When Pedestrian Crossings Become Danger Zones: Trauma and Mortality Risks in Elderly Pedestrians
Abstract
1. Introduction
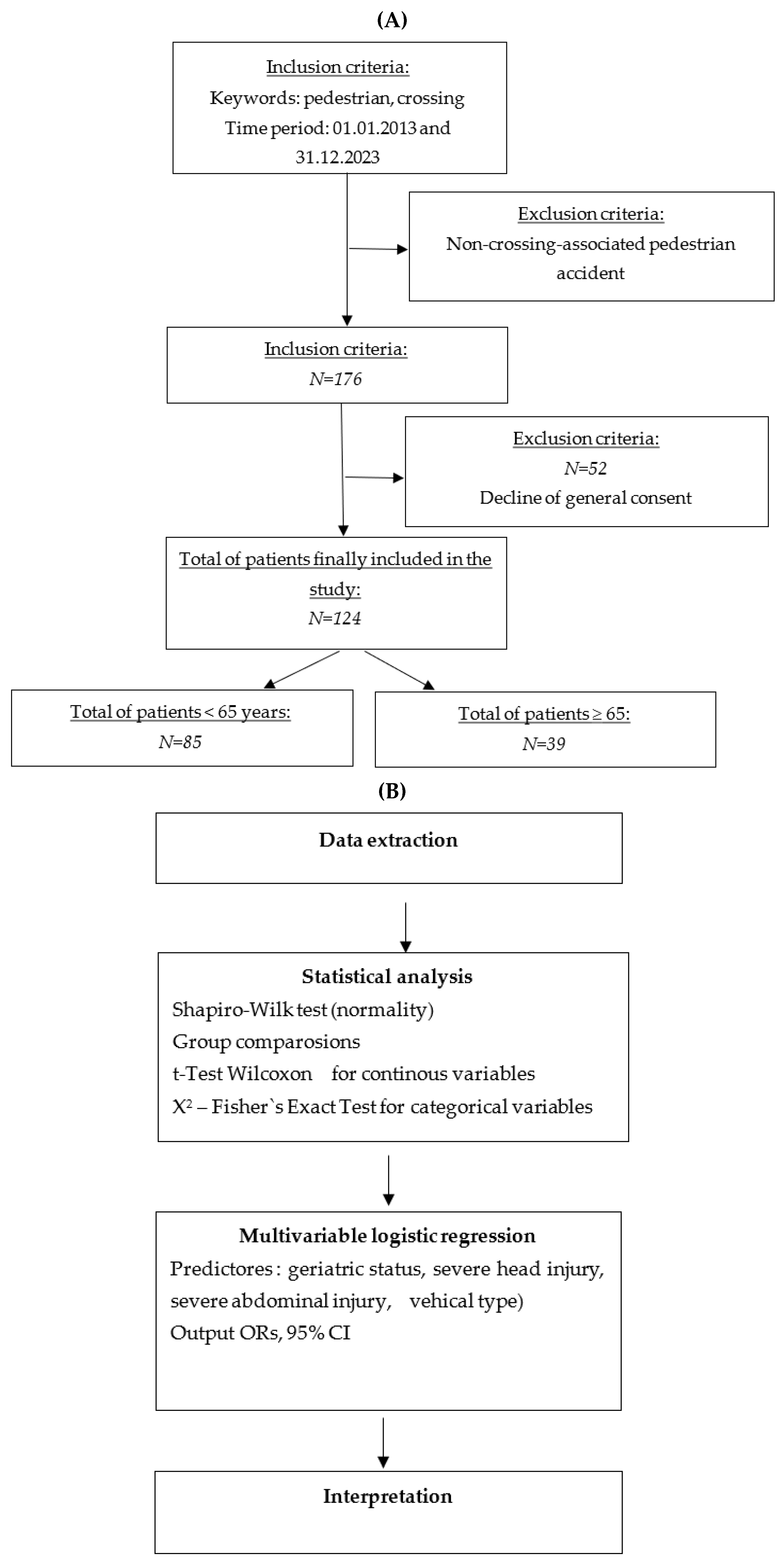
2. Materials and Methods
2.1. Data Collection and Retrospective Survey
2.2. Study Cohort and Data Sources
2.3. Demographics
2.4. Consultation Characteristics
2.5. Accident Type
2.6. Injury Characteristics
2.7. Trauma Severity
2.8. Outcomes
2.9. Statistical Analyses
2.10. Statistical Tests and Rationale
3. Results
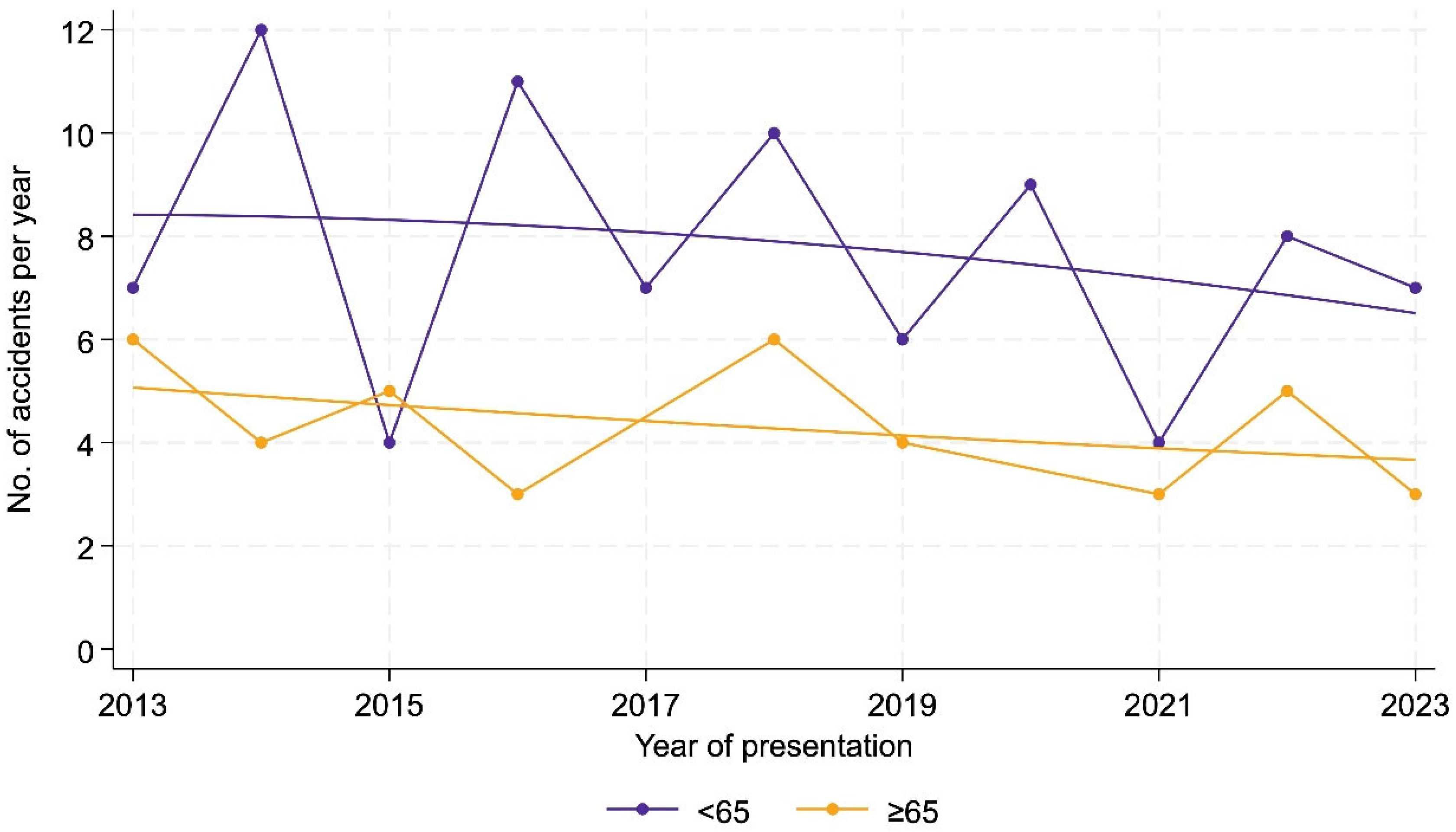
3.1. Design
3.2. Demographics
3.3. Discharge
3.4. Setting of the Accident
3.5. Type of Injury
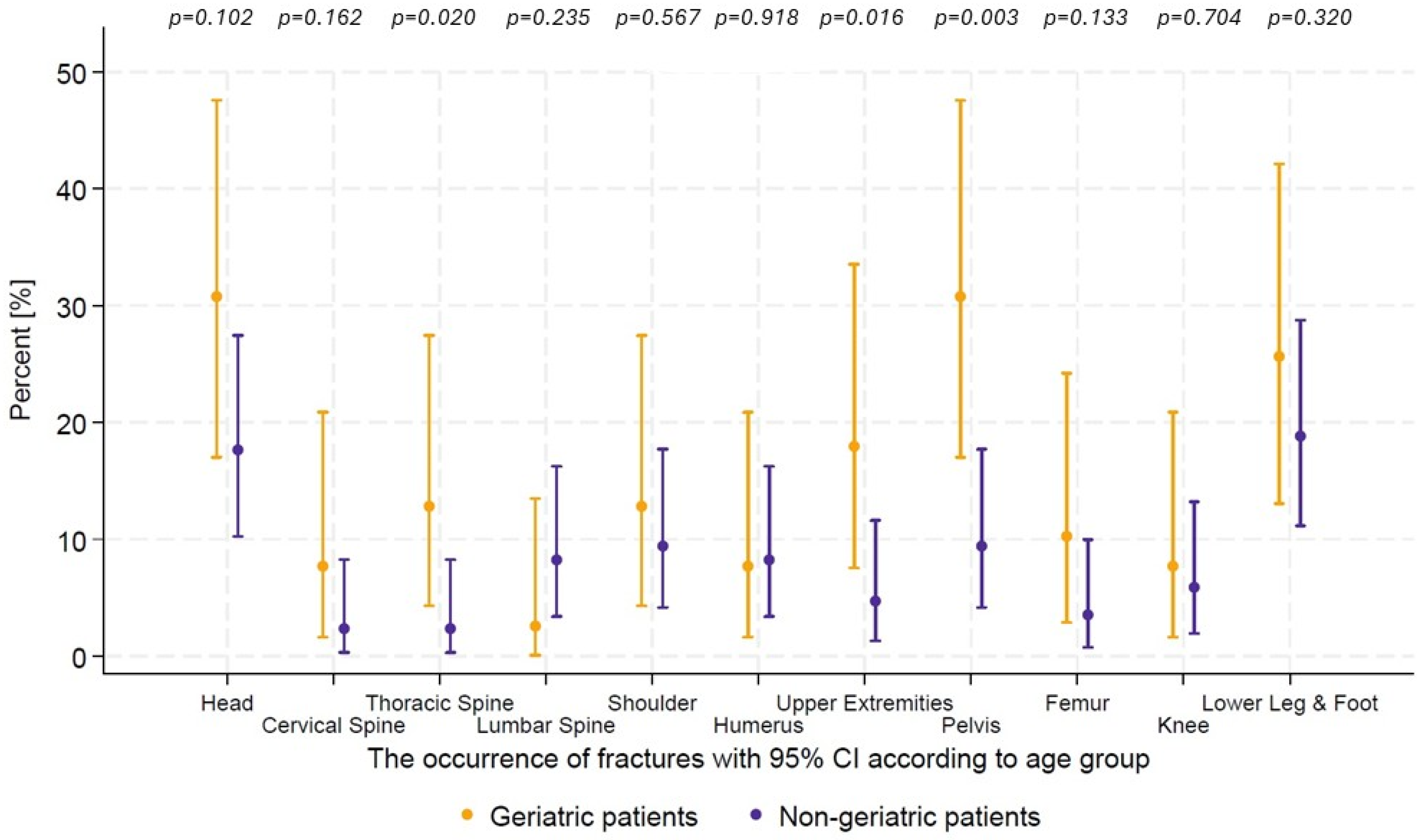
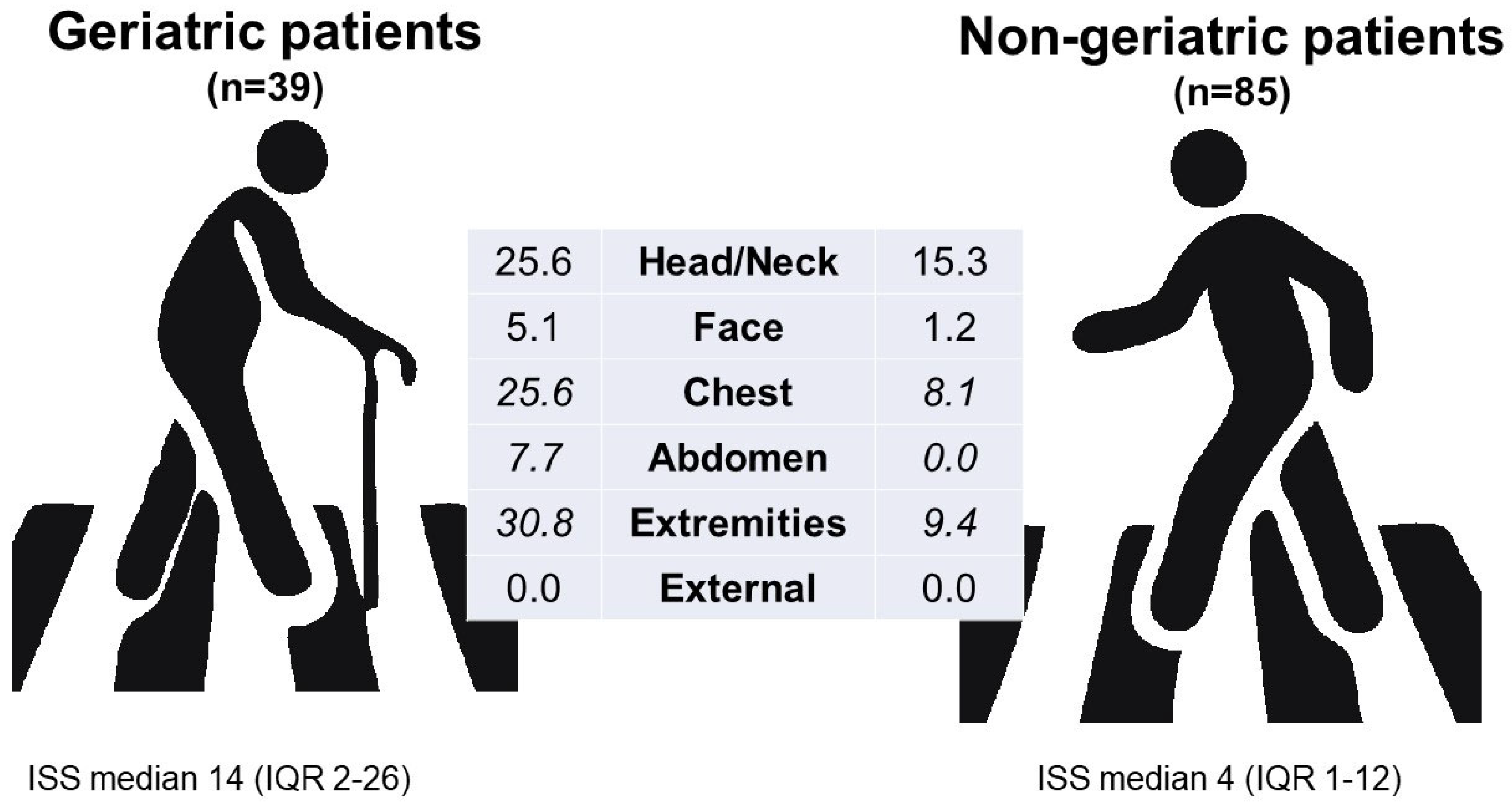
3.6. Pattern of Injury
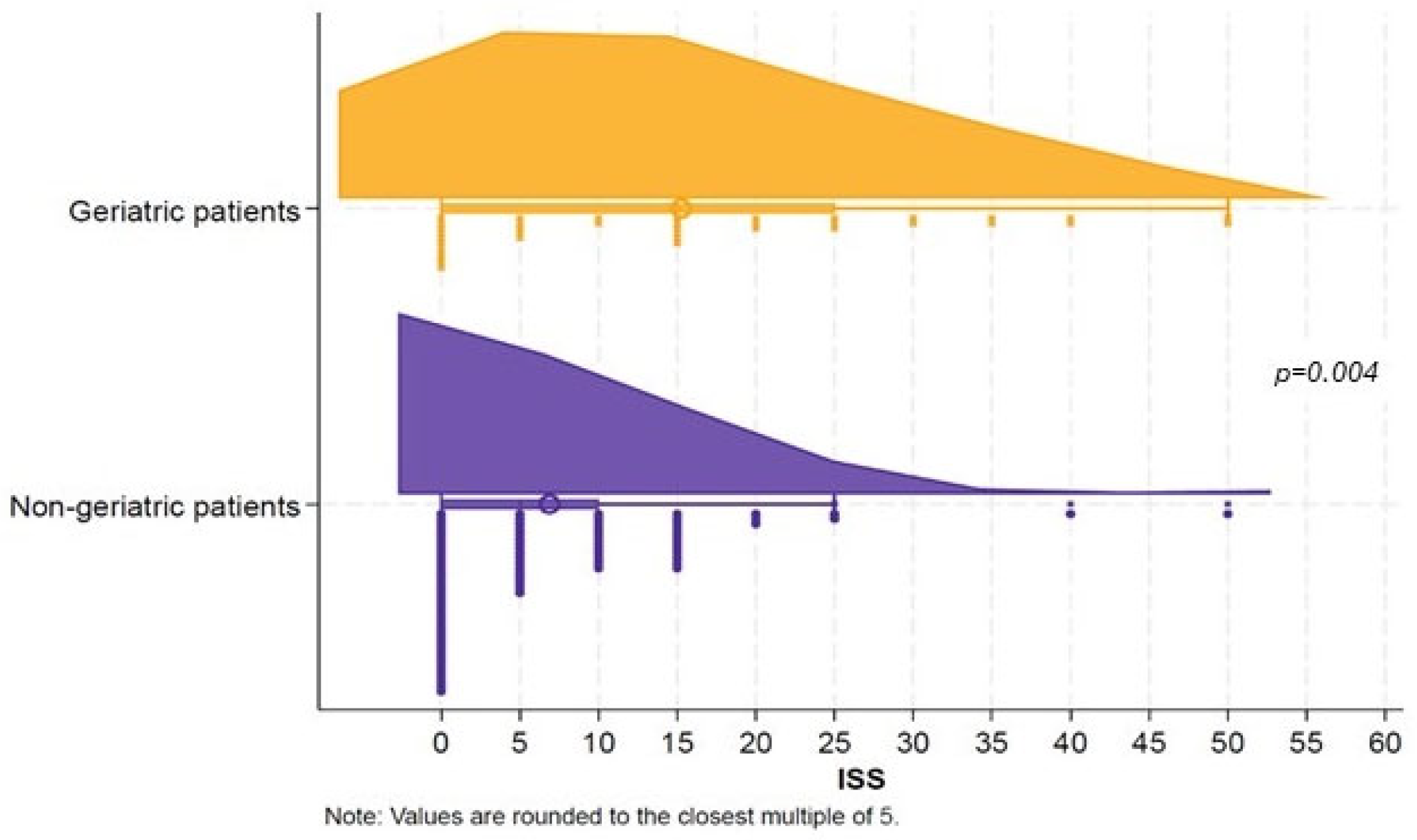
3.7. Outcomes
3.8. Multivariable Logistic Regression
4. Discussion
4.1. General and Study-Informed Recommendations
4.2. Limitations
5. Conclusions
Abbreviations
| AIS | Abbreviated Injury Scale |
| CHF | Swiss Francs |
| CT | Computed Tomography |
| ED | Emergency Department |
| EDH | Epidural Hematoma |
| EMS | Emergency Medical Services |
