The Relationship Between Food Environments and Health Outcomes: A Case Study in Lansing, Michigan
Abstract
1. Introduction
1.1. Food Environment Characterizations
1.2. Food Insecurity and Health Outcomes
1.3. Food Environments and Health Outcomes
2. Materials and Methods
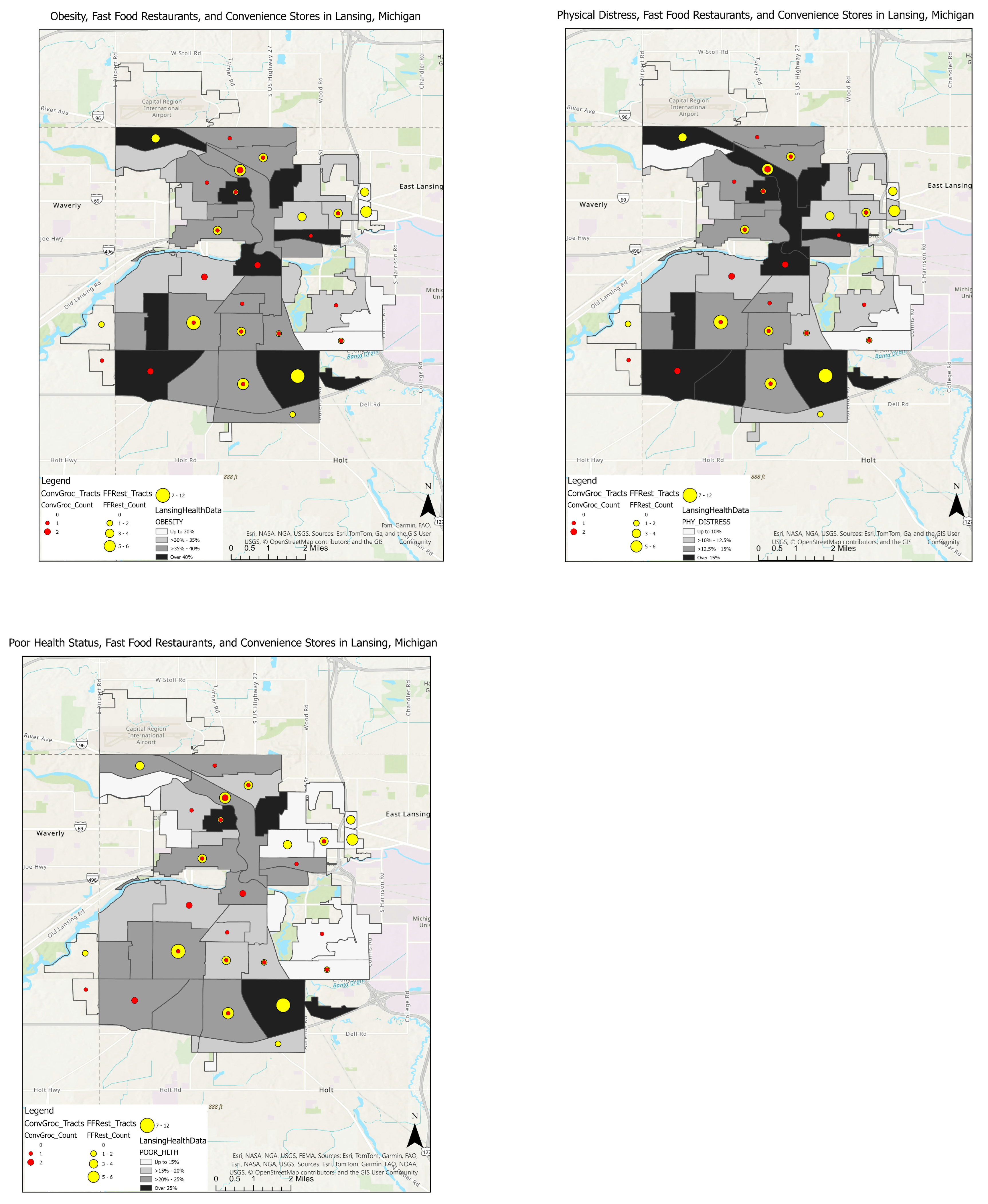
2.1. Study Area
2.2. Data Collection
2.3. Analyses
3. Result
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A


Appendix B
| Dependent Variable | Power Analysis: a1 | Power Analysis: b | Power Analysis: % Explained | Std. Error (CI Lower—CI Upper) |
|---|---|---|---|---|
| Obesity: Fast food direct effect Conv store indirect effect | 0.291 | 0.801 | 0.428 | 0.094 (−0.120–0.249) 10.342 (0.188–50.450) |
| Cholesterol: Fast food direct effect Conv store indirect effect | 0.291 | −0.100 | 0.011 | 0.153 (−0.106–0.494) 10.342 (0.188–50.450) |
| BP Fast food direct effect Conv store indirect effect | 0.291 | 0.333 | 0.129 | 0.216 (−0.167–0.680) 10.342 (0.188–50.450) |
| Diabetes: Fast food direct effect Conv store indirect effect | 0.291 | 0.555 | 0.326 | 0.078 (0.015–0.322) 10.342 (0.188–50.450) |
| Depression: Fast food direct effect Conv store indirect effect | 0.291 | 0.573 | 0.337 | 0.070 (−0.181–0.093) 10.342 (0.188–50.450) |
| CHD: Fast food direct effect Conv store indirect effect | 0.291 | 0.272 | 0.079 | 0.041 (0.029–0.189) 10.342 (0.188–50.450) |
| Physical distress: Fast food direct effect Conv store indirect effect | 0.291 | 0.827 | 0.434 | 0.059 (−0.014–0.219) 10.342 (0.188–50.450) |
| Mental distress: Fast food direct effect Conv store indirect effect | 0.291 | 0.801 | 0.428 | 0.075 (−0.173–0.120) 10.342 (0.188–50.450) |
| Poor health status: Fast food direct effect Conv store indirect effect | 0.291 | 0.905 | 0.452 | 0.101 (−0.007–0.390) 10.342 (0.188–50.450) |
| COPD: Fast food direct effect Conv store indirect effect | 0.291 | 0.680 | 0.397 | 0.059 (0.018–0.248) 10.342 (0.188–50.450) |
References
- Center for Disease Control. About Chronic Diseases. Available online: https://www.cdc.gov/chronic-disease/about/index.html (accessed on 27 September 2025).
- Boone-Heinonen, J.; Gordon-Larsen, P.; Kiefe, C.; Shikany, J.; Lewis, C.; Popkin, B.M. Fast Food restaurants and food stores longitudinal associations with diet in young to middle-aged adults: The CARDIA study. Arch. Intern. Med. 2011, 171, 1162–1170. [Google Scholar] [CrossRef] [PubMed]
- Ahern, M.; Brown, C.; Dukas, S. A national study of the association between food environments and county-level health outcomes. J. Rural Health 2011, 27, 367–379. [Google Scholar] [CrossRef] [PubMed]
