Unpacking Post-Traumatic Stress Disorder and Mental Health in Internally Displaced Persons: A Mediation-Moderation Model of Psychological Capital and Perceived Social Support
Abstract
1. Introduction
1.1. The Relationship Between PTSD and MH Among IDPs
1.2. The Relationship Between PTSD and PSS Among IDPs
1.3. Moderating Role of PSS in the Relationship Between PTSD and MH
1.4. The Mediation Role of PsyCap in the Relationship Between PTSD and MH
2. Methods
2.1. Participants and Setting
2.2. Procedures and Ethics
2.3. Instrumentation
2.4. PTSD (PCL-C)
2.5. Psychological Capital Scale
2.6. General Health Questionnaire
2.7. The Interpersonal Support Evaluation List (ISEL)
2.8. Data Analysis
3. Results
3.1. Descriptive Statistics
3.2. Construct Reliability and Validity Measures
3.3. Measurement Model Fit Analysis of the Variables
3.4. Hypothesis Tests for the Proposed Structural Model
3.5. Structural Model Fit Assessment
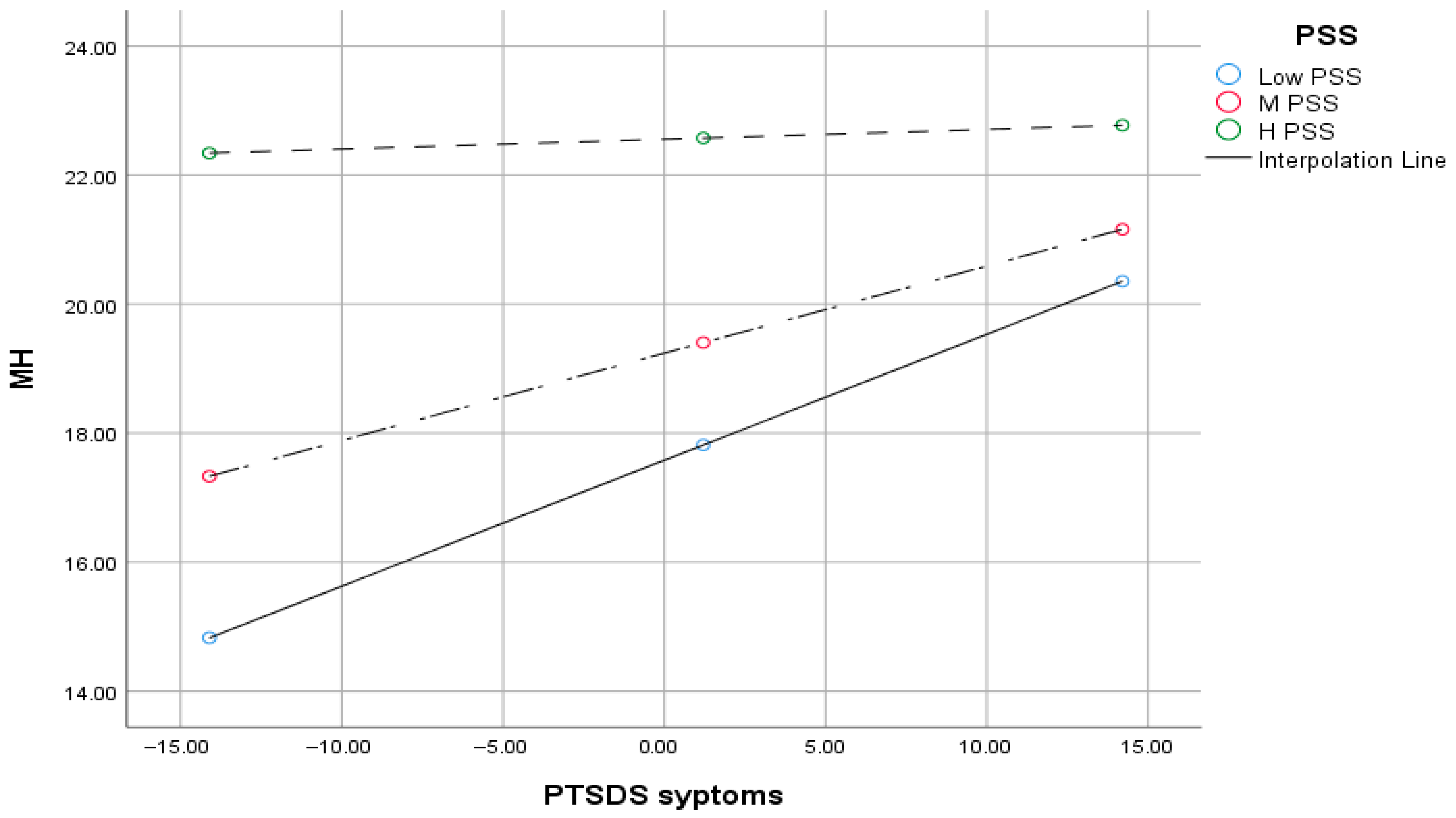
3.6. Moderation Effect of PSS in the Relationship Between PTSD and MH
3.7. Conditional Effects of PTSD on MH at Levels of PSS
4. Discussion
5. Summary, Conclusions, and Recommendations
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Idmc, N. Global Report on Internal Displacement 2019; Internal Displacement Monitoring Centre (IDMC): Geneva, Switzerland, 2019. [Google Scholar]
- Oh, W.; Muneepeerakul, R.; Rubenstein, D.; Levin, S. Emergent network patterns of internal displacement in Somalia driven by natural disasters and conflicts. Glob. Environ. Change 2024, 84, 102793. [Google Scholar] [CrossRef]
- Amna Adrees, M. Refugees: The Past, Present, and Future; (MS4, MPH) (Student Paper); Department of Family Medicine, University of Virginia: Charlottesville, VA, USA, 2022. [Google Scholar]
- Sönmez, D.; Hocaoglu, C. Post-traumatic stress disorder after natural disasters: A review. Duzce Med. J. 2023, 25, 103–114. [Google Scholar] [CrossRef]
- Yigzaw, G.S.; Abitew, E.B. Causes and impacts of internal displacement in Ethiopia. Afr. J. Soc. Work 2019, 9, 32–41. [Google Scholar]
- Madoro, D.; Kerebih, H.; Habtamu, Y.; Tsadik, M.; Mokona, H.; Molla, A.; Wondie, T.; Yohannes, K. Post-traumatic stress disorder and associated factors among internally displaced people in South Ethiopia: A cross-sectional study. Neuropsychiatr. Dis. Treat. 2020, 16, 2317–2326. [Google Scholar] [CrossRef] [PubMed]
- Nwosu, C.P.; Okafor, F.-C.N. United Nations High Commissioner for Refugees (UNHCR) and Management of Refugee Crisis in the Nigerian Section of Lake Chad Basin (2011–2023). Nnamdi Azikiwe J. Political Sci. 2024, 9, 174–190. [Google Scholar]
- Ghafoori, N.; Meng, C.; Yolchi, J. Internal Displacement and Sustainable Development Goals. Sustain. Dev. 2025, 33, 7876–7894. [Google Scholar] [CrossRef]
- Naseer, M.Z.; Muhib, K.; Mustafa, Z.; Shamsuddin, S. Refugee Crises and International Response Policy and Humanitarian Perspectives. J. Soc. Signs Rev. 2025, 3, 109–119. [Google Scholar]
- Council, N.R. Internal Displacement Monitoring Centre-IDMC. Glob. Rep. Intern. Displac. Accessed August 2019, 10, 2020. [Google Scholar]
- IDMC. Global Report on Internal Displacement; International Displacement Monitoring Centre/Norwegian Refugee Council: Geneva, Switzerland, 2020. [Google Scholar]
- McAuliffe, M.; Ruhs, M. World Migration Report 2018; International Organization for Migration: Geneva, Switzerland, 2017; pp. 1–32. [Google Scholar]
- Mamed, G.E.; Tefera, G.M.; Bitew, M.; Yu, M. The overlooked war in Northern Ethiopia: Examining psychological capital, mental distress, and post-traumatic stress disorder among internally displaced people in Amhara region. Int. J. Soc. Psychiatry 2024, 71, 705–714. [Google Scholar] [CrossRef]
