The Influence of Rehabilitation Programs on the Mental State and Quality of Life in Patients with Fibromyalgia: A Comparative Cohort Study from Romania
Abstract
1. Introduction
2. Materials and Methods
2.1. Assessments
2.2. Statistical Analysis
2.3. Sample Size and Randomization
3. Results
3.1. General Characteristics
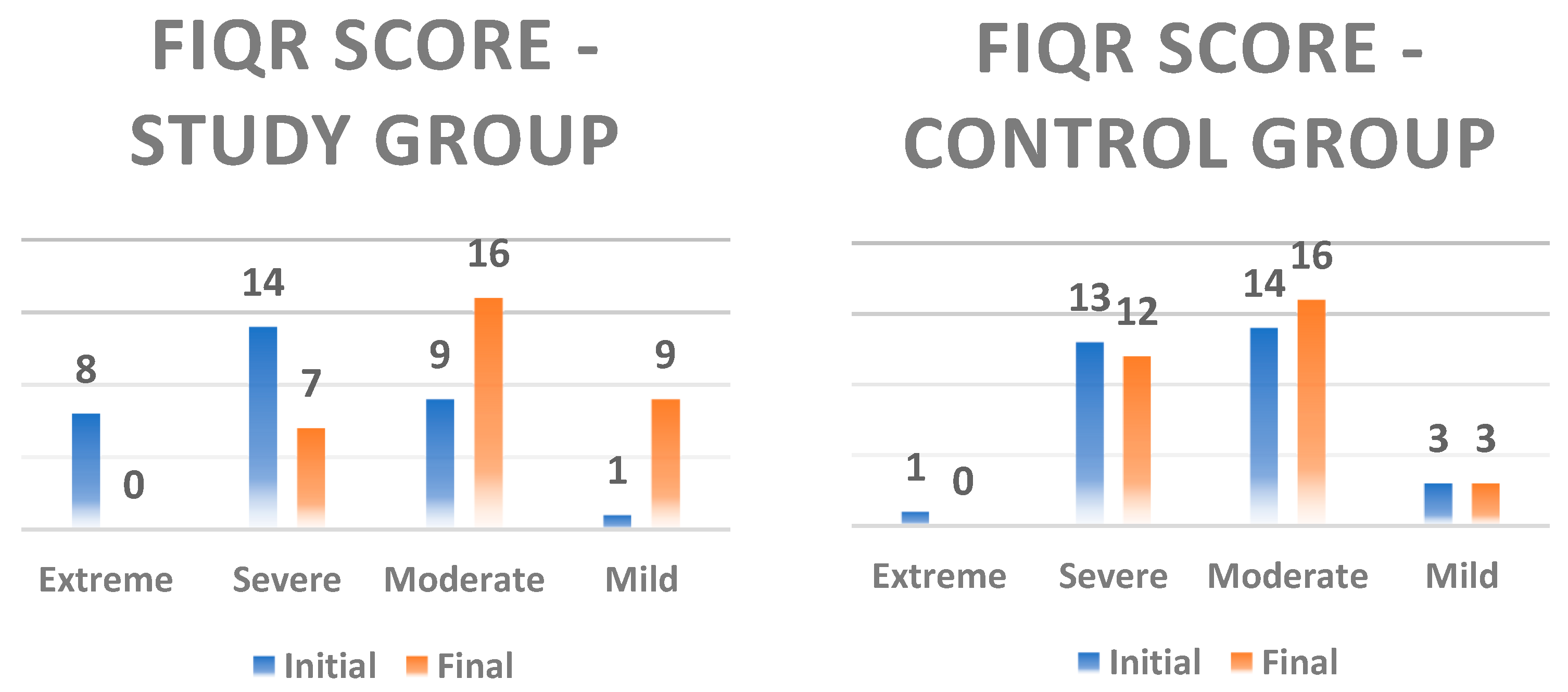
3.2. Results of the FIQR Score
Comparison of Average FIQR Scores by Dimensions at the Initial and Final Moment
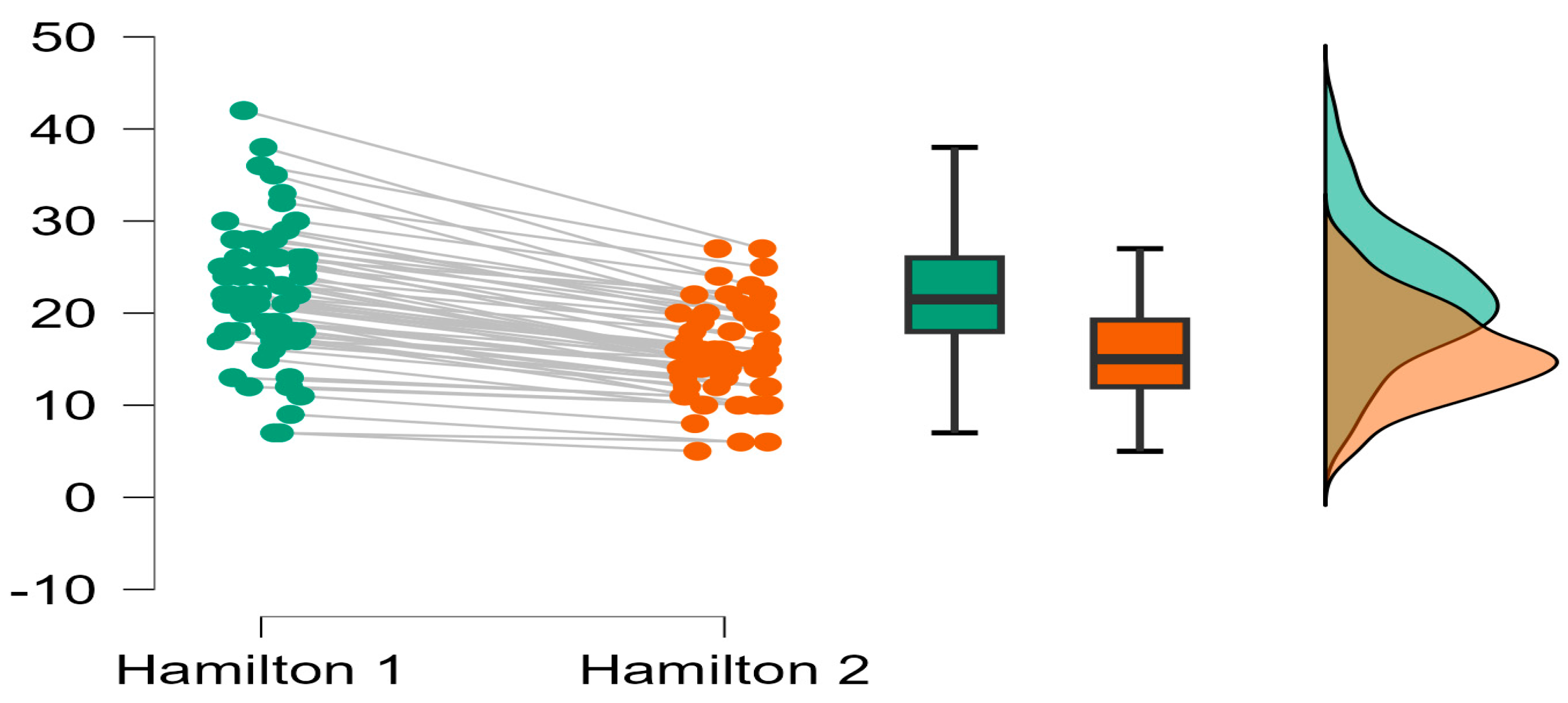
3.3. Assessment of Anxiety
3.4. Correlation of Function with Anxiety
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FM | Fibromyalgia |
| FIQR | The Revised Fibromyalgia Impact Questionnaire of FM |
| Ham—A | Hamilton Anxiety Scale |
| SG | Study Group |
| CG | Control Group |
References
- Segura-Jiménez, V.; Álvarez-Gallardo, I.C.; Carbonell-Baeza, A.; Aparicio, V.A.; Ortega, F.B.; Casimiro, A.J.; Delgado-Fernández, M. Fibromyalgia has a larger impact on physical health than on psychological health, yet both are markedly affected: The al-Ándalus project. Semin. Arthritis Rheum. 2015, 44, 563–570. [Google Scholar] [CrossRef]
- Sarzi-Puttini, P.; Giorgi, V.; Marotto, D.; Atzeni, F. Fibromyalgia: An update on clinical characteristics, aetiopathogenesis and treatment. Nat. Rev. Rheumatol. 2020, 16, 645–660. [Google Scholar] [CrossRef]
- Cabo-Meseguer, A.; Cerdá-Olmedo, G.; Trillo-Mata, J.L. Fibromyalgia: Prevalence, epidemiologic profiles and economic costs. Med. Clin. 2017, 149, 441–448. [Google Scholar] [CrossRef]
- Heidari, F.; Afshari, M.; Moosazadeh, M. Prevalence of fibromyalgia in general population and patients, a systematic review and meta-analysis. Rheumatol. Int. 2017, 37, 1527–1539. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.; Croucamp, M. Physical activity and quality of life of patients with fibromyalgia. S. Afr. J. Sports Med. 2023, 35, v35i1a14781. [Google Scholar] [CrossRef] [PubMed]
- Marques, A.P.; Santo, A.D.; Berssaneti, A.A.; Matsutani, L.A.; Yuan, S.L.K. Prevalence of fibromyalgia: Literature review update. Rev. Bras. Reumatol. 2017, 57, 356–363. [Google Scholar] [CrossRef]
- Goldberg, D.S.; McGee, S.J. Pain as a global public health priority. BMC Public Health 2011, 11, 770. [Google Scholar] [CrossRef]
