Abstract
Given the increasing integration of trusted leaders in public health science, including vaccination programs, context-specific understandings of community perceptions and levels of trust are critical to intervention. This study aimed to understand the perspectives and attitudes of the southeastern Louisiana community and inform the development of a community-engaged action plan. A cross-sectional survey of 555 southeastern Louisianans—including faith-based organization (FBO) members, community pharmacy (CommRx) customers, community-based organization (CBO) contacts, and Louisiana community-dwelling residents—was conducted from November 2020 to March 2021. Multivariable logistic regression was used to explore factors associated with COVID-19 vaccination likelihood. Of the participants, 89.9% were Black and 56.9% were women (mean age = 53.3 years). Doctors/healthcare providers (HCPs) were the most trusted COVID-19 information sources. Vaccination likelihood was associated with increasing age (odds ratio (OR) = 1.47; 95% confidence interval (CI): 1.27–1.72), trust in doctors/HCPs (OR = 2.83; 95% CI: 1.64–4.88), trust in government (OR = 4.26; 95% CI: 2.44–7.43), and motivations to keep one’s community safe (OR = 1.52; 95% CI: 1.36–1.70). CommRx customers (OR = 1.93; 95% CI: 1.02–3.65) and CBO contacts (OR = 2.57; 95% CI: 1.37–4.83) were more likely to receive a COVID-19 vaccine than FBO members. Engaging underserved communities and trusted stakeholders through collaborative Community–Academic—Public health—Practice (CAPP) partnerships such as the Louisiana Community Engagement Alliance can promote health and wellness and optimize health interventions.
1. Introduction
Widespread misinformation and disinformation during the COVID-19 pandemic highlighted the need for improved access to quality public health messaging delivered by trusted voices, particularly among underserved communities hardest hit by the disease [1,2]. COVID-19 vaccine acceptance varies globally and is influenced by several factors, including trust in healthcare providers and public health infrastructure [3]. Trusted messengers are individuals with longstanding, personal relationships and roots in communities, and often include personal healthcare providers (HCPs), pharmacists, and faith leaders, who can play a crucial role in increasing vaccine confidence [4,5]. However, despite being recognized as an integral link between social determinants of health (SDoH) and health outcomes due to their central role in promoting community health and wellness [5,6], trusted leaders often remain an ill-equipped and under-supported community resource for addressing vaccine hesitancy.
Recently, community–academic partnerships have gained traction as an opportunity to harness the potential of trusted community leaders [7,8,9,10]. Calls for meaningful partnerships between academic institutions, HCPs, and trusted community stakeholders have been issued as a means to reducing hesitancy, increasing vaccine confidence and acceptance, and building trust at all stages, from vaccine development to dissemination [10,11]. Yet, vaccine uptake remains context-specific, and variations in communities as well as socio-cultural determinants necessitate a nuanced approach to public health intervention, as demonstrated in previous studies that highlight how factors such as local beliefs, trust in government, and perceived vaccine safety significantly influenced COVID-19 vaccine decisions and acceptance/hesitancy [4,12,13]. Considering global trends in vaccine hesitancy and acceptance [3], the increasing integration of trusted leaders in public health science, including vaccination programs and health messaging, in addition to establishing a localized understanding of community perceptions and levels of trust, is critical to informing the evolving role of trusted leaders in their respective contexts [14].
The Louisiana Community Engagement Alliance (LA-CEAL) Community—Academic—Public health—Practice (CAPP) partnership was formed in November of 2020 to understand the disproportionate impact of COVID-19 on Black Louisianans and respond to community concerns about COVID-19 prevention and treatment strategies. Building on existing trusted partnerships with multiple stakeholders, including faith-based organizations (FBOs), community-based organizations (CBOs), federally qualified health centers (FQHCs), and community pharmacies (CommRx), the LA-CEAL CAPP partnership aimed to develop and execute a rapid community-engaged action plan to support COVID-19 vaccine acceptance among faith leaders, CBOs, and local pharmacists who were on the front lines in their communities, responding to the crisis and building awareness and public trust in the safety and efficacy of COVID-19 vaccines.
