Air Quality Index as a Predictor of Respiratory Morbidity in At-Risk Populations
Abstract
1. Introduction
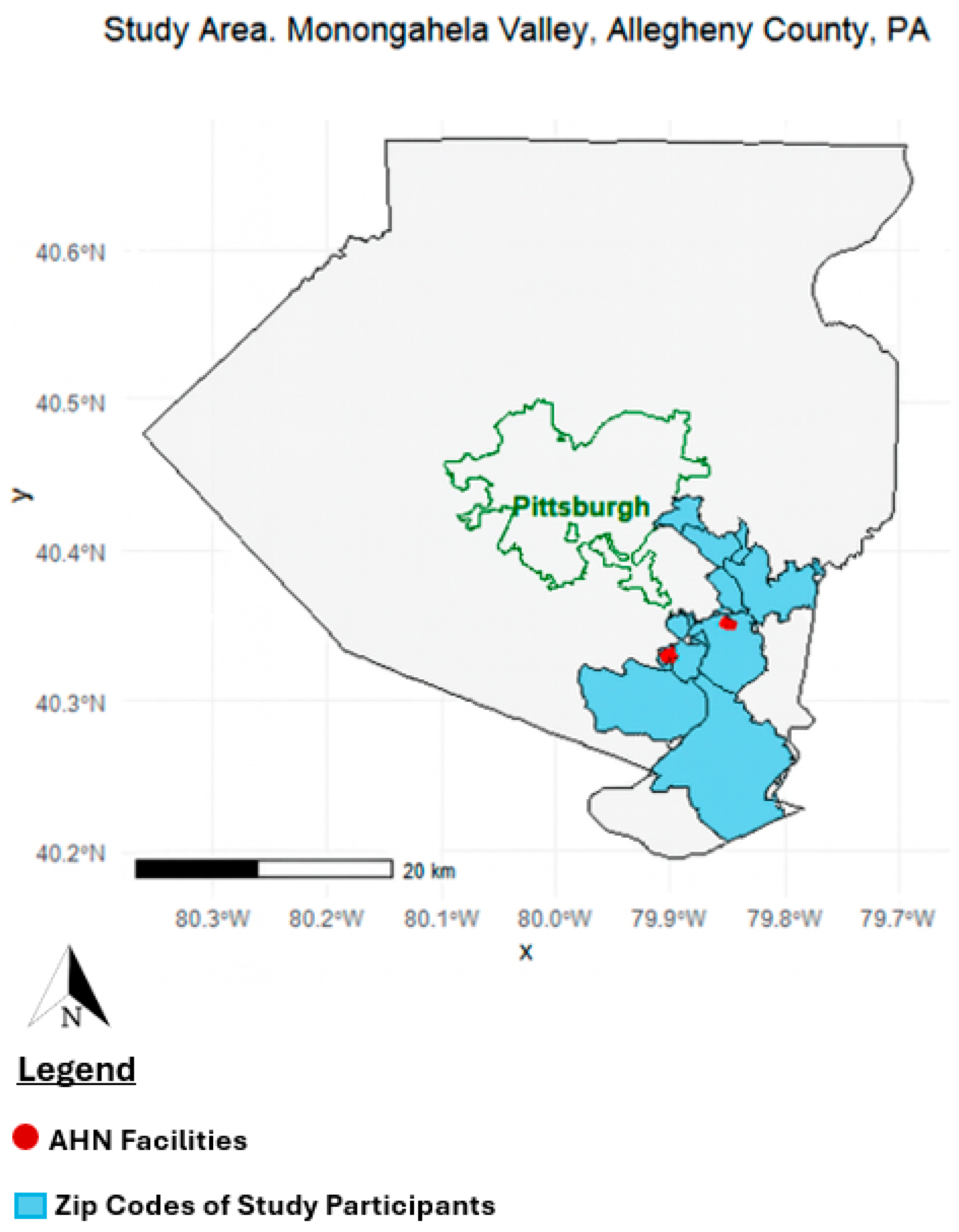
2. Methods
Statistical Methods
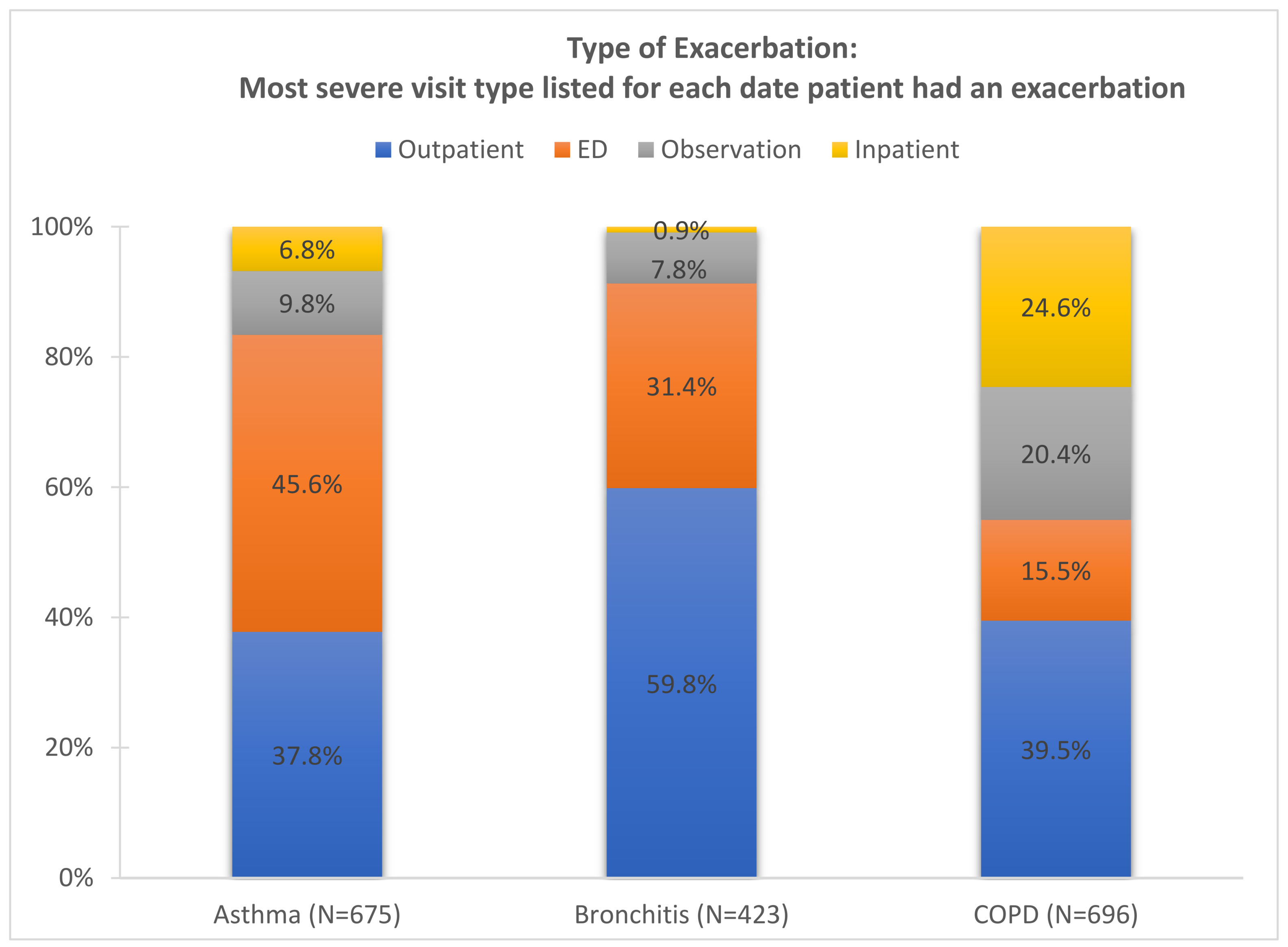
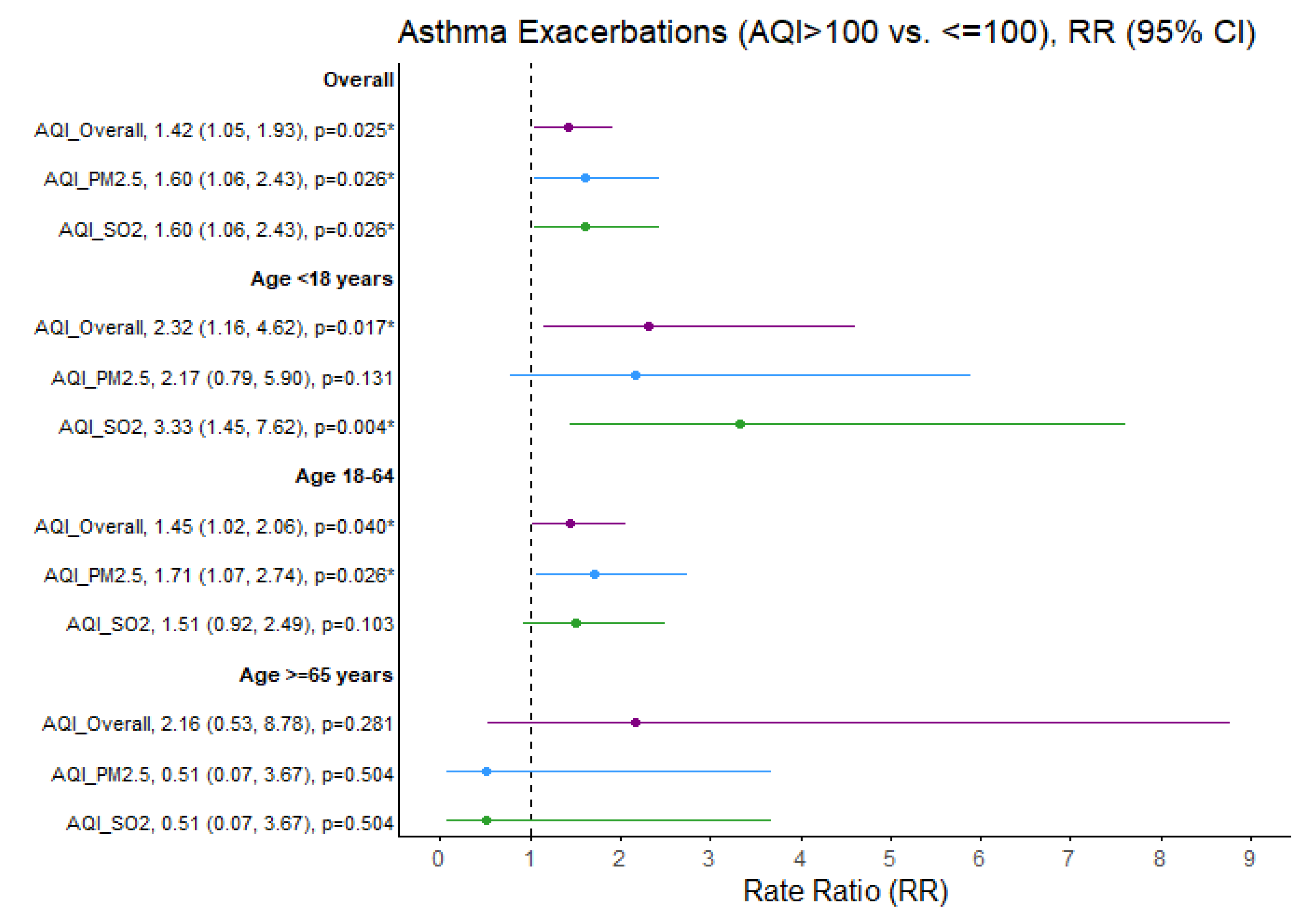
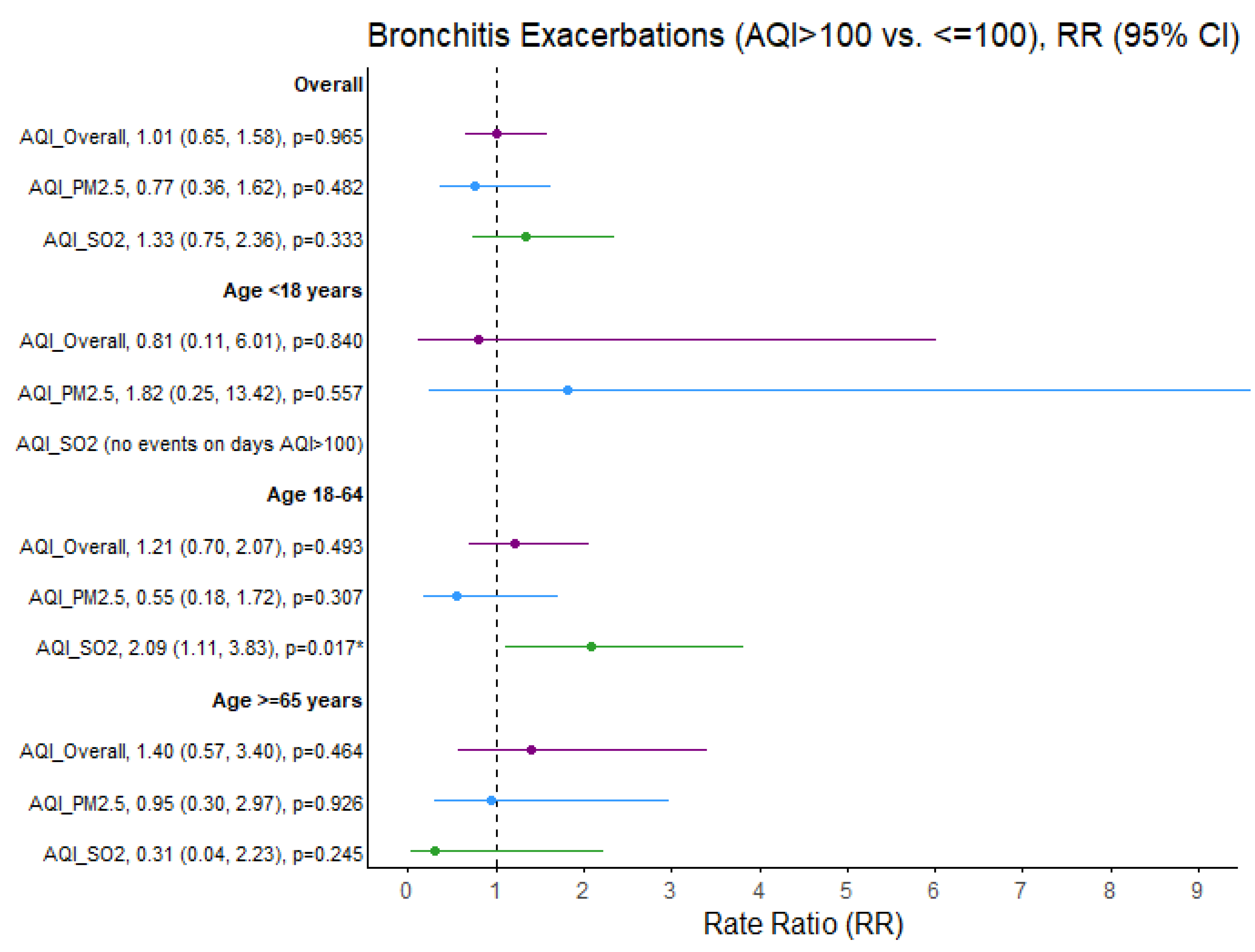
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AQI | Air Quality Index |
| ED | Emergency Department |
| PM2.5 | Particulate matter less than 2.5 μm in diameter |
| PM10 | Particulate matter less than 10 μm in diameter |
| SO2 | Sulfur dioxide |
| SES | Socioeconomic status |
| COPD | Chronic obstructive pulmonary disorder |
| IRB | Institutional review board |
| AHN | Allegheny Health Network |
| ACS | American Community Survey |
| EPA | Environmental Protection Agency |
Appendix A
| Zip Codes | City Name | Number of Residents Living Within Zip Code |
|---|---|---|
| 15025 | Jefferson Hills | 16,298 |
| 15034 | Dravosburg | 1730 |
| 15037 | Elizabeth | 10,485 |
| 15045 | Glassport | 4371 |
| 15104 | Braddock | 8669 |
| 15110 | Duquesne | 5543 |
| 15122 | West Mifflin | 19,745 |
| 15132 | McKeesport | 21,136 |
| 15133 | McKeesport | 6189 |
| 15137 | North Versailles | 9884 |
| 15218 | Pittsburgh | 13,495 |
| Date | AQI Responsible Pollutant(s) (AQI > 100) | Lawrenceville Ozone (ppm) 8 h | Liberty PM2.5 (μg/m3) 24 h Ave. | Liberty SO2 (ppb) Max 1 h | N. Braddock SO2 (ppb) Max 1 h | Lawrenceville NO2 (ppb) Max 1 h | Parkway E. NO2 (ppb) Max 1 h |
|---|---|---|---|---|---|---|---|
| 03-Jan-2018 | PM2.5 Liberty | 0.023 | 47.458 | 32 | 12 | 35 | 37.1 |
| 19-Jan-2018 | SO2 Liberty | 0.033 | 18.417 | 130 | 5 | 19 | 13.4 |
| 10-Feb-2018 | SO2 N. Braddock | 31.208 | 68 | 91 | 28 | 34.1 | |
| 18-Mar-2018 | PM2.5 Liberty | 0.040 | 37.391 | 62 | 7 | 34 | 43.7 |
