Can an Evidence-Based Mental Health Intervention Indirectly Benefit Caregivers and Peers of Intervention Participants in Rural Sierra Leone?
Abstract
1. Introduction
2. Methods and Materials
2.1. Participants and Setting
2.2. Data Collection Procedures
2.3. The Youth Readiness Intervention (YRI)
2.4. Measures
2.5. Data Analysis Approach
3. Results
3.1. Descriptive Statistics
3.2. Peer Models
3.2.1. Peer Network Correlational Structures
3.2.2. Peer Network Centrality Measures
3.3. Caregiver Models
3.3.1. Caregiver Network Correlational Structure
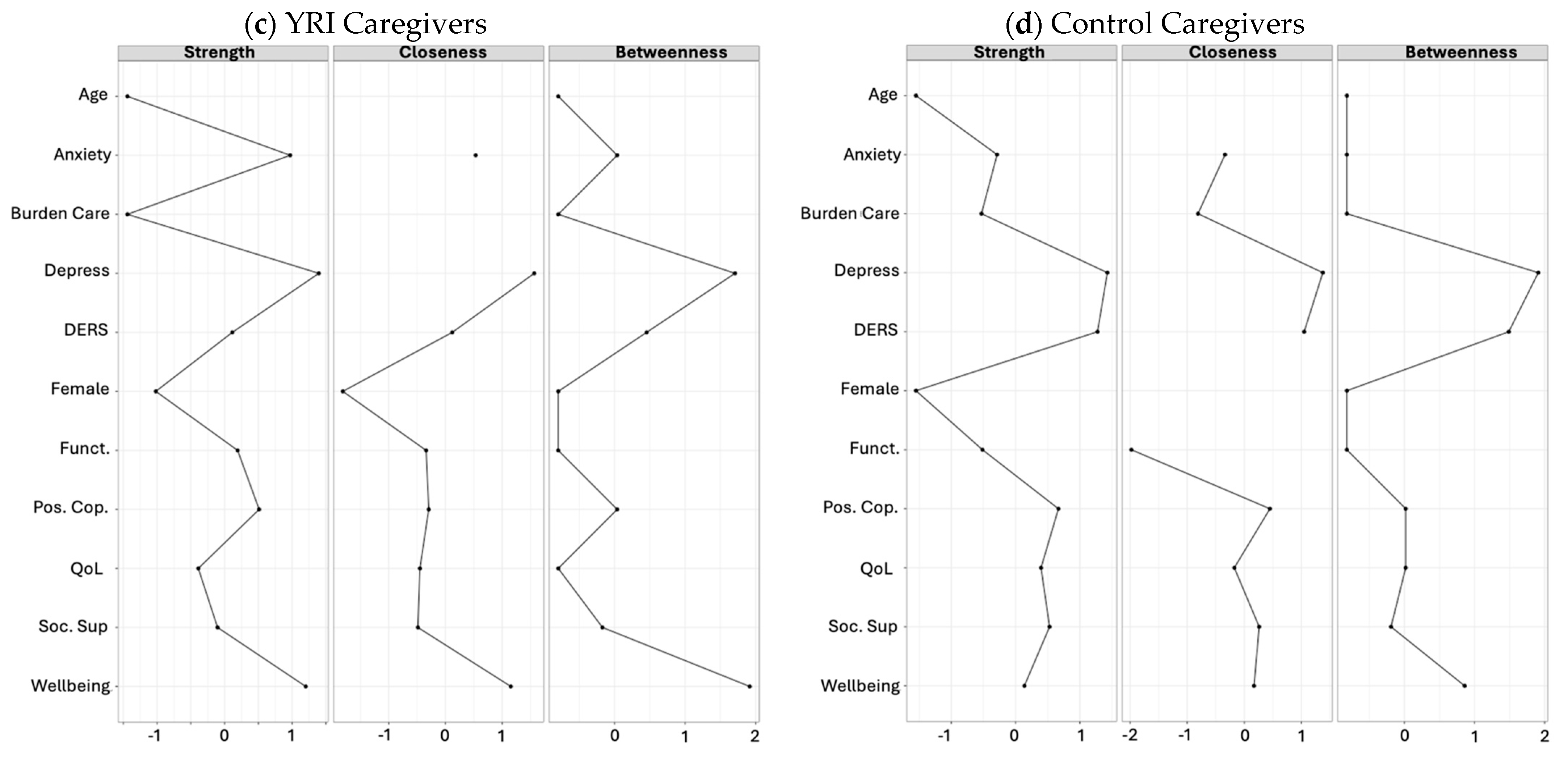
3.3.2. Caregiver Network Centrality Measures
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2019, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Rathod, S.; Pinninti, N.; Irfan, M.; Gorczynski, P.; Rathod, P.; Gega, L.; Naeem, F. Mental health service provision in low- and middle- income countries. Health Serv. Insights. 2017, 10, 1178632917694350. [Google Scholar] [CrossRef] [PubMed]
- Hopwood, H.; Sevalie, S. The burden of mental disorder in Sierra Leone: A retrospective observational evaluation of programmatic data from the roll out of decentralised nurse-led mental health units. Int. J. Ment. Health Syst. 2021, 15, 31. [Google Scholar] [CrossRef] [PubMed]
- Barry, M.M.; Clarke, A.M. A systematic review of the effectiveness of mental health promotion interventions for young people in low-and middle-income countries. BMC Public Health 2013, 13, 835. [Google Scholar] [CrossRef]
- Betancourt, T.S.; McBain, R.; Newnham, E.A.; Akinsulure-Smith, A.M.; Brennan, R.T.; Weisz, J.R.; Hansen, N.B. Behavioral tntervention for war-affected youth in Sierra Leone: A randomized controlled trial. J. Am. Acad. Child. Adolesc. 2014, 53, 1288–1297. [Google Scholar] [CrossRef]
- McMullen, J.; O’Callaghan, P.; Shannon, C.; Black, A.; Eakin, J. Group trauma-focused cognitive-behavioral therapy with former child soldiers and other war-affected boys in the DR Congo: A randomized controlled trial. JCCP 2013, 54, 1231–1241. [Google Scholar]
- Murray, L.K.; Skavenski, S.; Kane, J.C.; Mayeya, J.; Dorsey, S.; Cohen, J.A.; Michalopoulos, L.T.M.; Imaskiu, M.; Bolton, P.A. Effectiveness of trauma-focused cognitive behavioral therapy among trauma-affected children in Lusaka, Zambia. JAMA. Pediatr. 2015, 169, 761–769. [Google Scholar] [CrossRef]
- Al-Janabi, H.; van Exel, J. A Framework for Including Family Health Spillovers in Economic Evaluation. Med. Decis. Mak. 2016, 36, 176–186. [Google Scholar]
- Bobinac, A.; van Exel, N.J.; Rutten, F.F.; Brouwer, W.B. Health effects in significant others: Separating family and care-giving effects. Med. Decis. Making. 2011, 31, 292–298. [Google Scholar] [CrossRef]
- Bobinac, A.; van Exel, N.J.; Rutten, F.F.; Brouwer, W.B. Caring for and caring about: Disentangling the caregiver effect and the family effect. J. Health Econ. 2010, 29, 549–556. [Google Scholar] [CrossRef]