Via the LA-CEAL CAPP, we aimed to better appreciate the diverse perspectives and attitudes of the southeastern Louisiana community and inform the design and execution of a community-engaged action plan. To do so, this study examined trusted sources of information, COVID-19 preventive behavior engagement, motivations, likelihood of vaccination, and overall sentiment toward vaccination among a broad sample of southeastern Louisiana community groups, including FBO members, CommRx customers, CBOs contacts, and residents of Louisiana communities. Results and lessons learned regarding COVID-19 vaccination likelihood among patients receiving care in Louisiana FQHCs have been previously reported [15].
2. Methods
2.1. Target Population and Sampling
Given the disproportionate death and disease burden of COVID-19 among Black communities in Louisiana [16], the study was designed to oversample African American community residents. Using non-probability convenience sampling methods, 555 adult (i.e., ≥18 years of age) participants were recruited from CommRx customers, members of partner FBOs, individuals identified via CBO contacts, and residents of Louisiana neighborhoods. The analytic sample included 527 survey respondents with complete (i.e., non-missing) data on key variables of interest.
2.2. Survey Instrument and Data Collection
The survey was developed in coordination with national CEAL leadership and statewide CEAL team leaders via an iterative process that aimed to ensure the inclusion of key themes (e.g., knowledge, attitudes, beliefs, perceived risks and benefits, barriers and facilitators, trust in research(ers), SDoH, information seeking, and other behaviors) underlying COVID-19 research participation and the uptake of COVID-19 preventive strategies. Surveys were completed in person and at community sites, with direct data entry into study tablets or computers via the REDCap (Research Electronic Data Capture) platform. Trained study personnel and research assistants facilitated the self-administration or interviewer-assisted administration of surveys, according to participant preferences. All participants provided verbal informed consent. Study procedures were approved by the Tulane University Institutional Review Board and completed in accordance with institutional guidelines.
2.3. Study Measures
Socio-demographics (e.g., age, sex, race, education, income, and employment status) were self-reported. Age was estimated from the month and year of birth, with participants assigned a value of ‘1’ as the day of birth, and rescaled by dividing the original scale by 10 years. Participants were asked to self-report race using predefined categories (i.e., White, Black or African American, Asian, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, Other [please specify], or prefer not to answer). Those who selected “prefer not to answer” were classified as unknown. The “Other races” category included those who identified as “Asian”, “American Indian or Alaska Native”, “Native Hawaiian or other Pacific Islander”, “Other [please specify]”, and those who selected more than one race category. Educational attainment and employment status were collected via a single question. Annual household income was categorized as <USD 25,000, ≥USD 25,000, and unknown (i.e., for those who preferred not to answer this question).
Healthcare access and health literacy were also captured. Healthcare access was defined as having seen an HCP in the past 12 months, while low health literacy was defined as needing someone to help you read written information from your doctor or drug store, “sometimes”, “often”, or “always”. COVID-19-related SDoH were measured using questions asking about challenges faced by participants due to COVID-19 in obtaining needed healthcare (including mental health), having a place to live, having enough food to eat, having clean water to drink, obtaining needed medicine, and getting to where they needed to go. Each challenge was rated as “No, this is not a challenge”, “Yes, this is a minor challenge”, or “Yes, this is a major challenge”. Responses were dichotomized as major/minor challenge vs. not a challenge and summed to indicate the number of challenges experienced by participants (range 0–6).
To assess attitudes, motivations, and trust in COVID-19 messaging and behavioral recommendations, additional questions explored engagement in COVID-19 preventive behaviors, motivations to vaccinate, and trusted sources of COVID-19 information. Three preventive behaviors (i.e., wearing a face covering or mask, washing hands with soap or using hand sanitizer several times daily, and staying at least 6 feet away from others) were examined by asking about engagement in each practice in the past seven days. Engagement in preventive behaviors was positively coded if participants noted engaging in each of the three practices “very often” or “all of the time”. Reasons to receive the COVID-19 vaccine were grouped together, and summed scores were used to describe participant motivations to receive the COVID-19 vaccine. Those motivated by a concern for community safety and return to normalcy included respondents who answered yes to any of 6 items concerning wanting to keep family safe, wanting to keep community safe, wanting to keep one’s self safe, wanting to feel safe around others, not wanting to get really sick from COVID-19, and a belief that life will not go back to normal until most people receive a COVID-19 vaccine (Cronbach’s alpha = 0.9). Those motivated by health concerns/HCP’s advice included respondents who answered yes to having chronic health problems (e.g., asthma, diabetes) or having received a doctor’s recommendation to receive a COVID-19 vaccine (Cronbach’s alpha = 0.6). Higher scores indicated stronger motivation. Finally, trusted sources of information about COVID-19 included doctors/HCPs, faith leaders, family/close friends, work-/classmates, traditional news media, social media contacts, the U.S. government, the U.S. Coronavirus Task Force, the Louisiana state government, and local city/town government. Each item was measured on a 3-point Likert scale and dichotomized as “a great deal” versus “a little”, “not at all”, or “not applicable”.
