Convergent Validity of the Lower Quarter Y Balance Test Against Two-Step and Timed Up and Go Tests in Thai Older Adults with and Without Locomotive Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Considerations
2.3. Participants
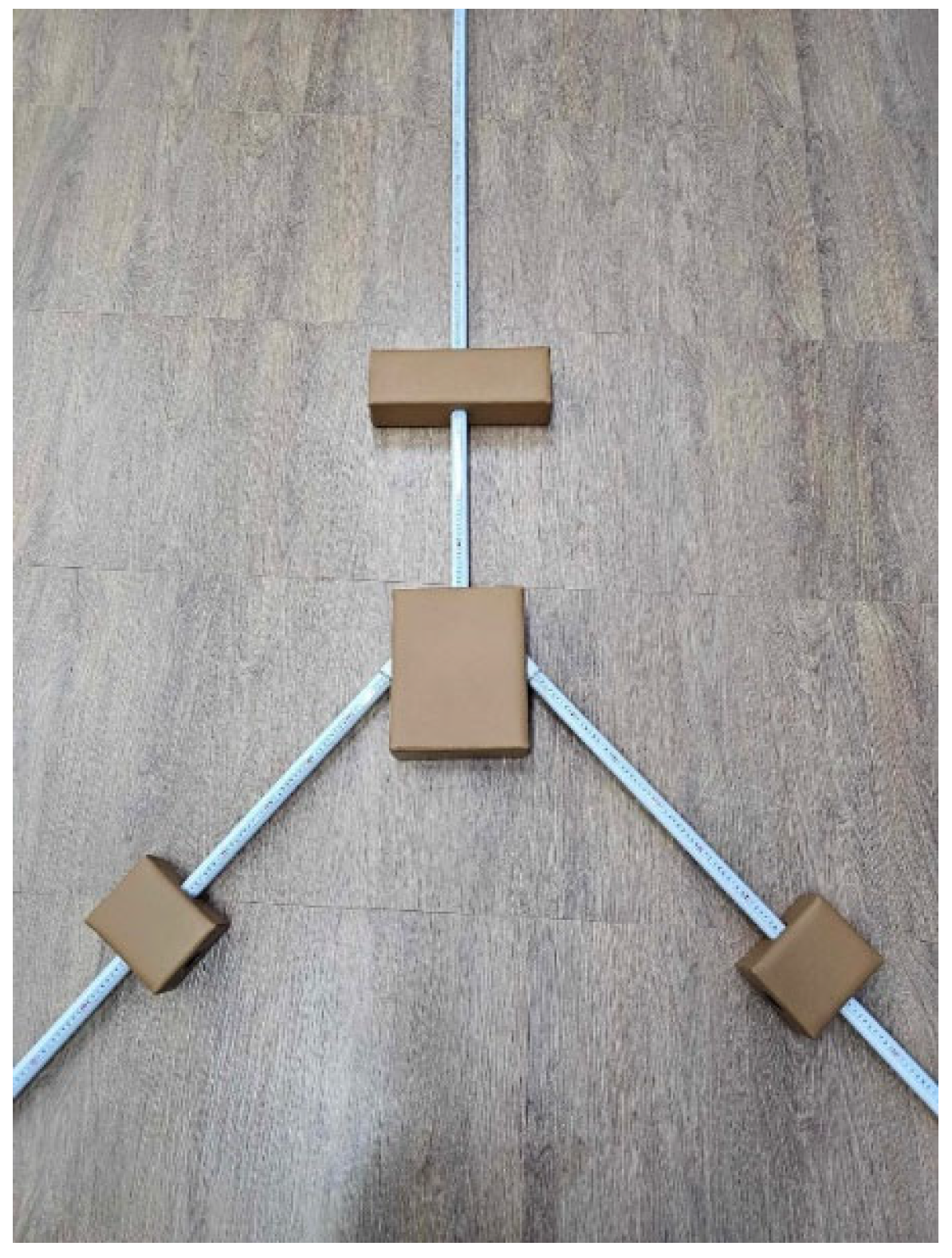
2.4. Tools and Instruments
2.5. Procedure
2.5.1. Baseline Anthropometric Measurements
2.5.2. Two-Step Test
2.5.3. YBT-LQ Test
2.5.4. TUG Test
2.6. Sample Size Calculation
2.7. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Performance Comparisons
