Clinical, Economical, and Organizational Impact of Chronic Ischemic Cardiovascular Disease in Italy: Evaluation of 2019 Nationwide Hospital Admissions Data
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Population, and Data Sources
2.2. Statistical Analysis
3. Results
3.1. Hospitalizations
3.2. Economic Impact
3.3. Organizational Impact on Healthcare Facilities
3.4. Gender Inequalities
4. Discussion
4.1. Interpretation and Generalizability
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Komajda, M.; Weidinger, F.; Kerneis, M.; Cosentino, F.; Cremonesi, A.; Ferrari, R.; Kownator, S.; Steg, P.G.; Tavazzi, L.; Valgimigli, M.; et al. EURObservational Research Programme: The Chronic Ischaemic Cardiovascular Disease Registry: Pilot phase (CICD-PILOT). Eur. Heart J. 2016, 37, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Wang, C. The Strengths, Weaknesses, Opportunities, and Threats Analysis of Big Data Analytics in Healthcare. Int. J. Big Data Anal. Healthc. 2019, 4, 1–14. [Google Scholar] [CrossRef]
- Zhou, P.; Li, D.; Li, H.; Fang, H.; Huang, C.; Zhang, Y.; Zhang, H.; Zhao, L.; Zhou, J.; Wang, H.; et al. Distribution of radionuclides in a marine sediment core off the waterspout of the nuclear power plants in Daya Bay, northeastern South China Sea. J. Environ. Radioact. 2015, 145, 102–112. [Google Scholar] [CrossRef]
- Crea, F.; Camici, P.G.; De Caterina, R.; Lanza, G.A. Chronic Ischaemic Heart Disease. In The ESC Textbook of Cardiovascular Medicine; Camm, A.J., Lüscher, T.F., Serruys, P.W., Eds.; Oxford University Press: Oxford, UK, 2009; pp. 597–664. Available online: https://academic.oup.com/book/43686/chapter/366946684 (accessed on 30 January 2025).
- Rao, S.V.; Reynolds, H.R.; Hochman, J.S. Chronic Coronary Disease Guidelines. Circulation 2023, 148, 729–731. Available online: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.123.064623 (accessed on 12 March 2025). [PubMed]
- Siriwardhana, C.; Carrazana, E.; Liow, K.; Chen, J.J. Racial/Ethnic Disparities in the Alzheimer’s Disease Link with Cardio and Cerebrovascular Diseases, Based on Hawaii Medicare Data. J. Alzheimers Dis. Rep. 2023, 7, 1103–1120. [Google Scholar] [CrossRef]
- Welsh, R.C.; Kay, R.; Bainey, K.R. Evaluation and management of chronic kidney disease patients with stable ischemic heart disease. Atherosclerosis 2022, 351, 26–28. [Google Scholar] [CrossRef]
- Nguyen, A.H.; Murrin, E.; Moyo, A.; Sharma, G.; Sullivan, S.A.; Maxwell, G.L.; Kennedy, J.L.W.; Saad, A.F. Ischemic heart disease in pregnancy: A practical approach to management. Am. J. Obstet. Gynecol. MFM 2024, 6, 101295. [Google Scholar] [CrossRef]
- Vrints, C.; Andreotti, F.; Koskinas, K.C.; Rossello, X.; Adamo, M.; Ainslie, J.; Banning, A.P.; Budaj, A.; Buechel, R.R.; Chiariello, G.A.; et al. 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur. Heart J. 2024, 45, 3415–3537. [Google Scholar] [CrossRef]
- Komajda, M.; Cosentino, F.; Ferrari, R.; Kerneis, M.; Kosmachova, E.; Laroche, C.; Maggioni, A.P.; Rittger, H.; Steg, P.G.; Szwed, H.; et al. Profile and treatment of chronic coronary syndromes in European Society of Cardiology member countries: The ESC EORP CICD-LT registry. Eur. J. Prev. Cardiol. 2021, 28, 432–445. [Google Scholar] [CrossRef]
- Stone, P.H.; Libby, P.; Boden, W.E. Fundamental Pathobiology of Coronary Atherosclerosis and Clinical Implications for Chronic Ischemic Heart Disease Management—The Plaque Hypothesis: A Narrative Review. JAMA Cardiol. 2023, 8, 192. [Google Scholar] [CrossRef]