| GCS | Glasgow Coma Scale |
| HR | Heart Rate |
| ICB | Intracranial Bleeding |
| ICH | Intracerebral Hemorrhage |
| ICU | Intensive Care Unit |
| IQR | Interquartile Range |
| ISS | Injury Severity Score |
| KEK | Kantonale Ethikkommission |
| LOS | Length of Stay |
| MRI | Magnetic Resonance Imaging |
| NTDB | National Trauma Data Bank |
| SAH | Subarachnoid Hemorrhage |
| SBP | Systolic Blood Pressure |
| SD | Standard Deviation |
| SDH | Subdural Hematoma |
| TBI | Traumatic Brain Injury |
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kakara, R.; Bergen, G.; Burns, E.; Stevens, M. Nonfatal and Fatal Falls Among Adults Aged ≥ 65 Years—United States, 2020–2021. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 938–943. [Google Scholar] [CrossRef] [PubMed]
- Colón-Emeric, C.S.; McDermott, C.L.; Lee, D.S.; Berry, S.D. Risk Assessment and Prevention of Falls in Older Community-Dwelling Adults: A Review. Jama 2024, 331, 1397–1406. [Google Scholar] [CrossRef]
- Klukowska-Rötzler, J.; Graber, F.; Exadaktylos, A.; Ziaka, M.; Jakob, D. Gender-Specific Patterns of Injury in Older Adults After a Fall from a Four-Wheeled Walker (Rollator): Retrospective Study from a Swiss Level 1 Trauma Centre. Int. J. Environ. Res. Public Health 2025, 22, 143. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Darvishi, N.; Ahmadipanah, M.; Shohaimi, S.; Mohammadi, M. Global prevalence of falls in the older adults: A comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 334. [Google Scholar] [CrossRef] [PubMed]
- Stewart Williams, J.; Kowal, P.; Hestekin, H.; O’Driscoll, T.; Peltzer, K.; Yawson, A.; Biritwum, R.; Maximova, T.; Salinas Rodríguez, A.; Manrique Espinoza, B.; et al. Prevalence, risk factors and disability associated with fall-related injury in older adults in low- and middle-income countries: Results from the WHO Study on global AGEing and adult health (SAGE). BMC Med. 2015, 13, 147. [Google Scholar] [CrossRef]
- Federal Statistical Office. Transport Accidents and Environmental Impact in Switzerland. Available online: https://www.bfs.admin.ch/bfs/en/home/statistics/mobility-transport/accidents-environmental-impact.html (accessed on 20 September 2025).
