A Geographic Weighted Regression Analysis of the Health Opportunity Index and Stroke Prevalence in Health and Human Services Region 3
Abstract
1. Background
1.1. Neighborhood Effect of Social Determinants of Health
1.2. Health Opportunity Index (HOI): A Tool for Measuring SDOH
1.3. Research Problem
1.4. Study Justification/Purpose
2. Methodology
2.1. Data Sources
- (a)
- U.S Census Bureau, American Community Survey (ACS) datasets: Education index, income inequality, Job participation, Townsend deprivation index, Spatial segregation index, Population churning, Population weighted density
- (b)
- USDA Food Access Research Atlas: Food Access Index
- (c)
- Center for Neighborhood Technology (CNT) Datasets: Affordability Index, Employment Access Index
- (d)
- U.S. Environmental Protection Agency (EPA), Environmental Justice Screening (EJScreen) datasets: Environmental Quality Index, Walkability Index
- (e)
- Health Resources and Services Administration (HRSA): Healthcare Access Index
2.2. HOI Computation
2.3. Data Analysis Plan
3. Results
3.1. Demographic Characteristics of HHS Region 3
3.2. Interpretation of GWR Coefficient Maps
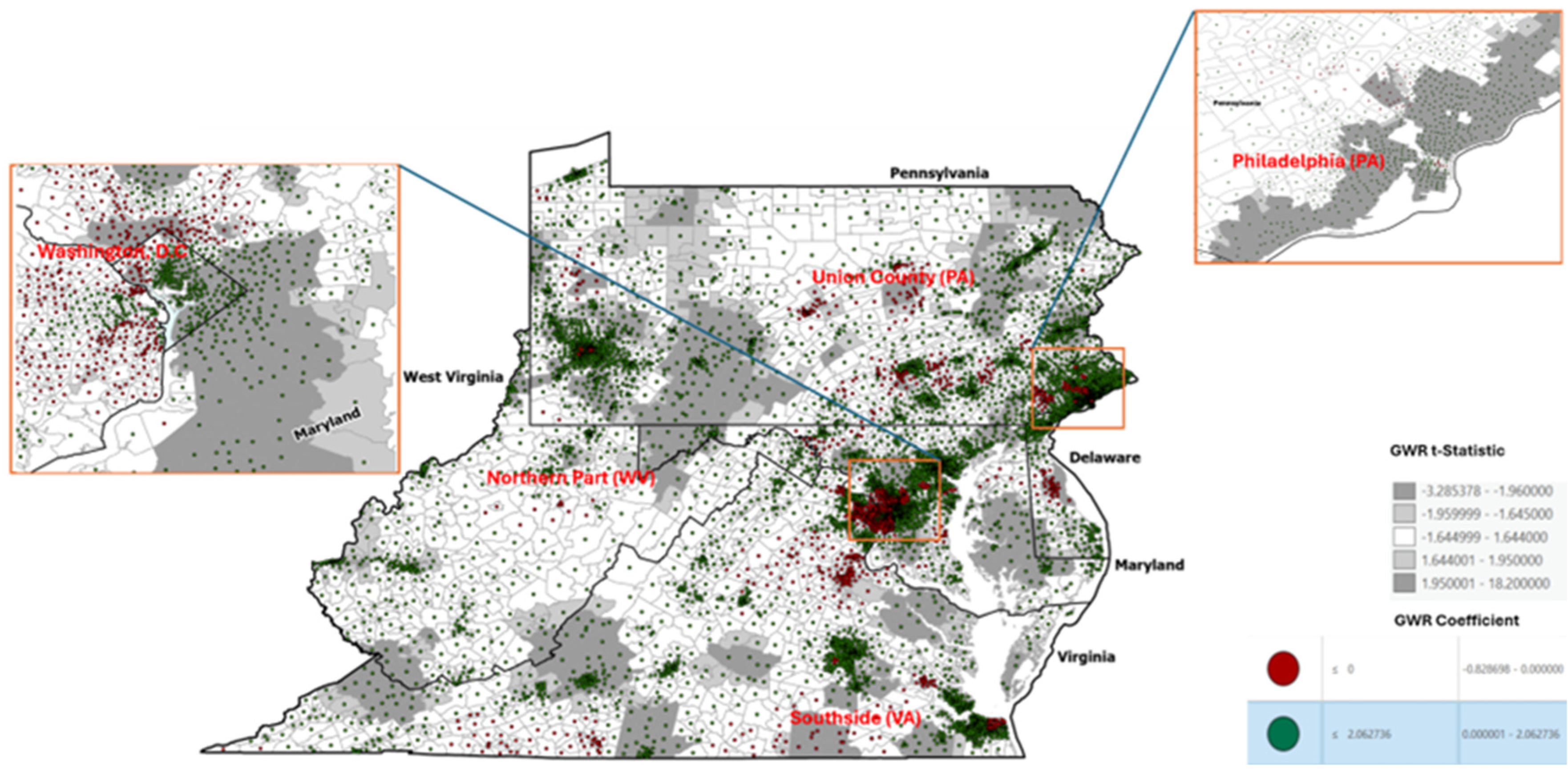
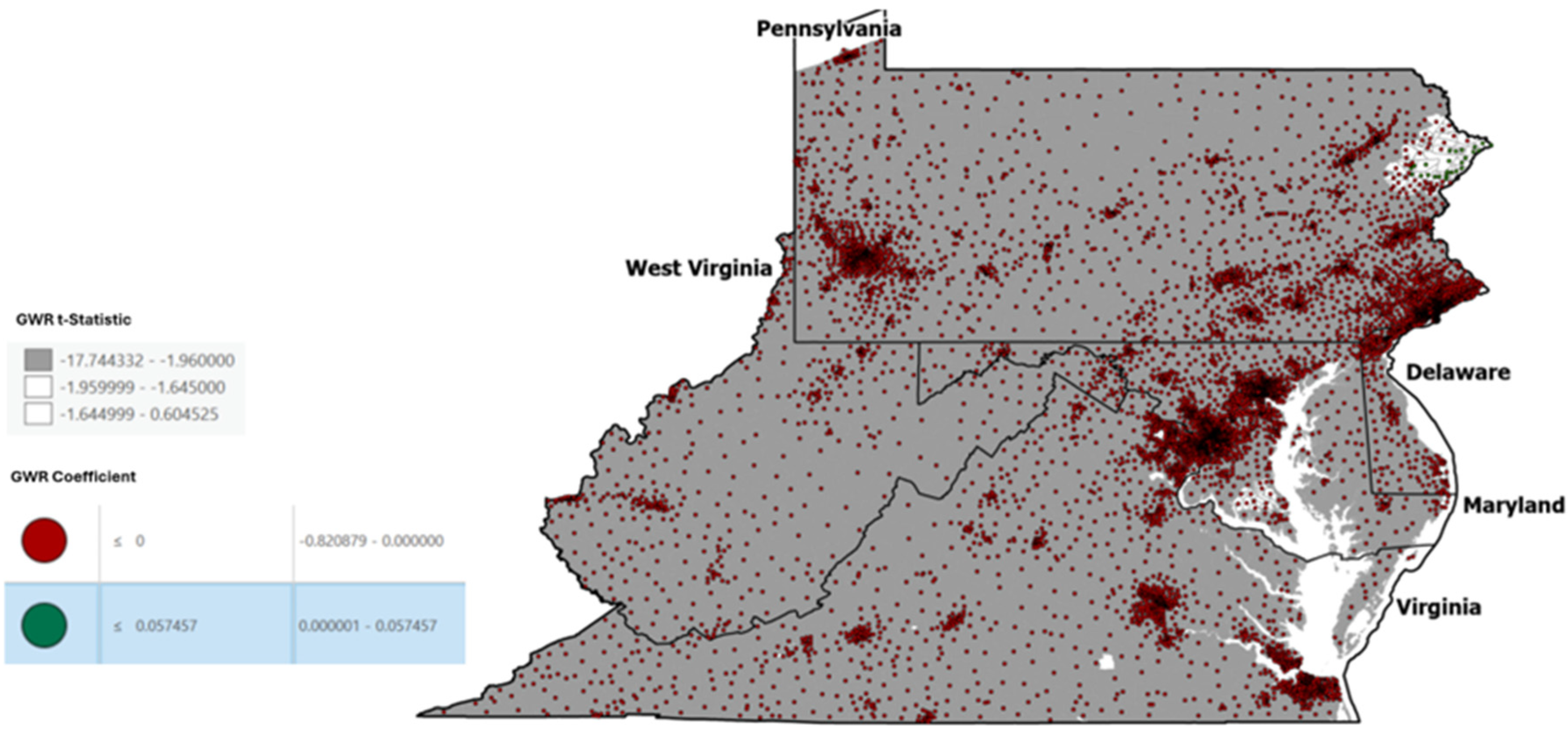
3.2.1. Neighborhood and Built Environment (Profile1)
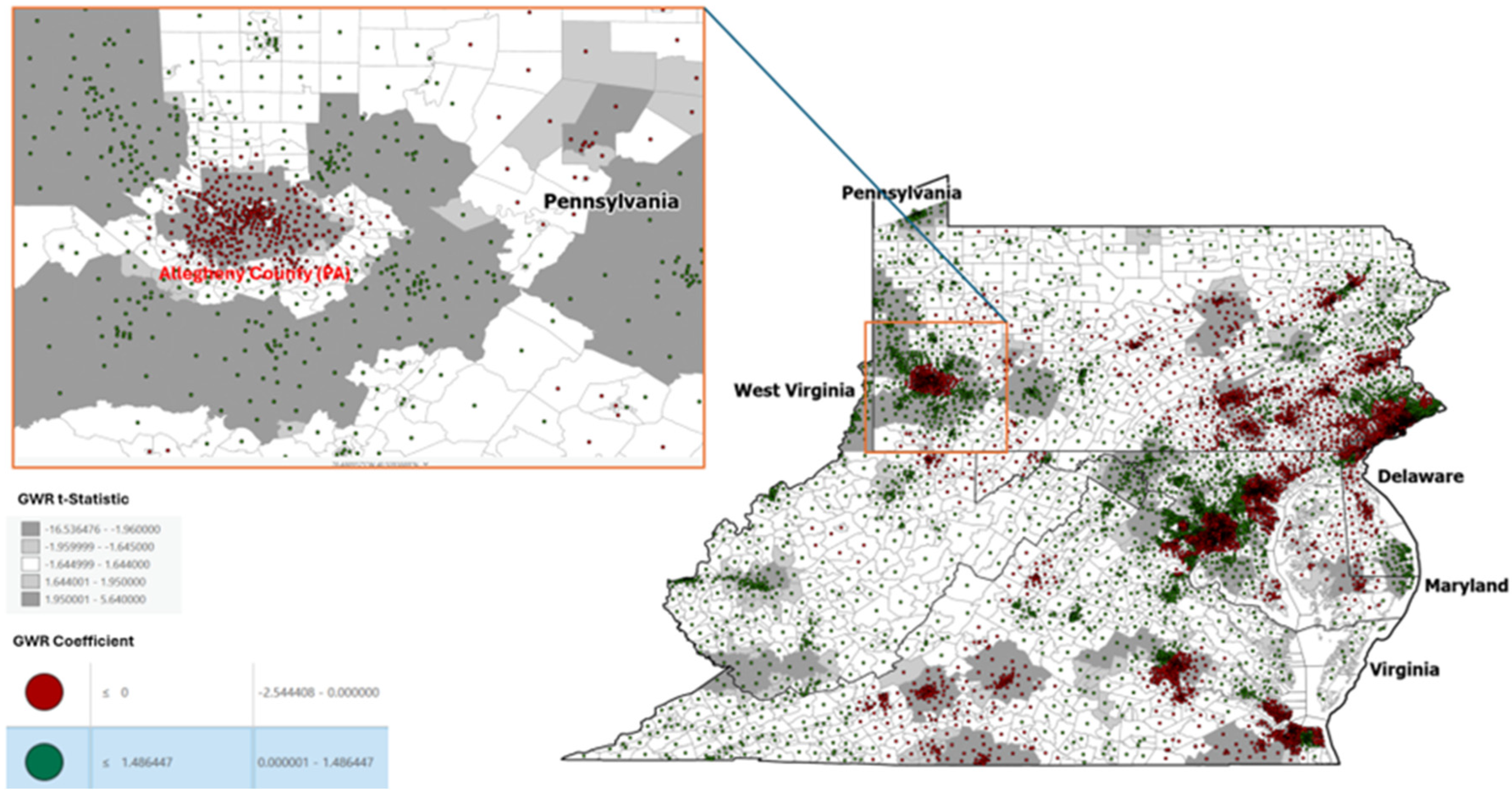
3.2.2. Employment Access Indicator
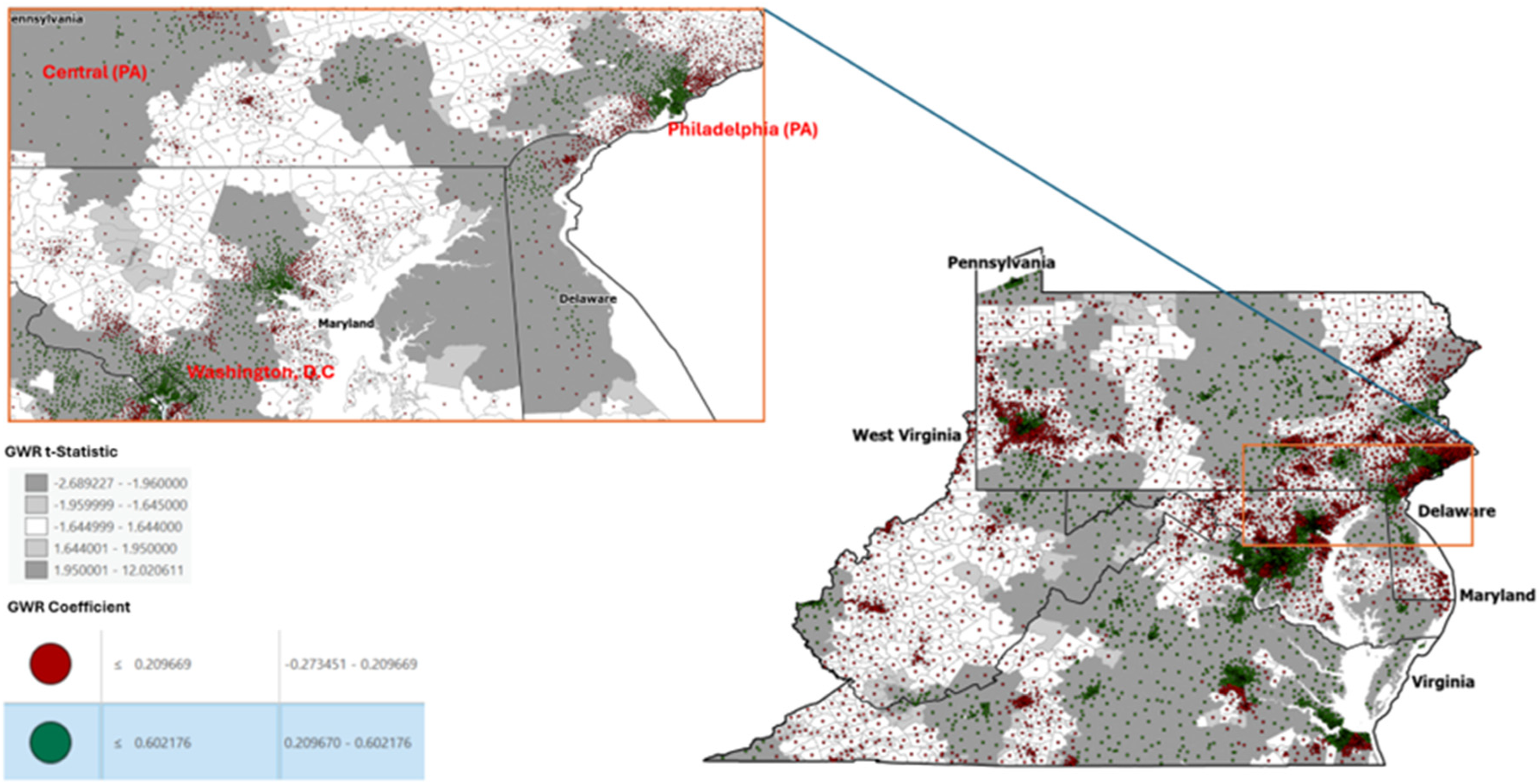
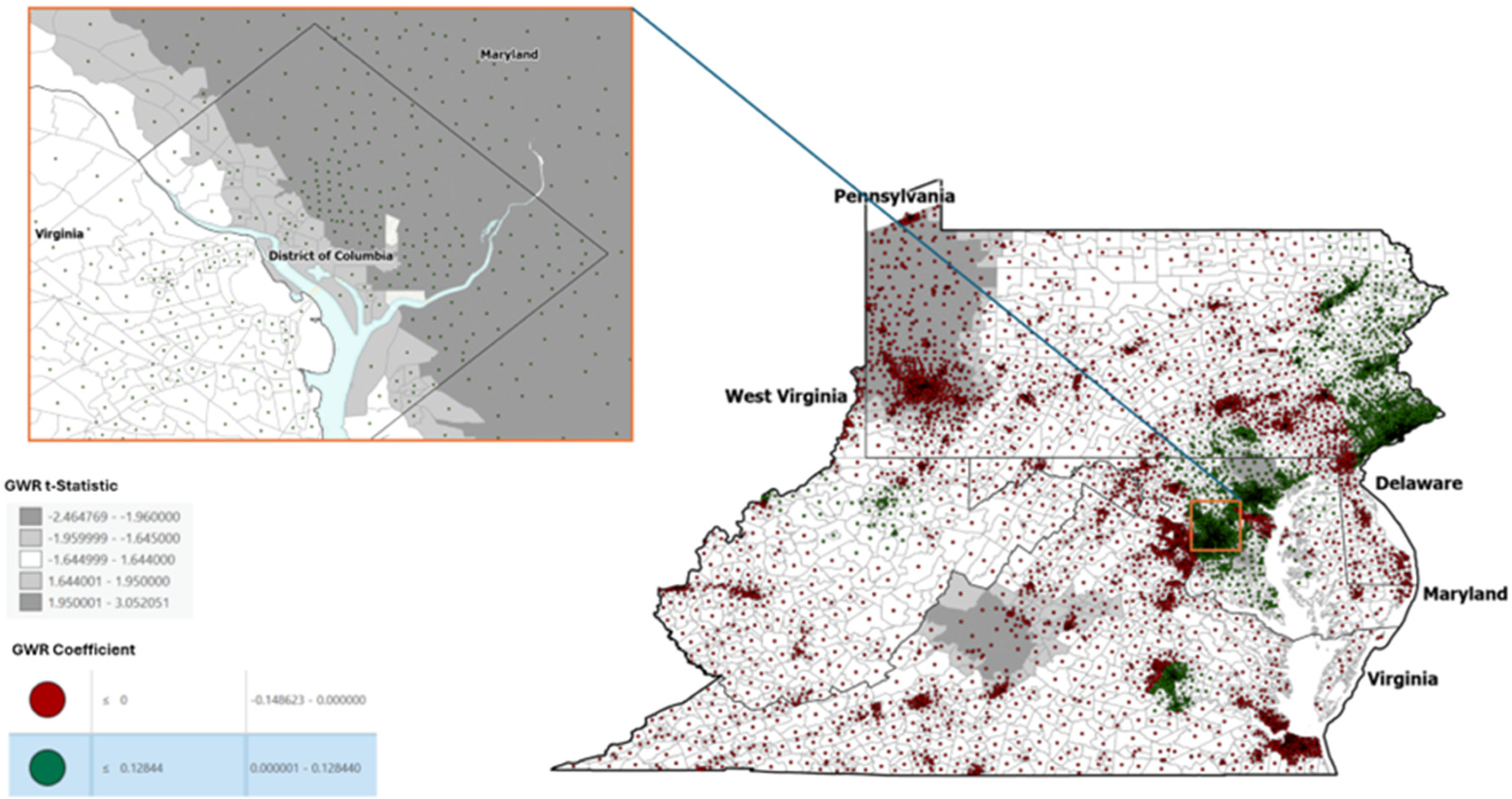
3.2.3. Affordability Indicator
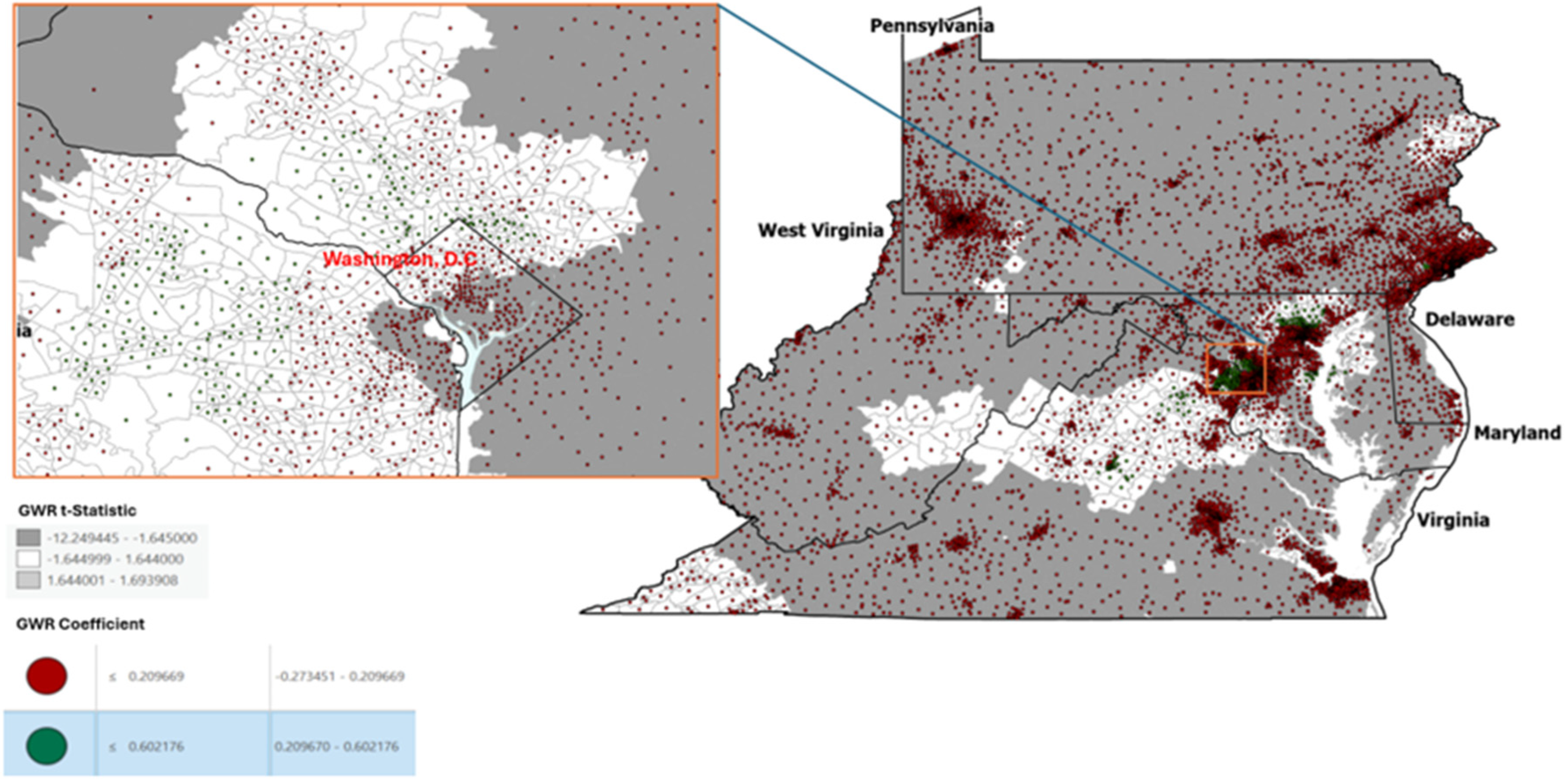
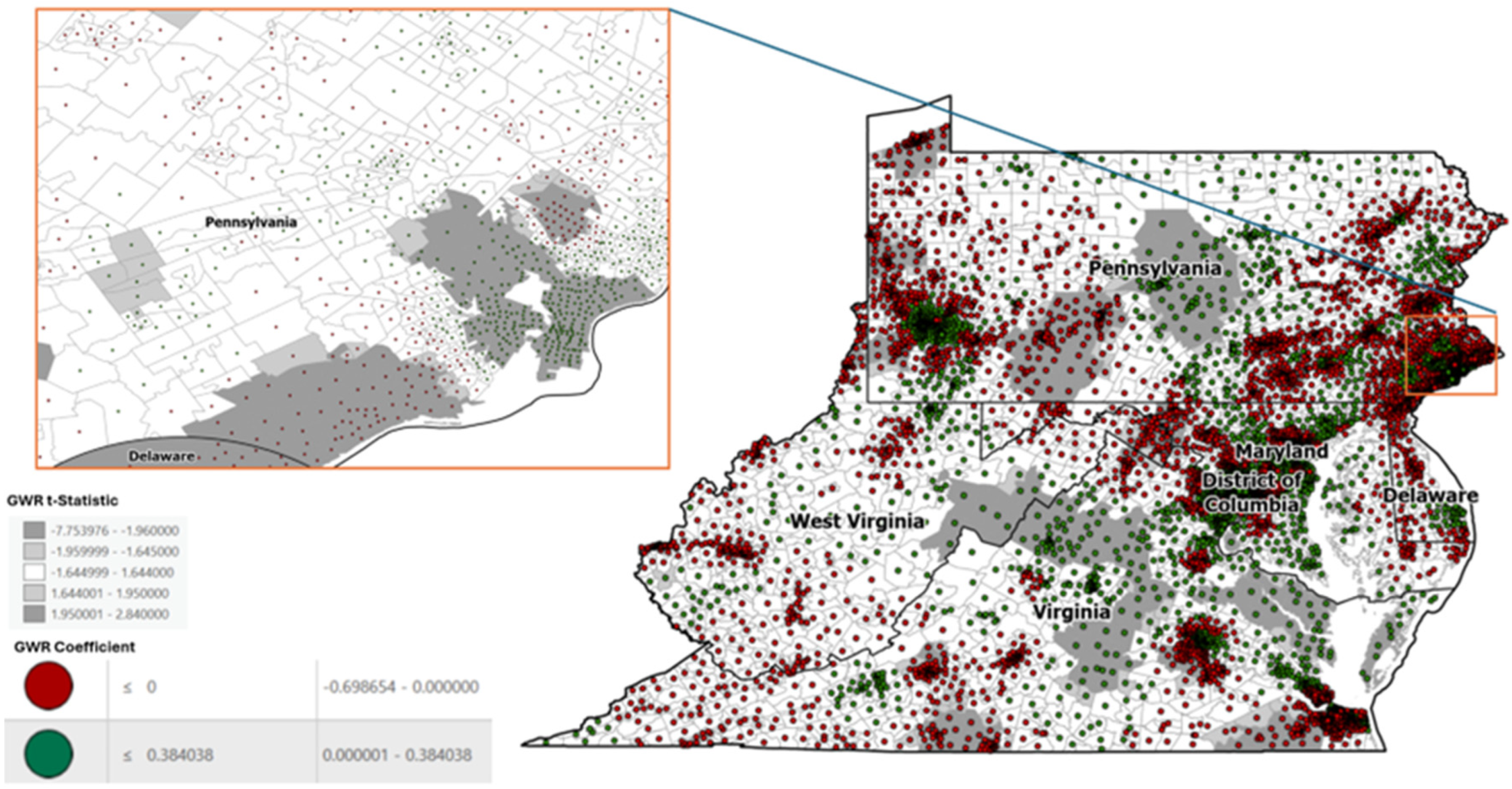
3.2.4. Walkability Indicator
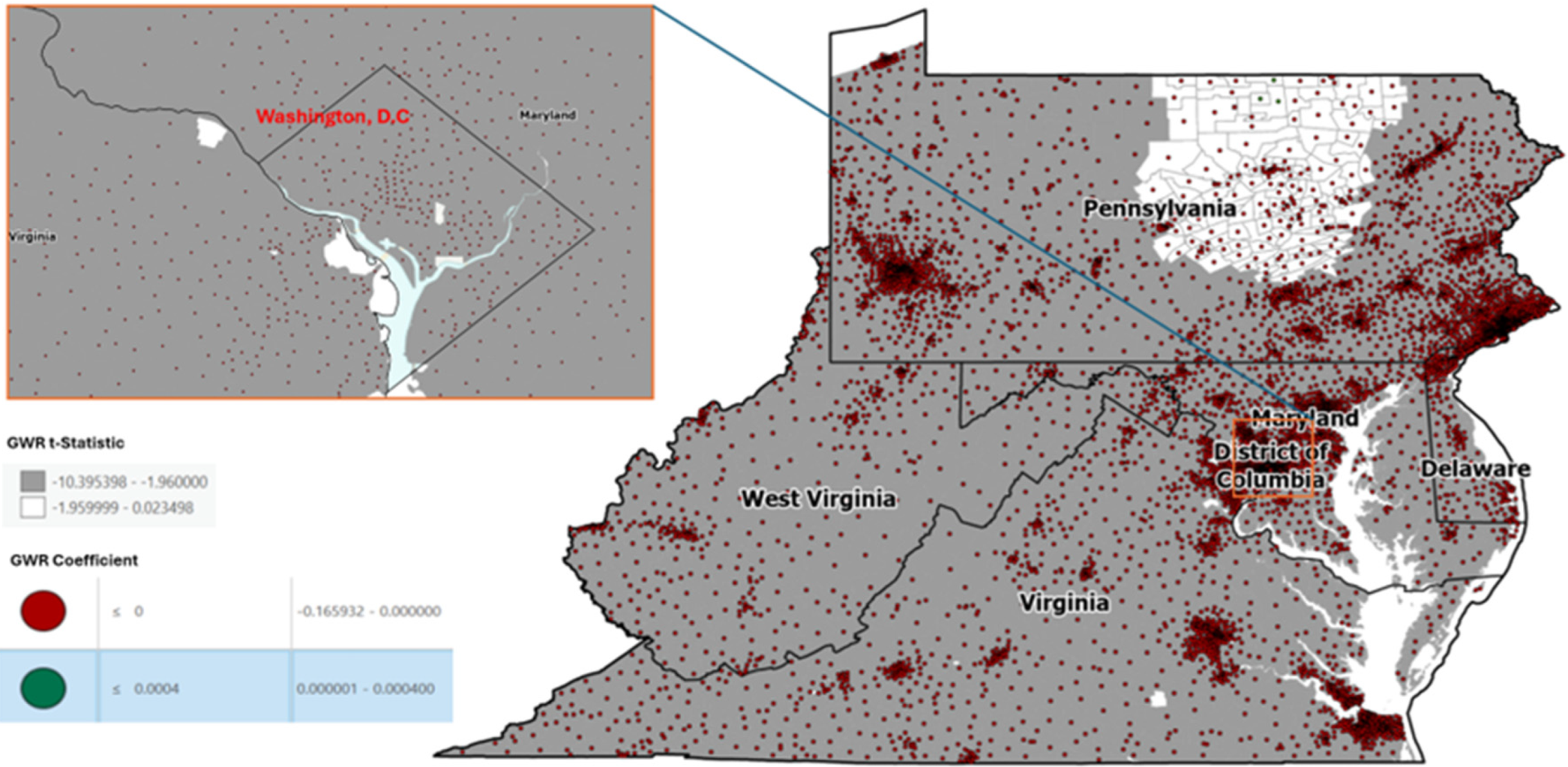
3.2.5. Population Weighted Density Indicator
3.2.6. Social and Community Context (Profile 2)
3.2.7. Geographic Mobility Indicator
3.2.8. Townsend Deprivation Indicator
3.2.9. Food Access Indicator
3.2.10. Education Indicator
3.2.11. Job Participation Indicator
3.2.12. Resource Profile (Profile 3)
3.2.13. Segregation Indicator
3.2.14. Health Access Indicator
3.2.15. Economic Profile (Profile 4)
3.2.16. Income Inequality Indicator
3.2.17. Environmental Hazard Indicator
3.3. GWR Residual Diagnostics
4. Discussion
