Abstract
Background: Postural changes are considered a public health issue and have gathered significant interest in both research and clinical practice. Aims: To evaluate the effectiveness of Global Postural Reeducation (GPR) in improving postural changes and postural stability in healthy young adults. Additionally, this study aims to identify the main postural changes in the sample population. Methods: A longitudinal study was conducted with a sample of students (n = 38) from the 2nd and 3rd years of undergraduate programs at Coimbra Health School, divided into an experimental group (EG) with 20 subjects and a control group (CG) with 18 subjects. The EG underwent a GPR intervention, while the CG received no intervention. Postural changes were assessed using a 3D motion analysis system (Qualisys), and stabilometry was evaluated using a Bertec force platform. Results: At baseline (T0), the groups were homogeneous regarding sample characterization variables, as well as postural and stabilometric variables (p > 0.05). After four weeks of the intervention (T1), no significant differences were observed between the EG and CG for any of the variables studied (p > 0.05). However, within-group analysis for the experimental group revealed a significant difference (p = 0.04) in anterior-posterior velocity, indicating a reduction in this parameter from T0 to T1. In the control group, a significant difference was observed (p = 0.03) in the left knee valgus, indicating a reduction in valgus alignment. Conclusions: GPR does not appear to be effective in improving postural changes or center of pressure displacement in healthy young students.
1. Introduction
Posture can be described as any position adopted to maintain balance with maximal stability, utilizing minimal energy and avoiding overloading anatomical structures [1]. It results from a complex neuromotor and biomechanical system and is a dynamic, continuously evolving phenomenon. Posture corresponds to a body position maintained in space for a certain period, under the continuous control of the central nervous system (CNS), aiming to provide postural alignment and balance, thereby enabling the maintenance of a stable upright position against gravity [2,3]. The importance of quantifying posture has been widely emphasized in the literature. However, despite the availability of various methods for its assessment, each is related to specific strengths and limitations [4]. Optoelectronic motion capture systems are considered the gold standard for analyzing human movement [5]. On the other hand, maintaining posture while ensuring its stability is a fundamental task of the central nervous system (CNS) [6] for carrying out daily life activities, contributing to the well-being, independence, and quality of life of an adult human being [7]. The modern lifestyle associated with inadequate postural habits can contribute to early postural changes and subsequently to musculoskeletal symptoms, increasing the relevance of studying young and healthy populations [8,9]. It is established that upright posture is not completely static, with changes observed over short intervals of time when assessed through the center of pressure (COP) [10]. Parameters derived from COP trajectories, obtained using high-precision force platforms, are considered the gold standard for evaluating postural sway [11]. Postural changes are considered to be a public health issue and have gathered significant interest in both research and clinical practice [12]. Studies have revealed a prevalence of postural deviations ranging from 22% to 65% among children and adolescents aged 6 to 17 years [13,14]. In young adults (18 to 25 years), musculoskeletal pain symptoms are more prevalent in the neck, shoulders, and lumbar region, with percentages varying between 44.3% and 60.8%, 35.2% and 40.0%, and 46.8% and 50.2%, respectively [15,16]. Lumbar hyperlordosis [17,18], pelvic anteversion [17], genu valgum [19], forward head posture [20], and cervical hyperlordosis [21] have been described as the most frequent postural deviations. In students, one of the most common musculoskeletal issues is functional postural disorders [22]. A sedentary lifestyle is identified as a significant factor in the reduction of hamstring flexibility due to the shortening of muscles, tendons, and fascia resulting from long periods spent in a seated position [23]. The flexibility of the hamstring muscles is considered one of the main muscular influences of pelvic position. The stiffness of these muscles during spinal flexion can limit anterior pelvic tilt, exacerbating muscle and ligament tension in the lumbar region. This can, in turn, generate high compressive forces on the lumbar spine, compromising the anterior trunk flexion movement, a motion commonly present in daily life activities [24].