- Owoaje, E.T.; Uchendu, O.C.; Ajayi, T.; Cadmus, E. A review of the health problems of the internally displaced persons in Africa. Niger. Postgrad. Med. J. 2016, 23, 161–171. [Google Scholar] [CrossRef]
- Bayu, E.K.; Sunjo, E. An assessment of conflict-induced internal displacement trends and situations of idps in Ethiopia. EPH Int. J. Humanit. Soc. Sci. 2023, 8, 47–66. [Google Scholar] [CrossRef]
- Easton-Calabria, E.; Ahmed, A.; Mohamed, D.; Singh, A. Anticipatory Action in Complex Crises: Lessons from Ethiopia; Feinstein International Center, Tufts University: Medford, MA, USA, 2023; 27p. [Google Scholar]
- Bekele, B. Reimagining Shelter: Design Solution for Internally Displaced Persons. Undergraduate Thesis, Adama Science and Technology University, Adama, Ethiopia, 2024. [Google Scholar]
- Miller, K.E.; Rasmussen, A. War exposure, daily stressors, and mental health 15 years on: Implications of an ecological framework for addressing the mental health of conflict-affected populations. Epidemiology Psychiatr. Sci. 2024, 33, e78. [Google Scholar] [CrossRef] [PubMed]
- Orendain, D.J.A.; Djalante, R. Ignored and invisible: Internally displaced persons (IDPs) in the face of COVID-19 pandemic. Sustain. Sci. 2020, 16, 337–340. [Google Scholar] [CrossRef] [PubMed]
- Oginni, S.O.; Opoku, M.P.; Alupo, B.A. Terrorism in the Lake Chad region: Integration of refugees and internally displaced persons. J. Borderl. Stud. 2020, 35, 725–741. [Google Scholar] [CrossRef]
- Tassang, A.E.; Guoqing, S.; Akintunde, T.Y.; Sayibu, M.; Isangha, S.O.; Adedeji, A.; Musa, T.H. Social integration, solidarity, and psychological health of internally displaced persons in Cameroon: Exploring the role of community satisfaction. Heliyon 2023, 9, e20361. [Google Scholar] [CrossRef]
- Akuto, G. Challenges of internally displaced persons (IDPs) in Nigeria: Implications for counselling and the role of key stakeholders. Int. J. Innov. Psychol. Soc. Dev. 2017, 5, 21–27. [Google Scholar]
- Workneh, A.F. The State of Knowledge on Posttraumatic Stress Disorder, Depression and Anxiety among Refugee Women in Africa: A Scoping Review. Master’s Thesis, Université d’Ottawa/University of Ottawa, Ottawa, ON, Canada, 2017. [Google Scholar]
- Ugbe, U.M.-J.; Esu, E.B.; Efut, J.A.; Bisongedam, M.M.; Awa, T.M.; Ekpo, O.I. Sociodemographic correlates and associated factors of depression and anxiety among internally displaced adults in Ogoja, Nigeria. Gen. Psychiatry 2022, 35, e100749. [Google Scholar] [CrossRef]
- Rowell, K.; Thomley, R. Recovering Emotionally from Disaster; American Psychological Association: Washington, DC, USA, 2013. [Google Scholar]
- Gebreyesus, A.; Gebremariam, A.G.; Kidanu, K.G.; Gidey, S.; Haftu, H.; Nigusse, A.T.; Shishay, F.; Mamo, L. Post-traumatic stress disorder symptoms among internally displaced persons: Unveiling the impact of the war of Tigray. Discov. Ment. Health 2024, 4, 18. [Google Scholar] [CrossRef]
- Bromet, E.J.; Atwoli, L.; Kawakami, N.; Navarro-Mateu, F.; Piotrowski, P.; King, A.J.; Aguilar-Gaxiola, S.; Alonso, J.; Bunting, B.; Demyttenaere, K.; et al. Post-traumatic stress disorder associated with natural and human-made disasters in the World Mental Health Surveys. Psychol. Med. 2017, 47, 227–241. [Google Scholar] [CrossRef]
- Du, J.; Diao, H.; Zhou, X.; Zhang, C.; Chen, Y.; Gao, Y.; Wang, Y. Post-traumatic stress disorder: A psychiatric disorder requiring urgent attention. Med. Rev. 2022, 2, 219–243. [Google Scholar] [CrossRef]