4.1. Policy Implications
4.2. Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Employment Access Indicator

Appendix B. Affordability Indicator
Appendix C. Walkability Indicator

Appendix D. Population Weighted Density Indicator

Appendix E. Geographic Mobility Indicator
Appendix F. Townsend Deprivation Indicator
Appendix G. Food Access Indicator
Appendix H. Education Indicator
Appendix I. Job Participation Indicator

Appendix J. Segregation Indicator
Appendix K. Health Access Indicator
Appendix L. Income Inequality Indicator

Appendix M. Environmental Hazard Indicator
References
- Govoni, V.; Coletta, E.D.; Fallica, E.; Cesnik, E. The urgent neurological consultation in the population of the province of Ferrara, Italy. Neurol. Sci. 2018, 39, 1253–1259. [Google Scholar] [CrossRef] [PubMed]
- Donkor, E.S. Stroke in the 21st century: A snapshot of the burden, epidemiology and quality of life. Stroke Res. Treat. 2018, 2018, 3238165. [Google Scholar] [CrossRef]
- Kuriakose, D.; Xiao, Z. Pathophysiology and treatment of stroke: Present status and future perspectives. Int. J. Mol. Sci. 2020, 21, 7609. [Google Scholar] [CrossRef]
- Liyuan, P.; Wang, L.; Zhang, R.; Zhao, T.; Jiang, Y.; Han, L. Projected global trends in ischemic stroke incidence, deaths and disability-adjusted life years from 2020 to 2030. Stroke 2023, 54, 1330–1339. [Google Scholar] [CrossRef]
- Global Burden of Disease 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the global burden of disease study. Lancet Neurol. 2021, 20, P795–P820. [Google Scholar] [CrossRef]
- Vaughan, A.S.; Woodruff, R.C.; Shay, C.M.; Loustalot, F.; Casper, M. Progress toward achieving national targets for reducing coronary heart disease and stroke mortality: A county-level perspective. J. Am. Heart Assoc. 2021, 10, e019562. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart disease and stroke statistics—2020 update: A report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef]
- Reshetnyak, E.; Ntamatungiro, M.; Pinheiro, L.C.; Howard, V.J.; Carson, A.P.; Martin, K.D.; Safford, M.M. Impact of multiple social determinants of health on incident stroke. Stroke 2020, 51, 2445–2453. [Google Scholar] [CrossRef] [PubMed]
- Yadav, R.S.; Chaudhary, D.; Avula, V.; Shahjouei, S.; Azarpazhooh, M.R.; Abedi, V.; Li, J.; Zand, R. Social determinants of stroke hospitalization and mortality in United States counties. J. Clin. Med. 2022, 11, 4101. [Google Scholar] [CrossRef] [PubMed]
- Sarfo, F.S.; Ovbiagele, B. Utilizing implementation science to bridge cerebrovascular health disparities: A local to global perspective. Curr. Neurol. Neurosci. Rep. 2022, 22, 293–303. [Google Scholar] [CrossRef]
- Robertson, S.; Dawit, R.; Moore, J.; Odoi, A. An exploratory investigation of geographic disparities of stroke prevalence in Florida using circular and flexible spatial scan statistics. PLoS ONE 2019, 14, e0218708. [Google Scholar]
- Ciliberty-Vargas, M.; Sacco, R. Stroke Registries: Utilizing Comprehensive Data to Improve Outcomes; EMSWORLD: Malvern, PA, USA, 2023; Available online: https://www.hmpgloballearningnetwork.com/site/emsworld/article/219021/stroke-registries-utilizing-comprehensive-data-improve-outcomes (accessed on 10 March 2024).