- Gyorfi, M.; Rupp, A.; Abd-Elsayed, A. Fibromyalgia Pathophysiology. Biomedicines 2022, 10, 3070. [Google Scholar] [CrossRef]
- Moreno-Ligero, M.; Moral-Munoz, J.A.; Salazar, A.; Failde, I. Health Intervention for Improving Pain, Quality of Life, and Functional Disability in Patients with Chronic Pain: Systematic Review. JMIR Mhealth Uhealth 2023, 11, e40844. [Google Scholar] [CrossRef]
- Bhargava, J.; Hurley, J.A. Fibromyalgia; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Meyer, H.P. Myofascial pain syndrome and its suggested role in the pathogenesis and treatment of fibromyalgia syndrome. Curr. Pain Headache Rep. 2002, 6, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Rodríguez, A.; Rubio-Arias, J.Á.; Ramos-Campo, D.J.; Reche-García, C.; Leyva-Vela, B.; Nadal-Nicolás, Y. Psychological and Sleep Effects of Tryptophan and Magnesium-Enriched Mediterranean Diet in Women with Fibromyalgia. Int. J. Environ. Res. Public Health 2020, 17, 2227. [Google Scholar] [CrossRef]
- Lee, J.W.; Lee, K.E.; Park, D.J.; Kim, S.H.; Nah, S.S.; Lee, J.H.; Kim, S.K.; Lee, Y.A.; Hong, S.J.; Kim, H.S.; et al. Determinants of quality of life in patients with fibromyalgia: A structural equation modeling approach. PLoS ONE 2017, 12, e0171186. [Google Scholar] [CrossRef]
- Hoffman, D.L.; Dukes, E.M. The health status burden of people with fibromyalgia: A review of studies that assessed health status with the SF-36 or the SF-12. Int. J. Clin. Pract. 2008, 62, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Siracusa, R.; Paola, R.D.; Cuzzocrea, S.; Impellizzeri, D. Fibromyalgia: Pathogenesis, Mechanisms, Diagnosis and Treatment Options Update. Int. J. Mol. Sci. 2021, 22, 3891. [Google Scholar] [CrossRef]
- Bair, M.J.; Krebs, E.E. Fibromyalgia. Ann. Intern. Med. 2020, 172, Itc33–Itc48. [Google Scholar] [CrossRef]
- Schmidt-Wilcke, T.; Diers, M. New Insights into the Pathophysiology and Treatment of Fibromyalgia. Biomedicines 2017, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Macfarlane, G.J.; Kronisch, C.; Dean, L.E.; Atzeni, F.; Häuser, W.; Fluß, E.; Choy, E.; Amris, K.; Branco, J.; Dincer, F.; et al. EULAR revised recommendations for the management of fibromyalgia. Ann. Rheum. Dis. 2017, 76, 318–328. [Google Scholar] [CrossRef]