- Torrico, T.J.; Mikes, B.A. Posttraumatic Stress Disorder in Children; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Crone, C.; Fochtmann, L.J.; Attia, E.; Boland, R.; Escobar, J.; Fornari, V.; Golden, N.; Guarda, A.; Jackson-Triche, M.; Manzo, L.; et al. The American Psychiatric Association practice guideline for the treatment of patients with eating disorders. Am. J. Psychiatry 2023, 180, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Jellestad, L.; Vital, N.A.; Malamud, J.; Taeymans, J.; Mueller-Pfeiffer, C. Functional impairment in Posttraumatic Stress Disorder: A systematic review and meta-analysis. J. Psychiatr. Res. 2021, 136, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Charlson, F.; van Ommeren, M.; Flaxman, A.; Cornett, J.; Whiteford, H.; Saxena, S. New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. Lancet 2019, 394, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, E.H.; Kheir, D. Prevalence of post-traumatic stress disorder and depression and associated factors among internally displaced persons in Al-Galgala, Sudan. Neuropsychiatr. Dis. Treat. 2024, 20, 1155–1168. [Google Scholar] [CrossRef]
- Sanchez Gil, L. Being Together Through ICTs: Transnational Family Practices in the Context of Ukrainian Forced Migration. Master’s Thesis, Malmö University, Malmö, Sweden, 2023. [Google Scholar]
- Tol, W.A.; Barbui, C.; Galappatti, A.; Silove, D.; Betancourt, T.S.; Souza, R.; Golaz, A.; van Ommeren, M. Mental health and psychosocial support in humanitarian settings: Linking practice and research. Lancet 2011, 378, 1581–1591. [Google Scholar] [CrossRef]
- Miller, K.E.; Rasmussen, A. The mental health of civilians displaced by armed conflict: An ecological model of refugee distress. Epidemiology Psychiatr. Sci. 2017, 26, 129–138. [Google Scholar] [CrossRef]
- Silove, D.; Ventevogel, P.; Rees, S. The contemporary refugee crisis: An overview of mental health challenges. World Psychiatry 2017, 16, 130–139. [Google Scholar] [CrossRef]
- Bryant, R.A. A critical review of mechanisms of adaptation to trauma: Implications for early interventions for posttraumatic stress disorder. Clin. Psychol. Rev. 2021, 85, 101981. [Google Scholar] [CrossRef]
- Ying, L.; Jia, X.; Lin, C. The longitudinal associations between PTSD symptoms, depressive symptoms, and academic burnout in adolescence and early adulthood in the postdisaster context. Acta Psychol. 2023, 239, 104011. [Google Scholar] [CrossRef]
- O’dOnovan, A.; Cohen, B.E.; Seal, K.H.; Bertenthal, D.; Margaretten, M.; Nishimi, K.; Neylan, T.C. Elevated risk for autoimmune disorders in Iraq and Afghanistan veterans with posttraumatic stress disorder. Biol. Psychiatry 2015, 77, 365–374. [Google Scholar] [CrossRef]
- Kozhyna, H.; Zelenska, K.; Viun, V.; Khaustov, M.; Asieieva, Y. Clinical specifics of stress-related disorders in volunteers whose activities are related to Joint Forces Operation. Rev. Amaz. Investig. 2021, 10, 141–147. [Google Scholar] [CrossRef]
- Schick, M.; Morina, N.; Mistridis, P.; Schnyder, U.; Bryant, R.A.; Nickerson, A. Changes in post-migration living difficulties predict treatment outcome in traumatized refugees. Front. Psychiatry 2018, 9, 476. [Google Scholar] [CrossRef] [PubMed]
- Nickerson, A.; Creamer, M.; Forbes, D.; McFarlane, A.C.; O’Donnell, M.L.; Silove, D.; Steel, Z.; Felmingham, K.; Hadzi-Pavlovic, D.; Bryant, R.A. The longitudinal relationship between post-traumatic stress disorder and perceived social support in survivors of traumatic injury. Psychol. Med. 2017, 47, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Fel, S.; Jurek, K.; Lenart-Kłoś, K. Relationship between socio-demographic factors and posttraumatic stress disorder: A cross sectional study among civilian participants’ hostilities in Ukraine. Int. J. Environ. Res. Public Health 2022, 19, 2720. [Google Scholar] [CrossRef] [PubMed]
- Qi, R.; Luo, Y.; Zhang, L.; Weng, Y.; Surento, W.; Jahanshad, N.; Xu, Q.; Yin, Y.; Li, L.; Cao, Z.; et al. Social support modulates the association between PTSD diagnosis and medial frontal volume in Chinese adults who lost their only child. Neurobiol. Stress 2020, 13, 100227. [Google Scholar] [CrossRef]