- Lancellotti, P. Acute and chronic coronary artery disease. Acta Cardiol. 2024, 79, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Kerneis, M.; Cosentino, F.; Ferrari, R.; Georges, J.-L.; Kosmachova, E.; Laroche, C.; Maggioni, A.P.; Rittger, H.; Steg, P.G.; Maczynska, J.; et al. Impact of chronic coronary syndromes on cardiovascular hospitalization and mortality: The ESC-EORP CICD-LT registry. Eur. J. Prev. Cardiol. 2022, 29, 1945–1954. [Google Scholar] [CrossRef] [PubMed]
- Ren, Z.; Simons, P.I.H.G.; Wesselius, A.; Stehouwer, C.D.A.; Brouwers, M.C.G.J. Relationship between NAFLD and coronary artery disease: A Mendelian randomization study. Hepatology 2023, 77, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Boden, W.E.; Marzilli, M.; Crea, F.; Mancini, G.B.J.; Weintraub, W.S.; Taqueti, V.R.; Pepine, C.J.; Escaned, J.; Al-Lamee, R.; Gowdak, L.H.W.; et al. Evolving Management Paradigm for Stable Ischemic Heart Disease Patients. J. Am. Coll. Cardiol. 2023, 81, 505–514. [Google Scholar] [CrossRef]
- Chilet-Rosell, E. Gender bias in clinical research, pharmaceutical marketing, and the prescription of drugs. Glob. Health Action 2014, 7, 25484. [Google Scholar] [CrossRef]
- Ferron, R.; Agarwal, G.; Cooper, R.; Munkley, D. The effect of COVID-19 on emergency medical service call volumes and patient acuity: A cross-sectional study in Niagara, Ontario. BMC Emerg. Med. 2021, 21, 39. [Google Scholar] [CrossRef]
- Pietrantonio, F.; Vinci, A.; Rosiello, F.; Alessi, E.; Pascucci, M.; Rainone, M.; Delli Castelli, M.; Ciamei, A.; Montagnese, F.; D’Amico, R.; et al. Green Line Hospital-Territory Study: A Single-Blind Randomized Clinical Trial for Evaluation of Technological Challenges of Continuous Wireless Monitoring in Internal Medicine, Preliminary Results. Int. J. Environ. Res. Public. Health 2021, 18, 10328. [Google Scholar] [CrossRef]
- Kaminsky, L.A.; German, C.; Imboden, M.; Ozemek, C.; Peterman, J.E.; Brubaker, P.H. The importance of healthy lifestyle behaviors in the prevention of cardiovascular disease. Prog. Cardiovasc. Dis. 2022, 70, 8–15. [Google Scholar] [CrossRef]
- Del Buono, M.G.; Moroni, F.; Montone, R.A.; Azzalini, L.; Sanna, T.; Abbate, A. Ischemic Cardiomyopathy and Heart Failure After Acute Myocardial Infarction. Curr. Cardiol. Rep. 2022, 24, 1505–1515. [Google Scholar] [CrossRef]
- Varian, F.L.; Parker, W.A.E.; Fotheringham, J.; Storey, R.F. Treatment inequity in antiplatelet therapy for ischaemic heart disease in patients with advanced chronic kidney disease: Releasing the evidence vacuum. Platelets 2023, 34, 2154330. [Google Scholar] [CrossRef]
- Montelaro, B.M.; Ibrahim, R.; Thames, M.; Mehta, P.K. Optimal Medical Therapy for Stable Ischemic Heart Disease. Med. Clin. N. Am. 2024, 108, 455–468. [Google Scholar] [CrossRef] [PubMed]
- Pietrantonio, F.; Ciamei, A.; Vinci, A.; Ciarambino, T.; Alessi, E.; Pascucci, M.; Delli Castelli, M.; Zito, S.; Sanguedolce, S.; Rainone, M.; et al. Polypharmacy Management in a Gender Perspective: At the Heart of the Problem: Analysis of Major Cardiac Diseases, SARS-CoV-2 Affection and Gender Distribution in a Cohort of Patients in Internal Medicine Ward. Int. J. Environ. Res. Public. Health 2023, 20, 5711. [Google Scholar] [CrossRef]
- Melchiorre, M.; Socci, M.; Quattrini, S.; Lamura, G.; D’Amen, B. Frail Older People Ageing in Place in Italy: Use of Health Services and Relationship with General Practitioner. Int. J. Environ. Res. Public. Health 2022, 19, 9063. [Google Scholar] [CrossRef]
- AGENAS. Report PNE 2020. Ministero della Salute. Available online: https://www.agenas.gov.it/comunicazione/primo-piano/1836-presentazione-programma-nazionale-esiti-2020 (accessed on 30 January 2025).