The primary outcome measure was captured using a 7-point scale ranging from 1 (not at all likely) to 7 (very likely) in response to the question “How likely are you to get an approved COVID-19 vaccine when it becomes available?”
2.4. Statistical Plan
Descriptive statistics were used to describe the characteristics of the study sample. Means and standard deviations were computed for the continuous measures and frequency distributions obtained for categorical measures. The net promoter score (NPS)—a commonly used indicator of an individual’s experience that examines likelihood of service recommendation [17,18]—was derived using the 7-point Likert scale to gauge the likelihood of getting vaccinated. The NPS was calculated by subtracting the percentage with a score of 6 or 7 (considered “promoters”) from the percentage with scores between 1 and 3 (considered “detractors”). Those with a score of 4 or 5 were considered “passives” and were not included in the NPS calculation. NPSs range from −100 to +100. A score of −100 means all respondents are “detractors”, while a score of +100 indicates that every respondent is a “promoter”. The final outcome assessed likelihood of vaccination and was defined as a binary measure based on those with an NPS of 6 or 7. Stepwise logistic regression with backward elimination was performed to determine factors associated with vaccination likelihood, with a significance level of 0.10 set for removal from the model. All analyses were performed using Stata/SE 15.1.
3. Results
3.1. Sample Characteristics
The sample distribution included 47.3% FBO members, 19.2% CommRx customers, 15.8% Louisiana neighborhood residents, and 17.8% CBO contacts. Participants were predominantly of Black race (89.9%) with a mean age of 53.3 years (Table 1). The majority of the sample had a high school education or less (60.3%), and just over a third (34.5%) were employed either part-time or full-time. Nearly half of the sample (48.6%) reported an annual household income of less than USD 25,000. Regarding SDoH, 87.9% had seen an HCP in the past 12 months and few (14.2%) had low health literacy. Half of the sample (49.7%) reported not having any COVID-19-related challenges; among those affected by COVID-19 SDoH, obtaining needed healthcare (30.9%), getting where they needed to go (26.2%) and having enough food to eat (26.0%) were most often reported.

Table 1.
Participant characteristics including social determinants of health and COVID-19 prevention behaviors.
There were statistically significant differences across the four sampling groups in all characteristics except age, insurance ownership, and mean number of COVID-19-related challenges. Compared to FBO members, CBO contacts were less likely to be women (59.4% vs. 40.4%, p = 0.001). There were significantly fewer respondents of Black race among the neighborhood residents compared to the FBO member subsample (74.7% vs. 92.4%, p < 0.001). A greater proportion of CBO contacts reported an annual household income of less than USD 25,000 compared to their FBO counterparts (73.4% vs. 37.8%, p < 0.001). Low health literacy was more common among CommRx clients (26.7%) and CBO contacts (19.2%) compared to FBO members (8.8%, p < 0.001).
3.2. Attitudes Towards COVID-19 Messaging and Trusted Sources of Information
Compliance with each of the recommended COVID-19 preventive measures (face covering, hand washing, and social distancing) was high among sample respondents, ranging from 91.8 to 97.0%. Engagement in all three preventive behaviors was significantly lower among neighborhood residents compared with FBO members (75.9% vs. 89.6%, p = 0.007).
Across all groups, doctors/HCPs were the most trusted sources of information on COVID-19 (Figure 1). Other top trusted sources of information included faith leaders, family/close friends, and the U.S. Coronavirus Task Force. Social media contacts were least trusted across all groups.
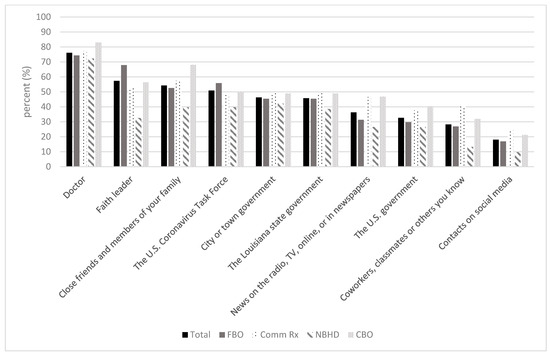
Figure 1.