- Shah, S.; Tahoor, S.S.; Sardar, Z.; Gul, M.; Anwar, M. The Role of Perceived Social Support in Building Resilience Among Individuals with Chronic Illnesses: Impacts on Emotional Well-Being and Coping with Disease-Related Stress. Crit. Rev. Soc. Sci. Stud. 2025, 3, 977–984. [Google Scholar] [CrossRef]
- Franz, V.A.; Arnkoff, D.B.; Glass, C.R.; Mete, M.; Dutton, M.A. Predictors of the impact of the September 11th terrorist attacks on victims of intimate partner violence. J. Trauma. Stress 2011, 24, 530–537. [Google Scholar] [CrossRef]
- Albert, K.M.; Potter, G.G.; McQuoid, D.R.; Taylor, W.D. Cognitive performance in antidepressant-free recurrent major depressive disorder. Depression Anxiety 2018, 35, 694–699. [Google Scholar] [CrossRef]
- Ito, D.; Koseki, S.; Ohtani, T. A Brief School-Based Cognitive-Behavioral Intervention for Japanese Adolescents With Severe Posttraumatic Stress. J. Trauma. Stress 2016, 29, 577–580. [Google Scholar] [CrossRef]
- Schweitzer, R.; Melville, F.; Steel, Z.; Lacherez, P. Trauma, Post-migration living difficulties, and social support as predictors of psychological adjustment in resettled sudanese refugees. Aust. New Zealand J. Psychiatry 2006, 40, 179–187. [Google Scholar] [CrossRef]
- Zalta, A.K.; Tirone, V.; Orlowska, D.; Blais, R.K.; Lofgreen, A.; Klassen, B.; Held, P.; Stevens, N.R.; Adkins, E.; Dent, A.L. Examining moderators of the relationship between social support and self-reported PTSD symptoms: A meta-analysis. Psychol. Bull. 2021, 147, 33–54. [Google Scholar] [CrossRef]
- Sippel, L.M.; Liebman, R.E.; Schäfer, S.K.; Ennis, N.; Mattern, A.C.; Rozek, D.C.; Monson, C.M. Sources of social support and trauma recovery: Evidence for bidirectional associations from a recently trauma-exposed community sample. Behav. Sci. 2024, 14, 284. [Google Scholar] [CrossRef]
- Scholte, W.F.; Olff, M.; Ventevogel, P.; de Vries, G.-J.; Jansveld, E.; Cardozo, B.L.; Crawford, C.A.G. Mental health symptoms following war and repression in Eastern Afghanistan. JAMA 2004, 292, 585–593. [Google Scholar] [CrossRef]
- Min, S.-Y.; Wong, Y.-L.I. Sources of social support and community integration among persons with serious mental illnesses in Korea. J. Ment. Health 2015, 24, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Seo, M.K.; Lee, M.H. Effects of community-based programs on integration into the mental health and non-mental health communities. Healthcare 2021, 9, 1181. [Google Scholar] [CrossRef] [PubMed]
- Wood, B.; Kallestrup, P. Benefits and challenges of using a participatory approach with community-based mental health and psychosocial support interventions in displaced populations. Transcult. Psychiatry 2021, 58, 283–292. [Google Scholar] [CrossRef] [PubMed]
- Seidi, P.A.-M.; Jaff, D.; Abas, N.Q.; Chung, E.O.; Wilson, M.W.; Potter, H.; Palmquist, A.E.L. Mental health status of internally displaced persons in the Garmian region of Kurdistan, Iraq: A cross-sectional survey. Med. Confl. Surviv. 2023, 39, 117–131. [Google Scholar] [CrossRef]
- Xing, L.; Lu, Y.; Zhang, H.; Shi, Z.; Chang, S.; Liu, W.; Kou, J.; Zhang, H. Mediating effect of psychological capital on the relationship between mental health literacy and coping styles among newly recruited nurses. BMC Nurs. 2024, 23, 178. [Google Scholar] [CrossRef]
- Alat, P.; Das, S.S.; Arora, A.; Jha, A.K. Mental health during COVID-19 lockdown in India: Role of psychological capital and internal locus of control. Curr. Psychol. 2023, 42, 1923–1935. [Google Scholar] [CrossRef]
- Luthans, F.; Avolio, B.J.; Avey, J.B.; Norman, S.M. Positive psychological capital: Measurement and relationship with performance and satisfaction. Pers. Psychol. 2007, 60, 541–572. [Google Scholar] [CrossRef]
- Youssef-Morgan, C.M. Psychological capital and mental health: Twenty-five years of progress. Organ. Dyn. 2024, 53, 101081. [Google Scholar] [CrossRef]