| 12-Apr-2018 | SO2 N. Braddock | 20.458 | 34 | 84 | 26 | 25.5 | |
| 13-Apr-2018 | SO2 N. Braddock | 0.060 | 27.667 | 50 | 113 | 16 | 20.9 |
| 01-May-2018 | PM2.5 Liberty | 0.067 | 38.000 | 65 | 62 | 26 | 38.1 |
| 02-May-2018 | SO2 Liberty | 0.059 | 35.000 | 76 | 50 | 22 | 36.8 |
| 04-May-2018 | SO2 Liberty | 0.051 | 12.350 | 155 | 2 | 15 | 17.6 |
| 09-May-2018 | SO2 Liberty | 0.062 | 19.958 | 144 | 30 | 20 | 21.8 |
| 12-May-2018 | SO2 Liberty | 0.053 | 21.875 | 122 | 18 | 8 | 15.4 |
| 26-May-2018 | Ozone | 0.072 | 27.045 | 34 | 2 | 20 | 19.1 |
| 28-May-2018 | Ozone | 0.076 | 24.292 | 36 | 7 | 13 | 16.6 |
| 08-Jun-2018 | Ozone | 0.076 | 26.708 | 24 | 13 | 15 | 25.1 |
| 29-Jun-2018 | Ozone | 0.074 | 30.375 | 43 | 15 | 16 | 20.0 |
| 30-Jun-2018 | Ozone | 0.079 | 27.273 | 0 | 5 | 8 | 24.6 |
| 10-Jul-2018 | Ozone | 0.073 | 25.739 | 50 | 16 | 11 | 29.0 |
| 01-Aug-2018 | SO2 Liberty | 0.043 | 13.917 | 79 | 3 | 13 | 17.0 |
| 13-Dec-2018 | PM2.5 Liberty | 0.019 | 42.875 | 70 | 51 | 32 | 33.3 |
| 26-Dec-2018 | PM2.5 Liberty & SO2 Liberty | 0.026 | 39.833 | 80 | 8 | 28 | 36.2 |
| 28-Dec-2018 | SO2 Liberty | 0.023 | 19.913 | 145 | 2 | 21 | |
| 02-Jan-2019 | SO2 Liberty | 0.018 | 11.625 | 81 | 8 | 13 | 16.0 |
| 03-Jan-2019 | SO2 Liberty | 0.019 | 11.478 | 85 | 9 | 20 | 15.6 |
| 07-Jan-2019 | SO2 N. Braddock | 0.024 | 7.458 | 17 | 83 | 23 | 13.2 |
| 08-Jan-2019 | SO2 Liberty | 0.033 | 26.091 | 80 | 34 | 16 | 15.0 |
| 02-Feb-2019 | PM2.5 Liberty | 0.027 | 69.625 | 64 | 10 | 33 | 32.8 |
| 03-Feb-2019 | PM2.5 Liberty | 0.025 | 75.750 | 61 | 41 | 33 | 32.8 |
| 04-Feb-2019 | PM2.5 Liberty | 0.039 | 74.625 | 52 | 82 | 41 | 38.3 |
| 24-Mar-2019 | PM2.5 Liberty | 0.046 | 38.292 | 54 | 29 | 27 | 34.9 |