- Di Bella, E.; Gandullia, L.; Leporatti, L.; Locatelli, W.; Montefiori, M.; Persico, L.; Zanetti, R. Frequent use of emergency departments and chronic conditions in ageing societies: A retrospective analysis based in Italy. Popul. Health Metr. 2020, 18, 29. [Google Scholar] [CrossRef]
- Dufour, I.; Chouinard, M.C.; Dubuc, N.; Beaudin, J.; Lafontaine, S.; Hudon, C. Factors associated with frequent use of emergency-department services in a geriatric population: A systematic review. BMC Geriatr. 2019, 19, 185. [Google Scholar] [CrossRef]
- McDonagh, M.S.; Smith, D.H.; Goddard, M. Measuring appropriate use of acute beds. Health Policy 2000, 53, 157–184. [Google Scholar] [CrossRef]
- Boccardi, V.; Mecocci, P. Intermediate Care in Italy: Addressing the Challenges and Opportunities for Person-Tailored Care. Geriatrics 2023, 8, 59. [Google Scholar] [CrossRef]
- Mehta, L.S.; Beckie, T.M.; DeVon, H.A.; Grines, C.L.; Krumholz, H.M.; Johnson, M.N.; Lindley, K.J.; Vaccarino, V.; Wang, T.Y.; Watson, K.E.; et al. Acute Myocardial Infarction in Women: A Scientific Statement From the American Heart Association. Circulation 2016, 133, 916–947. [Google Scholar] [CrossRef]
- Romeo, B.; Bergami, M.; Cenko, E.; Manfrini, O.; Bugiardini, R. Sex Disparities in Ischemic Heart Disease Mortality in Europe. JACC Adv. 2024, 3, 101252. [Google Scholar] [CrossRef]
- Pietrantonio, F.; Vinci, A.; Maurici, M.; Ciarambino, T.; Galli, B.; Signorini, A.; La Fazia, V.M.; Rosselli, F.; Fortunato, L.; Iodice, R.; et al. Intra- and Extra-Hospitalization Monitoring of Vital Signs—Two Sides of the Same Coin: Perspectives from LIMS and Greenline-HT Study Operators. Sensors 2023, 23, 5408. [Google Scholar] [CrossRef]
- Pietrantonio, F.; Piasini, L.; Spandonaro, F. Internal Medicine and emergency admissions: From a national Hospital Discharge Records (SDO) study to a regional analysis. Ital. J. Med. 2016, 10, 157–167. Available online: https://www.italjmed.org/ijm/article/view/itjm.2016.674 (accessed on 12 March 2025). [CrossRef]
- Vinci, A.; Furia, G.; Cammalleri, V.; Colamesta, V.; Chierchini, P.; Corrado, O.; Mammarella, A.; Ingravalle, F.; Bardhi, D.; Malerba, R.M.; et al. Burden of delayed discharge on acute hospital medical wards: A retrospective ecological study in Rome, Italy. PLoS ONE 2024, 19, e0294785. [Google Scholar] [CrossRef]
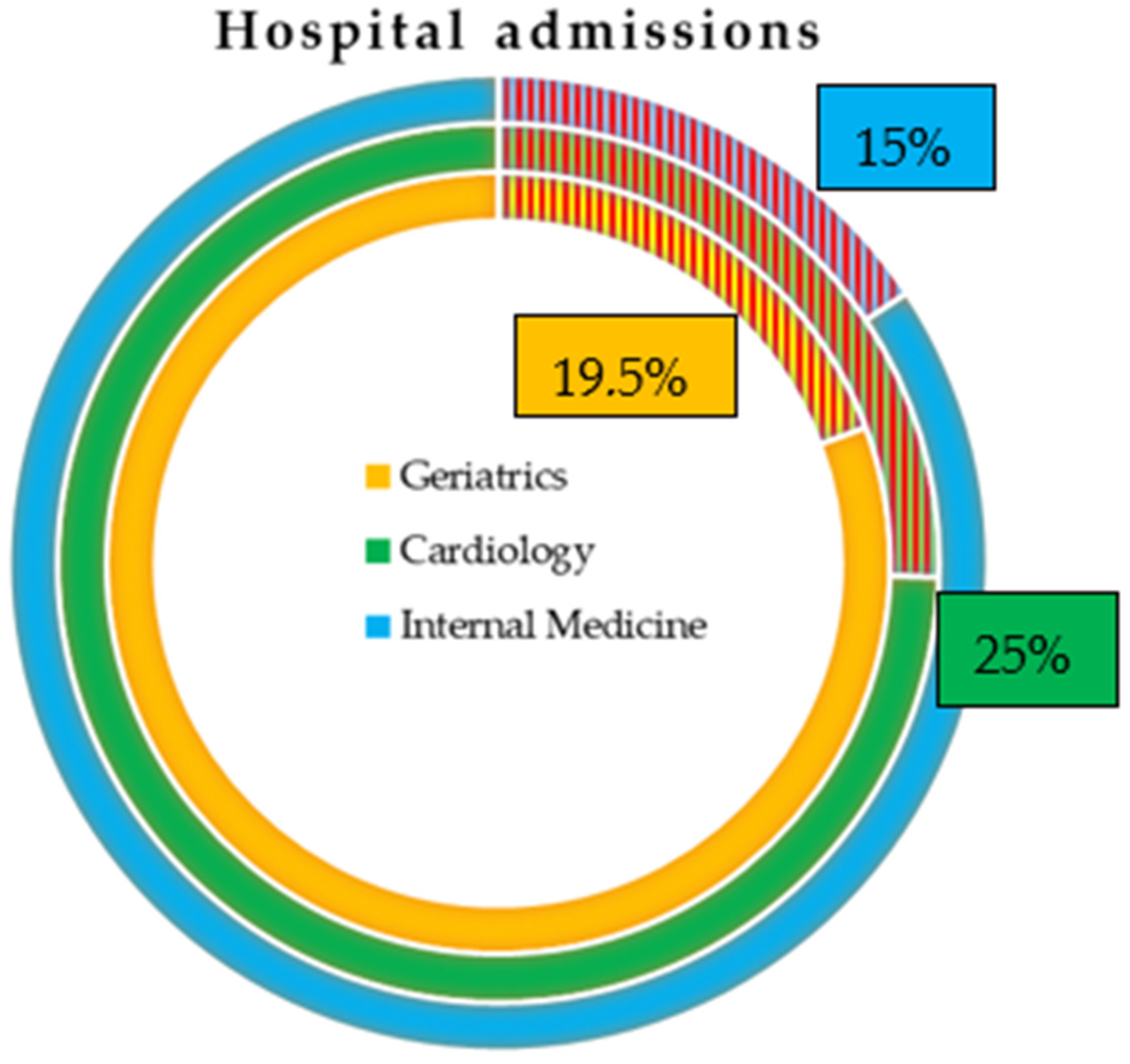
| Ward Type | Diagnosis | Total Admissions | Hospitalization Days | Avg. LOS | Avg. Age |
