Consensus on Care Competencies for Community Citizens in Japan: A Modified Delphi Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Panelists
2.3. Defining Care Competencies and List Development
2.4. Delphi Surveys Using the RAND/UCLA Method
2.4.1. First Evaluation
2.4.2. Panel Meeting
2.4.3. Second Evaluation
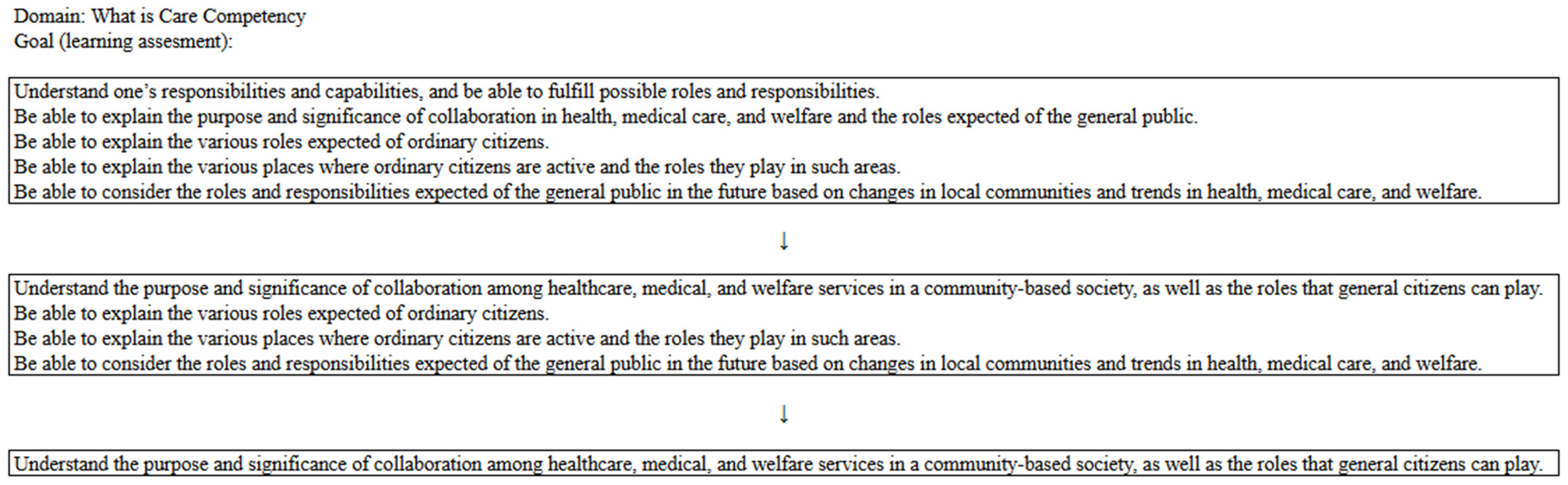
2.4.4. Final Version of the Competencies
3. Results
3.1. Defining Care Competencies
3.2. Delphi Surveys
3.2.1. Panelists
3.2.2. First Evaluation
3.2.3. Panel Meeting
3.2.4. Second Evaluation
3.2.5. Final Version of the Competencies
4. Discussion
4.1. Concept Distinction and Boundaries
4.2. Strengths and Practical Application
4.3. Comparison with International Initiatives
4.4. Limitations and Future Research Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| UCLA | University of California, Los Angeles |
| SDoH | Social Determinants of Health |
Appendix A
Appendix B

| Themes | Domains | ||
|---|---|---|---|
| Care competency | Foundations of care competency (76 items) | What care competency is Basics of health Basics of care Engaging with “health” Engaging with “care” Care techniques Ethics Understanding of Research Medical safety | This theme forms the foundation of care competencies, encompassing the knowledge, attitudes, and care skills required to provide and receive care.
|
| Care competency across the lifespan (31 items) | Sexuality and life Family Children Adults Older adults Advance care planning | Pregnancy; childbirth; and each process of birth, aging, and death, including knowledge, attitudes, and care skills.