- Galvez, M.; Hong, L.; Choi, E.; Liao, L.; Godbold, J.; Brenner, B. Childhood obesity and neighborhood food-store availability in an inner-city community. Acad. Pediatr. 2009, 9, 339–343. [Google Scholar] [CrossRef]
- Block, J.P.; Scribner, R.A.; DeSalvo, K.B. Fast-food, race/ethnicity, and income: A geographic analysis. Am. J. Prev. Med. 2004, 27, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Powell, L.M.; Slater, S.; Mirtcheva, D.; Bao, Y.; Chaloupka, F.J. Food store availability and neighborhood characteristics in the United States. Prev. Med. 2006, 44, 189–195. [Google Scholar] [CrossRef]
- Holston, D.; Cater, M.; Tuuri, G.; O’Neil, C. Exploring the rural nutrition environment: A case study from Louisiana. Curr. Dev. Nutr. 2019, 2, nzy033. [Google Scholar] [CrossRef]
- Bower, K.M.; Thorpe, R.; Rohde, C.; Gaskin, D.J. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Prev. Med. 2014, 58, 33–39. [Google Scholar] [CrossRef]
- Smoyer-Tomic, K.; Spence, J.; Raine, K.; Amrhein, C.; Cameron, N.; Yasenovskiy, V.; Cutumisu, N.; Hemphill, E.; Healy, J. The association between neighborhood socioeconomic status and exposure to supermarkets and fast food outlets. Health Place 2008, 14, 740–754. [Google Scholar] [CrossRef]
- LeDoux, T.; Vojnovic, I. Examining the role between the residential neighborhood food environment and diet among low-income households in Detroit, Michigan. Appl. Geogr. 2014, 55, 9–18. [Google Scholar] [CrossRef]
- Burns, C.M.; Inglis, A.D. Measuring food access in Melbourne: Access to healthy and fast foods by car, bus and foot in an urban municipality in Melbourne. Health Place 2007, 13, 877–885. [Google Scholar] [CrossRef]
- Gordon, C.; Purciel-Hill, M.; Ghai, N.R.; Kaufman, L.; Graham, R.; Van Wye, G. Measuring food deserts in New York City’s low-income neighborhoods. Health Place 2011, 17, 696–700. [Google Scholar] [CrossRef]
- Sloane, D.; Diamant, A.; Lewis, L.; Yancey, A.; Flynn, G.; Nascimento, L.; McCarthy, W.; Guinyard, J.; Cousineau, M. Improving the nutritional resource environment for healthy living through community-based participatory research. J. Gen. Intern. Med. 2003, 18, 568–575. [Google Scholar] [CrossRef] [PubMed]
- Zenk, S.; Lachance, L.; Schultz, A.; Mentz, G.; Kannan, S.; Ridella, W. Neighborhood retail food environment and fruit and vegetable intake in multiethnic urban population. Am. J. Health Promot. 2009, 23, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Gundersen, C.; Ziliak, J.P. Food Insecurity And Health Outcomes. Health Aff. 2015, 34, 1830–1839. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.; Laska, M.; Neumark-Sztainer, D. Food insecurity, diet quality, home food availability, and health risk behaviors among emerging adults: Findings from the EAT 2010–2018 study. Am. J. Public Health 2020, 110, 1422–1428. [Google Scholar] [CrossRef]