|---|---|---|---|---|---|
| Internal Medicine | CICD | 157,417 (15.7%) | 1,647,065 | 10.5 | 80.9 |
| Principal Diagnosis | 45,680 (4.6%) | 449,205 | 9.8 | 81.8 | |
| Secondary Diagnosis | 111,737 (11.1%) | 1,197,860 | 10.7 | 80.5 | |
| No CICD | 845,898 (84.3%) | 8,356,767 | 9.9 | 73.5 | |
| Cardiology | CICD | 118,296 (25.5%) | 806,981 | 6.8 | 71.7 |
| Principal Diagnosis | 56,443 (12.2%) | 334,730 | 9.8 | 70.8 | |
| Secondary Diagnosis | 61,853 (13.3%) | 472,251 | 7.6 | 72.5 | |
| No CICD | 345,208 (74.5%) | 1,911,783 | 5.5 | 68.1 | |
| Geriatrics | CICD | 24,523 (19.4%) | 279,525 | 11.4 | 85.3 |
| Principal Diagnosis | 7271 (5.7%) | 78,469 | 10.8 | 85.7 | |
| Secondary Diagnosis | 17,252 (13.6%) | 201,056 | 11.7 | 85.0 | |
| No CICD | 102,104 (80.6%) | 1,404,724 | 13.8 | 84.2 |
| Ward Type | Diagnosis | Total Costs (EUR) | Avg. Admission Cost |
|---|---|---|---|
| Internal Medicine | CICD | 555,264,058 (15.8%) | 3527.34 |
| Principal Diagnosis | 143,962,563 (4.1%) | 3151.54 | |
| Secondary Diagnosis | 411,301,495 (11.7%) | 3680.98 | |
| No CICD | 2,961,718,113 (84.2%) | 3501.27 | |
| TOTAL | 3,516,982,171 (84.5%) | 3505.36 | |
| Cardiology | CICD | 681,416,923 (27.8%) | 5760.27 |
| Principal Diagnosis | 301,869,561 (12.3%) | 5348.22 | |
| Secondary Diagnosis | 379,547,362 (15.5%) | 6136.28 | |
| No CICD | 1,766,179,940 (72.2%) | 5116.28 | |
| TOTAL | 2,447,596,863 (52.9%) | 5280.64 | |
| Geriatrics | CICD | 89,282,223 (19.3%) | 3640.75 |
| Principal Diagnosis | 23,340,960 (5.0%) | 3210.14 | |
| Secondary Diagnosis | 65,941,263 (14.3%) | 3822.24 | |
| No CICD | 372,958,862 (80.7%) | 3652.73 | |
| TOTAL | 462,241,085 | 3650.41 |
| Internal Medicine Wards | ||
|---|---|---|
| Primary Diagnosis (p-Value) | Secondary Diagnosis (p-Value) | |
| CICD vs. No CICD | 372.6 (<0.0001) | 195.4 (<0.0001) |
| Cardiology wards | ||
| Primary diagnosis | Secondary diagnosis | |
| CICD vs. No CICD | 92.4 (<0.0001) | 981.9 (<0.0001) |
| Geriatric wards | ||
| Primary diagnosis | Secondary diagnosis | |
| CICD vs. No CICD | 467.1 (<0.0001) | 198.9 (<0.0001) |
| Internal Medicine Wards—CICD as Primary Diagnosis | |||||||
|---|---|---|---|---|---|---|---|
| Total | Males | Females | |||||
| Subtotal | 65 Years | >65 | Subtotal | 65 Years | >65 Years | ||
| Admissions | 45,609 | 21,490 | 2025 | 19,465 | 24,119 | 905 | 23,214 |