| 28-Mar-2019 | PM2.5 Liberty & SO2 Liberty | 0.051 | 35.583 | 82 | 21 | 27 | 29.5 |
| 21-Dec-2019 | PM2.5 Liberty | 0.007 | 41.292 | 45 | 15 | 32 | 35.3 |
| 22-Dec-2019 | PM2.5 Liberty | 0.020 | 49.708 | 42 | 20 | 28 | 35.9 |
| 23-Dec-2019 | PM2.5 Liberty | 0.006 | 57.000 | 45 | 31 | 45 | 36.5 |
| 24-Dec-2019 | PM2.5 Liberty | 0.012 | 52.750 | 31 | 2 | 22 | 34.6 |
| 25-Dec-2019 | PM2.5 Liberty | 0.002 | 37.792 | 62 | 38 | 23 | 29.5 |
| 26-Dec-2019 | PM2.5 Liberty | 0.010 | 45.083 | 71 | 20 | 32 | 29.8 |
| 23-Feb-2020 | PM2.5 Liberty | 0.042 | 36.125 | 44 | 38 | 30 | 31.2 |
| Days | Daily Exacerbation Rate Ratios (95% CI) | |||
|---|---|---|---|---|
| AQI | N | Asthma | COPD | Bronchitis |
| Overall | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Good | 416 | ---- | ---- | ---- |
| Moderate | 337 | 0.97 (0.83, 1.13) | 1.09 (0.94, 1.27) | 1.08 (0.89, 1.31) |
| Unhealthy | 37 | 1.40 (1.02, 1.91) * | 0.99 (0.68, 1.43) | 1.05 (0.66, 1.65) |
| Ozone | ||||
| Good | 686 | ---- | ---- | ---- |
| Moderate | 69 | 1.01 (0.77, 1.31) | 1.15 (0.90, 1.48) | 0.87 (0.61, 1.24) |
| Unhealthy | 6 | 0.58 (0.19, 1.80) | 0.95 (0.39, 2.29) | 0.91 (0.29, 2.83) |
| PM2.5 | ||||
| Good | 443 | ---- | ---- | ---- |
| Moderate | 330 | 1.03 (0.88, 1.20) | 1.09 (0.93, 1.26) | 1.00 (0.83, 1.22) |
| Unhealthy | 17 | 1.62 (1.07, 2.48) * | 0.97 (0.57, 1.65) | 0.77 (0.36, 1.63) |
| SO2 | ||||
| Good | 693 | ---- | ---- | ---- |
| Moderate | 80 | 0.99 (0.77, 1.28) | 1.16 (0.92, 1.46) | 1.04 (0.76, 1.42) |
| Unhealthy | 17 | 1.60 (1.06, 2.43) * | 1.16 (0.71, 1.87) | 1.33 (0.75, 2.37) |
| NO2 | ||||
| Good | 790 | ---- | ---- | ---- |
| Moderate | 0 | |||
| Unhealthy | 0 | |||
| Days | Daily Exacerbation Rate Ratios (95% CI) | |||
|---|---|---|---|---|
| AQI | N | Asthma | COPD | Bronchitis |