- Busch, A.J.; Webber, S.C.; Brachaniec, M.; Bidonde, J.; Bello-Haas, V.D.; Danyliw, A.D.; Overend, T.J.; Richards, R.S.; Sawant, A.; Schachter, C.L. Exercise therapy for fibromyalgia. Curr. Pain Headache Rep. 2011, 15, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Paolucci, T.; de Sire, A.; Ferrillo, M.; di Fabio, D.; Molluso, A.; Patruno, A.; Pesce, M.; Lai, C.; Ciacchella, C.; Saggino, A.; et al. Telerehabilitation proposal of mind-body technique for physical and psychological outcomes in patients with fibromyalgia. Front. Physiol. 2022, 13, 917956. [Google Scholar] [CrossRef]
- Yoo, S.A.; Kim, C.Y.; Kim, H.D.; Kim, S.W. Effects of progressive muscle relaxation therapy with home exercise on pain, fatigue, and stress in subjects with fibromyalgia syndrome: A pilot randomized controlled trial. J. Back Musculoskelet. Rehabil. 2022, 35, 289–299. [Google Scholar] [CrossRef]
- Meulenberg, C.J.W.; de Bruin, E.D.; Marusic, U. A perspective on implementation of technology-driven exergames for adults as telerehabilitation services. Front. Psychol. 2022, 13, 840863. [Google Scholar] [CrossRef]
- Theadom, A.; Cropley, M.; Smith, H.E.; Feigin, V.L.; McPherson, K. Mind and body therapy for fibromyalgia. Cochrane Database Syst. Rev. 2015, 2015, CD001980. [Google Scholar] [CrossRef] [PubMed]
- Haugmark, T.; Hagen, K.B.; Smedslund, G.; Zangi, H.A. Mindfulness—And acceptance-based interventions for patients with fibromyalgia—A systematic review and meta-analyses. PLoS ONE 2019, 14, e0221897. [Google Scholar] [CrossRef]
- Cankurtaran, D.; Tezel, N.; Ercan, B.; Yildiz, S.Y.; Akyuz, E.U. The effects of COVID-19 fear and anxiety on symptom severity, sleep quality, and mood in patients with fibromyalgia: A pilot study. Adv. Rheumatol. 2021, 61, 41. [Google Scholar] [CrossRef] [PubMed]
- Agostini, F.; Mangone, M.; Ruiu, P.; Paolucci, T.; Santilli, V.; Bernetti, A. Rehabilitation setting during and after COVID-19: An overview on recommendations. J. Rehabil. Med. 2021, 53, jrm00141. [Google Scholar] [CrossRef]
- Zamunér, A.R.; Andrade, C.P.; Arca, E.A.; Avila, M.A. Impact of water therapy on pain management in patients with fibromyalgia: Current perspectives. J. Pain Res. 2019, 12, 1971–2007. [Google Scholar] [CrossRef]