Global Postural Reeducation (GPR) is considered an innovative method of postural correction based on solid biomechanical and physiological concepts [25]. This method distinguishes dynamic muscles, activated in a phasic way, and static activated in a tonic way [26,27], and utilizes the viscoelastic properties of muscles, which allow for permanent stretching as long as the tension caused by the stretch of antigravity muscles is maintained for as long as possible, according to Hooke’s and Newton’s models [27,28]. The therapeutic approach of GPR is based on the principles of individuality and causality, as the real cause of the problem must be identified and treated, determining that the body should be handled as a whole [27].
The therapeutic approach is based on the integrated idea that the muscular system is composed of muscle chains located anteriorly and posteriorly to the vertebral column [29,30,31], consisting of several interconnected muscles with specific functional roles [29,32], which can shorten due to musculoskeletal changes, as well as anthropometric, behavioral, and psychological factors [27,32,33,34]. Its goal is to actively stretch the shortened muscles, reduce the pressure and align the joints, placing the entire body in maximal stretch, preventing adjustments, and increasing the contraction of the antagonist muscles to avoid postural asymmetries [29,33,34]. GPR employs a unique method for evaluating and diagnosing changes in the neuromusculoskeletal system. This approach utilizes specific postures that involve the dynamic adjustment of the hip joint angle, progressing from flexion to extension. The method is characterized by movements where the hips and knees transition through various angles, including hip flexion at 90°, followed by gradual knee extensions. These postures are specifically designed to stretch shortened muscles along the inspiratory, anterior, and posterior chains. [27,35]. This method is commonly known for treating postural changes [27,36], including scoliosis, cervical straightening, and lumbar hyperlordosis, among others, with the aim of rectifying the treatment of symptoms with a biomechanical origin [29,32,33,37,38,39], as well as the treatment of movement pattern disorders resulting from neurological conditions [40]. Several studies have demonstrated its effectiveness when compared to conventional physical therapy [41] in muscle flexibility [42,43,44], postural organization [42,45], functionality [33,40], cognition, quality of life [30,40,46], and pain [30,47]. The identification of postural changes through a thorough postural assessment is fundamental for diagnosing, planning, and monitoring the development of individuals during physiotherapeutic treatment [9]. The adoption of therapeutic measures for postural reeducation can be justified not only by the fact that poor postural alignment can change load distribution and pressure on joint surfaces, contributing to joint compression and inappropriate muscle tension but also by its potential role in prevention and health promotion, thereby contributing to the quality of life of individuals. This study aimed to evaluate the effectiveness of GPR in improving postural changes and postural stability in healthy young adults. It is also intended to identify the main postural changes of the sample elements.
2. Materials and Methods
2.1. Subjects and Experimental Procedure
This study was conducted in the physiotherapy laboratory of the Coimbra Health School at the Polytechnic University of Coimbra.
A prospective longitudinal study with a non-probabilistic sampling technique was selected from a previous study [16]. A random sampling technique was employed using the website www.randomizer.org for allocation into the experimental and control groups. Two assessment time points were considered. Initial moment (T0): before the start of the intervention; and Final moment (T1): after the therapeutic intervention process (4 weeks). Participants were recruited via email and phone contact from a pre-determined list, which included individuals who had previously participated in a study [16] and were classified as having postural changes. To be eligible, participants had to be enrolled in the 2nd or 3rd year of the undergraduate programs at the Coimbra Health School and present a positive Adams test, indicating trunk asymmetry when flexing forward, along with a thoracic hump of 5 degrees or greater, measured using a scoliometer. Exclusion criteria included the presence of any known musculoskeletal, neuromuscular, or cardiorespiratory pathology or injury; pain symptoms lasting more than 3 months; moderate to severe pain (VAS pain ≥ 5.0) at the time of assessment; and failure to sign the informed consent. The final sample consisted of 38 individuals, age 19.32 ± 1.19 yr, height 167.34 ± 10.04 cm, and body mass 63.75 ± 11.83 kg of both sexes participated in this study.
The variables under study were: (i) parameters involved in the assessment of postural changes proposed by the RPG method [27], where anatomical regions of the head, shoulders, thoracic spine, lumbar spine, pelvis, knees, and heels are observed, and when marked, correspond to the shortening of muscles that make up the inspiratory, anterior, and posterior chains; (ii) Vertical alignment of the body; (iii) Anterior trunk flexion; and (iv) Stabilometry.