Trusted sources of COVID-19 information.
3.3. Likelihood of COVID-19 Vaccination
Regarding likelihood of vaccination, the sample included 60.3% “promoters” compared to 25.8% “detractors”, giving a positive NPS of 34.5% and suggesting that respondents were likely to receive the COVID-19 vaccine when available (Table 2). Notably, the NPS varied across groups and was highest among the CommRx subsample (NPS = 44.6%), followed by the FBO (NPS = 33.7%), CBO (NPS = 31.9%), and neighborhood (NPS = 27.7%) subgroups.

Table 2.
Likelihood of vaccination using NPS (n = 527).
Increasing age (odds ratio (OR) = 1.47; 95% confidence interval (CI): 1.27–1.72), trust in doctors/HCPs (OR = 2.83; 95% CI: 1.64–4.88), trust in government (OR = 4.26; 95% CI: 2.44–7.43), and the motivation to keep one’s community safe (OR = 1.52; 95% CI: 1.36–1.70) had higher odds of likelihood of vaccination (Table 3). In addition, CommRx customers (OR = 1.93; 95% CI: 1.02–3.65) and CBO contacts (OR = 2.57; 95% CI: 1.37–4.83) had significantly higher odds of likelihood of receiving a COVID-19 vaccine when available compared to FBO members.

Table 3.
Factors associated with likelihood of COVID-19 vaccination.
4. Discussion
The analysis of participant data revealed varied perceptions of trusted messaging, vaccination motivations, and vaccination likelihoods among the four sampling groups. Likelihood of vaccination was dependent upon age, sampling group, trust in sources of information, and a general concern for community wellbeing, safety, and return to normalcy. These findings resonate with published evidence that vaccine likelihood at the outset of a pandemic is multifaceted and context-dependent, including correlations to SDoH and related inequities, structural racism, mistrust, and exposure to (mis)information [2,4,13,19]. In our sample, the strongest associations with vaccination likelihood were having a great deal of trust in one’s doctor/HCP, having a great deal of trust in the U.S. government, and being a CommRx customer or CBO contact (compared to an FBO member).
Trust, particularly trust in government vaccine approval/development processes, is a key factor underlying vaccine hesitancy [20]. Notably, despite the legacy of mistrust of government, research, and healthcare institutions among underserved communities [21], some studies have noted that Black adults are more likely than non-Hispanic White and Hispanic/Latina/o/x adults to consider federal agencies (i.e., CDC, FDA), local or state governments (e.g., departments of health), and/or public health officials credible or trustworthy information sources [4]. In our study, despite the U.S. government being ranked among the lowest trusted sources of COVID-19 information (seventh out of ten listed sources), high trust in the government was associated with being very likely to get vaccinated. Research among FQHC patients in Louisiana similarly revealed trust in doctors/HCPs and government sources of COVID-19 information to have the strongest and most consistent associations with COVID-19 vaccination likelihood [15]. These findings support the need for honest, consistent, high-quality public health messaging to build trust and confidence in vaccines. The early politicization of the pandemic [22,23], coupled with an onslaught of misinformation, disinformation, anti-vax groups, and conspiracy theories [1,13,24], likely fueled vaccine hesitancy and skepticism—a special concern and public health priority among communities with low institutional trust and low vaccination coverage rates [5]. Our findings align with the potential utility of a collective, robust communication infrastructure and multimodal approach using trusted, informed community messengers (e.g., HCPs, non-governmental entities, influential public figures, and religious communities) and different communication channels (e.g., community outreach and forums, traditional media, electronic outreach, direct conversations) to address reluctance and build confidence in vaccines [1,4,5,25].