| Admissions cost | 143,744,870 | 68,081,073 | 6,547,729 | 61,533,344 | 75,663,797 | 2,872,865 | 72,790,932 |
| Avg. admission cost | 3151.7 | 3168.0 | 3233.4 | 3161.2 | 3137.1 | 3174.4 | 3135.6 |
| Hospitalization days | 448,471 | 205,835 | 16,842 | 188,993 | 242,636 | 8865 | 233,771 |
| Avg. length of stay | 9.8 | 9.6 | 8.3 | 9.7 | 10.1 | 9.8 | 10.1 |
| Avg. n° of diagnoses | 3.8 | 3.8 | 3.6 | 3.8 | 3.8 | 3.8 | 3.8 |
| Internal Medicine Wards—CICD as Secondary Diagnosis | |||||||
| Admissions | 111,690 | 62,382 | 6727 | 55,655 | 49,308 | 2266 | 47,042 |
| Admissions cost | 411,131,752 | 229,293,826 | 24,476,707 | 204,817,119 | 181,837,926 | 8,420,155 | 173,417,771 |
| Avg. admission cost | 3681.0 | 3675.6 | 3638.6 | 3680.1 | 3687.8 | 3715.9 | 3686.4 |
| Hospitalization days | 1,197,309 | 651,929 | 65,673 | 586,256 | 545,380 | 24,647 | 520,733 |
| Avg. length of stay | 10.7 | 10.5 | 9.8 | 10.5 | 11.1 | 10.9 | 11.1 |
| Avg. n° of diagnoses | 4.6 | 4.6 | 4.4 | 4.7 | 4.6 | 4.6 | 4.6 |
| Cardiology Wards—CICD as Primary Diagnosis | |||||||
| Total | Males | Females | |||||
| Subtotal | 65 years | ≤65 years | Subtotal | ≤65 years | >65 years | ||
| Admissions | 56,443 | 39,318 | 13,326 | 25,992 | 17,125 | 3617 | 13,508 |
| Admissions cost | 301,869,561 | 221,300,664 | 76,700,473 | 144,600,191 | 80,568,897 | 18,337,969 | 62,230,928 |
| Avg. admission cost | 5348.2 | 5628.5 | 5755.7 | 5563.3 | 4704.8 | 5069.9 | 4607.0 |
| Hospitalization days | 334,730 | 218,182 | 63,269 | 154,913 | 116,548 | 19,279 | 97,269 |
| Avg. length of stay | 5.9 | 5.5 | 4.7 | 6.0 | 6.8 | 5.3 | 7.2 |
| Avg. n° of diagnoses | 3.0 | 2.9 | 2.6 | 3.0 | 3.1 | 2.6 | 3.3 |
| Cardiology Wards—CICD as Secondary Diagnosis | |||||||
| Admissions | 61,853 | 44,501 | 12,399 | 32,102 | 17,352 | 2967 | 14,385 |
| Admissions cost | 379,547,362 | 279,212,720 | 79,037,497 | 200,175,223 | 100,334,642 | 17,535,073 | 82,799,569 |
| Avg. admission cost | 6136.3 | 6274.3 | 6374.5 | 6235.6 | 5782.3 | 5910.0 | 5756.0 |
| Hospitalization days | 472,251 | 328,313 | 84,678 | 243,635 | 143,938 | 21,882 | 122,056 |
| Avg. length of stay | 7.6 | 7.4 | 6.8 | 7.6 | 8.3 | 7.4 | 8.5 |
| Avg. n° of diagnoses | 4.1 | 4.1 | 3.8 | 4.2 | 4.2 | 3.8 | 4.3 |
| Geriatrics Wards—CICD as Primary Diagnosis | |||||||
| Total | Males | Females | |||||
| Subtotal | 65 years | >65 | Subtotal | 65 years | >65 years | ||
| Admissions | 7271 | 3054 | 38 | 3016 | 4217 | 17 | 4200 |