| Overall | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Good | 416 | ---- | ---- | ---- |
| Moderate | 337 | 0.72 (0.45, 1.13) | 0.82 (0.37, 1.83) | |
| Unhealthy | 37 | 2.02 (1.00, 4.11) ~ | 0.75 (0.10, 5.67) | |
| Ozone | ||||
| Good | 686 | ---- | ---- | ---- |
| Moderate | 69 | 0.90 (0.59, 1.37) | 0.40 (0.05, 2.94) | |
| Unhealthy | 6 | 0.44 (0.11, 1.81) | No events | |
| PM2.5 | ||||
| Good | 443 | ---- | ---- | ---- |
| Moderate | 330 | 0.79 (0.50, 1.22) | 0.90 (0.40, 1.99) | |
| Unhealthy | 17 | 1.97 (0.71, 5.43) | 1.74 (0.23, 13.15) | |
| SO2 | ||||
| Good | 693 | ---- | ---- | ---- |
| Moderate | 80 | 0.94 (0.45, 1.94) | 1.58 (0.54, 4.57) | |
| Unhealthy | 17 | 3.31 (1.44, 7.60) * | No events | |
| NO2 | ||||
| Good | 790 | ---- | ---- | ---- |
| Moderate | 0 | |||
| Unhealthy | 0 | |||
| Days | Daily Exacerbation Rate Ratios (95% CI) | |||
|---|---|---|---|---|
| AQI | N | Asthma | COPD | Bronchitis |
| Overall | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Good | 416 | ---- | ---- | ---- |
| Moderate | 337 | 1.03 (0.86, 1.24) | 1.15 (0.90, 1.47) | 1.13 (0.88, 1.46) |
| Unhealthy | 37 | 1.47 (1.02, 2.11) * | 1.03 (0.57, 1.86) | 1.28 (0.74, 2.22) |
| Ozone | ||||
| Good | 686 | ---- | ---- | ---- |
| Moderate | 69 | 1.00 (0.73, 1.38) | 1.40 (0.96, 2.02) ~ | 1.05 (0.68, 1.61) |
| Unhealthy | 6 | 0.52 (0.13, 2.10) | 1.00 (0.25, 4.04) | 0.52 (0.07, 3.74) |
| PM2.5 | ||||
| Good | 443 | ---- | ---- | ---- |
| Moderate | 330 | 1.11 (0.93, 1.33) | 1.07 (0.84, 1.37) | 1.01 (0.78, 1.30) |
| Unhealthy | 17 | 1.79 (1.11, 2.89) * | 1.09 (0.48, 2.46) | 0.55 (0.18, 1.74) |
| SO2 | ||||
| Good | 693 | ---- | ---- | ---- |
| Moderate | 80 | 0.96 (0.71, 1.29) | 1.18 (0.81, 1.71) | 0.88 (0.57, 1.36) |