Top trusted sources of COVID-19 information among the study population were doctors/HCPs, faith leaders, close friends/family members, and the U.S. Coronavirus Task Force, respectively. A recent systematic review similarly noted personal physicians as the most often mentioned type of trusted messenger, followed by one’s social network (e.g., friends, family, peers, neighbors), church and faith leaders, and local and/or state government officials [4]. The review further described other healthcare professionals (e.g., pharmacists), community leaders, and CBOs as particularly credible and trustworthy information sources among African Americans, with the added benefit of providing access to care and vaccine services [4]. Indeed, CBOs and FBOs were informal COVID-19 information dissemination sites in Louisiana throughout the pandemic, and community members would initiate conversations with trusted community voices and continue to seek reinforcement of this messaging from HCPs. Study findings thus further reinforce the need for a collective response to vaccine hesitancy, illustrating how healthcare professionals (e.g., doctors, nurse practitioners, pharmacists), FBOs, and CBOs, working in collaboration with science-based entities and connected to needed public health and clinical resources, can be a positive conduit for improved public health. Local CBOs understand the social and cultural dynamics essential to building mutually beneficial opportunities for community participation and outreach [2,9]. Ministries and FBOs are spiritual community assets that can help to meet community-wide needs while shepherding local communities in a health-promotion direction [26,27,28]. Doctors/HCPs are among the top trusted sources in their communities for health information and care [4], while pharmacists, given their strategic locations and flexible hours, are uniquely positioned for community response and engagement [5]. Ultimately, the LA-CEAL CAPP provided a collaborative entry point for all stakeholders to access vulnerable populations and share in the communication of COVID-19 information in ways most relevant to their own mission and most helpful to the missions of other collaborating groups (e.g., government, clinics, physicians, and community pharmacies).
Yet, beyond the trust and compliance of the general population, the success of public health interventions is reliant on multiple factors, including the effectiveness of communication methods and features of messaging, such as the content, style, and framing [4,25]. Possibly, due to messaging from their most trusted sources, more than 90% of surveyed participants were practicing COVID-19 prevention strategies. In addition, concern for community safety and return to normalcy were among the strongest factors associated with the likelihood of COVID-19 vaccination. These study findings suggest a sense of community and responsibility, and may also reflect a value for positive, hopeful messaging, as opposed to fear-based appeals, among this population. Indeed, evidence suggests that persuasive messaging using community-focused or collective action appeals (i.e., about protecting family members, including children and the elderly, as well as the “social other”) may resonate more strongly among African American communities than individual (i.e., self-focused) messaging to elicit a sense of unity and changes in behavior [4].
Strengths and Limitations
These results should be considered in the context of the study’s limitations, including the unprecedented nature of the COVID-19 pandemic and the timing of the study. The study was launched in an effort to understand and respond to a trend of overwhelming devastation and potential vaccine uptake disparity among vulnerable communities and Black Louisianans. A significant strength of the study was the formation of LA-CEAL, and the collective impact of the community, academic, public health, and clinical practice entities involved. However, this study began early in the pandemic during the initial roll out of the COVID-19 vaccines, following months of exposure to COVID-19 messaging and the likely formation and setting of community members’ opinions. As a result, community perceptions, behaviors, and trust in health interventions may have shifted over time, and not be fully captured in this study’s findings. This study affirmed that community members rely on their FBOs, CBOs, CommRx, and HCPs to access healthcare and treatment options, and to understand the pandemic’s ever-changing messaging. In turn, the results also showed that social factors such as age, experience with messenger sources, and trust may influence behaviors, engagement, and decision-making. However, this study did not fully account for the influence of varying and sometimes conflicting media messaging on community beliefs and attitudes toward COVID-19. A deeper analysis of the media’s role in shaping community perceptions could provide insights into how different information sources influenced behavior during this period. Yet, the convenience sample reflects the perspectives, attitudes, and behaviors of a predominantly Black, adult population in southeast Louisiana, and the results may not be generalizable to community contexts outside of this race and region.
5. Conclusions
COVID-19 challenged the traditional silos of systems and institutions in the U.S., necessitating collaboration and the removal of barriers for the sake of community health, safety, and prosperity. The LA-CEAL CAPP partnership worked together to address COVID-19 vaccine-related disparities within vulnerable Louisiana communities, specifically among Black individuals, via the development of culturally tailored community education and outreach programs. The collective engagement of academic institutions, FBOs, CBOs, CommRx, government stakeholders, HCPs, and front-line workers in communities where systemic injustice has historically prevailed was an opportunity to demonstrate that sustainable, authentic, and collaborative CAPP partnerships are integral parts of public health and can be established via intentional, stepwise engagement with underserved communities and trusted community stakeholders [21,29].