| |
| Care competency by stages of illness (18 items) | Fundamentals of illness Mental health Acute phase Recovery phase Chronic phase Terminal phase | This includes knowledge and preparedness regarding the patient’s disease transition process from the onset of illness to the end of life.
| |
| Care competency through living in the community (26 items) | Community systems supporting care Disaster preparedness | This theme encompasses knowledge and care skills related to social resources and community structures where citizens reside.
|
| Themes | Domains | Goals (Learning Assessment) |
|---|---|---|
| Foundations of care competency | What care competency is | Understand what care competency entails. |
| Understand the purpose and significance of collaboration among healthcare, medical, and welfare services in a community-based society, as well as the roles that general citizens can play. | ||
| Basics of health | Be able to consider the meaning of health from one’s own perspective. | |
| Understand basic human needs. | ||
| Understand the changes in daily activities, emotions, communication, and social roles that occur with human growth and development. | ||
| Recognize that a healthy lifestyle varies from person to person. | ||
| Understand the relationship between health and factors such as the environment, nutrition/diet, excretion, activity, and rest. | ||
| Understand the influence of genetics and the environment (sociocultural, physio-bio-chemical, political, and economic environments) on health. | ||
| Understand the structure of dietary habits, factors affecting eating behaviors, and the significance of food for health. | ||
| Understand nutrition and energy metabolism. | ||
| Understand the structure and function of the digestive tract and glands related to nutrition and excretion. | ||
| Recognize the significance of excretion for health. | ||
| Understand the balance and rhythm (biological rhythms, exercise habits, sleep patterns, work/activity, and leisure) necessary for maintaining health. | ||
| Understand and respect the diversity of people’s values and social backgrounds in relation to a healthy and fulfilling life. | ||
| Understand the relationship between addictions (such as smoking, drinking, and gambling) and health. | ||
| Recognize the importance of considering individual lifestyles (such as daily habits, purpose in life, and religious practices) from a health and care perspective, considering diverse cultural backgrounds. | ||
| Basics of care | Be able to think about what care is and its purpose. | |
| Understand that care aims to ensure the safety, comfort, and independence of the care recipient. | ||
| Recognize the importance of supporting the care recipient within a care team centered on them. | ||
| Engaging with “health” | Recognize that one’s health is one’s own responsibility and possess the ability to engage proactively with medical care (understand how to seek a second opinion, how to respond when referred to a clinic in an outpatient setting, and how to approach medical consultations). | |
| Be able to critically evaluate various types of information related to health and daily life, as well as select and utilize relevant information. | ||
| Be able to manage one’s health condition and take action to seek support from others when necessary. | ||
| Be able to consider ways to prevent illnesses and disabilities. | ||
| Understand awareness-raising activities aimed at promoting an accurate understanding of physical and mental health disorders. | ||
| Understand the health checkup systems necessary for early detection, diagnosis, and treatment of physical and mental health disorders, as well as how to utilize them. | ||
| Recognize symptoms and situations that require urgent medical attention. | ||
| Be knowledgeable about hospital admission and discharge preparations appropriate for different illnesses and disabilities. | ||
| Be able to implement infection prevention measures. | ||
| Engaging with “care” | Develop an active attitude toward learning about care. | |
| Understand that communication is crucial to relationships related to care. | ||
| Recognize one’s communication tendencies and engage with care recipients while being aware of personal challenges. | ||
| Use various communication methods (such as verbal, non-verbal, written, and visual information) to build relationships tailored to the care recipient’s characteristics. | ||
| Understand that providing care requires accurate knowledge, reliable skills, and an appropriate attitude. | ||
| Recognize the importance of implementing care based on a plan, evaluating the outcomes, and improving future care. | ||
| Show interest in the care recipient. | ||
| Understand how to apply knowledge about care to support the care recipient in achieving better health. | ||
| Recognize the need to gather diverse information to gain a holistic understanding of the care recipient. | ||