- Avey, J.B.; Reichard, R.J.; Luthans, F.; Mhatre, K.H. Meta-analysis of the impact of positive psychological capital on employee attitudes, behaviors, and performance. Hum. Resour. Dev. Q. 2011, 22, 127–152. [Google Scholar] [CrossRef]
- Luthans, F.; Youssef, C.M.; Sweetman, D.S.; Harms, P.D. Meeting the leadership challenge of employee well-being through relationship PsyCap and health PsyCap. J. Leadersh. Organ. Stud. 2013, 20, 118–133. [Google Scholar] [CrossRef]
- Prasath, P.R.; Xiong, Y.; Zhang, Q.; Jeon, L. Psychological capital, well-being, and distress of international students. Int. J. Adv. Couns. 2022, 44, 529–549. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.; Xu, C.; Xue, J.; Su, J.; Lu, Q.; Wang, B. Perceived Stress, Psychological Capital, and Psychological Distress Among Chinese Nursing Students: A Cross-Sectional Study. BMC Nurs. 2022, 21, 128. [Google Scholar] [CrossRef]
- Xue, M.; Yuan, Y.; Chen, H.; Liu, Y.; Dai, M.; Sun, H.; Qu, J.; Zhou, T.; Zhou, J.; Qu, J.; et al. Perceived stress and symptoms of post-traumatic stress disorder in nurses: A moderated mediation model of maladaptive cognitive emotional regulation and psychological capital. Front. Psychiatry 2022, 13, 902558. [Google Scholar] [CrossRef]
- Mozaffari, S.; Delavar, A.; Dortaj, F. The role of quality of life components with the mediation of psychological capital in reducing PTSD among earthquake victims in Kermanshah. J. Adolesc. Youth Psychol. Stud. 2023, 4, 24–33. [Google Scholar] [CrossRef]
- Yıldırım, M.; Cengiz, S.; Aziz, I.A.; Ziapour, A.; Turan, M.E. Posttraumatic Stress Disorder (PTSD), psychological flexibility and psychological adjustment problems: Turkish validation of the PTSD checklist for short form DSM-5 (PCL-5-S). Eur. J. Trauma Dissociation 2024, 8, 100381. [Google Scholar] [CrossRef]
- Luo, Y.; Deng, Y.; Ma, T.; Jiang, Y. The influence of gratitude on depressive symptoms among Chinese college students during the COVID-19 pandemic: The moderating effect of psychological capital. Psychol. Sch. 2023, 60, 2447–2459. [Google Scholar] [CrossRef]
- Kogan, L.S. Variance designs in psychological research. Psychol. Bull. 1953, 50, 1. [Google Scholar] [CrossRef]
- Zewude, G.T.; Bereded, D.G.; Abera, E.; Tegegne, G.; Goraw, S.; Segon, T. The impact of internet addiction on mental health: Exploring the mediating effects of positive psychological capital in university students. Adolescents 2024, 4, 200–221. [Google Scholar] [CrossRef]
- Weathers, F.W.; Litz, B.; Herman, D.; Juska, J.; Keane, T. PTSD checklist—Civilian version. J. Occup. Health Psychology 1994. [Google Scholar]
- López-Núñez, M.I.; de Jesús, S.N.; Viseu, J.; Santana-Cárdenas, S. Capital psicológico de los trabajadores en España. Análisis factorial confirmatorio del PCQ-12. Rev. Iberoam. Diagnóstico Y Evaluación-E Avaliação Psicol. 2018, 3, 67–79. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Williams, P. A User’s Guide to the General Health Questionnaire; NFER-Nelson: Windsor, UK, 1988. [Google Scholar]
- Goldberg, D.P.; Gater, R.; Sartorius, N.; Ustun, T.B.; Piccinelli, M.; Gureje, O.; Rutter, C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 1997, 27, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Hoberman, H.M. Positive events and social supports as buffers of life change stress. J. Appl. Soc. Psychol. 1983, 13, 99–125. [Google Scholar] [CrossRef]
- Cohen, S.; Mermelstein, R.; Kamarck, T.; Hoberman, H.M. Measuring the functional components of social support. In Social Support: Theory, Research and Applications; Springer: Berlin/Heidelberg, Germany, 1985; pp. 73–94. [Google Scholar]