Author Contributions
Conceptualization, L.W. and L.S.C.; Methodology, L.W., L.S.C., E.P., M.K.-W. and D.S.; Investigation, L.W. and L.S.C.; Resources, L.W. and L.S.C.; Data curation, L.W., L.S.C., E.P., M.K.-W. and D.S.; Writing—original draft, L.W., L.S.C. and D.S.; Writing—review & editing, L.W., L.S.C., E.P., T.F., S.A.-D., F.H., C.G., B.S., K.T., M.W., G.D., M.V., C.S., L.F., K.C., M.K.-W. and D.S.; Visualization, L.W. and D.S.; Project administration, L.W., M.K.-W., E.P. and D.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was, in part, funded by the National Institutes of Health (NIH) Agreement OT2HL158287. The authors also received funding from the NIMHD, which funds the Center for Minority Health and Health Disparities Research and Education 5S21MD0000100-12 (Williams) and the Research Centers in Minority Institutions (RCMI) Center for Cancer and Health Disparities 5U54MD007595-17 (Williams), the National Institute of General Medical Sciences of the NIH, which funds the Louisiana Clinical and Translational Sciences Center (U54 GM10490; Williams, Krousel-Wood), and from U54 TR001368 (Krousel-Wood) and R33 AG068481 (Krousel-Wood, Peacock). S. Al-Dahir receives funding support from Genentech-Roche Program P-05302 and Pfizer (grant 75035725) for work not related to the Louisiana Community Engagement Alliance.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Tulane University (protocol code 2020-1600 and date of approval 10-23-2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article.
Acknowledgments
We are grateful to our study participants, Tulane and Xavier staff and administrators supporting the LA-CEAL CAPP partnership, LA-CEAL Community Advisory Board members, Tulane and Xavier students assisting with data collection, and all individuals supporting the CEAL Initiative. We also extend special thanks to our FBO, CommRx, and CBO partners and liaisons: Baptist Community Ministries (BCM), Bethel Lutheran Church, Blessed Trinity Parish, Calvary Missionary Baptist Church, Cathedral of Prayer and Deliverance, Catholic Archdiocese of New Orleans and Baton Rouge, Cummings Wilson AME, Faith Full Gospel Baptist Church, Faith Presbyterian Church, Grace and Glory, Greater Living Witness Sanctuary, Hispanic Apostolate, Holy Cross Lutheran Church, Israelite Baptist Church, King’s Children Full Gospel Fellowship, Masjid Rahim Mosque, Mt. Carmel Baptist Church, New Covenant Faith Church, New St. John Missionary Baptist Association, New St. Mark, Next Level Church, Pentecost Baptist Church, Pure Light Baptist Church, Prayer House Ministry, Second Free Mission Baptist Church, St. Augustine, St. Joseph the Worker Catholic Church Health Ministry, St. Peter Claver, Starlight Missionary Baptist Church, True Love Missionary Baptist Church, United Fellowship, The Way Jesus Christ Christian Church, and Westbank United 7th Day Adventist; St. Bernard Drugs, Best Life Pharmacy and Wellness, Crescent City Pharmacy, and C&S Family Pharmacy.
Conflicts of Interest
M.V. is an employer of St. Bernard Drugs, C.S. is an employer of Best Life Pharmacy, L.F. is an employer of Crescent City Pharmacy, F.H. is an employer of Baptist Community Ministries, and K.C. is an employer of C & S Family Pharmacy. M. K-W. is a member of the United States Preventive Services Task Force (USPSTF). This article does not necessarily represent the views and policies of the USPSTF. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The views and conclusions contained in this document are those of the authors and should not be interpreted as representing the official policies, either expressed or implied, of the NIH.