| Unhealthy | 17 | 1.51 (0.92, 2.48) | 1.07 (0.48, 2.41) | 2.07 (1.13, 3.79) * |
| NO2 | ||||
| Good | 790 | ---- | ---- | ---- |
| Moderate | 0 | |||
| Unhealthy | 0 | |||
| Days | Daily Exacerbation Rate Ratios (95% CI) | |||
|---|---|---|---|---|
| AQI | N | Asthma | COPD | Bronchitis |
| Overall | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Good | 416 | ---- | ---- | ---- |
| Moderate | 337 | 0.90 (0.59, 1.37) | 1.06 (0.87, 1.28) | 1.04 (0.75, 1.45) |
| Unhealthy | 37 | 0.44 (0.11, 1.81) | 0.97 (0.61, 1.54) | 0.73 (0.30, 1.80) |
| Ozone | ||||
| Good | 686 | ---- | ---- | ---- |
| Moderate | 69 | 0.74 (0.32, 1.69) | 0.98 (0.70, 1.38) | 0.67 (0.34, 1.31) |
| Unhealthy | 6 | No events | 0.92 (0.29, 2.86) | 1.71 (0.42, 6.89) |
| PM2.5 | ||||
| Good | 443 | ---- | ---- | ---- |
| Moderate | 330 | 0.87 (0.57, 1.33) | 1.09 (0.90, 1.33) | 1.02 (0.73, 1.41) |
| Unhealthy | 17 | 0.48 (0.07, 3.49) | 0.90 (0.44, 1.82) | 0.95 (0.30, 3.02) |
| SO2 | ||||
| Good | 693 | ---- | ---- | ---- |
| Moderate | 80 | 1.22 (0.65, 2.30) | 1.12 (0.83, 1.52) | 1.22 (0.74, 2.00) |
| Unhealthy | 17 | 0.52 (0.07, 3.76) | 1.21 (0.67, 2.21) | 0.32 (0.05, 2.28) |
| NO2 | ||||
| Good | 790 | ---- | ---- | ---- |
| Moderate | 0 | |||
| Unhealthy | 0 | |||
References
- United States Environmental Protection Agency (EPA). Air Quality Index: A Guide to Air Quality and Your Health; U.S. Environmental Protection Agency: Research Triangle Park, NC, USA, 2014. Available online: https://www.airnow.gov/aqi/aqi-basics/ (accessed on 9 September 2025).
- World Health Organization (WHO). Air Quality and Health; World Health Organization: Geneva, Switzerland, 2018; Available online: https://www.who.int/health-topics/air-pollution (accessed on 6 September 2025).