- Merz, E.L.; Roesch, S.C.; Malcarne, V.L.; Penedo, F.J.; Llabre, M.M.; Weitzman, O.B.; Navas-Nacher, E.L.; Perreira, K.M.; Gonzalez, F.; Ponguta, L.A.; et al. Validation of interpersonal support evaluation list-12 (ISEL-12) scores among English- and Spanish-speaking Hispanics/Latinos from the HCHS/SOL sociocultural ancillary study. Psychol. Assess. 2014, 26, 384–394. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; Guilford Press: New York, NY, USA; London, UK, 2015. [Google Scholar]
- Hair, J.F., Jr.; Howard, M.C.; Nitzl, C. Assessing measurement model quality in PLS-SEM using confirmatory composite analysis. J. Bus. Res. 2020, 109, 101–110. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Hayes, A.F. Partial, conditional, and moderated moderated mediation: Quantification, inference, and interpretation. Commun. Monographs 2018, 85, 4–40. [Google Scholar] [CrossRef]
- Ahmed, D.R.; Mesbah, S.M.; Azzawi, M.A.D.A.; Heun, R. Trauma and mental health problems among Iraqi IDPs following the 2014 ISIS Invasion: A systematic review. Med. Confl. Surviv. 2024, 40, 366–387. [Google Scholar] [CrossRef]
- Bekeko, S.D.; Nimani, T.D.; Darcho, S.D.; Bayisa, F.S. Depression, anxiety and its predictor among internally displaced person in metekel Ethiopia, 2023: Using a structural equation model. Front. Psychiatry 2025, 15, 1458939. [Google Scholar] [CrossRef]
- Olufadewa, I.I.; Adesina, M.A.; Oladele, R.I.; Ayorinde, T.A. “Watching my family being killed by terrorists made me really depressed”: Mental health experiences, challenges and needed support of young internally displaced persons in northern Nigeria. J. Migr. Health 2022, 6, 100121. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, T.L.; Mohammed, A.; Eseigbe, E.; Adekeye, T.; Nuhu, F.T.; Lasisi, M.; Muhammad, A.; Sulaiman, Z.T.; Abdullateef, A.A.; Hayyatudeen, N.; et al. Descriptive characterization of psycho-trauma, psychological distress, and post-traumatic stress disorder among children and adolescent internally displaced persons in Kaduna, Nigeria. Front. Psychiatry 2016, 7, 179. [Google Scholar] [CrossRef] [PubMed]
- Chukwuorji, J.B.C.; Ifeagwazi, C.M.; Eze, J.E. Event centrality influences posttraumatic stress disorder symptoms via core beliefs in internally displaced older adults. Aging Ment. Health 2019, 23, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, R.; Othieno, C.; Omollo, R.; Ongeri, L.; Sifuna, P.; Mboroki, J.K.; Kiima, D.; Ogutu, B. Probable post traumatic stress disorder in kenya and its associated risk factors: A cross-sectional household survey. Int. J. Environ. Res. Public Health 2015, 12, 13494–13509. [Google Scholar] [CrossRef]
- Perrin, M.; Vandeleur, C.L.; Castelao, E.; Rothen, S.; Glaus, J.; Vollenweider, P.; Preisig, M. Determinants of the development of post-traumatic stress disorder, in the general population. Chest 2014, 49, 447–457. [Google Scholar] [CrossRef]
- Ali, A.M.A.; Adam, O.A.M.; Salem, S.E.M.; Hamad, S.H.I.; Ahmed, N.E.M.; Ali, H.M.A.; Abass, A.A.M.; Abass, H.-A.A.M.; Albasher, A.I.-E.; Yousif, M.E.E.; et al. Prevalence of physical and mental health problems among internally displaced persons in White Nile state, Sudan 2023: A cross sectional study. BMC Public Health 2024, 24, 3448. [Google Scholar] [CrossRef]
- Sabhlok, S.R.; Pender, V.; Mauer, E.; Lipnick, M.S.; Kaur, G. Addressing the gaps in mental health care for internally displaced persons. J. Glob. Health 2020, 10, 010346. [Google Scholar] [CrossRef]
- Debbarma, R.; Majumdar, C.B.; Bhattacharjee, A. Internally displaced persons and mental health issues: A review analysis. Indian J. Health Wellbeing 2021, 12, 171–176. [Google Scholar]
- Idemudia, E.S.; Olawa, B.D.; Wyatt, G.E.; Milburn, N. Pre-displacement stressors, psychological morbidity, and PTSD symptoms among displaced women by Boko-Haram in North-East Nigeria: The buffering roles of psychological capital. J. Psychol. Afr. 2020, 30, 307–314. [Google Scholar] [CrossRef]