- Wennberg, A.M.; Ek, S.; Na, M. Food insecurity, vision impairment, and longitudinal risk of frailty and falls in The National Health and Aging Trends Study. J. Frailty Aging 2024, 13, 285–292. [Google Scholar] [CrossRef]
- de Cássia Ribeiro-Silva, R.; Oliveira-Assis, A.M.; Junqueira, S.B.; Fiaccone, R.L.; Dos Santos, S.M.C.; Barreto, M.L.; de Jesus Pinto, E.; da Silva, L.A.; Rodrigues, L.C.; Alcantara-Neves, N.M. Food and nutrition insecurity: A marker of vulnerability to asthma symptoms. Public Health Nutr. 2014, 17, 14–19. [Google Scholar] [CrossRef]
- Wang, H.; El-Abbadi, N. Food insecurity, race and ethnicity, and cognitive function among United States older adults. J. Nutr. 2024, 154, 233–242. [Google Scholar] [CrossRef]
- Dubowitz, T.; Ghosh-Dastidar, M.; Eibner, C.; Slaughter, M.; Fernandes, M.; Whitsel, E.; Bird, C.; Jewell, A.; Margolis, K.; Li, W.; et al. The Women’s Health Initiative: The food environment, neighborhood socioeconomic status, BMI, and blood pressure. Obesity 2012, 20, 862–871. [Google Scholar] [CrossRef]
- Larson, N.I.; Story, M.T.; Nelson, M.C. Neighborhood Environments Disparities in Access to Healthy Foods in the US. Am. J. Prev. Med. 2009, 36, 74–81. [Google Scholar] [CrossRef]
- Rundle, A.; Neckerman, K.; Freeman, L.; Lovasi, G.; Purciel, M.; Quinn, J.; Richards, C.; Sircar, N.; Weiss, C. Neighborhood food environment and walkability predict obesity and New York city. Environ. Health Persp. 2009, 117, 442–447. [Google Scholar] [CrossRef]
- Bodor, J.; Rice, J.; Farley, T.; Swalm, C.; Rose, D. The association between obesity and urban food environments. J. Urban Health 2010, 87, 771–781. [Google Scholar] [CrossRef] [PubMed]
- Burgoine, T.; Forouhi, N.; Griffin, S.; Wareham, N.; Monsivais, P. Associations between exposure to takeaway food outlets, takeaway food consumption, and body weight in Cambridgeshire, UK: Population based, cross sectional study. BMJ Brit. Med. J. 2014, 348, g1464. [Google Scholar] [CrossRef]
- Burgoine, T.; Sarkar, C.; Webster, C.; Monsivais, P. Examining the interaction of fast-food outlet exposure and income on diet and obesity: Evidence from 51,361 UK Biobank participants. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 71. [Google Scholar] [CrossRef] [PubMed]