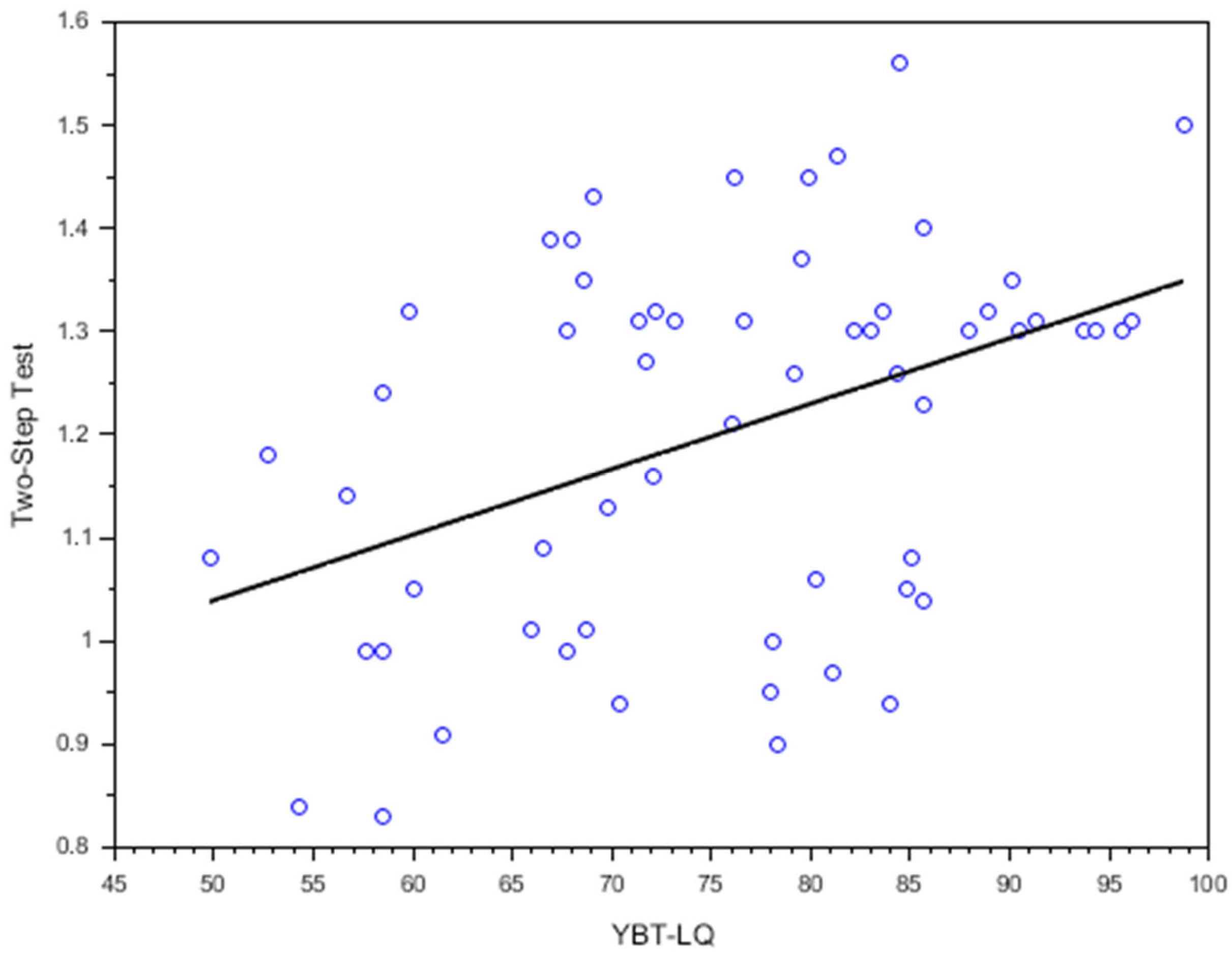
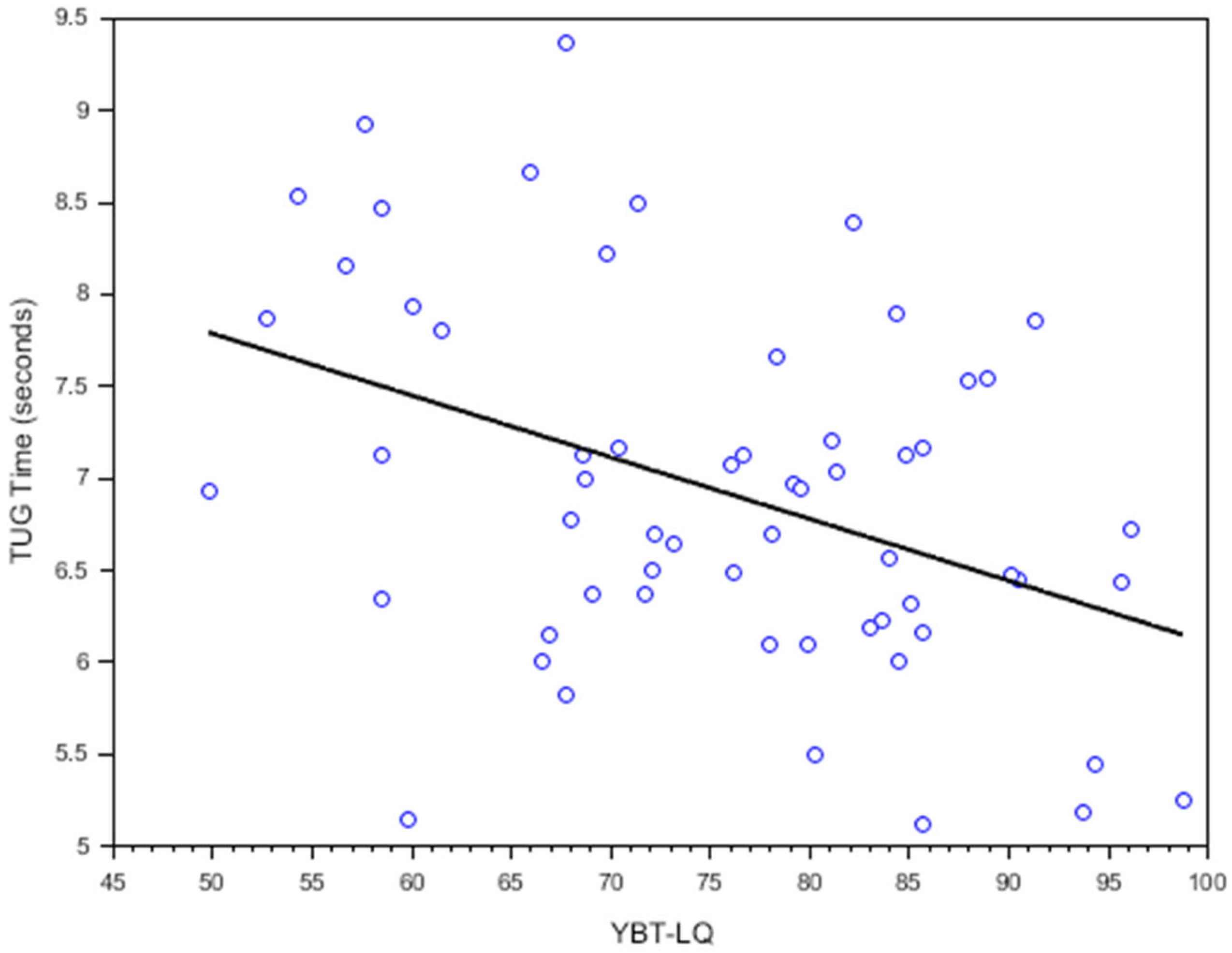
3.3. Correlation Results
3.4. Directional Reach Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| LS | Locomotive Syndrome |
| Non-LS | Non-Locomotive Syndrome |
| TUG | Timed Up and Go |
| YBT-LQ | Y Balance Test Lower Quarter |
References
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2022: Summary of Results; United Nations: New York, NY, USA, 2022; Available online: https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/undesa_pd_2022_wpp_key-messages.pdf (accessed on 25 January 2025).
- Glinskaya, E.; Walker, T.; Wanniarachchi, T. Caring for Thailand’s Aging Population; World Bank: Washington, DC, USA, 2021; Available online: https://documents1.worldbank.org/curated/en/249641622725700707/pdf/Labor-Markets-and-Social-Policy-in-a-Rapidly-Transforming-Caring-for-Thailand-s-Aging-Population.pdf (accessed on 25 January 2025).