- Adam, M.; Schikowski, T.; Carsin, A.E.; Cai, Y.; Jacquemin, B.; Sanchez, M.; Vierkötter, A.; Marcon, A.; Keidel, D.; Sugiri, D.; et al. Adult lung function and long-term air pollution exposure. ESCAPE: A multicenter cohort study and meta-analysis. Eur. Respir. J. 2015, 45, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Altman, M.C.; Kattan, M.; O’Connor, G.T.; Murphy, R.C.; Whalen, E.; LeBeau, P.; Calatroni, A.; Gill, M.A.; Gruchalla, R.S.; Liu, A.H.; et al. Associations between outdoor air pollutants and nonviral asthma exacerbations and airway inflammatory responses in children and adolescents living in urban areas in the USA: A retrospective secondary analysis. Lancet Planet Health 2023, 7, e33. [Google Scholar] [CrossRef] [PubMed]
- Guilbert, A.; De Cremer, K.; Heene, B.; Demoury, C.; Aerts, R.; Declerck, P.; Brasseur, O.; Van Nietuwenhuyse, A. Personal exposure to traffic-related air pollutants and relationships with respiratory symptoms and oxidative stress: A pilot cross-sectional study among urban green space workers. Sci. Total Environ. 2019, 649, 620–628. [Google Scholar] [CrossRef]
- Anderson, H.R.; Ponce De Leon, A.; Bland, J.M.; Bower, J.S.; Emberlin, J.; Strachan, D.P. Air pollution, pollens, and daily admissions for asthma in London 1987–1992. Thorax 1998, 53, 842–848. [Google Scholar] [CrossRef]
- Horn, S.A.; Dasgupta, P.K. The Air Quality Index (AQI) in historical and analytical perspective a tutorial review. Talanta 2024, 267, 125260. [Google Scholar] [CrossRef]
- Ikram, M.; Yan, Z.J. Statistical Analysis of the Impact of AQI on Respiratory Disease in Beijing: Application Case 2009. Energy Procedia 2017, 107, 340–344. [Google Scholar] [CrossRef]
- Allegheny County Health Department. Allegheny County Emission Inventory Report, 2015–2017; Allegheny County Health Department: Pittsburgh, PA, USA, 2019.
- Jacobs, E.T.; Burgess, J.L.; Abbott, M.B. The Donora Smog Revisited: 70 Years After the Event That Inspired the Clean Air Act. Am. J. Public Health 2018, 108, S85–S88. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gentile, D.A.; Morphew, T.; Elliott, J.; Presto, A.A.; Skoner, D.P. Asthma Prevalence and Control among Schoolchildren Residing near Outdoor Air Pollution Sites. J. Asthma 2020, 59, 12–22. [Google Scholar] [CrossRef]
- Fabisiak, J.P.; Jackson, E.M.; Brink, L.A.L.; Presto, A.A. A risk-based model to assess environmental justice and coronary heart disease burden from traffic-related air pollutants. Environ. Health. 2020, 19, 34. [Google Scholar] [CrossRef]
- Gentile, D.A.; Sossong, N.; Morphew, T.; Presto, A.; Elliott, J. Impact of Environmental Factors on Recurrent Asthma Exacerbations among Inner-CIty Schoolchildren from the Pittsburgh Region. J. Allergy Clin. Immunol. 2017, 139, AB5. [Google Scholar] [CrossRef]
- DePerrior, S.; Rager, J.R.; Gentile, D.; Talbott, E.O. The Relationship between Pollen, Air Pollution and Asthma Exacerbations in Children in Allegheny County, Pennsylvania: A Case-Crossover Analysis. Arch. Epidemiol. 2021, 5, 148. [Google Scholar] [CrossRef]
- Kaiser, J.E.; Bakian, A.V.; Silver, R.M.; Clark, E.A.S. Clinical variables associated with adverse maternal outcomes in puerperal group a streptococci infection. Obstet. Gynecol. 2018, 132, 179–184. [Google Scholar] [CrossRef]
- Liu, J.; Clark, L.P.; Bechle, M.J.; Hajat, A.; Kim, S.Y.; Robinson, A.L.; Sheppard, L.; Szpiro, A.A.; Marshall, J.D. Disparities in Air Pollution Exposure in the United States by Race/Ethnicity and Income, 1990–2010. Environ. Health Perspect. 2021, 129, 127005. [Google Scholar] [CrossRef]
- Cohen, A.J.; Brauer, M.; Burnett, R.; Anderson, H.R.; Frostad, J.; Estep, K.; Sheppard, L.; Szpiro, A.A.; Marshall, J.D.; Balakrishnan, K.; et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017, 389, 1907–1918. [Google Scholar] [CrossRef]
- Smith, R.B.; Beevers, S.D.; Gulliver, J.; Dajnak, D.; Fecht, D.; Blangiardo, M.; Douglass, M.; Hansell, A.L.; Anderson, H.R.; Kelly, F.J.; et al. Impacts of air pollution and noise on risk of preterm birth and stillbirth in London. Environ. Int. 2020, 134, 105290. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency (EPA). Download Daily Data; EPA: Washington, DC, USA, 2025. Available online: https://www.epa.gov/outdoor-air-quality-data/download-daily-data (accessed on 11 September 2025).
- Chen, C.; Wang, Y.; Song, J.; Yan, J. The impact of air pollution on hospitalization for COPD patients in China. Eur. J. Public Health 2024, 34, 150–155. [Google Scholar] [CrossRef]
- U.S. Census Bureau. American Community Survey 5-Year Estimates, 2015–2019; U.S. Census Bureau: Washington, DC, USA, 2020.