| Admissions cost | 23,340,960 | 9,930,304 | 140,933 | 9,789,371 | 13,410,656 | 71,125 | 13,339,531 |
| Avg. admission cost | 3210.1 | 3251.6 | 3708.8 | 3245.8 | 3180.1 | 4183.8 | 3176.1 |
| Hospitalization days | 78,469 | 32,749 | 327 | 32,422 | 45,720 | 174 | 45,546 |
| Avg. length of stay | 10.8 | 10.7 | 8.6 | 10.8 | 10.8 | 10.2 | 10.8 |
| Avg. n° of diagnoses | 3.9 | 3.9 | 4.8 | 3.9 | 3.9 | 4.2 | 3.9 |
| Geriatrics Wards—CICD as Secondary Diagnosis | |||||||
| Admissions | 17,252 | 8517 | 113 | 8404 | 8735 | 42 | 8693 |
| Admissions cost | 65,941,263 | 32,606,182 | 477,108 | 32,129,074 | 33,335,081 | 148,856 | 33,186,225 |
| Avg. admission cost | 3822.2 | 3828.4 | 4222.2 | 3823.1 | 3816.3 | 3544.2 | 3817.6 |
| Hospitalization days | 201,056 | 97,570 | 1095 | 96,475 | 103,486 | 356 | 103,130 |
| Avg. length of stay | 11.7 | 11.5 | 9.7 | 11.5 | 11.8 | 8.5 | 11.9 |
| Avg. n° of diagnoses | 4.8 | 4.8 | 4.8 | 4.8 | 4.8 | 4.6 | 4.8 |
| Internal Medicine Wards—CICD as Primary Diagnosis | ||
|---|---|---|
| Average Costs Difference (p-Value) | Average Length of Stay Difference (p-Value) | |
| Males 65 years vs. Males > 65 | 72.2 (0.010) | 1.4 (<0.0001) |
| Females 65 years vs. Females > 65 | 38.8 (0.167) | 0.3 (0.249) |
| Males 65 years vs. Females 65 years | 59.0 (0.448) | 1.5 (<0.0001) |
| Males > 65 vs. Females > 65 | 25.6 (0.004) | 0.4 (<0.0001) |
| Males vs. Females | 30.9 (0.001) | 0.5 (<0.0001) |
| Internal Medicine wards—CICD as secondary diagnosis | ||
| Males 65 years vs. Males > 65 | 41.5 (0.110) | 0.8 (<0.0001) |
| Females 65 years vs. Females > 65 | 29.4 (0.458) | 0.2 (0.306) |
| Males 65 years vs. Females 65 years | 77.3 (0.204) | 1.1 (<0.0001) |
| Males > 65 vs. Females > 65 | 6.3 (0.591) | 0.5 (<0.0001) |
| Males vs. Females | 12.2 (0.298) | 0.6 (<0.0001) |
| Cardiology wards—CICD as primary diagnosis | ||
| Costs | Hospitalization days | |
| Males 65 years vs. Males > 65 | 197.6 (<0.0001) | 1.2 (<0.0001) |
| Females 65 years vs. Females > 65 | 468.6 (<0.0001) | 1.9 (<0.0001) |
| Males 65 years vs. Females 65 years | 692.2 (<0.0001) | 0.6 (<0.0001) |
| Males > 65 vs. Females > 65 | 963.2 (<0.0001) | 1.2 (<0.0001) |
| Males vs. Females | 931.2 (<0.0001) | 1.3 (<0.0001) |
| Cardiology wards—CICD as secondary diagnosis | ||
| Males 65 years vs. Males > 65 | 138.9 (0.025) | 0.8 (<0.0001) |
| Females 65 years vs. Females > 65 | 154.1 (0.206) | 1.1 (<0.0001) |
| Males 65 years vs. Females 65 years | 464.5 (<0.0001) | 0.5 (<0.0002) |