- Switzerland Population Ages 65 and Above (% of Total). Available online: https://tradingeconomics.com/switzerland/population-ages-65-and-above-percent-of-total-wb-data.html (accessed on 20 September 2025).
- Allin, S.; Laporte, A. Technology as a Fix for the Age-Old Challenge of Aging in Place? Healthc. Pap. 2024, 22, 5–9. [Google Scholar] [CrossRef]
- Volpi, E.; Nazemi, R.; Fujita, S. Muscle tissue changes with aging. Curr. Opin. Clin. Nutr. Metab. Care 2004, 7, 405–410. [Google Scholar] [CrossRef]
- Cordeiro, T.D.C.; Silva, L.M.; Monteiro, E.A.; Pontes, M.L.F.; Casemiro, F.G.; Rodrigues, R.A.P. Physiological changes in vision during aging: Perceptions of older adults and healthcare providers. Investig. Educ. Enferm. 2021, 39, e11. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Josephson, K.R. Falls and their prevention in elderly people: What does the evidence show? Med. Clin. N. Am. 2006, 90, 807–824. [Google Scholar] [CrossRef]
- Lee, S. Falls associated with indoor and outdoor environmental hazards among community-dwelling older adults between men and women. BMC Geriatr. 2021, 21, 547. [Google Scholar] [CrossRef]
- Global Status Report on Road Safety. 2023. Available online: https://www.who.int/teams/social-determinants-of-health/safety-and-mobility/global-status-report-on-road-safety-2023 (accessed on 20 September 2025).
- Bhattacharya, B.; Maung, A.; Schuster, K.; Davis, K.A. The older they are the harder they fall: Injury patterns and outcomes by age after ground level falls. Injury 2016, 47, 1955–1959. [Google Scholar] [CrossRef]
- Kelsey, J.L.; Berry, S.D.; Procter-Gray, E.; Quach, L.; Nguyen, U.S.; Li, W.; Kiel, D.P.; Lipsitz, L.A.; Hannan, M.T. Indoor and outdoor falls in older adults are different: The maintenance of balance, independent living, intellect, and Zest in the Elderly of Boston Study. J. Am. Geriatr. Soc. 2010, 58, 2135–2141. [Google Scholar] [CrossRef] [PubMed]
- Moreland, B.L.; Kakara, R.; Haddad, Y.K.; Shakya, I.; Bergen, G. A Descriptive Analysis of Location of Older Adult Falls That Resulted in Emergency Department Visits in the United States, 2015. Am. J. Lifestyle Med. 2021, 15, 590–597. [Google Scholar] [CrossRef]
- Burford, K.G.; Itzkowitz, N.G.; Crowe, R.P.; Wang, H.E.; Lo, A.X.; Rundle, A.G. Clinical trauma severity of indoor and outdoor injurious falls requiring emergency medical service response. Inj. Epidemiol. 2024, 11, 36. [Google Scholar] [CrossRef] [PubMed]
- Pfortmueller, C.A.; Kunz, M.; Lindner, G.; Zisakis, A.; Puig, S.; Exadaktylos, A.K. Fall-related emergency department admission: Fall environment and settings and related injury patterns in 6357 patients with special emphasis on the elderly. Sci. World J. 2014, 2014, 256519. [Google Scholar] [CrossRef]
- WHO. Health Data Overview for the Swiss Confederation. Available online: https://data.who.int/countries/756 (accessed on 20 September 2025).
- WHO Europe. Switzerland Physical Activity Facts Sheet. 2019. Available online: https://cdn.who.int/media/docs/librariesprovider2/country-sites/switzerland/switzerland-physical-activity-factsheet-2019-eng.pdf?sfvrsn=30782f62_5&download=true (accessed on 20 September 2025).