Table 1.
Postural Variables, Anatomical Markers, and Description of Calculation.

Table 2.
Description of the stabilometric variables, based on the studies of Oliveira et al. and Prieto et al. [54,55,56].
In the quantification of these postural changes, based on the angles and distances collected through the Qualysis system and described in Table 1, the following data were all considered normative values. For head position, a normal angle between 50° and 57° was considered [57,58,59]. A smaller angle was considered a forward head posture [48,60,61,62]. For the shoulders, the smaller the angle, the more anterior the shoulders are [48,60,63]. Angles below 52° represent rounded shoulders [59]. On the other hand, in the assessment of elevated shoulders, a positive angle indicates that the right shoulder is elevated, while a negative angle indicates the left shoulder is elevated [48]. The normal values for cervical lordosis and thoracic kyphosis range between 20° and 40° [63,64,65,66]. Lumbar lordosis is considered normal between 20° and 45° [67]. In the pelvis, the reference considers the positioning of the ASIS and PSIS in the same plane, corresponding to zero degrees [68]. However, a value of 12.26 ± 5.81° is acceptable [52]. Positive values indicate anterior pelvic tilt, while negative values correspond to posterior pelvic tilt [48]. Knee alignment corresponds to an angle of 180°. Alterations were considered for variations greater than 2.8° [69]. Angles greater than 180° correspond to varus, and angles less than 180° correspond to valgus [48]. For the calcaneus, values between 0° and 5° are considered normal [51]. Positive angles correspond to calcaneal valgus, and negative angles correspond to varus. To quantify the vertical alignment of the body, the angle defined by the intersection of the line connecting the acromion to the lateral malleolus with a vertical line was considered. An angle of 1.73 ± 0.94° was considered normal [52]. Trunk forward flexion was measured by the finger-to-floor distance, considering that the smaller the distance to the floor, the greater the spinal flexibility [70]. It is believed that the test represents the maximum length of the posterior muscle chain. Large distances between the fingers and toes, as well as increased angles at the ankle or hip, may indicate shortened muscles [71,72,73].
During data collection, participants were instructed to remain in a comfortable static position on the force platform, with their arms along the body, looking straight ahead, and with their forefeet abducted at a 30-degree angle [74]. The data collection for the standing position lasted 60 s, and participants were asked to position their upper limbs anatomically during the first 5 s. The duration of data collection for the forward trunk flexion was 30 s, and participants were asked to attempt to reach the floor with their fingers as much as possible, with their knees extended and arms and heads relaxed [75]. Data collection was performed once using ten high-speed infrared cameras from Qualisys Oqus 300, at a rate of 200 Hz, synchronized with a Bertec® FP4060 force platform (Bertec Corporation, Columbus, OH, USA) with a sampling rate of 200 Hz. The capture and synchronization of kinetic and kinematic data were conducted using the Qualisys Track Manager (QTM) software, version 2.3. A total of 81 reflective markers were placed according to the protocol of the Istituto Ortopedico Rizzoli’s (IOR) [76] and the LABIOMEP Full Body Marker setup. The anatomical markers, the calculation of the postural variables of interest, and their interpretation are described in Table 1 and Table 2.
This study received approval from the Ethics Committee of the Faculty of Sport at the University of Porto (CEFADE 17.2019) on 17 July 2019 and was conducted in accordance with the Declaration of Helsinki.
2.2. Processing and Analysis of Data
The assessment and processing of kinematic data during the postural analysis were performed using the Qualisys Track Manager v2.15 software (Qualisys AB, Gothenburg, Sweden). The trajectory of each of the 81 markers used in the model was identified and labelled. The resulting three-dimensional (3D) data was exported to a tab-separated values (.tsv) file. A script was developed using R programming language (R version 4.2.2, Vienna, Austria) to process the .tsv file and calculate the variables described in Table 1.
Force plate data was also exported from QTM to a .tsv file, and analysed using the R “stabilo” package (version 0.1.1, https://doi.org/10.32614/CRAN.package.stabilo) [54]. Extracted variables are detailed in Table 2.
2.3. Intervention
The individuals in the experimental group underwent two weekly sessions of GPR, each lasting approximately 45 to 50 min. The sessions were conducted in groups consisting of 2 to 3 participants and were led by the same physiotherapist with experience in applying the method over a period of 4 weeks. The 6 GPR postures described by Souchard et al. [35] were applied, three of which involved opening the hip angle, characterized by a progression from flexion to the extension of hips and knees to stretch the inspiratory and anterior chain (“frog on the ground”, standing with the back against the wall, and standing in the middle) and three involved closing the hip angle, characterized by hips at 90° of flexion and performed gradual knee extensions to stretch the inspiratory and posterior chain (“frog in the air”, sitting, and standing with the body leaning forward) (Figure 1). Each posture was held for 15 min, except for the standing in the middle posture, which lasted 5 min. The progression process will depend greatly on the individuality of each participant. This means that the stretching was increased as the participant was able to maintain all postural corrections without compensations.
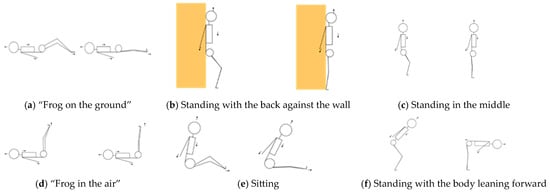
Figure 1.
Global Postural Reeducation Postures. Arrows indicate direction of movement and orange color represents the wall.
The description, details, and progression of the postures are presented in Table 3. All postures were performed with the intervention and supervision of the physiotherapist, involving manual contact to provide traction of the cervical and lumbar spine and to optimize the stretch while discouraging adjustments movements during the postures. The postures were also performed with the arms kept at a 45° abduction angle, with participants verbally instructed to adduct the scapulae, extend the arms toward the ground, and fully extend the elbows, wrists, and fingers.