| Be able to collect as much relevant information as possible based on the care recipient’s condition. | ||
| Integrate collected information to consider the care recipient’s lifestyle and health status from multiple perspectives. | ||
| Support care recipients in making informed decisions for maintaining and improving their health. | ||
| Understand methods for evaluating whether the care provided was effective. | ||
| Care techniques | Be able to adjust the care recipient’s posture to ensure they remain in a comfortable position. | |
| Be able to make adjustments that help the care recipient remain mentally calm. | ||
| Be able to create an environment necessary for the care recipient to live safely and comfortably. | ||
| Be able to support the care recipient in eating safely and comfortably. | ||
| Be able to support the care recipient in excreting safely and comfortably. | ||
| Be able to support the care recipient in engaging in daily activities and resting safely and comfortably. | ||
| Be able to support the care recipient in maintaining cleanliness and appropriate clothing habits. | ||
| Be able to support the care recipient in maintaining stable respiratory and circulatory conditions. | ||
| Be able to perform necessary measurements (such as body temperature, SpO2, and blood pressure) to assess the physical and mental condition of the care recipient. | ||
| Be able to support the care recipient in taking medication safely, including self-care. | ||
| Be able to perform basic life support (such as using an automated external defibrillator) and first aid (emergency care). | ||
| Ethics | Understand that fundamental human rights form the foundation of care practice within one’s responsibilities and capabilities. | |
| Maintain an attitude that respects life and human dignity. | ||
| Understand the means and methods to protect people’s fundamental human rights in daily care (including the significance and necessity of informed consent and assent, confidentiality, and methods of protecting personal information). | ||
| Recognize that care is an interaction between the care recipient and provider and that the rights of care providers must also be protected. | ||
| Be able to uphold confidentiality and the protection of personal information. | ||
| Understanding of research | Understand how research findings are applied to address social issues related to health. | |
| Recognize the necessity of ethical considerations in medical and care-related research. | ||
| Medical safety | Understand that medical treatment carries both benefits and risks (such as complications and side effects). | |
| Understand the effects of drugs and radiation on health and daily life. | ||
| Understand safe care practices and methods for preventing adverse events related to care (such as falls, pressure ulcers, and medication errors). | ||
| Recognize the safety measures required in medical, caregiving, and welfare services, as well as the role of care recipients in ensuring their safety. | ||
| Understand the importance of systems for the safe management of pharmaceuticals and medical devices, as well as the significance of building a safe medical environment. | ||
| Recognize the importance of reflecting on accidents and near-miss incidents that occur at home. | ||
| Care competency across the lifespan | Sexuality and life | Understand the health issues specific to each stage of a woman’s life cycle and the necessary care associated with them. |
| Understand the diversity of sexuality. | ||
| Recognize social issues related to people’s sexual and reproductive health and rights. | ||
| Understand maternal and child health, as well as postpartum care, childcare support, and maternal and child health systems. | ||
| Understand care that supports parent–child bonding and family development during the perinatal period. | ||
| Understand sexuality and reproduction in daily life. | ||
| Recognize the physical, psychological, and social characteristics, as well as physiological changes during pregnancy, childbirth, postpartum, and the neonatal period. | ||
| Be able to implement necessary support for health promotion during pregnancy, childbirth, postpartum, and the neonatal period. | ||
| Family | Understand the developmental tasks of individuals and families. | |
| Recognize the process of childbirth and family development, as well as the functions of the family. | ||
| Understand the self-care functions of families. | ||
| Children | Recognize the importance of protecting children’s rights. | |
| Understand children’s growth and development, along with appropriate care methods for each stage. | ||
| Be aware of issues related to the growth, development, and health of children and the care needs of children in hospitals, homes, schools, and other settings. | ||
| Understand the impact of illness and hospitalization on children. | ||