- Cooksey Stowers, K.; Jiang, Q.; Atoloye, A.; Lucan, S.; Gans, K. Racial differences in perceived food swamp and food desert exposure and disparities in self-reported dietary habits. Int. J. Environ. Res. Public Health 2020, 17, 7143. [Google Scholar] [CrossRef]
- Murphy, M.; Badland, H.; Jordan, H.; Koohsari, M.; Giles-Corti, B. Local food environments, suburban development, and BMI: A mixed methods study. Int. J. Environ. Res. Public Health 2018, 15, 1392. [Google Scholar] [CrossRef]
- Li, F.; Harmer, P.; Cardinal, B.; Bosworth, M.; Johnson-Shelton, D. Obesity and the built environment: Does the density of neighborhood fast-food outlets matter? Am. J. Health Promot. 2009, 23, 203–209. [Google Scholar] [CrossRef]
- Kraft, A.N.; Thatcher, E.J.; Zenk, S.N. Neighborhood food environment and health outcomes in U.S. low-socioeconomic status, racial/ethnic minority, and rural populations: A systematic review. J. Health Care Poor Underserved 2020, 31, 1078–1114. [Google Scholar] [CrossRef]
- Rosenberg, D.E.; Cruz, M.F.; Mooney, S.J.; Bobb, J.F.; Drewnowski, A.; Moudon, A.V.; Cook, A.J.; Hurvitz, P.M.; Lozano, P.; Anau, J.; et al. Neighborhood built and food environment in relation to glycemic control in people with type 2 diabetes in the Moving to Health Study. Health Place 2024, 86, 103216. [Google Scholar] [CrossRef]
- Phillips, A.; Rodriguez, H. Adults with diabetes residing in “food swamps” have higher hospitalization rates. Health Serv. Res. 2019, 54, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Mujahid, M.; Roux, A.; Morenoff, J.; Raghunathan, T.; Cooper, R.; Ni, H.; Shea, S. Neighborhood characteristics and hypertension. Epidemiology 2008, 19, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Landaeta-Diaz, L.; Vergara-Perucich, F.; Aguirre-Nunez, C.; Cancino-Contrearas, F.; Correa-Parra, J.; Ulloa-Leon, F. Urban food deserts and cardiovascular health: Evaluating the impact of nutritional inequities on elderly populations in Santiago. Appl. Sci. 2024, 14, 7575. [Google Scholar] [CrossRef]
- Ly, C.; Essman, M.; Zimmer, C.; Ng, S.W. Developing an index to estimate the association between the food environment and CVD mortality rates. Health Place 2020, 66, 102469. [Google Scholar] [CrossRef]
- Mooney, S.J.; Lemaitre, R.N.; Siscovick, D.S.; Hurvitz, P.; Goh, C.E.; Kaufman, T.K.; Zulaika, G.; Sheehan, D.M.; Sotoodehnia, N.; Lovasi, G.S. Neighborhood food environment, dietary fatty acid biomarkers, and cardiac arrest risk. Health Place 2018, 53, 128–134. [Google Scholar] [CrossRef] [PubMed]
- U.S. Census Bureau; U.S. Department of Commerce. 2024 ACS Demographic and Housing Estimates. Available online: https://www.socialexplorer.com/explore-tables (accessed on 15 September 2024).