- Bherer, L.; Erickson, K.I.; Liu-Ambrose, T. A review of the effects of physical activity and exercise on cognitive and brain functions in older adults. J. Aging Res. 2013, 2013, 657508. [Google Scholar] [CrossRef] [PubMed]
- Verghese, J.; Wang, C.; Lipton, R.B.; Holtzer, R.; Xue, X. Quantitative gait dysfunction and risk of cognitive decline and dementia. J. Neurol. Neurosurg. Psychiatry 2007, 78, 929–935. [Google Scholar] [CrossRef]
- Nakamura, K.; Ogata, T. Locomotive Syndrome: Definition and Management. Clin. Rev. Bone Miner. Metab. 2016, 14, 56–67. [Google Scholar] [CrossRef]
- Yurube, T.; Ito, M.; Takeoka, T.; Watanabe, N.; Inaoka, H.; Kakutani, K.; Kuroda, R.; Nishida, K. Possible Improvement of the Sagittal Spinopelvic Alignment and Balance Through “Locomotion Training” Exercises in Patients with: Locomotive Syndrome”: A Literature Review. Adv. Orthop. 2019, 2019, 6496901. [Google Scholar] [CrossRef]
- Tanaka, S.; Ando, K.; Kobayashi, K.; Hida, T.; Seki, T.; Hamada, T.; Ito, K.; Tsushima, M.; Morozumi, M.; Machino, M.; et al. Increasing Postural Sway in Balance Test Is Related to Locomotive Syndrome Risk: A Cross-Sectional Study. J. Orthop. Sci. 2019, 24, 912–917. [Google Scholar] [CrossRef]
- Nakamura, M.; Hashizume, H.; Nomura, S.; Kono, R.; Utsunomiya, H. The Relationship between Locomotive Syndrome and Depression in Community-Dwelling Elderly People. Curr. Gerontol. Geriatr. Res. 2017, 2017, 4104802. [Google Scholar] [CrossRef]
- Muramoto, A.; Imagama, S.; Ito, Z.; Hirano, K.; Ishiguro, N.; Hasegawa, Y. Physical Performance Tests Are Useful for Evaluating and Monitoring the Severity of Locomotive Syndrome. J. Orthop. Sci. 2012, 17, 782–788. [Google Scholar] [CrossRef]
- Coughlan, G.F.; Fullam, K.; Delahunt, E.; Gissane, C.; Caulfield, B.M. A Comparison between Performance on Selected Directions of the Star Excursion Balance Test and the Y Balance Test. J. Athl. Train. 2012, 47, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Gribble, P.A.; Hertel, J.; Plisky, P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: A literature and systematic review. J. Athl. Train. 2012, 47, 339–357. [Google Scholar] [CrossRef]
- Picot, B.; Terrier, R.; Forestier, N.; Fourchet, F.; McKeon, P.O. The Star Excursion Balance Test: An Update Review and Practical Guidelines. Int. J. Athl. Ther. Train. 2021, 26, 285–293. [Google Scholar] [CrossRef]
- Hubbard, T.J.; Kramer, L.C.; Denegar, C.R.; Hertel, J. Correlations among Multiple Measures of Functional and Mechanical Instability in Subjects with Chronic Ankle Instability. J. Athl. Train. 2007, 42, 361–366. [Google Scholar] [PubMed]
- Sipe, C.L.; Ramey, K.D.; Plisky, P.P.; Taylor, J.D. Y-Balance Test: A Valid and Reliable Assessment in Older Adults. J. Aging Phys. Act. 2019, 27, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.K.; Kang, M.H.; Lee, T.S.; Oh, J.S. Relationships among the Y Balance Test, Berg Balance Scale, and Lower Limb Strength in Middle-Aged and Older Females. Braz. J. Phys. Ther. 2015, 19, 227–234. [Google Scholar] [CrossRef]
- Hirase, T.; Inokuchi, S.; Matsusaka, N.; Okita, M. Effects of a balance training program using a foam rubber pad in community-based older adults: A randomized controlled trial. J. Geriatr. Phys. Ther. 2015, 38, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Rieger, M.M.; Papegaaij, S.; Pijnappels, M.; Steenbrink, F.; van Dieën, J.H. Transfer and retention effects of gait training with anterior-posterior perturbations to postural responses after medio-lateral gait perturbations in older adults. Clin. Biomech. 2020, 75, 104988. [Google Scholar] [CrossRef]