| Recognize child-specific care techniques, including childcare-related support and emergency response. | ||
| Be able to implement necessary support for children’s self-care acquisition and overall growth and development. | ||
| Adults | Be able to consider health issues in adulthood from physical, psychological, and social perspectives. | |
| Be able to consider the balance between work and family life when managing necessary medical care and self-care. | ||
| Older adults | Be able to comprehensively consider the situation of older adults receiving care, considering age-specific physical, psychological, and social changes, as well as individual lifestyles, values, and spirituality. | |
| Understand health risks specific to older adults (such as falls, pain, delirium, cognitive decline, depression, malnutrition, swallowing disorders, and pressure ulcers) and prevention methods. | ||
| Understand ways to support older adults and their families in maintaining individuality while maximizing their abilities, based on their self-care capabilities. | ||
| Recognize how older adults can live authentically by accessing support from various professionals and institutions according to different health levels. | ||
| Understand the characteristics of individuals with dementia and the appropriate care for them. | ||
| Recognize the types and characteristics of older adult abuse and the roles that citizens can play in addressing them. | ||
| Be able to consider care that supports the dignity and quality of life of older adults. | ||
| Understand frailty, sarcopenia, locomotive syndrome, and their prevention methods. | ||
| Advance care planning | Be able to consider end-of-life care based on the values of individuals in the final stages of life, including their views on life and death. | |
| Recognize the importance of collaborating with relevant institutions and professionals to support individuals in living their final stage of life in a way that aligns with their wishes. | ||
| Understand the characteristics of the decision-making process for individuals in the final stage of life and the methods to support their decisions. | ||
| Recognize the need for personalized care that considers values, family, and social backgrounds at the end of life. | ||
| Care competency by stages of illness | Fundamentals of illness | Understand the characteristics and treatment progress of different stages of diseases. |
| Recognize major symptoms (such as consciousness disorders, seizures, hematemesis/hemoptysis, chest pain, oliguria/anuria/frequent urination, and pain, including chronic pain) and their management. | ||
| Understand the physical and psychological responses of individuals to illness. | ||
| Recognize how illness and disabilities impact family life and relationships among family members. | ||
| Understand palliative care from a holistic perspective for individuals with illnesses. | ||
| Be able to consider the distress and anxiety experienced by individuals with symptoms. | ||
| Mental health | Be able to consider mental health issues. | |
| Understand the relationship between stress and health, as well as the causes of stress. | ||
| Be able to identify early signs of mental illness in oneself and others and connect them to appropriate support. | ||
| Recognize developmental challenges and psychological crises in different life cycle stages. | ||
| Understand methods to improve mental health in settings such as homes, schools, and workplaces. | ||
| Recognize the importance of supporting perinatal mothers and families to maintain mental health and promote the healthy psychological development of children. | ||
| Understand developmental disorders and ways to provide appropriate environmental support. | ||
| Be aware of available support resources for suicide prevention that can be accessed by individuals at risk and their families. | ||
| Understand the support available for individuals with addiction and their families. | ||
| Understand the stages of recovery and the corresponding care required at each stage, from hospitalization to discharge support, for individuals with mental illness. | ||
| Understand the need for and methods of collaboration with relevant parties to provide community living support for individuals with mental illness. | ||
| Acute phase | Understand the physical, psychological, and social characteristics of individuals in the acute or severe phase. | |
| Understand the psychology and anxiety of individuals in the acute or severe phase, and those of their families. | ||
| Recovery phase | Understand the situation of families supporting individuals recovering from illness or disability. | |
| Understand the concept of normalization. | ||
| Understand functional disabilities (such as physical, intellectual, higher cognitive, mental, and developmental) and the concept of rehabilitation. | ||