| Income | Food | Convenience Stores | Older Adults | Total Population | |
|---|---|---|---|---|---|
| % of Variance Explained | 40.912 | 19.921 | 8.833 | 5.849 | 5.270 |
| Variables within each component (ordered by their contributing roles and factor loadings shown in parentheses) | Food insecurity (0.952) On food stamps (0.949) No transportation (0.942) Housing insecurity (0.942) No insurance (0.913) Poverty (0.820) Housing cost burden (0.773) Percent minority (0.739) High school degree (0.736) | All restaurants (0.945) Ethical restaurants (0.910) Fast-food restaurants (0.842) All grocery stores (0.808) | Unemployment (0.825) Convenience stores (0.771) | No Internet (0.638) Older adults (0.609) | Total Population (0.969) |
| Dependent Variables | Obesity | Cholesterol | BP | Diabetes | Depression | CHD | Physical Distress | Mental Distress | Poor Health | COPD |
|---|---|---|---|---|---|---|---|---|---|---|
| Income t value | 0.859 *** 11.962 | 0.541 *** 4.080 | 0.713 *** 6.381 | 0.573 *** 4.911 | 0.400 *** 2.877 | 0.848 *** 10.908 | 0.835 *** 12.454 | 0.903 *** 15.310 | 0.731 *** 6.917 | |
| Food t value | 0.133 * 1.852 | −0.004 −0.031 | 0.140 1.248 | 0.222 * 1.904 | 0.121 0.868 | 0.158 ** 2.028 | 0.263 *** 3.930 | 0.191 *** 3.236 | 0.150 1.418 | |
| Conv_Stores t value | 0.193 ** 2.692 | 0.075 0.569 | 0.026 0.234 | 0.271 ** 2.327 | −0.008 −0.056 | 0.169 ** 20.177 | 0.208 *** 3.107 | 0.135 ** 2.293 | 0.144 1.360 | |
| OA t value | 0.018 0.245 | 0.233 * 1.758 | 0.127 1.135 | −0.056 −0.483 | 0.347 ** 2.500 | 0.052 0.670 | −0.076 −1.135 | 0.012 0.212 | 0.136 1.289 | |
| Tot0. Pop0. t value | −0.143 * −1.997 | 0.121 0.913 | 0.069 0.621 | −0.238 ** −2.039 | 0.097 0.700 | −0.082 −1.057 | −0.149 ** −2.226 | −0.064 −1.077 | −0.051 −0.487 | |
| R2 | 0.788 | 0.279 | 0.488 | 0.442 | 0.208 | 0.752 | 0.816 | 0.857 | 0.542 |
| Food Insecurity | Fast-Food Restaurants | Convenience Stores | Older Adults | Total Population | |
|---|---|---|---|---|---|
| Food Insecurity | 1 | ||||
| Fast-Food Restaurants | 0.2045 | 1 | |||
| Convenience Stores | 0.3275 | 0.2701 | 1 | ||
| Older Adults | −0.5192 | 0.1086 | −0.2025 | 1 | |
| Total Population | −0.1498 | 0.1152 | 0.0412 | 0.3049 | 1 |
| VIF | 1.571 | 1.189 | 1.200 | 1.580 | 1.121 |
| Dependent Variables | Obesity | Cholesterol | BP | Diabetes | Depression | CHD | Phy. Distress | Mtl. Distress | Poor Health | COPD |
|---|---|---|---|---|---|---|---|---|---|---|
| Food_Insecurity t value | 0.910 *** 8.471 | 0.331 ** 2.148 | 0.830 *** 6.045 | 0.938 *** 7.716 | 0.301 ** 2.165 | 0.740 *** 5.153 | 0.947 *** 9.612 | 0.564 *** 5.794 | 0.968 *** 13.121 | 0.897 *** 7.214 |
| FF_Rest t value | −0.012 −0.124 | −0.185 −10.381 | −0.111 −0.926 | 0.027 0.251 | 0.135 1.129 | 0.074 0.590 | 0.036 0.423 | 0.139 1.642 | 0.070 10.093 | 0.051 0.474 |
| Conv_Stores t value | 0.089 0.943 | 0.090 0.668 | 0.074 0.619 | −0.052 −0.492 | 0.079 0.657 | −0.034 −0.272 | 0.027 0.317 | −0.015 −0.173 | −0.018 −0.279 | 0.018 0.169 |