- Lacroix, A.; Kressig, R.W.; Muehlbauer, T.; Gschwind, Y.J.; Pfenninger, B.; Bruegger, O.; Granacher, U. Effects of a supervised versus an unsupervised combined balance and strength training program on balance and muscle power in healthy older adults: A randomized controlled trial. Gerontology 2016, 62, 275–288. [Google Scholar] [CrossRef]
- Kocaman, A.A.; Kırdı, N.; Aksoy, S.; Elmas, Ö.; Dogu, B.B. The effect of different exercise training types on functionality in older fallers: A pilot randomized controlled trial. Top. Geriatr. Rehabil. 2021, 37, 114–127. [Google Scholar] [CrossRef]
- Li, F.; Harmer, P.; Fitzgerald, K.; Eckstrom, E.; Akers, L.; Chou, L.S.; Pidgeon, D.; Voit, J.; Winters-Stone, K. Effectiveness of a therapeutic Tai Ji Quan intervention vs a multimodal exercise intervention to prevent falls among older adults at high risk of falling: A randomized clinical trial. JAMA Intern. Med. 2018, 178, 1301–1310. [Google Scholar] [CrossRef]
- Plisky, P.J.; Gorman, P.P.; Butler, R.J.; Kiesel, K.B.; Underwood, F.B.; Elkins, B. The Reliability of an Instrumented Device for Measuring Components of the Star Excursion Balance Test. N. Am. J. Sports Phys. Ther. 2009, 4, 92–99. [Google Scholar]
- Ishibashi, H. Locomotive syndrome in Japan. Osteoporos. Sarcopenia 2018, 4, 86–94. [Google Scholar] [CrossRef]
- Ahmad, A.A.; Zamani Sani, S.H.; Rezaie, Z.F.; Aghdasi, M.T. Concurrent Validity of Functional Gait Assessment, Timed Up and Go, and Gait Speed Tests in Persian Community-Dwelling Older Adults. Iran. Rehabil. J. 2010, 8, 15–20. [Google Scholar]
- Nicholson, V.; Watts, N.; Chani, Y.; Keogh, J.W.L. Motor imagery training improves balance and mobility outcomes in older adults: A systematic review. J. Physiother. 2019, 65, 200–207. [Google Scholar] [PubMed]
- Wang, Q.; Fu, H. Relationship Between Proprioception and Balance Control Among Chinese Senior Older Adults. Front. Physiol. 2022, 13, 1078087. [Google Scholar] [CrossRef]
- Lee, J.E.; Chun, H.; Kim, Y.S.; Jung, H.W.; Jang, I.Y.; Cha, H.M.; Son, K.Y.; Cho, B.; Kwon, I.S.; Yoon, J.L. Association between Timed Up and Go Test and Subsequent Functional Dependency. J. Korean Med. Sci. 2020, 35, e25. [Google Scholar] [CrossRef]
- Beauchet, O.; Fantino, B.; Allali, G.; Muir, S.W.; Montero-Odasso, M.; Annweiler, C. Timed Up and Go Test and Risk of Falls in Older Adults: A Systematic Review. J. Nutr. Health Aging 2011, 15, 933–938. [Google Scholar] [CrossRef]
- Park, S.H. Tools for Assessing Fall Risk in the Elderly: A Systematic Review and Meta-Analysis. Aging Clin. Exp. Res. 2018, 30, 1–16. [Google Scholar]
- Delahunt, E.; Bleakley, C.M.; Bossard, D.S.; Caulfield, B.M.; Docherty, C.L.; Doherty, C.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; et al. Clinical Assessment of Acute Lateral Ankle Sprain Injuries (ROAST): 2019 Consensus Statement and Recommendations of the International Ankle Consortium. Br. J. Sports Med. 2018, 52, 1304–1310. [Google Scholar] [CrossRef]
- Hubbard, T.J.; Hertel, J.; Sherbondy, P. Fibular position in individuals with self-reported chronic ankle instability. J. Orthop. Sports Phys. Ther. 2006, 36, 3–9. [Google Scholar] [CrossRef]
- Bergamin, M.; Gobbo, S.; Bullo, V.; Zanotto, T.; Vendramin, B.; Duregon, F.; Cugusi, L.; Camozzi, V.; Zaccaria, M.; Neunhaeuserer, D.; et al. Effects of a Pilates Exercise Program on Muscle Strength, Postural Control and Body Composition: Results from a Pilot Study in a Group of Post-Menopausal Women. Age 2015, 37, 118. [Google Scholar] [CrossRef]