- Masiero, S.; Litwocenko, S.; Agostini, F. On behalf section of Rehabilitation in Environmental Thermal for Italian Society of Physical Medicine and Rehabilitation. Rehabilitation in an Italian thermal setting: A new therapeutic strategy for patients with musculoskeletal disability-the results of an Italian survey. Int. J. Biometeorol. 2020, 64, 951–954. [Google Scholar]
- Vaidya, B.; Nakarmi, S.A. Qualitative Study of Patients’ Beliefs and Perception on Medicinal Properties of Natural Hot Spring Bath for Musculoskeletal Problems. J. Environ. Public Health 2020, 2020, 3694627. [Google Scholar] [CrossRef] [PubMed]
- Fioravanti, A.; Cantarini, L.; Guidelli, G.M.; Galeazzi, M. Mechanisms of action of spa therapies in rheumatic diseases: What scientific evidence is there? Rheumatol. Int. 2011, 31, 1–8. [Google Scholar] [CrossRef]
- Naumann, J.; Sadaghiani, C. Therapeutic benefit of balneotherapy and hydrotherapy in the management of fibromyalgia syndrome: A qualitative systematic review and meta-analysis of randomized controlled trials. Arthritis Res. Ther. 2014, 16, R141. [Google Scholar] [CrossRef]
- de Sousa, A.P.; Almeida, L.A.; Lourenço, B.P.; Alvares, L.D.; Avila, M.A. Pain neuroscience education improves quality of life when added to aquatic exercise therapy for women with fibromyalgia: Randomized controlled clinical trial. Disabil. Rehabil. 2023, 46, 1559–1569. [Google Scholar] [CrossRef]
- Hoskin, T.L.; Whipple, M.O.; Nanda, S.; Vincent, A. Longitudinal stability of fibromyalgia symptom clusters. Arthritis Res. Ther. 2018, 20, 37. [Google Scholar] [CrossRef]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.-A.; Goldenberg, D.L.; Häuser, W.; Katz, R.L.; Mease, P.J.; Russell, A.S.; Russell, I.J.; Walitt, B. Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin. Arthritis Rheum. 2016, 46, 319–329. [Google Scholar] [CrossRef]
- Tomioka, M. Relaxation Techniques. Jpn. J. Psychosom. Med. 2017, 57, 1025–1031. [Google Scholar]
- Bennett, R.M.; Friend, R.; Jones, K.D.; Ward, R.; Han, B.K.; Ross, R.L. The Revised Fibromyalgia Impact Questionnaire (FIQR): Validation and psychometric properties. Arthritis Res. Ther. 2009, 11, R120. [Google Scholar] [CrossRef]