- Ciumărnean, L.; Milaciu, M.V.; Negrean, V.; Orășan, O.H.; Vesa, S.C.; Sălăgean, O.; Iluţ, S.; Vlaicu, S.I. Cardiovascular Risk Factors and Physical Activity for the Prevention of Cardiovascular Diseases in the Elderly. Int. J. Environ. Res. Public Health 2021, 19, 207. [Google Scholar] [CrossRef]
- Barnett, A.; Smith, B.; Lord, S.R.; Williams, M.; Baumand, A. Community-based group exercise improves balance and reduces falls in at-risk older people: A randomised controlled trial. Age Ageing 2003, 32, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Keadle, S.K.; McKinnon, R.; Graubard, B.I.; Troiano, R.P. Prevalence and trends in physical activity among older adults in the United States: A comparison across three national surveys. Prev. Med. 2016, 89, 37–43. [Google Scholar] [CrossRef]
- Widodo, A.F.; Chen, C.; Chan, C.W.; Saleh, W.; Wiratama, B.S.; Pai, C.W. Walking against traffic and pedestrian injuries in the United Kingdom: New insights. BMC Public Health 2023, 23, 2205. [Google Scholar] [CrossRef]
- Dai, D. Identifying clusters and risk factors of injuries in pedestrian–vehicle crashes in a GIS environment. J. Transp. Geogr. 2012, 24, 9. [Google Scholar] [CrossRef]
- Kroupa, J. Definition of “polytrauma” and “polytraumatism”. Acta Chir. Orthop. Traumatol. Cech. 1990, 57, 347–360. [Google Scholar]
- Siram, S.M.; Sonaike, V.; Bolorunduro, O.B.; Greene, W.R.; Gerald, S.Z.; Chang, D.C.; Cornwell, E.E., 3rd; Oyetunji, T.A. Does the pattern of injury in elderly pedestrian trauma mirror that of the younger pedestrian? J. Surg. Res. 2011, 167, 14–18. [Google Scholar] [CrossRef]
- Gálvez-Pérez, D.; Guirao, B.; Ortuño, A.; Picado-Santos, L. The Influence of Built Environment Factors on Elderly Pedestrian Road Safety in Cities: The Experience of Madrid. Int. J. Environ. Res. Public Health 2022, 17, 2280. [Google Scholar] [CrossRef]
- Oxley, J.; Fildes, B.; Ihsen, E.; Charlton, J.; Day, R. Differences in traffic judgements between young and old adult pedestrians. Accid. Anal. Prev. 1997, 29, 839–847. [Google Scholar] [CrossRef]
- Dommes, A.; Cavallo, V.; Oxley, J. Functional declines as predictors of risky street-crossing decisions in older pedestrians. Accid. Anal. Prev. 2013, 59, 135–143. [Google Scholar] [CrossRef]
- Tournier, I.; Dommes, A.; Cavallo, V. Review of safety and mobility issues among older pedestrians. Accid. Anal. Prev. 2016, 91, 24–35. [Google Scholar] [CrossRef] [PubMed]
- Arregui-Dalmases, C.; Lopez-Valdes, F.J.; Segui-Gomez, M. Pedestrian injuries in eight European countries: An analysis of hospital discharge data. Accid. Anal. Prev. 2010, 42, 1164–1171. [Google Scholar] [CrossRef] [PubMed]
- Malin, D.; Silla, A.; Mladenović, M. Prevalence and factors associated with pedestrian fatalities and serious injuries: Case Finland. Eur. Transp. Res. Rev. 2020, 12, 18. [Google Scholar] [CrossRef]
- Buehler, R.; Pucher, J. Overview of Walking Rates, Walking Safety, and Government Policies to Encourage More and Safer Walking in Europe and North America. Sustainability 2023, 15, 24. [Google Scholar] [CrossRef]
- Hertach, P.; Huwiler, K.; Aigner-Breuss, E.; Gehlert, T.; Gaster, K.; Holte, H.; Straβgütl, L.; Niemann, S. Age-based medical screening of drivers in Switzerland: An ecological study comparing accident rates with Austria and Germany. Swiss Med. Wkly. 2022, 152, 40005. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, M.J.; Hong, J.Y.; Myung, J.; Roh, Y.H.; Chung, S.P. The elderly age criterion for increased in-hospital mortality in trauma patients: A retrospective cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2021, 29, 133. [Google Scholar] [CrossRef] [PubMed]
- Peterer, L.; Ossendorf, C.; Jensen, K.O.; Osterhoff, G.; Mica, L.; Seifert, B.; Werner, C.M.L.; Simmen, H.P.; Pape, H.C.; Sprengel, K. Implementation of new standard operating procedures for geriatric trauma patients with multiple injuries: A single level I trauma centre study. BMC Geriatr. 2019, 19, 359. [Google Scholar] [CrossRef]
- Werman, H.A.; Erskine, T.; Caterino, J.; Riebe, J.F.; Valasek, T. Development of statewide geriatric patients trauma triage criteria. Prehosp. Disaster Med. 2011, 26, 170–179. [Google Scholar] [CrossRef]
- Zagalioti, S.C.; Fyntanidou, B.; Exadaktylos, A.; Lallas, K.; Ziaka, M. The first positive evidence that training improves triage decisions in Greece: Evidence from emergency nurses at an Academic Tertiary Care Emergency Department. BMC Emerg. Med. 2023, 23, 60. [Google Scholar] [CrossRef]
- Sasse, N.; Ziaka, M.; Brockhus, L.; Müller, M.; Exadaktylos, A.K.; Klukowska-Rötzler, J. Trampolining Accidents in an Adult Emergency Department: Analysis of Trampolining Evolution Regarding Severity and Occurrence of Injuries. Int. J. Environ. Res. Public Health 2022, 19, 1212. [Google Scholar] [CrossRef]
- Dethlefsen, R.; Orlik, L.; Müller, M.; Exadaktylos, A.K.; Scholz, S.M.; Klukowska-Rötzler, J.; Ziaka, M. Work-Related Injuries among Insured Construction Workers Presenting to a Swiss Adult Emergency Department: A Retrospective Study (2016–2020). Int. J. Environ. Res. Public Health 2022, 19, 11294. [Google Scholar] [CrossRef]
- European Road Safety Observatory National Road Safety Profile—Switzerland. Available online: https://road-safety.transport.ec.europa.eu/document/download/1c160fc1-f1dd-4c43-b7ac-5ec120e016e9_en?filename=erso-country-overview-2023-switzerland_1.pdf (accessed on 20 September 2025).
- Gálvez-Pérez, D.; Guirao, B.; Ortuño, A. Analysis of the elderly pedestrian traffic accidents in urban scenarios: The case of the Spanish municipalities. Int. J. Inj. Contr. Saf. Promot. 2024, 31, 376–395. [Google Scholar] [CrossRef]
- Azami-Aghdash, S.; Aghaei, M.H.; Sadeghi-Bazarghani, H. Epidemiology of Road Traffic Injuries among Elderly People; A Systematic Review and Meta-Analysis. Bull. Emerg. Trauma 2018, 6, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Arbizu Fernández, E.; Galbete Jimenez, A.; Belzunegui Otano, T.; Fortún Moral, M.; Echarri Sucunza, A. Analysis of serious trauma injury patterns in Navarre (Spain) (2010–2019). An. Sist. Sanit. Navar. 2024, 29, e1085. [Google Scholar] [CrossRef]
- Etehad, H.; Yousefzadeh-Chabok, S.; Davoudi-Kiakalaye, A.; Moghadam Dehnadi, A.; Hemati, H.; Mohtasham-Amiri, Z. Impact of road traffic accidents on the elderly. Arch. Gerontol. Geriatr. 2015, 61, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Harvey, L.A.; Close, J.C. Traumatic brain injury in older adults: Characteristics, causes and consequences. Injury 2012, 43, 1821–1826. [Google Scholar] [CrossRef]
- Savioli, G.; Ceresa, I.F.; Ciceri, L.; Sciutti, F.; Belliato, M.; Iotti, G.A.; Luzzi, S.; Del Maestro, M.; Mezzini, G.; Lafe, E.; et al. Mild head trauma in elderly patients: Experience of an emergency department. Heliyon 2020, 6, e04226. [Google Scholar] [CrossRef]
- Fakhry, S.M.; Shen, Y.; Garland, J.M.; Wilson, N.Y.; Wyse, R.J.; Morse, J.L.; Hunt, D.L.; Acuna, D.; Dunne, J.; Kurek, S.J.; et al. The burden of geriatric traumatic brain injury on trauma systems: Analysis of 348,800 Medicare inpatient claims. J. Am. Geriatr. Soc. 2023, 71, 516–527. [Google Scholar]