- Rezaei, A.; Bhat, S.G.; Cheng, C.H.; Pignolo, R.J.; Lu, L.; Kaufman, K.R. Age-Related Changes in Gait, Balance, and Strength Parameters: A Cross-Sectional Study. PLoS ONE 2024, 19, e0310764. [Google Scholar] [CrossRef]
- Miller, K.J.; Adair, B.S.; Pearce, A.J.; Said, C.M.; Ozanne, E.; Morris, M.M. Effectiveness and Feasibility of Virtual Reality and Gaming System Use at Home by Older Adults for Enabling Physical Activity to Improve Health-Related Domains: A Systematic Review. Age Ageing 2014, 43, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Hrysomallis, C. Relationship Between Balance Ability, Training, and Sports Injury Risk. Sports Med. 2007, 37, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Vaishnavi, G.; Chandralekha, S.; Tharani, G.; Kamatchi, K.; Kirupa, K.; Kamali, R.; Rajasri, R.; Rajavel, R. To Compare the Effectiveness of Balance Training and Conventional Exercises for Elderly Individuals. Res. J. Pharm. Technol. 2021, 14, 1274–1278. [Google Scholar]
- Gobbo, S.; Bergamin, M.; Sieverdes, J.C.; Ermolao, A.; Zaccaria, M. Effects of Exercise on Dual-Task Ability and Balance in Older Adults: A Systematic Review. Arch. Gerontol. Geriatr. 2014, 58, 177–187. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Kumar, C. The Patient Who Falls: “It’s Always a Trade-Off”. JAMA 2010, 303, 258–266. [Google Scholar] [CrossRef]
- Liu, C.J.; Latham, N.K. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst. Rev. 2009, 3, CD002759. [Google Scholar] [CrossRef]
- Granacher, U.; Gollhofer, A.; Hortobágyi, T.; Kressig, R.W.; Muehlbauer, T. The importance of trunk muscle strength for balance, functional performance, and fall prevention in seniors: A systematic review. Sports Med. 2013, 43, 627–641. [Google Scholar] [CrossRef]
- Marigold, D.S.; Eng, J.J.; Dawson, A.S.; Inglis, J.T.; Harris, J.E.; Gylfadottir, S. Exercise leads to faster postural reflexes, improved balance and mobility, and fewer falls in older persons with chronic stroke. J. Am. Geriatr. Soc. 2005, 53, 416–423. [Google Scholar] [CrossRef]
- Topp, R.; Mikesky, A.; Dayhoff, N.E.; Holt, W. Effect of resistance training on strength, postural control, and gait velocity among older adults. Clin. Nurs. Res. 1996, 5, 407–427. [Google Scholar] [CrossRef]
- Lesinski, M.; Hortobágyi, T.; Muehlbauer, T.; Gollhofer, A.; Granacher, U. Effects of balance training on balance performance in healthy older adults: A systematic review and meta-analysis. Sports Med. 2015, 45, 1721–1738. [Google Scholar] [CrossRef]
- Hue, O.; Simoneau, M.; Marcotte, J.; Berrigan, F.; Doré, J.; Marceau, P.; Marceau, S.; Tremblay, A.; Teasdale, N. Body weight is a strong predictor of postural stability. Gait Posture 2007, 26, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Greve, J.; Alonso, A.; Bordini, A.C.; Camanho, G.L. Correlation between body mass index and postural balance. Clinics 2007, 62, 717–720. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.; da Silva, R.A.; de Oliveira, M.R.; Souza, R.D.N.; Borges, R.J.; Vieira, E.R. Effect of body mass index and fat mass on balance force platform measurements during a one-legged stance in older adults. Aging Clin. Exp. Res. 2018, 30, 441–447. [Google Scholar] [CrossRef]
- Huang, A.R.; Mallet, L.; Rochefort, C.M.; Eguale, T.; Buckeridge, D.L.; Tamblyn, R. Medication-related falls in the elderly: Causative factors and preventive strategies. Drugs Aging 2012, 29, 359–376. [Google Scholar] [CrossRef]