- Price, J.M.; Roesch, S.; Walsh, N.E.; Landsverk, J. Effects of KEEP foster parent intervention on child and sibling behavior problems and parental stress during a randomized implementation trial. Prev. Sci. 2015, 16, 685–695. [Google Scholar] [CrossRef] [PubMed]
- McBain, R.K.; Salhi, C.; Hann, K.; Kellie, J.; Kamara, A.; Salomon, J.A.; Kim, J.J.; Betancourt, T.S. Improving outcomes for caregivers through treatment of young people affected by was: A randomized controlled trial in Sierra Leone. Bull World Health Organ. 2015, 93, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Kim, Y.; Devine, B. Spillover effects of mental health disorders on family members’ health-related quality of life: Evidence from a US sample. Med. Dec. Making. 2022, 42, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Henry, E.; Cullinan, J. Mental health spillovers from serious family illness: Doubly robust estimation using EQ-5D-3L population normative data. Soc. Sci. Med. 2021, 279, 113996. [Google Scholar] [CrossRef]
- Wang, J.; Mann, F.; Lloyd-Evans, B. Associations between loneliness and perceived social support and outcomes of mental health problems: A systematic review. BMC Psychiatry 2018, 18, 156. [Google Scholar] [CrossRef]
- Harandi, T.F.; Taghinasab, M.M. The correlation of social support with mental health: A meta-analysis. Electron. Physician 2017, 9, 5212–5222. [Google Scholar] [CrossRef]
- van der Helm, G.H.P.; Kuiper, C.H.Z. Group climate and treatment motivation in secure residential and forensic youth care from the perspective of self determination theory. Child. Youth Serv. Rev. 2018, 93, 339–344. [Google Scholar] [CrossRef]
- Ashida, S.; Sewell, D.K. Social network members who engage in activities with older adults: Do they bring more social benefits than other members? Ageing Soc. 2018, 39, 1050–1069. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. A self-determination theory approach to psychotherapy: The motivational basis for effective change. Can. Psychol./Psychol. Can. 2018, 49, 186–193. [Google Scholar] [CrossRef]
- Koper, N.; van der Heijden, R.M. The effectiveness of interventions for youth that activate the social network: A meta-analytic study. Appl. Dev. Sci. 2024, 1–25. [Google Scholar] [CrossRef]
- Desrosiers, A.; Bond, L. Exploring Naturalistic Diffusion of an Evidence-Based Mental Health Intervention across Peer Networks of Youth in Sierra Leone. Int. J. Environ. Res. Public Health 2023, 20, 4059. [Google Scholar] [CrossRef]
- Desrosiers, A.; Schafer, C. Exploring potential mental health spillover effects among caregivers and partners of youth in Sierra Leone: A qualitative study. Camb. Prism. Glob. Ment. Health 2023, 10, e40. [Google Scholar] [CrossRef] [PubMed]