- Howard, G. Rural-urban differences in stroke risk. Prev. Med. 2021, 152, 106661. [Google Scholar] [CrossRef]
- Yaemsiri, S.; Alfier, J.M.; Moy, E.; Rossen, L.M.; Bastian, B.; Bolin, B.; Ferdinald, A.O.; Callaghan, T.; Heron, M. Healthy people 2020: Rural areas lag in achieving targets for major causes of death. Health Aff. 2019, 38, 2027–2031. [Google Scholar] [CrossRef]
- Wang, C.H.; Chen, N. A geographically weighted regression approach to investigating the spatially varied built-environment effects on community opportunity. J. Transp. Geogr. 2017, 62, 136–147. [Google Scholar] [CrossRef]
- Lachkhem, Y.; Minvielle, E.; Rican, S. Geographic variations of stroke hospitalization across France: A diachronic cluster analysis. Stroke Res. Treat. 2018, 2018, 1897569. [Google Scholar] [CrossRef]
- Balamurugan, A.; Delongchamp, R.; Batees, J.H.; Mehla, J.L. The neighborhood where you live is a risk factor for stroke. Circ. Cardiovasc. Qual. Outcomes 2013, 6, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Ogojiaku, C.N.; Allen, J.C.; Anson-Dwamena, R.; Barnett, K.S.; Adetona, O.; Im, W.; Hood, D.B. The health opportunity index: Understanding the input to disparate health outcomes in vulnerable and high-risk census tracts. Int. J. Environ. Res. Public Health 2020, 17, 5767. [Google Scholar] [CrossRef]
- Friedman, C. The social determinants of health index. Rehabil. Psychol. 2020, 65, 11–21. [Google Scholar] [CrossRef]
- Wang, R.; Dong, P.; Dong, G.; Xiang, X.; Huang, J.; Yang, L. Exploring the impacts of street-level greenspace on stroke and cardiovascular diseases in Chinese adults. Ecotoxicol. Environ. Saf. 2022, 243, 113974. [Google Scholar] [CrossRef]
- Nunez, M.B.F.; Suzman, L.C.; Maneja, R.; Bach, A.; Marquet, O.; Anguelovski, I.; Knobel, P. The differences by sex and gender in the relationship between urban greenness and cardiometabolic health: A systematic review. J. Urban Health 2022, 99, 1054–1067. [Google Scholar] [CrossRef] [PubMed]
- Oakes, J.M.; Andrade, K.E.; Biyoow, I.M.; Cowan, L.T. Twenty years of neighborhood effect research: An assessment. Curr. Epidemiol. Rep. 2015, 2, 80–87. [Google Scholar] [CrossRef]
- Fareed, N.; Singh, P.; Jonnaiagadda, P.; Swoboda, C.; Odden, C.; Doogan, N. Construction of the Ohio children’s opportunity index. Front. Public Health 2022, 10, 734105. [Google Scholar] [CrossRef]
- U.S. Census Bureau. Quick Facts United States. 2024. Available online: https://www.census.gov/quickfacts/ (accessed on 30 March 2024).
- Cruz-Flores, S.; Rabinstein, A.; Biller, J.; Elkind, M.S.V.; Griffith, P.; Gorelick, P.B.; Howard, G.; Leira, E.C.; Morgenstern, L.B.; Ovbiagele, B.; et al. Racial-ethnic disparities in stroke care: The American experience: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011, 42, 2091–2116. [Google Scholar] [CrossRef]
- U.S. Department of Health & Human Services. Region 3. 2021. Available online: https://www.hhs.gov/ash/about-ash/regional-offices/region-3/index.html (accessed on 10 March 2024).
- Integrated Public Use Microdata Series, National Historical Geographic Information System. Geographic Crosswalks. 2024. Available online: https://www.nhgis.org/geographic-crosswalks (accessed on 10 March 2024).
- Stiefel, M.C.; Straszewski, T.; Taylor, J.C.; Huang, C.; An, J.; Wilson-Anumudu, F.J.; Cheadle, A. Using the county health rankings framework to create national percentile scores for health outcomes and health factors. Perm. J. 2021, 25, 20.012. [Google Scholar] [CrossRef]
- Lessani, M.N.; Zhenlong, L. SGWR: Similarity and geographically weighted regression. Int. J. Geogr. Inf. Sci. 2024, 38, 1232–1255. [Google Scholar] [CrossRef]
- Environmental System Research Institute. How Geographically Weighted Regression Works. Available online: https://pro.arcgis.com/en/pro-app/latest/tool-reference/spatial-statistics/how-geographicallyweightedregression-works.htm (accessed on 10 March 2024).
- Environmental System Research Institute. How Multiscale Geographic Weighted Regression (MGWR) Works. Available online: https://pro.arcgis.com/en/pro-app/latest/tool-reference/spatial-statistics/how-multiscale-geographically-weighted-regression-mgwr-works.htm (accessed on 10 March 2024).
- BioMedware. Spatial Autocorrelation Analysis of Residuals and Geographically Weighted Regression; BioMedware: Ann Arbor, MI, USA, 2014. [Google Scholar]
- D.C. Policy Center. Reducing Barriers for Job-Seekers. 2018. Available online: https://www.dcpolicycenter.org/publications/reducing-barriers-for-job-seekers-in-d-c-and-the-metro-region/ (accessed on 10 March 2024).
- Hoehner, C.M.; Barlow, C.E.; Allen, P.; Schootman, M. Commuting distance, cardiorespiratory fitness, and metabolic risk. Am. J. Prev. Med. 2012, 42, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Sabih, A.; Tadi, P.; Kumar, A. Stroke Prevention, 3. In StartPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024; Available online: https://www.ncbi.nlm.nih.gov/books/NBK470234 (accessed on 10 March 2024).
- Baltimore City Department of Transportation. Baltimore City Strategic Highway Safety Plan (2022–2026). Available online: https://transportation.baltimorecity.gov/sites/default/files/Baltimore%20City%20SHSP%20Part%201.pdf (accessed on 10 March 2024).