- Scotti, P.; Séguin, C.; Lo, B.W.Y.; de Guise, E.; Troquet, J.M.; Marcoux, J. Antithrombotic agents and traumatic brain injury in the elderly population: Hemorrhage patterns and outcomes. J. Neurosurg. 2020, 133, 486–495. [Google Scholar] [CrossRef]
- Oliveros, E.; Patel, H.; Kyung, S.; Fugar, S.; Goldberg, A.; Madan, N.; Williams, K.A. Hypertension in older adults: Assessment, management, and challenges. Clin. Cardiol. 2020, 43, 99–107. [Google Scholar] [PubMed]
- Hsiao, K.Y.; Lin, L.C.; Li, W.C.; Lin, M.H.; Wang, C.H.; Chen, K.H. The association between hypertension and traumatic intracranial haemorrhage. Injury 2015, 46, 859–862. [Google Scholar] [CrossRef] [PubMed]
- Bettschen, D.; Tsichlaki, D.; Chatzimichail, E.; Klukowska-Rötzler, J.; Müller, M.; Sauter, T.C.; Exadaktylos, A.K.; Ziaka, M.; Doulberis, M.; Burkhard, J.P. Epidemiology of maxillofacial trauma in elderly patients receiving oral anticoagulant or antithrombotic medication; a Swiss retrospective study. BMC Emerg. Med. 2024, 24, 121. [Google Scholar] [CrossRef]
- Dunham, C.M.; Hoffman, D.A.; Huang, G.S.; Omert, L.A.; Gemmel, D.J.; Merrell, R. Traumatic intracranial hemorrhage correlates with preinjury brain atrophy, but not with antithrombotic agent use: A retrospective study. PLoS ONE 2014, 9, e109473. [Google Scholar] [CrossRef]
- McElroy, L.M.; Juern, J.J.; Bertleson, A.; Xiang, Q.; Szabo, A.; Weigelt, J. A single urban center experience with adult pedestrians struck by motor vehicles. WMJ 2013, 112, 117–122. [Google Scholar] [PubMed]
- Rod, J.E.; Oviedo-Trespalacios, O.; Senserrick, T.; King, M. Older adult pedestrian trauma: A systematic review, meta-analysis, and GRADE assessment of injury health outcomes from an aggregate study sample of 1 million pedestrians. Accid. Anal. Prev. 2021, 152, 105970. [Google Scholar] [CrossRef]
- Burkhard, J.P.M.; Pitteloud, C.; Klukowska-Rötzler, J.; Exadaktylos, A.K.; Iizuka, T.; Schaller, B. Changing trends in epidemiology and management of facial trauma in a Swiss geriatric population. Gerodontology 2019, 36, 358–364. [Google Scholar] [CrossRef]
- Kashkooe, A.; Yadollahi, M.; Pazhuheian, F. What factors affect length of hospital stay among trauma patients? A single-center study, Southwestern Iran. Chin. J. Traumatol. 2020, 23, 176–180. [Google Scholar] [CrossRef]
- Olszewski, P.; Szagała, P.; Wolański, M.; Zielińska, A. Pedestrian fatality risk in accidents at unsignalized zebra crosswalks in Poland. Accid. Anal. Prev. 2015, 84, 83–91. [Google Scholar] [CrossRef]
- Mathew, P.J.; Jehan, F.; Kulvatunyou, N.; Khan, M.; O’Keeffe, T.; Tang, A.; Gries, L.; Hamidi, M.; Zakaria, E.R.; Joseph, B. The burden of excess length of stay in trauma patients. Am. J. Surg. 2018, 216, 881–885. [Google Scholar] [CrossRef] [PubMed]
- Bala, M.; Kashuk, J.L.; Willner, D.; Kaluzhni, D.; Bdolah-Abram, T.; Almogy, G. Looking beyond discharge: Clinical variables at trauma admission predict long term survival in the older severely injured patient. World J. Emerg. Surg. 2014, 9, 10. [Google Scholar] [CrossRef]
- Takanishi, D.M., Jr.; Yu, M.; Morita, S.Y. Increased fatalities and cost of traumatic injuries in elderly pedestrians in Hawaii: A challenge for prevention and outreach. Asia Pac. J. Public. Health 2008, 20, 327–339. [Google Scholar] [CrossRef]
- Chong, S.L.; Chiang, L.W.; Allen, J.C., Jr.; Fleegler, E.W.; Lee, L.K. Epidemiology of Pedestrian-Motor Vehicle Fatalities and Injuries, 2006–2015. Am. J. Prev. Med. 2018, 55, 98–105. [Google Scholar] [CrossRef]
- Peng, R.Y.; Bongard, F.S. Pedestrian versus motor vehicle accidents: An analysis of 5,000 patients. J. Am. Coll. Surg. 1999, 189, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Demetriades, D.; Murray, J.; Martin, M.; Velmahos, G.; Salim, A.; Alo, K.; Rhee, P. Pedestrians injured by automobiles: Relationship of age to injury type and severity. J. Am. Coll. Surg. 2004, 199, 382–387. [Google Scholar] [CrossRef]
- Clement, N.D.; Tennant, C.; Muwanga, C. Polytrauma in the elderly: Predictors of the cause and time of death. Scand. J. Trauma Resusc. Emerg. Med. 2010, 18, 26. [Google Scholar] [CrossRef] [PubMed]
- Schubert, A.; Babisch, S.; Scanlon, J.M.; Campolettano, E.T.; Roessler, R.; Unger, T.; McMurry, T.L. Passenger and heavy vehicle collisions with pedestrians: Assessment of injury mechanisms and risk. Accid. Anal. Prev. 2023, 190, 107139. [Google Scholar] [CrossRef]
- Niebuhr, T.; Junge, M.; Rosén, E. Pedestrian injury risk and the effect of age. Accid. Anal. Prev. 2016, 86, 121–128. [Google Scholar] [CrossRef]
- Matsui, Y.; Oikawa, S.; Aoki, Y.; Sekine, M.; Mitobe, K. Features of the Vision of Elderly Pedestrians when Crossing a Road. Stapp. Car Crash J. 2014, 58, 233–250. [Google Scholar]
- Noh, Y.; Kim, M.; Yoon, Y. Elderly pedestrian safety in a rapidly aging society-Commonality and diversity between the younger-old and older-old. Traffic Inj. Prev. 2018, 19, 874–879. [Google Scholar] [CrossRef]
- Larsson, L.; Degens, H.; Li, M.; Salviati, L.; Lee, Y.I.; Thompson, W.; Kirkland, J.L.; Sandri, M. Sarcopenia: Aging-Related Loss of Muscle Mass and Function. Physiol. Rev. 2019, 99, 427–511. [Google Scholar] [CrossRef] [PubMed]
- Fang, T.; Xu, F.; Zou, Z. Causal Factors in Elderly Pedestrian Traffic Injuries Based on Association Analysis. Appl. Sci. 2025, 15, 15. [Google Scholar] [CrossRef]
- Goetzl, E.J.; Feeley, B. Musculoskeletal Disorders of the Elderly. Am. J. Med. 2025, 138, 1197–1200. [Google Scholar] [CrossRef] [PubMed]
- Samaras, N.; Chevalley, T.; Samaras, D.; Gold, G. Older patients in the emergency department: A review. Ann. Emerg. Med. 2010, 56, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Lucke, J.A.; Mooijaart, S.P.; Heeren, P.; Singler, K.; McNamara, R.; Gilbert, T.; Nickel, C.H.; Castejon, S.; Mitchell, A.; Mezera, V.; et al. Providing care for older adults in the Emergency Department: Expert clinical recommendations from the European Task Force on Geriatric Emergency Medicine. Eur. Geriatr. Med. 2022, 13, 309–317. [Google Scholar] [CrossRef]
- Legramante, J.M.; Morciano, L.; Lucaroni, F.; Gilardi, F.; Caredda, E.; Pesaresi, A.; Coscia, M.; Orlando, S.; Brandi, A.; Giovagnoli, G.; et al. Frequent Use of Emergency Departments by the Elderly Population When Continuing Care Is Not Well Established. PLoS ONE 2016, 11, e0165939. [Google Scholar] [CrossRef]
- Evans, C.S.; Platts-Mills, T.F.; Fernandez, A.R.; Grover, J.M.; Cabanas, J.G.; Patel, M.D.; Vilke, G.M.; Brice, J.H. Repeated Emergency Medical Services Use by Older Adults: Analysis of a Comprehensive Statewide Database. Ann. Emerg. Med. 2017, 70, 506–515.e3. [Google Scholar] [CrossRef] [PubMed]
- Platts-Mills, T.F.; Leacock, B.; Cabañas, J.G.; Shofer, F.S.; McLean, S.A. Emergency medical services use by the elderly: Analysis of a statewide database. Prehosp. Emerg. Care 2010, 14, 329–333. [Google Scholar] [CrossRef] [PubMed]
- BFU. Fussgängerstreifen Überqueren: Haben Fussgängerinnen und Fussgänger Immer Vortritt? Available online: https://www.bfu.ch/de/services/rechtsfragen/haben-fussgaenger-immer-vortritt (accessed on 20 September 2025).