| Understand the social resources available for individuals in the recovery phase to live with their disabilities. | ||
| Chronic phase | Understand the foundational principles of support for individuals with chronic illnesses. | |
| Be able to assess one’s own or a family member’s self-care status and challenges based on awareness of illness or disability, self-management status, and test results. | ||
| Understand the causes of sudden deterioration of illness and the need for prevention. | ||
| Terminal phase | Be able to think about the concept of death and the meaning of death, as well as end-of-life care for individuals and their families. | |
| Understand the physical changes in individuals at the final stage of life. | ||
| Understand grief counseling for individuals who have lost a close person (such as family, friends, and acquaintances). | ||
| Care competency through living in the community | Community systems supporting care | Understand the concept of community-based integrated care. |
| Understand self-help, mutual aid, cooperative support, and public assistance in the Integrated Community Care System. | ||
| Understand the meaning of dependence on others and independence in society, and how this balance impacts daily life. | ||
| Understand the necessity of health support in familiar communities for individuals at various life cycle stages and health levels. | ||
| Understand the necessity of considering the health conditions and care needs of all individuals living in the community. | ||
| Understand the types of social security systems (such as social insurance, public assistance, and social welfare). | ||
| Understand the types of social insurance (health insurance, pension insurance, workers’ compensation insurance, employment insurance, and long-term care insurance). | ||
| Understand the roles of various health, medical, and welfare institutions and how to utilize them to achieve the desired way of living. | ||
| Understand the social resources available for community residents, home-care patients, and their families. | ||
| Understand the types and functions of medical facilities providing healthcare. | ||
| Understand the characteristics of home care institutions such as visiting nursing offices, nurse-led comprehensive community care, community comprehensive support centers, and support centers for children and families. | ||
| Understand how medical and long-term care services are provided in care insurance-related service institutions. | ||
| Understand the characteristics of welfare facilities (residential and daycare) for mothers and children, older adults, and individuals with physical and mental disabilities, among others. | ||
| Understand how occupational health services are provided in companies. | ||
| Understand how health services are provided in schools. | ||
| Understand how health services are provided in national and local government administrations. | ||
| Be able to gather information about regional health, medical, and welfare systems. | ||
| Understand the local healthcare system and the division of roles among various institutions in one’s community. | ||
| Disaster preparedness | Understand the impact of disasters on health and daily life. | |
| Understand disaster types, disaster cycles, regional disaster prevention plans, and support systems. | ||
| Understand that different stages of medical relief activities exist during disasters and the corresponding care required at each stage. | ||
| Understand assistance for daily life (e.g., meals, excretion, sleep, hygiene, and environmental maintenance) and physical/mental health management at living facilities during disasters (rescue stations, evacuation centers, welfare evacuation centers, temporary housing, and damaged medical facilities), including self-care. | ||
| Understand the care needs of vulnerable individuals and those requiring evacuation assistance during disasters. | ||
| Understand the necessity for and methods of cooperation and collaboration with disaster-affected communities and multi-professional teams for care. | ||
| Understand the occurrence and risks of secondary disasters. | ||
| Understand stress and mental healthcare for disaster victims and relief workers, including self-care. |
References
- Thiam, Y.; Allaire, J.F.; Morin, P.; Hyppolite, S.R.; Doré, C.; Zomahoun, H.T.V.; Garon, S. A conceptual framework for integrated community care. Int. J. Integr. Care 2021, 21, 5. [Google Scholar] [CrossRef]
- Hua, K.; Pan, Y.; Fang, J.; Wu, H.; Hua, Y. Integrating social, climate and environmental changes to confront accelerating global aging. BMC Public Health 2024, 24, 2838. [Google Scholar] [CrossRef]
- Cabinet Office, Government of Japan. Annual Report on the Ageing Society, Summary; Cabinet Office: Tokyo, Japan, 2024. Available online: https://www8.cao.go.jp/kourei/english/annualreport/2024/pdf/2024.pdf (accessed on 18 June 2025).