- D.C. Policy Center. D.C. Policy Center’s Research and Publications on Racial Equity and Economic and Social Inequalities. 2024. Available online: https://www.dcpolicycenter.org/research-and-publications-on-racial-equity-and-economic-and-social-inequalities/ (accessed on 10 March 2024).
- Rundle, A.G.; Neckerman, K.M.; Judd, S.E.; Colabianchi, N.; Moore, K.A.; Quinn, J.W.; Hirsch, J.A.; Lovasi, G.S. Cumulative experience of neighborhood walkability and change in weight and waist circumference in REGARDS. Am. J. Epidemiol. 2023, 192, 1960–1970. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.; Khan, M.A.; Zehra, F.; Wasay, M.; Khan, R.N.; Aisha. Potential risk factors of stroke: A community-based, cross-sectional study from Sindh province of Pakistan. Khyber Med. Univ. J. 2020, 12, 25–28. [Google Scholar] [CrossRef]
- Tran, P.; Tran, L.; Tran, L. A cross-sectional analysis of differences in physical activity levels between stroke belt and non-stroke belt U.S. adults. J. Stroke Cerebrovasc. Dis. 2019, 28, 104432. [Google Scholar] [CrossRef]
- Piamjariyakul, U.; Mckenrick, S.R.; Smothers, A.; Giolzetti, A.; Melnick, H.; Beaver, M.; Shafique, S.; Wang, K.; Carte, K.J.; Grimes, B.; et al. Developing, implementing, and evaluating the visiting Neighbors’ program in rural Appalachia: A quality improvement protocol. PLoS ONE 2024, 19, e0296438. [Google Scholar] [CrossRef]
- Garcia, M.C.; Faul, M.; Dowling, N.F.; Thomas, C.C.; Iadermarco, M.F. Bridging the gap in potentially excess deaths between rural and urban counties in the United States. Public Health Rep. 2020, 135, 177–180. [Google Scholar] [CrossRef] [PubMed]
- Sayin, Y.; Calma, E. Priced Out: Where Can D.C’s Essential Workers Afford to Live? District of Columbia Policy Center: Washington, DC, USA, 2024; Available online: https://www.dcpolicycenter.org/publications/priced-out-where-can-d-c-s-essential-workers-afford-to-live/ (accessed on 20 March 2024).
- Brink-Johnson, A.; Lubin, J. Structural Racism in Washington, DC Facts, Figures and Opportunities for Advancing Racial Equity; Center for Urban and Racial Equity: Washington, DC, USA, 2020; Available online: https://urbanandracialequity.org/wp-content/uploads/2020/08/Structural-Racism-in-Washington-DC-1.pdf (accessed on 20 March 2024).
- Zhang, B.; Sun, Q.; Lv, Y.; Sun, T.; Zhao, W.; Yan, R.; Guo, Y. Influencing factors for decision-making delay in seeking medical care among acute ischemic stroke patients in rural areas. Patient Educ. Couns. 2023, 108, 107614. [Google Scholar] [CrossRef] [PubMed]
- Radosavljevic, S.; Haider, L.J.; Lade, S.J.; Schluter, M. Implications of poverty traps across levels. World Dev. 2021, 144, 105437. [Google Scholar] [CrossRef]
- Farah, M.J.; Hook, C.J. Trust and the poverty trap. Proc. Natl. Acad. Sci. USA 2017, 114, 5327–5329. [Google Scholar] [CrossRef]
- Sheth, M.S.; Jeong, I.; Chu, A.; Basque, S.; Fang, J.; Austin, P.C.; McNaughton, C.D.; Abdel-Qadir, H.M.; Ko, D.T.; Lee, D.S.; et al. Abstract 15416: High neighborhood-level material deprivation is associated with increased rates of cardiovascular outcomes in patients with ASCVD: A population-based cohort study. Circulation 2023, 148, A15416. [Google Scholar] [CrossRef]
- Thorpe, L.E.; Adhikari, S.; Lopez, P.; Kanchi, R.; McClure, L.A.; Hirsch, A.G.; Howell, C.R.; Zhu, A.; Alemi, F.; Rummo, P.; et al. Neighborhood socioeconomic environment and risk of type 2 diabetes: Associations and mediation through food environment pathways in three independent study samples. Diabetes Care 2022, 45, 798–810. [Google Scholar] [CrossRef]
- Oh, W.A.; Yoon, S.; Noh, J.; Sohn, J.; Kim, C.; Heo, J. Geographical variations and influential factors in prevalence of cardiometabolic diseases in South Korea. PLoS ONE 2018, 13, e0205005. [Google Scholar] [CrossRef]
- Hou, J.; Zhou, W.; Zhu, K.; Ren, X. The impact of labor force participation on elderly health in China. Healthcare 2023, 11, 160. [Google Scholar] [CrossRef]
- Boheim, R.; Horvath, T.; Leoni, T.; Sielauer, M. The impact of health and education on labor force participation in aging societies: Projections for the United States and Germany from dynamic microsimulations. Popul. Res. Policy Rev. 2023, 42, 39. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Stroke Facts. 2024. Available online: https://www.cdc.gov/stroke/data-research/facts-stats/index.html (accessed on 20 March 2024).
- U.S. Census Bureau. 2020 Census Tallies. 2022. Available online: https://www.census.gov/geographies/reference-files/time-series/geo/tallies.html (accessed on 20 March 2024).
- Cummings, D.M.; Patil, S.P.; Long, D.L.; Guo, B.; Cherrington, A.; Safford, M.A.; Judd, S.E.; Howard, V.J.; Howard, G.; Carson, A.P. Does the association between Hemoglobin A1C and risk of cardiovascular events vary by residential segregation? The reasons for geographic and racial differences in stroke (REGARDS) study. Diabetes Care 2021, 44, 1151–1158. [Google Scholar] [CrossRef]
- Sims, M.; Kershaw, K.N.; Breathett, K.; Jackson, E.A.; Lewis, L.M.; Mujahid, M.S.; Suglia, S.F. The importance of housing and cardiovascular health and wellbeing: A scientific statement from the American Heart Association. Circ. Cardiovasc. Qual. Outcome 2020, 13, e000089. [Google Scholar] [CrossRef] [PubMed]
- Allen, E.M.; Call, K.T.; Beebe, T.J.; McAlpine, D.D.; Johnson, P.J. Barriers to care and healthcare utilization among the publicly insured. Med. Care 2017, 55, 207–214. [Google Scholar] [CrossRef] [PubMed]
- District of Columbia Department of Health. Health Equity Summary Report. 2018. Available online: https://disb.dc.gov/sites/default/files/dc/sites/disb/publication/attachments/her_summary_report_final_with_letter_and_table_02_08_2019.pdf (accessed on 20 March 2024).
- D.C. Policy Center. Inequalities in Health Care Need and Demand Across the District. 2021. Available online: https://www.dcpolicycenter.org/publications/inequalities-health-care-need-demand/ (accessed on 20 March 2024).