| Males > 65 vs. Females > 65 | 479.6 (<0.0001) | 0.9 (<0.0001) |
| Males vs. Females | 492.0 (<0.0001) | 0.9 (<0.0001) |
| Geriatrics wards—CICD as primary diagnosis | ||
| Costs | Hospitalization days | |
| Males 65 years vs. Males > 65 | 463.0 (0.243) | 2.1 (0.010) |
| Females 65 years vs. Females > 65 | 1007.7 (0.215) | 0.6 (0.735) |
| Males 65 years vs. Females 65 years | 475.1 (0.546) | 1.6 (0.314) |
| Males > 65 vs. Females > 65 | 69.7 (0.001) | 0.1 (0.600) |
| Males vs. Females | 71.4 (<0.0001) | 0.1 (0.508) |
| Geriatrics wards—CICD as secondary diagnosis | ||
| Males 65 years vs. Males > 65 | 399.1 (0.399) | 1.8 (0.034) |
| Females 65 years vs. Females > 65 | 273.4 (0.581) | 3.4 (0.010) |
| Males 65 years vs. Females 65 years | 678.0 (0.415) | 1.2 (0.427) |
| Males > 65 vs. Females > 65 | 5.5 (0.861) | 0.4 (0.004) |
| Males vs. Females | 12.1 (0.702) | 0.4 (0.003) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pietrantonio, F.; Carrieri, C.; Rosiello, F.; Spandonaro, F.; Vinci, A.; d’Angela, D. Clinical, Economical, and Organizational Impact of Chronic Ischemic Cardiovascular Disease in Italy: Evaluation of 2019 Nationwide Hospital Admissions Data. Int. J. Environ. Res. Public Health 2025, 22, 530. https://doi.org/10.3390/ijerph22040530
Pietrantonio F, Carrieri C, Rosiello F, Spandonaro F, Vinci A, d’Angela D. Clinical, Economical, and Organizational Impact of Chronic Ischemic Cardiovascular Disease in Italy: Evaluation of 2019 Nationwide Hospital Admissions Data. International Journal of Environmental Research and Public Health. 2025; 22(4):530. https://doi.org/10.3390/ijerph22040530
Chicago/Turabian StylePietrantonio, Filomena, Ciro Carrieri, Francesco Rosiello, Federico Spandonaro, Antonio Vinci, and Daniela d’Angela. 2025. "Clinical, Economical, and Organizational Impact of Chronic Ischemic Cardiovascular Disease in Italy: Evaluation of 2019 Nationwide Hospital Admissions Data" International Journal of Environmental Research and Public Health 22, no. 4: 530. https://doi.org/10.3390/ijerph22040530
APA StylePietrantonio, F., Carrieri, C., Rosiello, F., Spandonaro, F., Vinci, A., & d’Angela, D. (2025). Clinical, Economical, and Organizational Impact of Chronic Ischemic Cardiovascular Disease in Italy: Evaluation of 2019 Nationwide Hospital Admissions Data. International Journal of Environmental Research and Public Health, 22(4), 530. https://doi.org/10.3390/ijerph22040530