References
- Grewal, M.; Chow, E.J. Trust by Proxy. Cureus 2023, 15, e49130. [Google Scholar] [CrossRef] [PubMed]
- Wiley, Z.; Khalil, L.; Lewis, K.; Lee, M.; Leary, M.; Cantos, V.D.; Ofotokun, I.; Rouphael, N.; Rebolledo, P.A. A Framework for Inspiring COVID-19 Vaccine Confidence in African American and Latino Communities. Vaccines 2022, 10, 1319. [Google Scholar] [CrossRef] [PubMed]
- Hassan, W.; Kazmi, S.K.; Tahir, M.J.; Ullah, I.; Royan, H.A.; Fahriani, M.; Nainu, F.; Rosa, S.G.V. Global acceptance and hesitancy of COVID-19 vaccination: A narrative review. Narra J. 2021, 1, e57. [Google Scholar] [CrossRef] [PubMed]
- Rabin, Y.; Kohler, R.E. COVID-19 Vaccination Messengers, Communication Channels, and Messages Trusted Among Black Communities in the USA: A Review. J. Racial Ethn. Health Disparities 2023. [Google Scholar] [CrossRef]
- Shen, A.K.; Tan, A.S.L. Trust, influence, and community: Why pharmacists and pharmacies are central for addressing vaccine hesitancy. J. Am. Pharm. Assoc. 2022, 62, 305–308. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.A.R.; Saint Onge, J.M.; Gurley-Calvez, T.; Anderson, R.; Mosley, J.; Brooks, J.V. Aligning research and practice: The role of academic-community partnerships for improving measurement and process. Eval. Program. Plann 2021, 89, 101990. [Google Scholar] [CrossRef]
- Hippalgaonkar, N.; Nguyen, R.H.; Cohn, E.B.; Horowitz, J.; Waite, A.W.; Mersha, T.; Sandoval, C.; Khan, S.; Salum, K.; Thomas, P.; et al. Are We the Problem? A Call to Action for Addressing Institutional Challenges to Engaging Community Partners in Research. Int. J. Environ. Res. Public Health 2024, 21, 236. [Google Scholar] [CrossRef]
- Adams, D.R. Social Work’s Role in Collaborative Community-Academic Partnerships: How Our Past Informs Our Future. Soc. Work. 2019, 64, 19–28. [Google Scholar] [CrossRef]
- Nguyen, K.H.; Fields, J.D.; Cemballi, A.G.; Desai, R.; Gopalan, A.; Cruz, T.; Shah, A.; Akom, A.; Brown, W., 3rd; Sarkar, U.; et al. The Role of Community-Based Organizations in Improving Chronic Care for Safety-Net Populations. J. Am. Board. Fam. Med. 2021, 34, 698–708. [Google Scholar] [CrossRef] [PubMed]
- McClure, J.; Mendoza, L.; Sokol, T.; Brown, D.; LaVeist, T.; Brown, S.; Peacock, E.; Williams, L.; Mushatt, D.; Katzmarzyk, P.; et al. Advancing Health Equity: The Role of a Community-Academic-Public Health-Practice (CAPP) Partnership in Addressing COVID-19 Disparities in Louisiana. Am. J. Public Health 2024, 114, S55–S58. [Google Scholar] [CrossRef] [PubMed]
- Thompson, H.S.; Manning, M.; Mitchell, J.; Kim, S.; Harper, F.W.K.; Cresswell, S.; Johns, K.; Pal, S.; Dowe, B.; Tariq, M.; et al. Factors Associated With Racial/Ethnic Group-Based Medical Mistrust and Perspectives on COVID-19 Vaccine Trial Participation and Vaccine Uptake in the US. JAMA Netw. Open 2021, 4, e2111629. [Google Scholar] [CrossRef] [PubMed]
- Mohi, A.R.; Kusuma, I.Y.; Massi, M.N.; Bahar, M.A. Factors related to first COVID-19 booster vaccine acceptance in Indonesia: A cross-sectional multi-center study. Narra J. 2024, 4, e858. [Google Scholar] [CrossRef] [PubMed]
- Marcinowicz, L.; Fejfer-Wirbal, E.; Dudzik, A.; Genowska, A.; Terlikowski, S. Barriers and Facilitators to COVID-19 Vaccine Uptake among Polish Patients: A Qualitative Interview Study. Vaccines 2023, 11, 177. [Google Scholar] [CrossRef] [PubMed]
- Piraux, A.; Cavillon, M.; Ramond-Roquin, A.; Faure, S. Assessment of Satisfaction with Pharmacist-Administered COVID-19 Vaccinations in France: PharmaCoVax. Vaccines 2022, 10, 440. [Google Scholar] [CrossRef] [PubMed]