- Ko, U.W.; Kyung, S.Y. Adverse Effects of Air Pollution on Pulmonary Diseases. Tuberc. Respir. Dis. 2022, 85, 313–319. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, H.; Jung, J.H.; Kim, B.G.; Park, D.W.; Park, T.S.; Moon, J.-Y.; Kim, T.-H.; Sohn, J.W.; Yoon, H.J.; et al. Asthma Increases Long-Term Risk of Death by Suicide: A Nationwide Population-Based Cohort Study. J. Allergy Clin. Immunol. Pract. 2025, 13, 559–567.e3. [Google Scholar] [CrossRef]
- Chen, M.J.; Leon Guo, Y.; Lin, P.; Chiang, H.C.; Chen, P.C.; Chen, Y.C. Air quality health index (AQHI) based on multiple air pollutants and mortality risks in Taiwan: Construction and validation. Environ. Res. 2023, 231 Pt 2, 116214. [Google Scholar] [CrossRef]
- Cvietusa, P.J.; Goodrich, G.K.; Steiner, J.F.; Shoup, J.A.; King, D.K.; Ritzwoller, D.P.; Ritzwoller, D.P.; Shetterly, S.M.; Bender, B.G. Transition to Virtual Asthma Care During the COVID-19 Pandemic: An Observational Study. J. Allergy Clin. Immunol. Pract. 2022, 10, 1569. [Google Scholar] [CrossRef]
- Hartman, M.; Mináriková, J.; Batalik, L.; Pepera, G.; Formiga, M.F.; Cahalin, L.; Dosbaba, F. Effects of Home-Based Training with internet Telehealth Guidance in COPD Patients Entering Pulmonary Rehabilitation: A Systematic Review. Int. J. Chronic Obstr. Pulm. Dis. 2023, 18, 2305–2319. [Google Scholar] [CrossRef]
- Koh, J.H.; Chong, L.C.Y.; Koh, G.C.H.; Tyagi, S. Telemedical Interventions for Chronic Obstructive Pulmonary Disease Management: Umbrella Review. J. Med. Res. 2023, 25, e33185. [Google Scholar] [CrossRef] [PubMed]
- Sousa-Pinto, B.; Louis, R.; Anto, J.M.; Amaral, R.; Sá-Sousa, A.; Czarlewski, W.; Brussino, L.; Canonica, G.; Loureiro, C.C.; Cruz, A.; et al. Adherence to inhaled corticosteroids and long-acting β2-agonists in asthma: A MASK-air study. Pulmonology 2025, 31, 2416869. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Li, G.; Tian, L.; Guo, Q.; Pan, X. Short-term exposure to air pollution and morbidity of COPD and asthma in East Asian area: A systematic review and meta-analysis. Environ. Res. 2016, 148, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Li, Q.; Kaufman, J.S.; Wang, J.; Copes, R.; Su, Y.; Benmarhnia, T. Effect of air quality alerts on human health: A regression discontinuity analysis in Toronto, Canada. Lancet Planet Health. 2018, 2, e19–e26. [Google Scholar] [CrossRef]
- Byrwa-Hill, B.M.; Presto, A.A.; Wenzel, S.; Fabisiak, J.P. Impact of a pollution breach at a coke oven factory on asthma control in nearby vulnerable adults. J. Allergy Clin. Immunol. 2021, 148, 225–233. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- American Academy of Pediatrics. Air Pollution: Improving Knowledge and Awareness Project Year 2025; American Academy of Pediatrics: Elk Grove Village, IL, USA, 2025; Available online: https://www.aap.org/en/advocacy/community-health-and-advocacy/community-pediatrics-funded-projects/air-pollution-improving-knowledge-and-awareness/ (accessed on 11 September 2025).
- Chakraborty, J.; Maantay, J.A.; Brender, J.D. Disproportionate proximity to environmental health hazards: Methods, models, and measurement. Am. J. Public Health 2011, 101 (Suppl. 1), S27–S36. [Google Scholar] [CrossRef]
- Byrwa-Hill, B.M.; Morphew, T.L.; Presto, A.A.; Fabisiak, J.P.; Wenzel, S.E. Living in environmental justice areas worsens asthma severity and control: Differential interactions with disease duration, age at onset, and pollution. J. Allergy Clin. Immunol. 2023, 152, 1321–1329.e5. [Google Scholar] [CrossRef]
- Patel, M.M.; Chillrud, S.N.; Correa, J.C.; Hazi, Y.; Feinberg, M.; Deepti, K.; Prakash, S.; Ross, J.M.; Levy, D.; Kinney, P.L. Traffic-Related Particulate Matter and Acute Respiratory Symptoms among New York City Area Adolescents. Environ. Health Perspect. 2010, 118, 1338. [Google Scholar] [CrossRef]
- U.S. Census Bureau QuickFacts: Pittsburgh City, Pennsylvania. Available online: https://www.census.gov/quickfacts/fact/table/pittsburghcitypennsylvania/ (accessed on 22 April 2025).
- U.S. Environmental Protection Agency. Technical Assistance Document for the Reporting of Daily Air Quality — the Air Quality Index (AQI); (EPA 454/B-18-007); 2018. Available online: https://cfpub.epa.gov/ols/catalog/advanced_full_record.cfm?&FIELD1=SUBJECT&INPUT1=Indexes&a... (accessed on 22 September 2025).
- Posit Team (Formerly RStudio Team). RStudio: Integrated Development Environment for R. Version 2025.05.0+496 “Mariposa Orchid” (f0b76cc00df96fe7f0ee687d4bed0423bc3de1f8, Released 2025-05-04); Posit Software, PBC: Boston, MA, USA, 2025. [Google Scholar]

| Overall | Age Group: | |||