- Wilmut, K.; Purcell, C. Why Are Older Adults More at Risk as Pedestrians? A Systematic Review. Hum. Factors 2022, 64, 1269–1291. [Google Scholar] [CrossRef]
- Schumacher, J.G.; Deimling, G.T.; Meldon, S.; Woolard, B. Older adults in the Emergency Department: Predicting physicians’ burden levels. J. Emerg. Med. 2006, 30, 455–460. [Google Scholar] [CrossRef]
- Leipzig, R.M.; Granville, L.; Simpson, D.; Anderson, M.B.; Sauvigné, K.; Soriano, R.P. Keeping granny safe on July 1: A consensus on minimum geriatrics competencies for graduating medical students. Acad. Med. 2009, 84, 604–610. [Google Scholar] [CrossRef]
- Hesselink, G.; Demirbas, M.; Rikkert, M.O.; Schoon, Y. Geriatric Education Programs for Emergency Department Professionals: A Systematic Review. J. Am. Geriatr. Soc. 2019, 67, 2402–2409. [Google Scholar] [CrossRef]
- Meakes, S.; Enninghorst, N.; Weaver, N.; Hardy, B.M.; Balogh, Z.J. Long-term functional outcomes in polytrauma: A fundamentally new approach is needed in prediction. Eur. J. Trauma Emerg. Surg. 2024, 50, 1439–1452. [Google Scholar] [CrossRef]
- Li, H.; Ma, Y.F. New injury severity score (NISS) outperforms injury severity score (ISS) in the evaluation of severe blunt trauma patients. Chin. J. Traumatol. 2021, 24, 261–265. [Google Scholar] [CrossRef]
- Simmel, S.; Drisch, S.; Haag, S.; Bühren, V. Long-term results after multiple trauma with ISS ≥ 25. Outcome and predictors of quality of life. Chirurg 2013, 84, 771–779. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.; Ng, Y.S.; Koh, G.C.; De Silva, D.A.; Earnest, A.; Barbier, S. Disability impacts length of stay in general internal medicine patients. J. Gen. Intern. Med. 2014, 29, 885–890. [Google Scholar] [CrossRef] [PubMed]

| Variables | Total | Age < 65 | Age ≥ 65 | p Value |
|---|---|---|---|---|
| (n = 124) | (n = 85) | (n = 39) | ||
| Sex | 0.53 | |||
| Female | 75 (60.5) | 53 (62.4) | 22 (56.4) | |
| Male | 49 (39.5) | 32 (37.6) | 17 (43.6) | |
| Year of presentation | 0.204 | |||
| 2013 | 13 (10.5) | 7 (8.2) | 6 (15.4) | |
| 2014 | 16 (12.9) | 12 (14.1) | 4 (10.3) | |
| 2015 | 9 (7.3) | 4 (4.7) | 5 (12.8) | |
| 2016 | 14 (11.3) | 11 (12.9) | 3 (7.7) | |
| 2017 | 7 (5.6) | 7 (8.2) | 0 (0.0) | |
| 2018 | 16 (12.9) | 10 (11.8) | 6 (15.4) | |
| 2019 | 10 (8.1) | 6 (7.1) | 4 (10.3) | |
| 2020 | 9 (7.3) | 9 (10.6) | 0 (0.0) | |
| 2021 | 7 (5.6) | 4 (4.7) | 3 (7.7) | |
| 2022 | 13 (10.5) | 8 (9.4) | 5 (12.8) | |
| 2023 | 10 (8.1) | 7 (8.2) | 3 (7.7) | |
| Month of presentation | 0.120 | |||
| January | 19 (15.3) | 12 (14.1) | 7 (17.9) | |
| February | 10 (8.1) | 10 (11.8) | 0 (0.0) | |
| March | 8 (6.5) | 6 (7.1) | 2 (5.1) | |
| April | 4 (3.2) | 3 (3.5) | 1 (2.6) | |
| May | 3 (2.4) | 2 (2.4) | 1 (2.6) | |
| June | 4 (3.2) | 2 (2.4) | 2 (5.1) | |
| July | 7 (5.6) | 4 (4.7) | 3 (7.7) | |
| August | 10 (8.1) | 9 (10.6) | 1 (2.6) | |
| September | 12 (9.7) | 8 (9.4) | 4 (10.3) | |
| October | 14 (11.3) | 10 (11.8) | 4 (10.3) | |
| November | 15 (12.1) | 12 (14.1) | 3 (7.7) | |
| December | 18 (14.5) | 7 (8.2) | 11 (28.2) | |
| Weekday of presentation | 0.245 | |||
| Monday | 25 (20.2) | 15 (17.6) | 10 (25.6) | |
| Tuesday | 20 (16.1) | 13 (15.3) | 7 (17.9) | |
| Wednesday | 20 (16.1) | 11 (12.9) | 9 (23.1) | |
| Thursday | 14 (11.3) | 10 (11.8) | 4 (10.3) | |
| Friday | 20 (16.1) | 17 (20.0) | 3 (7.7) | |
| Saturday | 14 (11.3) | 9 (10.6) | 5 (12.8) | |
| Sunday | 11 (8.9) | 10 (11.8) | 1 (2.6) | |
| Time of presentation | 0.014 | |||
| 0.01–6.00 | 6 (4.8) | 6 (7.1) | 0 (0.0) | |
| 6.01–12.00 | 32 (25.8) | 21 (24.7) | 11 (28.2) | |
| 12.01–18.00 | 40 (32.3) | 21 (24.7) | 19 (48.7) | |
| 18.01–0.00 | 46 (37.1) | 37 (43.5) | 9 (23.1) | |
| Way of presentation | 0.029 * | |||
| Self-admission to the hospital | 17 (13.7) | 15 (17.6) | 2 (5.1) | |
| Ambulance | 77 (62.1) | 54 (63.5) | 23 (59.0) | |
| Air-Ambulance | 13 (10.5) | 6 (7.1) | 7 (17.9) | |
| External hospital transfer | 12 (9.7) | 5 (5.9) | 7 (17.9) | |
| Family doctor or urgent care centre | 3 (2.4) | 3 (3.5) | 0 (0.0) | |
| Repatriation | 2 (1.6) | 2 (2.4) | 0 (0.0) | |
| Triage | 0.169 | |||