| OA t value | 0.200 * 1.854 | 0.771 *** 4.993 | 0.636 *** 4.615 | 0.437 *** 3.582 | −0.408 *** −2.951 | 0.636 *** 4.413 | 0.195 * 1.971 | −0.372 *** −3.815 | 0.087 1.182 | 0.355 *** 2.845 |
| Tot. Pop. t value | −0.006 −0.065 | 0.080 0.614 | 0.119 1.028 | 0.128 1.242 | −0.208 * −1.786 | 0.078 0.641 | 0.032 0.380 | −0.141 * −1.719 | 0.039 0.628 | 0.052 0.498 |
| Adj. R2 | 0.692 | 0.366 | 0.496 | 0.605 | 0.493 | 0.448 | 0.741 | 0.747 | 0.855 | 0.586 |
| Cholesterol | BP | Diabetes | Depression | Mental Distress | |
|---|---|---|---|---|---|
| Food Insecurity | 0.186 ** | 0.616 *** | 0.274 *** | 0.100 | 0.274 *** |
| FF_Rest | −0.105 | −0.182 | 0.067 | 0.063 | 0.144 ** |
| Conv_Stores | 0.830 | 0.700 | −0.032 | 0.205 | −0.124 |
| OA | 0.476 *** | 0.592 *** | 0.174 *** | −0.128 ** | −0.205 *** |
| Tot. Pop | 0.000 | 0.000 | 0.000 | −0.000 | −0.000 |
| Model | LAG | OLS | LAG | LAG | LAG |
| Lag Y (rho) | 0.723 *** | n/a | 0.649 ** | 0.361 | 0.196 |
| Spatial Pseudo R2 | 0.460 | n/a | 0.523 | 0.585 | 0.782 |
| A-K Test | Not significant | n/a | Not significant | Not significant | Not significant |
| Dependent Variable | Convenience Stores | Fast-Food Restaurants | Convenience Stores | Fast-Food Restaurants | R2 |
|---|---|---|---|---|---|
| Direct Effects (β) | Indirect Effect (via Food Insecurity as the Mediator) (β) | ||||
| Obesity | 0.488 | 0.065 | 10.571 ** | 0.231 | 0.702 |
| Cholesterol | 0.233 | 0.194 | −0.181 | −0.027 | 0.022 |
| BP | 0.349 | 0.257 | 0.788 * | 0.116 | 0.162 |
| Diabetes | −0.110 | 0.168 ** | 0.602 ** | 0.089 | 0.379 |
| Depression | 0.406 | −0.044 | 0.550 * | 0.187 | 0.374 |
| CHD | −0.014 | 0.109 *** | 0.153 | 0.023 | 0.156 |
| Physical Distress | 0.064 | 0.102 * | 0.957 ** | 0.141 | 0.746 |
| Mental Distress | 0.096 | −0.026 | 10.155 ** | 0.170 | 0.643 |
| Poor Health | −0.125 | 0.191 * | 10.977 ** | 0.291 | 0.866 |
| COPD | −0.013 | 0.133 ** | 0.592 ** | 0.087 | 0.553 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kotval-K, Z.; Nedd, O.R. The Relationship Between Food Environments and Health Outcomes: A Case Study in Lansing, Michigan. Int. J. Environ. Res. Public Health 2025, 22, 1589. https://doi.org/10.3390/ijerph22101589
Kotval-K Z, Nedd OR. The Relationship Between Food Environments and Health Outcomes: A Case Study in Lansing, Michigan. International Journal of Environmental Research and Public Health. 2025; 22(10):1589. https://doi.org/10.3390/ijerph22101589
Chicago/Turabian StyleKotval-K, Zeenat, and Olivia R Nedd. 2025. "The Relationship Between Food Environments and Health Outcomes: A Case Study in Lansing, Michigan" International Journal of Environmental Research and Public Health 22, no. 10: 1589. https://doi.org/10.3390/ijerph22101589
APA StyleKotval-K, Z., & Nedd, O. R. (2025). The Relationship Between Food Environments and Health Outcomes: A Case Study in Lansing, Michigan. International Journal of Environmental Research and Public Health, 22(10), 1589. https://doi.org/10.3390/ijerph22101589