- Peacock, E.; Craig, L.S.; Wilson, M.; Williams, L.; Dahir, S.A.; Tang, W.; Cyprian, A.; Dery, M.; Gilliam, D.; Nguyen, D.; et al. COVID-19 vaccination likelihood among federally qualified health center patients: Lessons learned for future health crises. Am. J. Med. Sci. 2023, 366, 321–329. [Google Scholar] [CrossRef]
- Hu, G.; Hamovit, N.; Croft, K.; Roberts, J.D.; Niemeier, D. Assessing inequities underlying racial disparities of COVID-19 mortality in Louisiana parishes. Proc. Natl. Acad. Sci. USA 2022, 119, e2123533119. [Google Scholar] [CrossRef]
- Aguinis, H.; Burgi-Tian, J. Measuring performance during crises and beyond: The Performance Promoter Score. Bus. Horiz. 2021, 64, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Picazo, J.J.; Vidal-Abarca, I.; Beteta, D.; López-Ibáñez, M.; García-Vázquez, E. Impact of the COVID-19 Pandemic on the Hospital: Inpatient’s Perceived Quality in Spain. J. Patient Exp. 2021, 8, 2374373521998625. [Google Scholar] [CrossRef] [PubMed]
- Martinez Leal, I.; Njoh, J.; Chen, T.A.; Foreman-Hays, F.; Reed, B.C.; Haley, S.A.; Chavez, K.; Reitzel, L.R.; Obasi, E.M. Exploring COVID-19 Vaccine Attitudes among Racially and Ethnically Minoritized Communities: Community Partners’ and Residents’ Perspectives. Int. J. Environ. Res. Public Health 2023, 20, 3372. [Google Scholar] [CrossRef] [PubMed]
- Szilagyi, P.G.; Thomas, K.; Shah, M.D.; Vizueta, N.; Cui, Y.; Vangala, S.; Fox, C.; Kapteyn, A. The role of trust in the likelihood of receiving a COVID-19 vaccine: Results from a national survey. Prev. Med. 2021, 153, 106727. [Google Scholar] [CrossRef]
- Michener, L.; Aguilar-Gaxiola, S.; Alberti, P.M.; Castaneda, M.J.; Castrucci, B.C.; Harrison, L.M.; Hughes, L.S.; Richmond, A.; Wallerstein, N. Engaging With Communities—Lessons (Re)Learned From COVID-19. Prev. Chronic Dis. 2020, 17, E65. [Google Scholar] [CrossRef]
- Abbas, A.H. Politicizing the Pandemic: A Schemata Analysis of COVID-19 News in Two Selected Newspapers. J. Racial Ethn. Health Disparities 2022, 35, 883–902. [Google Scholar] [CrossRef]
- Lyu, J.C.; Han, E.L.; Luli, G.K. COVID-19 Vaccine-Related Discussion on Twitter: Topic Modeling and Sentiment Analysis. J. Med. Internet Res. 2021, 23, e24435. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Mukerjee, S.; Qin, H. Topics and Sentiments Influence Likes: A Study of Facebook Public Pages’ Posts About COVID-19 Vaccination. Cyberpsychol Behav. Soc. Netw. 2022, 25, 552–560. [Google Scholar] [CrossRef] [PubMed]
- Dascalu, S.; Flammer, P.G.; Ghafari, M.; Henson, S.C.; Nascimento, R.; Bonsall, M.B. Engaging Religious Institutions and Faith-Based Communities in Public Health Initiatives: A Case Study of the Romanian Orthodox Church During the COVID-19 Pandemic. Front. Public Health 2021, 9, 768091. [Google Scholar] [CrossRef]
- Levin, J. The Faith Community and the SARS-CoV-2 Outbreak: Part of the Problem or Part of the Solution? J. Relig. Health 2020, 59, 2215–2228. [Google Scholar] [CrossRef] [PubMed]
- El-Majzoub, S.; Narasiah, L.; Adrien, A.; Kaiser, D.; Rousseau, C. Negotiating Safety and Wellbeing: The Collaboration Between Faith-Based Communities and Public Health During the COVID-19 Pandemic. J. Relig. Health 2021, 60, 4564–4578. [Google Scholar] [CrossRef] [PubMed]
- Levin, J.; Idler, E.L.; VanderWeele, T.J. Faith-Based Organizations and SARS-CoV-2 Vaccination: Challenges and Recommendations. Public Health Rep. 2022, 137, 11–16. [Google Scholar] [CrossRef]
- Shaw, A.R.; Perales-Puchalt, J.; Moore, T.; Weatherspoon, P.; Robinson, M.; Hill, C.V.; Vidoni, E.D. Recruitment of Older African Americans in Alzheimer’s Disease Clinical Trials Using a Community Education Approach. J. Prev. Alzheimers Dis. 2022, 9, 672–678. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