- Güler, A.; Gül, S.; Yıldırım, M. Social comparison, resilience, life satisfaction, depression, and anxiety among earthquake survivors in Turkey. Int. J. Disaster Risk Reduct. 2024, 105, 104426. [Google Scholar] [CrossRef]
- Baluku, M.M.; Nansubuga, F.; Musanje, K.; Nantamu, S.; Otto, K. The role of mindfulness, psychological capital, and social capital in the well-being of refugees in Uganda. Curr. Res. Ecol. Soc. Psychol. 2023, 5, 100148. [Google Scholar] [CrossRef]
- Burns, R.; Wickramage, K.; Musah, A.; Siriwardhana, C.; Checchi, F. Health status of returning refugees, internally displaced persons, and the host community in a post-conflict district in northern Sri Lanka: A cross-sectional survey. Confl. Health 2018, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- George, J.; Adelaja, A. Forced Displacement and Agriculture: Implications for Host Communities. Sustainability 2021, 13, 5728. [Google Scholar] [CrossRef]
- White, B.; Driver, S.; Warren, A.M. Resilience and indicators of adjustment during rehabilitation from a spinal cord injury. Rehabilitation Psychol. 2010, 55, 23–32. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Brewin, C.R.; Kaniasty, K.; Greca, A.M.L. Weighing the costs of disaster: Consequences, risks, and resilience in individuals, families, and communities. Psychol. Sci. Public Interest 2010, 11, 1–49. [Google Scholar] [CrossRef]
- Boettcher, V.S.; Neuner, F. Posttraumatic stress among refugees: The moderating effect of perceived social support. J. Migr. Health 2025, 11, 100323. [Google Scholar] [CrossRef]
- Kowalchyk, M.; Chernoff, E.; Brinkman, H.R.; Brown, A.D.; Pietrzak, R.H.; Feder, A. Perceived social support moderates the relation between forward-focused coping and PTSD symptoms in World Trade Center trauma survivors. J. Psychiatr. Res. 2023, 159, 130–134. [Google Scholar] [CrossRef]
- Teismann, T.; Naghavi, A.; Asgari, Z.; Grundei, L.; Brailovskaia, J. Posttraumatic stress disorder symptoms and suicidal ideation/behavior: The moderating effects of positive mental health and social support among Iranian and German students. Curr. Psychol. 2023, 42, 20757–20764. [Google Scholar] [CrossRef]
- Panagioti, M.; Gooding, P.; Taylor, P.; Tarrier, N. Perceived social support buffers the impact of PTSD symptoms on suicidal behavior: Implications into suicide resilience research. Compr. Psychiatry 2014, 55, 104–112. [Google Scholar] [CrossRef]
- Blessing, A.; Russell, P.; DeBeer, B.B.; Morissette, S.B. Perceived family support buffers the impact of PTSD-depression symptoms on suicidal ideation in college students. Psychol. Rep. 2025, 128, 1661–1673. [Google Scholar] [CrossRef] [PubMed]
- Hassan, G.; Ventevogel, P.; Jefee-Bahloul, H.; Barkil-Oteo, A.; Kirmayer, L.J. Mental health and psychosocial wellbeing of Syrians affected by armed conflict. Epidemiology Psychiatr. Sci. 2016, 25, 129–141. [Google Scholar] [CrossRef] [PubMed]
- Manrique, I.R. Examining the Moderating Effects of Social Support and Displacement on the Relationship Between Natural Disaster-Related Stress and Physical Health; University of Louisiana at Lafayette: Lafayette, LA, USA, 2024. [Google Scholar]
- Michael, O.C.; Țânculescu-Popa, L. The moderating effect of resilience and social support on the relationship between post-migration stress and psychological well-being among Ukrainian refugees in Romania. Rev. de Psihol. 2024, 70, 75–95. [Google Scholar] [CrossRef]
- Duren, R.; Yalçın, Ö. Social capital and mental health problems among Syrian refugee adolescents: The mediating roles of perceived social support and post-traumatic symptoms. Int. J. Soc. Psychiatry 2021, 67, 243–250. [Google Scholar] [CrossRef] [PubMed]