- Epskamp, S.; Rhemtulla, M. Generalized Network Psychometrics: Combining Network and Latent Variable Models. Psychometrika 2017, 82, 904–927. [Google Scholar] [CrossRef] [PubMed]
- Cramer, A.O.J.; Waldorp, L.J. Comorbidity: A network perspective. Behav. Brain Sci. 2010, 33, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Van Der Maas, H.L.J.; Dolan, C.V. A dynamical model of general intelligence: The positive manifold of intelligence by mutualism. Psychol. Rev. 2016, 113, 842–861. [Google Scholar] [CrossRef]
- Aldao, A.; Nolen-Hoeksema, S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef]
- Kessler, R.C.; McLeod, J.D. Social support and mental health in community samples. In Social Support and Health; Academic Press: Cambridge, MA, USA, 1985; pp. 219–240. [Google Scholar]
- Gariepy, G.; Honkaniemi, H. Social support and protection from depression: Systematic review of current findings in Western countries. Br. J. Psychiatry 2016, 209, 284–293. [Google Scholar] [CrossRef]
- Reed, R.V.; Fazel, M. Mental health of displaced and refugee children resettled in low-income and middle-income countries: Risk and protective factors. Lancet 2012, 379, 250–265. [Google Scholar] [CrossRef]
- Newnham, E.A.; McBain, R.K.; Hann, K.; Akinsulure-Smith, A.M.; Weisz, J.; Lilienthal, G.M.; Hansen, N.; Betancourt, T.S. The Youth Readiness Intervention for war-affected youth. J. Adolesc. Health 2015, 56, 606–611. [Google Scholar] [CrossRef]
- Gratz, K.L.; Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- World Health Organization. WHO Disability Assessment Schedule (WHODAS) 2.0; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- 33. Betancourt, T.; Newnham, E.; Hann, K.; McBain, R.K.; AkinsulureSmith, A.M.; Weisz, J.; Lilienthal, G.M.; Hansen, N. Addressing the Consequences of Violence and Adversity: The Development of a Group Mental Health Intervention for War-Affected Youth in Sierra Leone. In From Research to Practice in Child and Adolescent Mental Health; Raynaud, J., Gau, S., Hodes, M., Eds.; Rowman & Littlefield: Lanham, MD, USA, 2014; pp. 157–178. [Google Scholar]
- WHO Process of Translation and Adaptation of Instruments. 2012. Available online: https://www.who.int/docs/default-source/publishing-policies/whoqol-100-guidelines/translation-methodology.pdf?sfvrsn=74cdb8f5_2 (accessed on 22 March 2025).
- Derogatis, L.R.; Lipman, R.S.; Rickels, K.; Uhlenhuth, E.H.; Covi, L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behav. Sci. 1974, 19, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S. You want to measure coping but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [PubMed]
- Barrera, M., Jr.; Sandler, I.N.; Ramsay, T.B. Inventory of Socially Supportive Behaviors (ISSB) [Database Record]. APA PsycTests. 1981. Available online: https://psycnet.apa.org/doiLanding?doi=10.1037%2Ft02399-000 (accessed on 22 March 2025).