- Thompson, E. Hamilton Rating Scale for Anxiety (HAM-A). Occup. Med. 2015, 65, 601. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows, Version 29.0; IBM Corp.: Armonk, NY, USA, 2022. [Google Scholar]
- Maier, W.; Buller, R.; Philipp, M.; Heuser, I. The Hamilton Anxiety Scale: Reliability, validity and sensitivity to change in anxiety and depressive disorders. J. Affect. Disord. 1998, 14, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959, 32, 50–55. [Google Scholar] [CrossRef]
- Salaffi, F.; Sarzi-Puttini, P.; Girolimetti, R.; Atzeni, F.; Gasparini, S.; Grassi, W. Health-related quality of life in fibromyalgia patients: A comparison with rheumatoid arthritis patients and the general population using the SF-36 health survey. Clin. Exp. Rheumatol. 2009, 27 (Suppl. S56), S67–S74. [Google Scholar] [PubMed]
- Bungau, S.G.; Popa, V.C. Between religion and science: Some aspects: Concerning illness and healing in antiquity. Transylv. Rev. 2015, 26, 3–19. [Google Scholar]
- Maindet, C.; Maire, A.; Vermorel, C.; Cracowski, C.; Rolland, C.; Forestier, R.; Comte, A.; Roques, C.-F.; Serra, E.; Bosson, J.-L. Spa Therapy for the Treatment of Fibromyalgia: An Open, Randomized Multicenter Trial. J. Pain 2021, 22, 940–951. [Google Scholar] [CrossRef] [PubMed]
- Naumann, J.; Kruza, I.; Denkel, L.; Kienle, G.; Huber, R. Effects and feasibility of hyperthermic baths in comparison to exercise as add-on treatment to usual care in depression: A randomised, controlled pilot study. BMC Psychiatry 2020, 20, 536. [Google Scholar] [CrossRef]
- Rodríguez-Huguet, M.; Ayala-Martínez, C.; Góngora-Rodríguez, P.; Rosety-Rodríguez, M.Á.; Martín-Valero, R.; Góngora-Rodríguez, J. Aquatic Exercise in Physical Therapy Treatment for Fibromyalgia: Systematic Review. Healthcare 2024, 12, 701. [Google Scholar] [CrossRef]
- Zhang, K.D.; Wang, L.Y.; Zhang, Z.H.; Zhang, D.X.; Lin, X.W.; Meng, T.; Qi, F. Effect of Exercise Interventions on Health-Related Quality of Life in Patients with Fibromyalgia Syndrome: A Systematic Review and Network Meta-Analysis. J. Pain Res. 2022, 15, 3639–3656. [Google Scholar] [CrossRef]
- Relaxation Techniques: What You Need to Know. National Center for Complementary and Integrative Health. 2021. Available online: https://www.nccih.nih.gov/health/relaxation-techniques-what-you-need-to-know (accessed on 17 January 2024).
