD 95.7–2870 million (+) | The size of the present value of mortality benefits is sensitive to VSL and discount rate. |
| Evans et al. (2021) [40] | Health benefits (VSL) | PSA | / | NB: USD 150 million/year (+) | PSA: 88–97% prob. on cost-eff. |
| Feng et al. (2021) [41] | Health benefits (/) | Mentioned but not reported | / | NB: CNY 289.54–26,234.44 million CBR: 1/4.49 (+) | / |
| Fisk et al. (2017) [43] | Health benefits (/) | / | / | Intervention cost exceeds the economic benefits, but economic benefits of reduced mortality exceed the intervention costs of interventions i1–i3 (+) | / |
| Fisk et al. (2017a) [42,43] | Health benefits (/) | PSA | / | BCR: i1: circa 4. i2: 14–25, i4–i7: 6–13, i8–i9: 74–133 (i3, i8, i9 have the lowest cost/premature mortality) (+) | / |
| Gao et al. (2016) [44] | Health, climate, and economic benefits (HCM, WTP) | Performed but not specified | / | NB: CNY 629.76 billion BCR: 1.10–38.25 (+) | Unit emission reduction costs, unit subsidy, and GDP growth rate are the most sensitive in all scenarios. |
| Giannadaki et al. (2018) [74] | Health benefits (VSL) | Scenario analysis | / | Net economic benefits: (1) 87.9 (2) 65.0 (3) 84.3 (4) 163 (5) 85.3 (+) | / |
| Giannakis et al. (2019) [30] | Health benefits (VSL) | / | / | CBR: (1) 186 (2) 63 (3) 4 (4) 59 (+) | / |
| Guo et al. (2023) [64] | Health and climate benefits (VSL) | OWSA | / | NB: USD 30–156 billion (+) | / |
| Howard et al. (2019) [31] | Health benefits (VSL) | Scenario analysis | / | BCR: (1) 60 (2) 103 (3) 89 (+) | - Dry years: PM10 emissions under more stringent standards increase by 18.5%. - The use of an alternative concentration response function increases mortality by a factor of 2.9–4.9. |
| Irfan et al. (2021) [45] | Health, economic, and climate benefits (VSL) | Scenario analysis | / | BCR: 0.38–4.64 NPV:–PKR 338.161 for different measures (±) | Even in most pessimistic scenario, the BCR is above 1, except for ICS. |
| Jeuland et al. (2016) [32] | Health, private, and social benefits (COI, VSL) | Monte carlo analysis, OWSA | / | Household perspective: all except LPG give +NB, due to high fuel cost Social perspective: significant social benefits (±) | Probability of private (and social) benefits: LPG stoves: 37% (70%); Biomass ICS: 40% (30%); Charcoal ICS: 50% (70%); Electric ICS: 64% (30%). OWSA: time savings and fuel costs have the most impact on net benefits. |
| Kim et al. (2020) [71] | QALYs (utilities) | OWSA Monte Carlo analysis | (1) EUR 1000 (France); EUR 3000 (Italy) (2) 0.04 QALY (France) 0.31 QALY (Italy) | Dominant result (ICER not calculated) (+) | OWSA: relative risk of asthma incidence in France and continuous cost for chronic CVD in Italy. Monte Carlo: 93.8% (Fr), 87.4% (It) were cost- and life-saving; 0.7% (Fr) and 10.1% (It) fell below WTP EUR 46,000; 98.7% (Fr), 96.0% (It) prob of cost-eff. on CEAC with WTP EUR 46,000. |
| Lavee et al. (2018) [65] | Health and other benefits: improved safety, savings on fuel (VSL) | / | / | NB: −ILS 6.6–400 million for different measures (±) | / |
| Levy et al. (2017) [46] | Health benefits (VSL) | / | (1) USD 190,000 (annual) (2) −USD 1.7 million | BCR: 9.7 (+) | / |
| Liu K et al. (2024) [67] | Health benefits (/) | / | / | CBI (deaths/million CNY) (3): 2.9; (5): 4.6; (6): 1.4 | / |
| Liu M. et al. (2019) [75] | Health benefits (/) | / | / | NB: USD 0.4 billion (+) | / |
| Liu Y. et al. (2021) [47] | Health benefits (VSL) | OWSA Monte Carlo analysis | / | NB: C-B: S1: 131; S2: 90; S3: −60; S4: −317 billion CBR: C/B per scenario: S1: 2.6; S2: 1.5; S3: 0.9; S4: 0.6 (±) | / |
| Liu Z et al. (2023) [68] | Health benefits (VSL) | / | / | CBR: NOx-AVOC-A: USD 0.23 trillion in BTH; USD 0.12 trillion in YRD (significant) NOx-AVOC-B: cost-effective regional but less nationwide NOx only: less effective | / |