- McGuire, A.P.; Gauthier, J.M.; Anderson, L.M.; Hollingsworth, D.W.; Tracy, M.; Galea, S.; Coffey, S.F. Social support moderates effects of natural disaster exposure on depression and posttraumatic stress disorder symptoms: Effects for displaced and nondisplaced residents. J. Trauma. Stress 2018, 31, 223–233. [Google Scholar] [CrossRef]
- Zhao, J.Y.; Jiang, J.F.; Shi, S.Y.; Su, X.Q.; Que, W.Q.; Zhu, L.L.; Guo, Y.J. Mediating Effects of Resilience and Perceived Social Support Between Gratitude and the Adaptability to Return-To-Work in Cancer Patients. J. Adv. Nursing 2025. [Google Scholar] [CrossRef]
| Variable | Min | Max | Mean | SD | Skewness | Kurtosis | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|---|---|---|---|
| PTSD | 24.00 | 116.00 | 56.79 | 13.73 | 0.08 | 0.12 | — | 0.517 ** | −0.460 ** | −0.402 ** |
| HM | 6.00 | 36.00 | 19.70 | 7.56 | 0.27 | −0.99 | — | — | −0.409 ** | −0.528 ** |
| PsyCap | 17.00 | 72.00 | 47.21 | 11.76 | −0.41 | −0.31 | — | — | — | 0.556 ** |
| PSS | 3.00 | 33.00 | 13.09 | 6.87 | 0.63 | −0.45 | — | — | — | — |
| Variables | CR | AVE | MSV | PTSD | MH | PsyCap | PSS |
|---|---|---|---|---|---|---|---|
| PTSD | 0.931 | 0.576 | 0.309 | 0.759 | |||
| MH | 0.924 | 0.551 | 0.309 | 0.517 ** | 0.742 | ||
| PsyCap | 0.934 | 0.587 | 0.309 | −0.460 *** | −0.409 ** | 0.766 | |
| PSS | 0.915 | 0.521 | 0.309 | −0.402 ** | 0.528 ** | 0.556 ** | 0.722 |
| Model | x2/df | CFI | TLI | SRMR | RMSEA |
|---|---|---|---|---|---|
| Model 1 | 1.34 * | 0.949 | 0.958 | 0.053 | 0.041 |
| Hypothesis | Path | β | SE | p | CI = 95% |
|---|---|---|---|---|---|
| Hypothesis 1 | PTSD → MH | 0.233 | 0.070 | *** | -- |
| Hypothesis 2 | PTSD → PsyCap | 0.673 | 0.0817 | 0.026 | -- |
| Hypothesis 3 | PsyCap → MH | 0.720 | 0.088 | *** | -- |
| Hypothesis 4 | PTSD → PsyCap→ MH | 0.564 | 0.142 | *** | -- |
| Hypothesis 5 | PTSD → PSS | 0.422 | 0.071 | 0.034 | -- |
| Hypothesis 6 | PSS → PsyCap | 0.380 | 0.050 | 0.038 | CI [0.230, 0.523] |
| Hypothesis 7 | PTSD → PSS → PsyCap | 0.324 | 0.066 | 0.011 | CI [0.133, 0.310] |
| Predictor | B | SE | t | p | 95% CI |
|---|---|---|---|---|---|
| Constant | 19.931 | 0.427 | 46.719 | 0.000 | [19.091, 20.770] |
| PTSD | 0.110 | 0.034 | 3.198 | 0.002 | [0.042, 0.178] |
| PSS | 0.332 | 0.063 | 5.264 | 0.000 | [0.208, 0.456] |
| PTSD × PSS | −0.012 | 0.005 | −2.231 | 0.027 | [−0.023, −0.001] |
| PSS Level | Effect | SE | t | p | 95% CI |
|---|---|---|---|---|---|
| Low (−1 SD) | 0.195 | 0.038 | 5.082 | 0.000 | [0.120, 0.271] |
| Medium (Mean) | 0.135 | 0.031 | 4.343 | 0.000 | [0.074, 0.197] |
| High (+1 SD) | 0.015 | 0.066 | 0.232 | 0.817 | [−0.114, 0.144] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Melese, A.K. Unpacking Post-Traumatic Stress Disorder and Mental Health in Internally Displaced Persons: A Mediation-Moderation Model of Psychological Capital and Perceived Social Support. Int. J. Environ. Res. Public Health 2025, 22, 1788. https://doi.org/10.3390/ijerph22121788
Melese AK. Unpacking Post-Traumatic Stress Disorder and Mental Health in Internally Displaced Persons: A Mediation-Moderation Model of Psychological Capital and Perceived Social Support. International Journal of Environmental Research and Public Health. 2025; 22(12):1788. https://doi.org/10.3390/ijerph22121788
Chicago/Turabian StyleMelese, Adane Kefale. 2025. "Unpacking Post-Traumatic Stress Disorder and Mental Health in Internally Displaced Persons: A Mediation-Moderation Model of Psychological Capital and Perceived Social Support" International Journal of Environmental Research and Public Health 22, no. 12: 1788. https://doi.org/10.3390/ijerph22121788
APA StyleMelese, A. K. (2025). Unpacking Post-Traumatic Stress Disorder and Mental Health in Internally Displaced Persons: A Mediation-Moderation Model of Psychological Capital and Perceived Social Support. International Journal of Environmental Research and Public Health, 22(12), 1788. https://doi.org/10.3390/ijerph22121788