- Steen, J.P.; Kannan, V.; Zaidi, A.; Cramer, H.; Ng, J.Y. Mind-body therapy for treating fibromyalgia: A systematic review. Pain Med. 2024, 25, 703–737. [Google Scholar] [CrossRef]
- Cohen-Biton, L.; Buskila, D.; Nissanholtz-Gannot, R. Review of Fibromyalgia (FM) Syndrome Treatments. Int. J. Environ. Res. Public Health 2022, 19, 12106. [Google Scholar] [CrossRef]
- Fontaine, K.R.; Conn, L.; Clauw, D.J. Effects of Lifestyle Physical Activity in Adults with Fibromyalgia: Results at Follow-Up. J. Clin. Rheumatol. 2011, 17, 68. [Google Scholar] [CrossRef] [PubMed]
- Hou, Q.; Zhang, J.; Su, Z.; Wang, X.; Fang, H.; Qian, S.; Shi, H.; Wang, Q.; Li, Y.; Lin, J.; et al. Clinical Trial of Ozonated Water Enema for the Treatment of Fibromyalgia: A Randomized, Double-Blind Trial. Pain Physician 2025, 28, E13–E22. [Google Scholar] [PubMed]

| Characteristics | Study Group | Control Group | p-Value |
|---|---|---|---|
| Female, N (%) | 30 (93.75) | 28 (90.32) | 0.810 |
| Male, N (%) | 2 (6.25) | 3 (9.67) | 0.672 |
| Use of medication NSAID | 32 (100) | 31 (100) | - |
| Age | Group | N | Min. | Max. | Mean | SD | Std. Error Mean | t | p |
| SG | 32 | 19 | 68 | 46.95 | 13.16 | 2.403 | 0.705 | 0.485 | |
| CG | 31 | 25 | 69 | 44.74 | 11.31 | 2.066 |
| BMI (kg/m2) | Group | N | Min. | Max. | Mean | SD | t | p |
| SG | 32 | 17.69 | 36.33 | 24.50 | 4.41 | 0.801 | 0.421 | |
| CG | 31 | 17.30 | 29.59 | 23.63 | 3.06 |
| Parameter | Group | Mean | SD | t | Mean-D | p-Value |
|---|---|---|---|---|---|---|
| FIQR it | CG | 56.569 | 11.466 | 3.22 | 9.510 | 0.002 |
| SG | 66.507 | 11.258 | ||||
| FIQR ft | CG | 54.819 | 10.786 | −1.78 | −4.989 | 0.08 |
| SG | 49.830 | 10.894 |
| Parameter | Group | Mean | SD | Coefficient of Variation | t | Mean-D | p-Value |
|---|---|---|---|---|---|---|---|
| FIQR i function | CG | 16.230 | 3.776 | 0.233 | 2.32 | 2.544 | 0.024 |
| SG | 18.774 | 4.663 | 0.248 | ||||
| FIQR f function | CG | 16.230 | 3.776 | 0.233 | −3.00 | −3.133 | 0.004 |
| SG | 13.097 | 4.282 | 0.327 | ||||
| FIQR i overall impact | CG | 13.167 | 3.239 | 0.246 | 2.65 | 2.167 | 0.010 |
| SG | 15.333 | 3.089 | 0.201 | ||||