- Herdman, M.; Gudex, C. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed]
- WHOQOL Group. Development of the World Health Organization. WHOQOL-BREF quality of life assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar] [CrossRef]
- WHO. WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment: Field Trial Version; World Health Organization: Geneva, Switzerland, 1996. [Google Scholar]
- Skevington, S.M.; Lotfy, M. The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual. Life Res. 2004, 13, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Reinhard, S.C.; Gubman, G.D. Burden assessment scale for families of the seriously mentally ill. Eval. Program. Plann. 1994, 17, 261–269. [Google Scholar]
- Borsboom, A.; Cramer, A.O.J. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef]
- Borsboom, D. A network theory of mental disorders. World Psychiatry 2017, 16, 5–13. [Google Scholar]
- Epskamp, S.; Borsboom, D. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef]
- Compare, A.; Zarbo, C. Emotional Regulation and Depression: A Potential Mediator between Heart and Mind. Cardiovasc. Psychiatry Neurol. 2014, 2014, 324374. [Google Scholar] [CrossRef] [PubMed]
- Joormann, J.; Gotlib, I. Emotion Regulation in Depression: Relation to Cognitive Inhibition. Cogn. Emot. 2010, 24, 281–298. [Google Scholar] [CrossRef] [PubMed]
- Freeman, J.A.; Farrar, J.C. Integrating Youth Readiness Intervention and Entrepreneurship in Sierra Leone: A Hybrid Type II Cluster Randomized Trial. J. Am. Acad. Child. Adolesc. Psychiatry 2024, 63, 708–719. [Google Scholar] [CrossRef] [PubMed]
- Dailey, S.F.; Parker, M.M. Social connectedness, mindfulness, and coping as protective factors during the COVID-19 pandemic. J. Couns. Dev. 2022, 101, 114–126. [Google Scholar] [CrossRef] [PubMed]
- Ozbay, F.; Johnson, D.C. Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry 2007, 4, 35–40. [Google Scholar]


| Peers | Caregivers | |||||
|---|---|---|---|---|---|---|
| Control (N = 416) | YRI (N = 440) | Total (N = 856) | Control (N = 141) | YRI (N = 132) | Total (N = 273) | |
| Age | ||||||
| Mean (SD) | 30.99 (9.27) | 30.99 (9.44) | 30.99 (9.36) | 37.50 (12.90) | 37.75 (12.51) | 37.62 (12.69) |
| Range | 16.30–64.00 | 16.50–63.90 | 16.30–64.00 | 17.70–80.00 | 18.70–64.30 | 17.70–80.00 |
| Gender | ||||||
| Female | 171 (41.1%) | 212 (48.2%) | 383 (44.7%) | 84 (59.6%) | 75 (56.8%) | 159 (58.2%) |
| Male | 245 (58.9%) | 228 (51.8%) | 473 (55.3%) | 57 (40.4%) | 57 (43.2%) | 114 (41.8%) |
| District | ||||||
| Kono | 106 (25.5%) | 98 (22.3%) | 204 (23.8%) | 38 (27.0%) | 32 (24.2%) | 70 (25.6%) |
| Koinadugu | 144 (34.6%) | 164 (37.3%) | 308 (36.0%) | 42 (29.8%) | 47 (35.6%) | 89 (32.6%) |
| Kailahun | 166 (39.9%) | 178 (40.5%) | 344 (40.2%) | 61 (43.3%) | 53 (40.2%) | 114 (41.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Desrosiers, A.; Noon, K.; Placencio-Castro, M.; Hansen, N.B.; Moigua, M.; Betancourt, T.S. Can an Evidence-Based Mental Health Intervention Indirectly Benefit Caregivers and Peers of Intervention Participants in Rural Sierra Leone? Int. J. Environ. Res. Public Health 2025, 22, 844. https://doi.org/10.3390/ijerph22060844
Desrosiers A, Noon K, Placencio-Castro M, Hansen NB, Moigua M, Betancourt TS. Can an Evidence-Based Mental Health Intervention Indirectly Benefit Caregivers and Peers of Intervention Participants in Rural Sierra Leone? International Journal of Environmental Research and Public Health. 2025; 22(6):844. https://doi.org/10.3390/ijerph22060844
Chicago/Turabian StyleDesrosiers, Alethea, Kathryn Noon, Matias Placencio-Castro, Nathan B. Hansen, Musu Moigua, and Theresa S. Betancourt. 2025. "Can an Evidence-Based Mental Health Intervention Indirectly Benefit Caregivers and Peers of Intervention Participants in Rural Sierra Leone?" International Journal of Environmental Research and Public Health 22, no. 6: 844. https://doi.org/10.3390/ijerph22060844
APA StyleDesrosiers, A., Noon, K., Placencio-Castro, M., Hansen, N. B., Moigua, M., & Betancourt, T. S. (2025). Can an Evidence-Based Mental Health Intervention Indirectly Benefit Caregivers and Peers of Intervention Participants in Rural Sierra Leone? International Journal of Environmental Research and Public Health, 22(6), 844. https://doi.org/10.3390/ijerph22060844