| Lomas et al. (2016) [14] | QALYs (HRQoL) | / | / | / | / |
| Lopez-Aparicio et al. (2020) [48] | Health benefits (/) | PSA | / | BCR = 1.24 (Scenario 1); 0.79 (Scenario 2) (±) | Conservative or high estimates do not significantly alter the result, but varying the cost of time has the largest effect, with net changes to the results varying by a maximum of 20%. |
| Mardones et al. (2021) [33] | Health benefits (VSL) | Monte Carlo analysis | / | CE (±): (1) CLP 5016/kg PM2.5; (2) CLP 5854/kg PM2.5; (4) ‘Infinite’ CBR: (1) 0.40; (2) 0.47; (4) 0 | - The effects of the replacement program on emissions; - Discount rate; - Dose–response relationships are the most influential parameters. |
| Meng et al. (2023) [34] | Health and climate benefits (VSL) | Monte Carlo analysis | (1) (only in figure): 1. CNY ±6000; 2. ±5800; 3. ±5800; 4. ±1500; 5. ±2000 /household (2) 1, 2, 3. CNY 100; 4. 53; 5. 59 million | BCR (+) (Only reported in figure): 1. ±5 2. ±5 3. ±5 4. ±22 5. ±20 | Sources of uncertainty: Costs: costs of power plants, power grids, natural gas pipelines, household appliances, and fuel Benefits: premature deaths, the value of a statistical life, and the social cost of carbon |
| Meng et al. (2023) [49] | Health benefits (/) | Monte Carlo (but no results reported) + SA on total cost | / | RMB 2.3 million /avoided death (+) | The gas price was the most significant factor that influenced the total cost. |
| Miranda et al. (2016) [50] | Not specified (/) | / | / | HYB: NB = −M EUR 0.5 /y; BKR = 0.75 FIR: NB = M EUR 1.0 /y; BKR = 2.25 LEZ: NB = M EUR 0.001 /y; BKR = 1.03 IND: NB = −M EUR 0.2 /y; BKR = 0.97 HYB + FIR: NB = M EUR 0.5 /y; BKR = 1.18 FIR + IND: NB = M EUR 0.9 /y; BKR = 1.14 HYB + FIR + LEZ + IND: NB = M EUR 0.3 /y; BKR = 1.03 (±) | / |
| Ramirez et al. (2024) [69] | Health, climate, and other benefits: time spent collecting fuel and cooking (VSL) | / | / | 1. Electric Stove: 9563 deaths, USD 1.27B saved/y 2. LPG: 8758 deaths, USD 0.96B saved/y 3. Biogas: 9267 deaths, USD 1.02B saved/y 4. Improved Biomass Cookstoves: 2833 deaths, USD 0.31B saved/y | / |
| Schmitt L.H.M. (2016) [72,80] | QALYs (/) | PSA, Monte Carlo analysis | / | / | / |
| Schucht et al. (2018) [51] | Health benefits (/) | / | / | NB for 48 different measures, both (non-)cost-effective (±) | / |
| Thompson et al. (2016) [52] | Health benefits (VSL) | Monte Carlo analysis | / | NB not specified | / |
| Wagner et al. (2015) [35] | Health, climate, and environmental benefits (VSL) | Performed but not specified | / | BCR: (1) 8.1 (BW), 8.4 (Br) (2)/ (3) 0.8 (poultry), /(pigs) (4) 7.6 (gran), 2.4 (sw. foil), 5.2 (concr. cover) (5) 0.9 (tr. hose), 3.2 (tr. shoe), 3.9 (inject) (6) 4.8 (chem. was), 2.2 (3state-syst), /(biofilter) (+) | The net benefits and GHRs of most measures remained positive even with variations in model parameters (except for biofilters). |
| Wagner et al. (2017) [53] | Health benefits (WTP) | PSA | / | Fl. Shoe: NB: 505 million, BKR: 4.2 Conc Inject: NB: 401 million, BKR: 3.6 (+) | When varying abatement potential, abatement costs, and avoided damage costs, abatement measures were consistently cost-effective. |
| Wan et al. (2023) [54] | Health benefits (VSL) | / | / | Most control measures yield monetised net benefits (no figures) (+) | / |
| Whitehurst et al. (2021) [66] | Health and climate benefits (HEAT) | OWSA | / | CBR: 0.1–4.9 for the different cities (+) | Time horizon, investment cost, and VSL values are the most influential parameters. |
| Wiser et al. (2017) [55] | Health and climate benefits (/) | Not specified | / | / | Not specified |
| Yang et al. (2024) [36] | Health benefits (VSL) | Monte Carlo analysis | (1) / (2) incremental DALY, but no outcomes reported | Different NE and COE in cities of China (no figures but shown on diagram) | / |