- Naveed, M. Income Inequality in DC Highest in the Country; DC Fiscal Policy Institute: Washington, DC, USA, 2017. [Google Scholar]
- Parcha, V.; Kalra, R.; Suri, S.S.; Malla, G.; Wang, T.J.; Arora, G. Geographic variation in cardiovascular health among American adults. Mayo Clin. Proc. 2021, 96, 1770–1781. [Google Scholar] [CrossRef]
- Cote, K.; Pudlo, M.; Jost-Price, E.; Leung, L. Neighborhood income inequality associated with functional independence after ischemic stroke: A cohort study (S28.007). Neurology 2022, 98, 626. [Google Scholar] [CrossRef]
- Environmental Protection Agency. EPA’s Environmental Justice Screening and Mapping Tool (Version 2.3). 2024. Available online: https://www.epa.gov/system/files/documents/2024-07/ejscreen-tech-doc-version-2-3.pdf (accessed on 20 March 2024).
- Gaines, B.; Kloog, I.; Zucker, I.; Ifergane, G.; Novack, V.; Libruder, C.; Hershkovitz, Y.; Sheffield, P.E.; Yitshak-Sade, M. Particulate air pollution exposure and stroke adults in Israel. Int. J. Environ. Res. Public Health 2023, 20, 1482. [Google Scholar] [CrossRef]
- Tang, C.; Chen, Y.; Song, Q.; Ma, J.; Zhou, Y.; Gong, L.; Chen, X.; Qu, J.; Luo, Y. Short-term exposure to air pollution and occurrence of emergency stroke in Chongqing, China. Int. Arch. Occup. Environ. Health 2021, 94, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Festa, N.; Burrows, K.; Kim, D.C.; Gill, T.M.; Bell, M.L. Residential exposure to petroleum refining and stroke in the southern united states. Environ. Res. Lett. 2022, 17, 094018. [Google Scholar] [CrossRef]
- City of Philadelphia Office of Sustainability. Greenworks Philadelphia. 2022. Available online: https://www.phila.gov/media/20220421120407/OOS-Greenworks-Review-2022.pdf (accessed on 20 March 2024).
- Hallum, S.H.; Hughey, S.M.; Wende, M.E.; Stowe, E.W.; Kaczynski, A.T. Healthy and unhealthy food environments are linked with neighborhood socio-economic disadvantage: An innovative geospatial approach to understanding food access inequities. Public Health Nutr. 2020, 23, 3190–3196. [Google Scholar] [CrossRef]
- Caetano, G.; Maheshri, V. A Unified Empirical Framework to Study Segregation; Center for the Economics of Human Development: Chicago, IL, USA, 2021; Available online: https://cehd.uchicago.edu/wp-content/uploads/2021/09/Caetano-Maheshri-Segregation-CM.pdf (accessed on 20 March 2024).
- D.C. Policy Center. Symposium: Achieving Racial Equity in Housing Outcomes in D.C. 2018. Available online: https://www.dcpolicycenter.org/publications/racial-equity-housing-symposium/ (accessed on 20 March 2024).
| Variables | U.S. | DE | VA | WV | PA | MD | DC |
|---|---|---|---|---|---|---|---|
| Persons 65+ years | 17.70% | 21.30% | 17.20% | 21.50% | 20.00% | 17.30% | 13.10% |
| Black | 13.70% | 24.10% | 20.00% | 3.80% | 12.30% | 31.60% | 44.40% |
| American Indian/ Alaskan Native | 1.30% | 0.70% | 0.60% | 0.30% | 0.50% | 0.80% | 0.70% |
| Asian | 6.40% | 4.40% | 7.40% | 0.90% | 4.20% | 7.10% | 4.90% |
| Native Hawaiian and other Pacific Islander | 0.30% | 0.10% | 0.10% | 0 | 0.10% | 0.10% | 0.20% |
| Two or more races | 3.10% | 3.10% | 3.50% | 2.10% | 2.40% | 3.30% | 3.30% |
| Hispanic or Latino | 19.50% | 11.10% | 11.20% | 2.20% | 8.90% | 12.60% | 12.00% |
| White | 58.40% | 58.90% | 59.10% | 90.90% | 74.10% | 47.30% | 37.70% |
| High school or higher | 89.10% | 91.20% | 91.10% | 88.40% | 91.70% | 91.00% | 92.70% |
| Uninsured (under 65) | 9.50% | 6.90% | 7.60% | 7.40% | 6.50% | 7.10% | 3.30% |
| Civilian labor force (age 16+) | 63.00% | 61.90% | 63.80% | 53.10% | 62.80% | 66.60% | 71.40% |
| Median income | $75,149 | $79,325 | $87,249 | $55,217 | $73,170 | $98,461 | $101,722 |
| Persons in poverty | 11.10% | 9.40% | 10.60% | 17.90% | 11.80% | 9.60% | 13.30% |
| Statistics | GWR |
|---|---|
| R-squared | 76.90% |
| Adjusted R-squared | 70.42% |
| AICc | 15,537.40 |
| Sigma-squared | 0.29 |
| Sigma-squared MLE | 0.23 |
| Effective degree of freedom | 6252.18 |
| Statistics | GWR |
|---|---|
| R-squared | 79.70% |
| Adjusted R-squared | 76.92% |
| AICc | 12,173.69 |
| Sigma-squared | 0.23 |
| Sigma-squared MLE | 0.2 |
| Effective degree of freedom | 7054.00 |
| Statistics | GWR |
|---|---|
| R-squared | 68.24% |
| Adjusted R-squared | 63.68% |
| AICc | 15,870.75 |
| Sigma-squared | 0.36 |
| Sigma-squared MLE | 0.32 |
| Effective degree of freedom | 7013.40 |
| Statistics | GWR |
|---|---|
| R-squared | 69.91% |
| Adjusted R-squared | 64.55% |
| AICc | 15,988.29 |
| Sigma-squared | 0.35 |
| Sigma-squared MLE | 0.3 |
| Effective degree of freedom | 6809.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tuktur, W.R.; Cai, B.; Sasser, H.C.; Anson-Dwamena, R. A Geographic Weighted Regression Analysis of the Health Opportunity Index and Stroke Prevalence in Health and Human Services Region 3. Int. J. Environ. Res. Public Health 2025, 22, 1542. https://doi.org/10.3390/ijerph22101542
Tuktur WR, Cai B, Sasser HC, Anson-Dwamena R. A Geographic Weighted Regression Analysis of the Health Opportunity Index and Stroke Prevalence in Health and Human Services Region 3. International Journal of Environmental Research and Public Health. 2025; 22(10):1542. https://doi.org/10.3390/ijerph22101542
Chicago/Turabian StyleTuktur, Wanderimam R., Bin Cai, Howell C. Sasser, and Rexford Anson-Dwamena. 2025. "A Geographic Weighted Regression Analysis of the Health Opportunity Index and Stroke Prevalence in Health and Human Services Region 3" International Journal of Environmental Research and Public Health 22, no. 10: 1542. https://doi.org/10.3390/ijerph22101542
APA StyleTuktur, W. R., Cai, B., Sasser, H. C., & Anson-Dwamena, R. (2025). A Geographic Weighted Regression Analysis of the Health Opportunity Index and Stroke Prevalence in Health and Human Services Region 3. International Journal of Environmental Research and Public Health, 22(10), 1542. https://doi.org/10.3390/ijerph22101542