- Hammond, T.; Wilson, A. Polypharmacy and falls in the elderly: A literature review. Nurs. Midwifery Stud. 2013, 2, 171–175. [Google Scholar] [CrossRef]
- Hartikainen, S.; Lönnroos, E.; Louhivuori, K. Medication as a risk factor for falls: Critical systematic review. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 1172–1181. [Google Scholar] [CrossRef]
| Characteristics | Non-Locomotive Syndrome (n = 30) | Locomotive Syndrome (n = 30) | p-Value | ||
|---|---|---|---|---|---|
| Mean ± SD | Range | Mean ± SD | Range | ||
| Age (years) | 67.2 ± 4.6 | 61–77 | 69.3 ± 6.2 | 60–87 | 0.156 a |
| Weight (kg) | 60.1 ± 10.4 | 48.0–99.5 | 63.8 ± 12.7 | 40–89 | 0.226 a |
| Height (cm) | 159.7 ± 7.7 | 147–185 | 160.1 ± 10.2 | 143–185 | 0.790 b |
| BMI (kg/m2) | 23.6 ± 4.3 | 17.6–38.9 | 25.5 ± 4.9 | 16.96–35.4 | 0.060 b |
| Two-Step test | 1.3 ± 0.1 | 1.0–1.6 | 1.1 ± 0.1 | 0.8–1.3 | <0.001 *,b |
| TUG test (sec) | 6.6 ± 0.8 | 5.2–8.5 | 7.2 ± 1.0 | 5.1–9.4 | 0.014 *,a |
| YBT-LQ (%) | 81.2 ± 10.4 | 59.8–98.7 | 70.1 ± 11.3 | 49.8–85.7 | <0.001 *,a |
| Two-Step Test | TUG Test | ||
|---|---|---|---|
| YBT-LQ | Correlation coefficient | 0.366 | −0.412 |
| p-value | 0.004 *,a | 0.001 *,b |
| Side | Direction | Non-Locomotive Syndrome | Locomotive Syndrome | p-Value |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Left leg | Anterior | 67.7 ± 6.9 | 59.7 ± 11.4 | 0.002 * |
| Posteromedial | 82.9 ± 11.3 | 71.0 ± 12.4 | <0.001 * | |
| Posterolateral | 85.6 ± 13.4 | 70.1 ± 14.7 | <0.001 * | |
| Right leg | Anterior | 69.2 ± 8.8 | 60.1 ± 8.9 | <0.001 * |
| Posteromedial | 80.8 ± 9.8 | 73.4 ± 12.9 | 0.015 * | |
| Posterolateral | 83.8 ± 13.5 | 72.4 ± 12.7 | 0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rungruangbaiyok, C.; Lektip, C.; Nawarat, J.; Miyake, E.; Aoki, K.; Ohtsuka, H.; Inaba, Y.; Kagaya, Y.; Yaemrattanakul, W. Convergent Validity of the Lower Quarter Y Balance Test Against Two-Step and Timed Up and Go Tests in Thai Older Adults with and Without Locomotive Syndrome. Int. J. Environ. Res. Public Health 2025, 22, 538. https://doi.org/10.3390/ijerph22040538
Rungruangbaiyok C, Lektip C, Nawarat J, Miyake E, Aoki K, Ohtsuka H, Inaba Y, Kagaya Y, Yaemrattanakul W. Convergent Validity of the Lower Quarter Y Balance Test Against Two-Step and Timed Up and Go Tests in Thai Older Adults with and Without Locomotive Syndrome. International Journal of Environmental Research and Public Health. 2025; 22(4):538. https://doi.org/10.3390/ijerph22040538
Chicago/Turabian StyleRungruangbaiyok, Chadapa, Charupa Lektip, Jiraphat Nawarat, Eiji Miyake, Keiichiro Aoki, Hiroyuki Ohtsuka, Yasuko Inaba, Yoshinori Kagaya, and Weeranan Yaemrattanakul. 2025. "Convergent Validity of the Lower Quarter Y Balance Test Against Two-Step and Timed Up and Go Tests in Thai Older Adults with and Without Locomotive Syndrome" International Journal of Environmental Research and Public Health 22, no. 4: 538. https://doi.org/10.3390/ijerph22040538
APA StyleRungruangbaiyok, C., Lektip, C., Nawarat, J., Miyake, E., Aoki, K., Ohtsuka, H., Inaba, Y., Kagaya, Y., & Yaemrattanakul, W. (2025). Convergent Validity of the Lower Quarter Y Balance Test Against Two-Step and Timed Up and Go Tests in Thai Older Adults with and Without Locomotive Syndrome. International Journal of Environmental Research and Public Health, 22(4), 538. https://doi.org/10.3390/ijerph22040538