| FIQR f overall impact | CG | 12.733 | 3.005 | 0.236 | −0.46 | −0.367 | 0.647 |
| SG | 12.367 | 3.157 | 0.255 | ||||
| FIQR i symptom | CG | 27.200 | 5.255 | 0.193 | 3.33 | 5.160 | 0.001 |
| SG | 32.360 | 6.648 | 0.205 | ||||
| FIQR f symptom | CG | 25.900 | 4.779 | 0.184 | −0.82 | −1.100 | 0.412 |
| SG | 24.800 | 5.497 | 0.222 |
| Parameter | Group | Mean | SD | t | Mean—D | p-Value |
|---|---|---|---|---|---|---|
| Hamilton initial | CG | 19.467 | 6.010 | 2.90 | 5.100 | 0.005 |
| SG | 24.567 | 7.514 | ||||
| Hamilton final | CG | 15.067 | 4.877 | 1.01 | 1.300 | 0.315 |
| SG | 16.367 | 5.055 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borze, T.F.; Pallag, A.; Ciobanu, D.I.; Kalman, K.; Ciurba, A.P.; Suciu, R.N.; Mureșan, M.; Nistor-Cseppento, C.D. The Influence of Rehabilitation Programs on the Mental State and Quality of Life in Patients with Fibromyalgia: A Comparative Cohort Study from Romania. Int. J. Environ. Res. Public Health 2025, 22, 1553. https://doi.org/10.3390/ijerph22101553
Borze TF, Pallag A, Ciobanu DI, Kalman K, Ciurba AP, Suciu RN, Mureșan M, Nistor-Cseppento CD. The Influence of Rehabilitation Programs on the Mental State and Quality of Life in Patients with Fibromyalgia: A Comparative Cohort Study from Romania. International Journal of Environmental Research and Public Health. 2025; 22(10):1553. https://doi.org/10.3390/ijerph22101553
Chicago/Turabian StyleBorze (Ursu), Theodora Florica, Annamaria Pallag, Doriana Ioana Ciobanu, Klara Kalman, Anca Paula Ciurba, Ramona Nicoleta Suciu, Mariana Mureșan, and Carmen Delia Nistor-Cseppento. 2025. "The Influence of Rehabilitation Programs on the Mental State and Quality of Life in Patients with Fibromyalgia: A Comparative Cohort Study from Romania" International Journal of Environmental Research and Public Health 22, no. 10: 1553. https://doi.org/10.3390/ijerph22101553
APA StyleBorze, T. F., Pallag, A., Ciobanu, D. I., Kalman, K., Ciurba, A. P., Suciu, R. N., Mureșan, M., & Nistor-Cseppento, C. D. (2025). The Influence of Rehabilitation Programs on the Mental State and Quality of Life in Patients with Fibromyalgia: A Comparative Cohort Study from Romania. International Journal of Environmental Research and Public Health, 22(10), 1553. https://doi.org/10.3390/ijerph22101553