- Masaaki, O. Community-based inclusive society and integrated care in Japan: Concepts and challenges for practice. J. Natl. Inst. Public Health 2024, 73, 32–41. [Google Scholar]
- Matsumoto, M.; Nakayama, K. Development of health literacy on social determinants of health questionnaire in Japanese adults. BMC Public Health 2017, 17, 30. [Google Scholar] [CrossRef]
- Nutbeam, D.; Lloyd, J.E. Understanding and responding to health literacy as a social determinant of health. Ann. Rev. Public Health 2021, 42, 159–173. [Google Scholar] [CrossRef]
- Santana, S.; Brach, C.; Harris, L.; Ochiai, E.; Blakey, C.; Bevington, F.; Kleinman, D.; Pronk, N. Updating health literacy for healthy people 2030: Defining its importance for a new decade in public health. J. Public Health Manag. Pract. 2021, 27, S258–S264. [Google Scholar] [CrossRef]
- Jones, D.; Lyle, D.; McAllister, L.; Randall, S.; Dyson, R.; White, D.; Smith, A.; Hampton, D.; Goldsworthy, M.; Rowe, A. The case for integrated health and community literacy to achieve transformational community engagement and improved health outcomes: An inclusive approach to addressing rural and remote health inequities and community healthcare expectations. Prim. Health Care Res. Dev. 2020, 21, e57. [Google Scholar] [CrossRef] [PubMed]
- Costantini, H.; Nihei, M.; Ueno, T. ‘Care literacy’ in super aging Japan. Open Res. Eur. 2021, 1, 85. [Google Scholar] [CrossRef] [PubMed]
- Papadakos, J.; Samoil, D.; Umakanthan, B.; Charow, R.; Jones, J.M.; Matthew, A.; Nissim, R.; Sayal, A.; Giuliani, M.E. What are we doing to support informal caregivers? A scoping review of caregiver education programs in cancer care? Patient Educ. Couns. 2022, 105, 1722–1730. [Google Scholar] [CrossRef]
- Salomone, E.; Ferrante, C.; Salandin, A.; Ferrara, F.; Torchio, E.; Foletti, G.; Ghersi, S.; CST Italy Team; WHO CST Team; Pacione, L.; et al. Acceptability and feasibility of the World Health Organization’s Caregiver Skills Training implemented in the Italian National Health System. Autism 2022, 26, 859–874. [Google Scholar] [CrossRef]
- Gemito, L.; Alves, E.; Moreira, J.; Marques, M.F.; Caldeira, E.; Ferreira, R.; Bico, I.; Pinho, L.; Fonseca, C.; Sousa, L.; et al. Programmes addressed to informal caregivers’ needs: A systematic literature review. Geriatrics 2024, 9, 71. [Google Scholar] [CrossRef]
- Aihara, Y.; Maeda, K. National dementia supporter programme in Japan. Dementia 2021, 20, 1723–1728. [Google Scholar] [CrossRef]
- Iida, M.; Sawada, U.; Usuda, K.; Hazumi, M.; Okazaki, E.; Ogura, K.; Kataoka, M.; Sasaki, N.; Ojio, Y.; Matsunaga, A.; et al. Effects of the mental health supporter training program on mental health-related public stigma among Japanese people: A pretest/posttest study. PCN Rep. 2024, 3, e176. [Google Scholar] [CrossRef]
- Fitch, K.; Bernstein, S.J.; Aguilar, M.D.; Burnand, B.; LaCalle, J.R.; Lázaro, P.; van het Loo, M.; McDonnell, J.; Vader, J.P.; Kahan, J.P. Appropriateness Method User’s Manual; Rand: Arlington, VA, USA, 2001; Available online: https://www.rand.org/content/dam/rand/pubs/monograph_reports/2011/MR1269.pdf (accessed on 28 April 2025).
- Miller, K.A.; Prieto, M.M.; Wing, R.; Goldman, M.P.; Polikoff, L.A.; Nishisaki, A.; Nagler, J. Development of a paediatric airway management checklist for the emergency department: A modified Delphi approach. Emerg. Med. J. 2023, 40, 287–292. [Google Scholar] [CrossRef]
- Ministry of Education, Culture, Sports, Science, and Technology. Model Core Curriculum for Nursing Education in Japan. Available online: https://www.mext.go.jp/content/20200428-mxt_igaku1217788_4.pdf (accessed on 28 April 2025).