| Acute life-threating | 34 (27.4) | 21 (24.7) | 13 (33.3) | |
| High urgency | 51 (41.1) | 33 (38.8) | 18 (46.2) | |
| Urgency | 35 (28.2) | 29 (34.1) | 6 (15.4) | |
| Less urgency | 4 (3.2) | 2 (2.4) | 2 (5.1) | |
| Shock room | 68(54.8) | 44(51.8) | 24(61.5) | 0.31 |
| Discharge | 0.001 * | |||
| Home | 65 (52.4) | 54 (63.5) | 11 (28.2) | |
| Hospital admission | 55 (44.4) | 30 (35.3) | 25 (64.1) | |
| Dead in ED | 2 (1.6) | 1 (1.2) | 1 (2.6) | |
| Transfer to other hospital | 2 (1.6) | 0 (0.0) | 2 (5.1) | |
| Hospitalisation department | 0.020 * | |||
| General internal medicine | 5 (4.1) | 1 (1.2) | 4 (10.3) | |
| Neurology/Neurosurgery | 13 (10.6) | 7 (8.3) | 6 (15.4) | |
| Intensive care | 13 (10.6) | 5 (6.0) | 8 (20.5) | |
| Orthopaedics | 20 (16.3) | 12 (14.3) | 8 (20.5) | |
| Hand surgery | 1 (0.8) | 1 (1.2) | 0 (0.0) | |
| Thorax surgery | 1 (0.8) | 1 (1.2) | 0 (0.0) | |
| Visceral surgery | 1 (0.8) | 1 (1.2) | 0 (0.0) | |
| Stroke | 1 (0.8) | 1 (1.2) | 0 (0.0) | |
| Rheumatology | 1 (0.8) | 1 (1.2) | 0 (0.0) |
| Variables | Total (n = 124) | Age < 65 (n = 85) | Age ≥ 65 (n = 39) | p Value |
|---|---|---|---|---|
| Mechanism of injury (accident versus) | ||||
| Vehicle type group | ||||
| One axis | 12 | 8 | 4 | 0.883 |
| Two axis | 122 | 77 | 45 | |
| Vehicle type | ||||
| Car | 109 (87.9) | 75 (88.2) | 34 (87.2) | 0.607 |
| Bicycle | 4 (3.2) | 3 (3.5) | 1 (2.6) | |
| E-bicycle | 3 (2.4) | 1 (1.2) | 2 (5.1) | |
| E-scooter | 1 (0.8) | 1 (1.2) | 0 (0.0) | |
| Tram | 1 (0.8) | 1 (1.2) | 0 (0.0) | |
| Motorcycle | 4 (3.2) | 3 (3.5) | 1 (2.6) | |
| Bus | 1 (0.8) | 1 (1.2) | 0 (0.0) | |
| Truck | 1 (0.8) | 0 (0.0) | 1 (2.6) | |
| Accident time | 0.187 | |||
| Day | 107 (86.3) | 71 (83.5) | 36 (92.3) | |
| Night | 17 (13.7) | 14 (16.5) | 3 (7.7) | |
| Vehicle speed | 30 (15; 40) | 30 (15; 40) | 37.5 (15; 40) | 0.697 |
| Patient hurled | 47 (56.6) | 26 (47.3) | 21 (75.0) | 0.016 * |
| Impact side | ||||
| Laterally | 112 (91.1) | 79 (92.9) | 33 (86.8) | 0.100 |
| Frontally | 9 (7.3) | 6 (7.1) | 3 (7.9) | |
| Behind | 2 (1.6) | 0 (0.0) | 2 (5.3) |
| Variables | Total (n = 124) | Age < 65 (n = 85) | Age ≥ 65 (n = 39) | p Value |
|---|---|---|---|---|
| ISS | 5 [1; 14] | 4 [1; 12] | 14 [2; 26] | 0.004 * |
| AIS > 2 | ||||
| AIS head & neck & cervical spine | 23 (18.5) | 13 (15.3) | 10 (25.6) | 0.169 |
| AIS face | 3 (2.4) | 1 (1.2) | 2 (5.1) | 0.184 |
| AIS chest & thoracic spine | 17 (13.7) | 7 (8.2) | 10 (25.6) | 0.009 * |
| AIS abdomen & pelvic contents & lumbar spine | 3 (2.4) | 0 (0.0) | 3 (7.7) | 0.010 * |
| AIS extremities & bony pelvis > 2 AIS external | 20 (16.1) | 8 (9.4) | 12 (30.8) | 0.003 * |
| AIS externa l > 2 | 0 (0.0) | 0 (0.0) | 0 (0.0) | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pavol, P.; Topalis, V.; Zagalioti, S.-C.; Kuzyo, O.; Müller, M.; Exadaktylos, A.K.; Ziaka, M.; Klukowska-Rötzler, J. When Pedestrian Crossings Become Danger Zones: Trauma and Mortality Risks in Elderly Pedestrians. Int. J. Environ. Res. Public Health 2025, 22, 1556. https://doi.org/10.3390/ijerph22101556
Pavol P, Topalis V, Zagalioti S-C, Kuzyo O, Müller M, Exadaktylos AK, Ziaka M, Klukowska-Rötzler J. When Pedestrian Crossings Become Danger Zones: Trauma and Mortality Risks in Elderly Pedestrians. International Journal of Environmental Research and Public Health. 2025; 22(10):1556. https://doi.org/10.3390/ijerph22101556
Chicago/Turabian StylePavol, Peter, Vasileios Topalis, Sofia-Chrysovalantou Zagalioti, Olha Kuzyo, Martin Müller, Aristomenis K. Exadaktylos, Mairi Ziaka, and Jolanta Klukowska-Rötzler. 2025. "When Pedestrian Crossings Become Danger Zones: Trauma and Mortality Risks in Elderly Pedestrians" International Journal of Environmental Research and Public Health 22, no. 10: 1556. https://doi.org/10.3390/ijerph22101556
APA StylePavol, P., Topalis, V., Zagalioti, S.-C., Kuzyo, O., Müller, M., Exadaktylos, A. K., Ziaka, M., & Klukowska-Rötzler, J. (2025). When Pedestrian Crossings Become Danger Zones: Trauma and Mortality Risks in Elderly Pedestrians. International Journal of Environmental Research and Public Health, 22(10), 1556. https://doi.org/10.3390/ijerph22101556