| Zhang et al. (2015) [57] | Health benefits (VSL) | Monte Carlo analysis | / | Average net benefit is USD 53.2/MWh for 600 MW generated under multi-pollutant strategies, USD 6.5/MWh higher than graduated pollutant strategy (+) | Capital cost and O&M costs have a small influence; discount rate has the most influence on control costs, and the intake fraction of sulphates and nitrates; and the CRR for total mortality has the greatest influence on health benefits. Health benefits are most sensitive to VSL values. |
| Zhang et al. (2019) [58] | Health and environmental benefits (WTP) | / | / | NB: RMB 818 billion CBR: 1.49 (+) | / |
| Zhang et al. (2020) [37] | Health and climate benefits (VSL) | / | / | / | / |
| Zhang et al. (2023) [56] | Health benefits (HCM) | Monte Carlo analysis | / | NB (+): S1: 184; S2: 275; S3: 301; S4: 203 | / |
| Zhao et al. (2022) [59] | Health benefits (VSL) | / | / | Ratio of economic benefit to government expenditure: 63.7% (+) | / |
| Zhou et al. (2019) [60] | Health and environmental benefits (HCM, COI) | / | / | NB: CNY 20.34 billion CBR: 1:2.49 (+) | / |
| Zhou et al. (2022) [61] | Health and private benefits | / | / | NB: CNY 92.69 CBR: 1:16.97 (+) | / |
| Author (Publication Year) | Outcome (Valuation Outcome) | Sensitivity Analysis | Incremental Costs (1) Incremental Benefits (2) | Results | Results of Sensitivity Analysis |
|---|---|---|---|---|---|
| Amann et al. (2017) [77] | Health, climate, and other benefits (VOLY, VSL) | Monte Carlo analysis | (1) / (2) / | BCR > 14 for lower estimate of mortality BCR > 50 for the higher estimate (+) | Benefits of the actions identified using the GAINS model significantly exceed the costs even under conservative assumptions. |
| Ballinger et al. (2016) [76] | Health benefits (VSL) | PSA | (1) / (2) / | ICER: GBP 441–25.199/QALY BCR: 3–149 For different measures (+) | Most interventions are robust and remain cost-effective under various assumptions and conditions. |
| Holland et al. (2014) [78] | Health and climate benefits (VSL) | Performed but not specified | (1) Incremental costs shown in table in appendix for 2025B1: 222; B2: 1201; B6: 3339; B3: 4628; B4: 4679; MTRF: 47,006b for 2030; B7: 3334; MTRF: 50,681 (2) / | All EU member states achieve net benefits when switching from the CLE to the B3 scenario but not when switching to the MTFR scenario, except in the least-conservative mortality valuation scenario (±) | Lower VOLY has no effect on results. |
| Srinivasan et al. (2018) [79] | Health benefits (VSL) | / | (1) / (2) Avoided mortality/morbidity INR 962.222 crore. | INR 1.36 crore–INR 1.44 crore/life avoided (+) | / |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vandenbulcke, B.; Verhaeghe, N.; Cruycke, L.; Lelie, M.; Simoens, S.; Putman, K. Evaluating the Cost-Effectiveness of Air Pollution Mitigation Strategies: A Systematic Review. Int. J. Environ. Res. Public Health 2025, 22, 926. https://doi.org/10.3390/ijerph22060926
Vandenbulcke B, Verhaeghe N, Cruycke L, Lelie M, Simoens S, Putman K. Evaluating the Cost-Effectiveness of Air Pollution Mitigation Strategies: A Systematic Review. International Journal of Environmental Research and Public Health. 2025; 22(6):926. https://doi.org/10.3390/ijerph22060926
Chicago/Turabian StyleVandenbulcke, Bo, Nick Verhaeghe, Lisa Cruycke, Max Lelie, Steven Simoens, and Koen Putman. 2025. "Evaluating the Cost-Effectiveness of Air Pollution Mitigation Strategies: A Systematic Review" International Journal of Environmental Research and Public Health 22, no. 6: 926. https://doi.org/10.3390/ijerph22060926
APA StyleVandenbulcke, B., Verhaeghe, N., Cruycke, L., Lelie, M., Simoens, S., & Putman, K. (2025). Evaluating the Cost-Effectiveness of Air Pollution Mitigation Strategies: A Systematic Review. International Journal of Environmental Research and Public Health, 22(6), 926. https://doi.org/10.3390/ijerph22060926