- Croasmun, J.T.; Ostrom, L.T. Using Likert-type scales in the Social Sciences. J. Adult Educ. 2011, 40, 19–22. [Google Scholar]
- Holt-Lunstad, J. Social connection as a public health issue: The evidence and a systemic framework for prioritizing the “Social” in Social Determinants of Health. Annu. Rev. Public Health 2022, 43, 193–213, Epub 12 January 2022. [Google Scholar] [CrossRef] [PubMed]
- Hatton, C.R.; Kale, R.; Pollack Porter, K.M.; Mui, Y. Inclusive and intersectoral: Community health improvement planning opportunities to advance the social determinants of health and health equity. BMC Public Health. 2024, 24, 170. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Adams, L.B.; Richmond, J.; Watson, S.N.; Cené, C.W.; Urrutia, R.; Ataga, O.; Dunlap, P.; Corbie-Smith, G. Community health worker training curricula and intervention outcomes in African American and Latinx communities: A systematic review. Health Educ. Behav. 2021, 48, 516–531. [Google Scholar] [CrossRef]
- Knowles, M.; Crowley, A.P.; Vasan, A.; Kangovi, S. Community health worker integration with and effectiveness in health care and public health in the United States. Ann. Rev. Public Health 2023, 44, 363–381. [Google Scholar] [CrossRef]
- Sultan, M.A.; Miller, E.; Tikkanen, R.S.; Singh, S.; Kullu, A.; Cometto, G.; Fitzpatrick, S.; Ajuebor, O.; Gillon, N.; Edward, A.; et al. Competency-based education and training for community health workers: A scoping review. BMC Health Serv. Res. 2025, 25, 263. [Google Scholar] [CrossRef]
- South, J.; Woodall, J.; Stansfield, J.; Mapplethorpe, T.; Passey, A.; Bagnall, A.M. A qualitative synthesis of practice-based learning from case studies on COVID community champion programmes in England, UK. BMC Public Health 2024, 24, 7. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.; McGrath, R.; Ang, K.; Bakolis, I.; Healey, A.; De La Torre, J.A.; Mdudu, I.; Gaughran, F.; Sadler, E.; Da Costa, M.P.; et al. Evaluating a volunteer “health champions” intervention supporting people with severe mental illness to manage their physical health: Feasibility hybrid randomised controlled trial. BJPsych Open 2024, 10, e172. [Google Scholar] [CrossRef] [PubMed]

| Themes | Domains | |
|---|---|---|
| Care competency | Foundations of care competency (76 items) | What care competency is Basics of health Basics of care Engaging with “health” Engaging with “care” Care techniques Ethics Understanding of research Medical safety |
| Care competency across the lifespan (31 items) | Sexuality and life Family Children Adults Older adults Advance care planning | |
| Care competency by stages of illness (18 items) | Fundamentals of illness Mental health Acute phase Recovery phase Chronic phase Terminal phase | |
| Care competency through living in the community (26 items) | Community systems supporting care Disaster preparedness |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takaoka, M.; Igarashi, A.; Yasaka, T.; Sumikawa, Y.; Yoshioka-Maeda, K.; Honda, C.; Matsumoto, H.; Kugai, H.; Futami, A.; Yamamoto-Mitani, N. Consensus on Care Competencies for Community Citizens in Japan: A Modified Delphi Study. Int. J. Environ. Res. Public Health 2025, 22, 1774. https://doi.org/10.3390/ijerph22121774
Takaoka M, Igarashi A, Yasaka T, Sumikawa Y, Yoshioka-Maeda K, Honda C, Matsumoto H, Kugai H, Futami A, Yamamoto-Mitani N. Consensus on Care Competencies for Community Citizens in Japan: A Modified Delphi Study. International Journal of Environmental Research and Public Health. 2025; 22(12):1774. https://doi.org/10.3390/ijerph22121774
Chicago/Turabian StyleTakaoka, Manami, Ayumi Igarashi, Taisuke Yasaka, Yuka Sumikawa, Kyoko Yoshioka-Maeda, Chikako Honda, Hiroshige Matsumoto, Haruna Kugai, Asako Futami, and Noriko Yamamoto-Mitani. 2025. "Consensus on Care Competencies for Community Citizens in Japan: A Modified Delphi Study" International Journal of Environmental Research and Public Health 22, no. 12: 1774. https://doi.org/10.3390/ijerph22121774
APA StyleTakaoka, M., Igarashi, A., Yasaka, T., Sumikawa, Y., Yoshioka-Maeda, K., Honda, C., Matsumoto, H., Kugai, H., Futami, A., & Yamamoto-Mitani, N. (2025). Consensus on Care Competencies for Community Citizens in Japan: A Modified Delphi Study. International Journal of Environmental Research and Public Health, 22(12), 1774. https://doi.org/10.3390/ijerph22121774