|---|---|---|---|---|
| <18 Years | 18–64 Years | ≥65 Years | ||
| N = 117,545 | N = 23,050 | N = 70,280 | N = 24,215 | |
| Sex: | ||||
| Male | 55,531 (47.2%) | 11,836 (51.3%) | 33,502 (47.7%) | 10,193 (42.1%) |
| Female | 62,014 (52.8%) | 11,214 (48.7%) | 36,778 (52.3%) | 14,022 (57.9%) |
| Insurance: | ||||
| Public | 53,151 (45.2%) | 11,212 (48.6%) | 18,711 (26.6%) | 23,592 (97.4%) |
| Private | 64,394 (54.8%) | 11,838 (51.4%) | 51,569 (73.4%) | 623 (2.6%) |
| Overall | Air Quality Index (790 Days) | ||||
|---|---|---|---|---|---|
| Mean (SD) | Median [IQR] | Good (AQI < 50) | Moderate (AQI 50–100) | Unhealthy (AQI >100) | |
| AQI: | #Days (%) | #Days (%) | #Days (%) | ||
| Overall | 53.1 (23.2) | 48.8 [36.5, 64.1] | 416 (52.7%) | 337 (42.7%) | 37 (4.7%) |
| Ozone | 34.7 (16.5) | 32.4 [24.1, 41.7] | 686 (90.1%) | 69 (9.1%) | 6 (0.8%) |
| PM2.5 | 48.1 (22.8) | 45.8 [30.8, 61.0] | 443 (56.1%) | 330 (41.8%) | 17 (2.2%) |
| SO2 | 23.6 (24.6) | 15.7 [4.3, 34.3] | 693 (87.7%) | 80 (10.1%) | 17 (2.2%) |
| NO2 | 18.8 (7.5) | 17.8 [13.4, 23.6] | 790 (100%) | ---- | ---- |
| Mean (SD) | Mean (SD) | Mean (SD) | |||
| Max Temp (F) | 60.1 (19.8) | 61.0 [42.0, 79.0] | 55.1 (19.1) | 66.1 (19.3) | 66.1 (19.3) * |
| Wind Speed (mph) | 16.7 (6.8) | 16.0 [11.5, 21.0] | 17.9 (7.03) | 15.1 (6.2) | 17.6 (6.6) * |
| RR Comparing AQI (>100 vs. ≤100) | Daily Exacerbation Rate Ratios (95% CI) | ||
|---|---|---|---|
| Asthma | Bronchitis | COPD | |
| AQI Overall | RR (95% CI) | RR (95% CI) | RR (95% CI) |
| LAG0 | 1.42 (1.05, 1.93) * | 1.01 (0.65, 1.58) | 0.95 (0.66, 1.36) |
| LAG1 | 0.79 (0.54, 1.17) | 0.93 (0.59, 1.47) | 0.95 (0.67, 1.36) |
| LAG5 | 1.04 (0.73, 1.47) | 1.11 (0.72, 1.70) | 1.17 (0.84, 1.62) |
| meanLAG0–5 a | 0.78 (0.35, 1.74) | 0.83 (0.31, 2.22) | 1.27 (0.68, 2.36) |
| AQI_PM2.5 b | |||
| LAG0 | 1.60 (1.06, 2.43) * | 0.77 (0.36, 1.62) | 0.93 (0.55, 1.58) |
| LAG1 | 0.96 (0.57, 1.63) | 0.99 (0.51, 1.91) | 0.86 (0.50, 1.50) |
| LAG5 | 0.89 (0.51, 1.54) | 0.76 (0.36, 1.60) | 1.41 (0.91, 2.17) |
| AQI_SO2 b | |||
| LAG0 | 1.60 (1.06, 2.43) * | 1.33 (0.75, 2.36) | 1.14 (0.70, 1.84) |
| LAG1 | 0.68 (0.37, 1.28) | 1.10 (0.59, 2.06) | 1.21 (0.76, 1.93) |
| LAG5 | 1.24 (0.78, 1.98) | 1.76 (1.08, 2.93) * | 0.93 (0.55, 1.58) |
| Asthma Exacerbation Rate Comparing AQI_ LAG0 > 100 vs. ≤100: | ||||
|---|---|---|---|---|
| AQI Overall RR (95% CI) | AQI Ozone RR (95% CI) | AQI PM2.5 RR (95% CI) | AQI SO2 RR (95% CI) | |
| Stratum: | ||||
| Overall | 1.42 (1.05, 1.93) * | 1.73 (0.56, 5.37) | 1.60 (1.06, 2.43) * | 1.60 (1.06, 2.43) * |
| Age < 18 years | 2.32 (1.16, 4.62) * | 1.50 (0.21, 10.76) | 2.17 (0.79,5.90) | 3.33 (1.45, 7.62) * |
| Sex: | ||||
| Male | 1.85 (0.67, 5.15) | ---- | 3.03 (0.94, 9.75) | 1.98 (0.48, 8.14) |
| Female | 2.91 (1.14, 7.42) * | 3.40 (0.50, 24.79) | 1.17 (0.16, 8.49) | 5.05 (1.80, 14.19) * |
| Insurance: | ||||
| Public | 2.47 (1.18, 5.14) * | 1.80 (0.25, 12.94) | 1.92 (0.61, 6.10) | 4.01 (1.74, 9.24) * |
| Private a | 1.57 (0.21, 11.97) | ---- | ---- | ---- |
| Age 18–64 years | 1.45 (1.02, 2.06) * | 0.52 (0.13, 2.10) | 1.71 (1.07, 2.74) * | 1.51 (0.92, 2.49) |
| Sex: | ||||
| Male | 1.61 (0.92, 2.84) | ---- | 1.87 (0.88, 3.99) | 2.15 (1.06, 4.37) * |
| Female | 1.36 (0.86, 2.13) | 0.81 (0.20, 3.26) | 1.62 (0.89, 2.95) | 1.17 (0.58, 2.35) |
| Insurance: | ||||
| Public | 1.44 (0.90, 2.29) | 0.93 (0.23, 3.72) | 1.64 (0.87, 3.07) | 1.30 (0.64, 2.62) |
| Private | 1.46 (0.85, 2.51) | ---- | 1.81 (0.89, 3.67) | 1.81 (0.89, 3.67) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Byrwa-Hill, B.M.; Morphew, T.; O’Neill, J.; Gentile, D. Air Quality Index as a Predictor of Respiratory Morbidity in At-Risk Populations. Int. J. Environ. Res. Public Health 2025, 22, 1493. https://doi.org/10.3390/ijerph22101493
Byrwa-Hill BM, Morphew T, O’Neill J, Gentile D. Air Quality Index as a Predictor of Respiratory Morbidity in At-Risk Populations. International Journal of Environmental Research and Public Health. 2025; 22(10):1493. https://doi.org/10.3390/ijerph22101493
Chicago/Turabian StyleByrwa-Hill, Brandy M., Tricia Morphew, John O’Neill, and Deborah Gentile. 2025. "Air Quality Index as a Predictor of Respiratory Morbidity in At-Risk Populations" International Journal of Environmental Research and Public Health 22, no. 10: 1493. https://doi.org/10.3390/ijerph22101493
APA StyleByrwa-Hill, B. M., Morphew, T., O’Neill, J., & Gentile, D. (2025). Air Quality Index as a Predictor of Respiratory Morbidity in At-Risk Populations. International Journal of Environmental Research and Public Health, 22(10), 1493. https://doi.org/10.3390/ijerph22101493