Table 3.
Description, details, and progression of the postures.
The participants in the control group did not undergo any type of intervention.
2.4. Statistics
In the description and characterization of the sample, frequencies, as well as measures of central tendency and dispersion (mean and standard deviation), were used. For the comparison between groups, in the case of continuous variables, the student’s t-test for mean comparison was used, or its non-parametric counterpart, the Mann-Whitney U test. For dichotomous variables, the Chi-square test was used. For the analysis of the same group at different assessment points, the paired t-test was applied, specifically its non-parametric counterpart, the Wilcoxon test. The probability level accepted for statistical significance was p < 0.05.
3. Results
Table 4 highlights the general characteristics of the sample, demonstrating its homogeneity. No statistically significant differences were observed between the groups regarding age, weight, height, body mass index, and sex (p > 0.05).

Table 4.
Sample characterization.
From the analysis of the data related to the postural variables at baseline, it can be identified that the sample exhibits the main postural changes as forward head posture, rounded shoulders, cervical hyperlordosis, knee and calcaneal valgus, and lumbar hypolordosis (Table 5).

Table 5.
Difference between groups in postural variables—T0 and T1.
In the comparison between groups (experimental and control), no statistically significant differences were observed (p > 0.05), either at baseline or post-intervention (Table 5).
The observations vary in terms of the number of subjects, as it was not possible to collect data on all individuals and for all variables, as there are markers that would not be visible.
The results of the stabilometric variables are presented in Table 6. As with the previous variables, no statistically significant differences were found between the experimental group and the control group (p > 0.05), both at baseline and post-intervention (Table 6).

Table 6.
Difference between groups in the center of pressure variables—T0 and T1.
Evolution T0 vs. T1
In the experimental group, when comparing T0 and T1, no statistically significant differences were observed (p > 0.05) in any of the postural variables. In the control group, only the variable ’Left Knee Valgus’ showed a significant difference (p = 0.033), indicating a decrease in knee valgus (Table 7). The observations vary in terms of the number of subjects, as it was not possible to collect data on all individuals and for all variables, as there are markers that would not be visible.

Table 7.
Comparison of postural variables at T0 and T1—Experimental and Control Groups.
In the control group, when comparing T0 and T1, no statistically significant differences were observed (p > 0.05) in any of the center of pressure variables. In the experimental group, only the anteroposterior velocity variable showed a significant difference (p = 0.044), indicating a decrease in anteroposterior velocity from T0 to T1 (Table 8).

Table 8.
Comparison of center of pressure variables at T0 and T1—Experimental and Control Groups.
4. Discussion
This study aimed to evaluate the effectiveness of GPR on postural changes, trunk vertical alignment, overall spinal flexibility, and postural stability (center of pressure displacement) in young adults.
Postural changes were identified based on the examination of the retraining in Global Postural Reeducation, which evaluates its presence in the body segments of the head, cervical spine, shoulders, thoracic spine, lumbar spine, pelvis, knees, and calcaneus, corresponding to the shortening of the inspiratory, anterior, and posterior muscle chains. Through this analysis, it is possible to justify the identification of the main postural changes observed in our sample, showing a pattern of forward head and pelvic tilt, rounded shoulders, cervical hyperlordosis, and valgus knees and Calcaneus (Table 2). This pattern of changes is consistent with the results found in the literature, which report that forward head posture [20], rounded shoulders [77], cervical hyperlordosis [30], and valgus knees [28] are the most prevalent alterations. However, we found the result regarding lumbar lordosis in the control group to be unusual, as lumbar hyperlordosis is also reported in the literature as prevalent [17,18]. On the other hand, several authors note that the values corresponding to an adequate curvature are controversial, that the ideal range of lordosis remains unknown, and that it may be related to a variety of individual factors, such as weight, activity level, muscle strength, and flexibility of the spine and lower limbs [67,78]. Therefore, the normative values we considered may not be the most suitable for identifying lumbar curvature. The postural changes observed in our sample appear to primarily correspond, based on the examination of the retractions, to the shortening of the inspiratory and anterior chains [20]. We also evaluated the vertical alignment of the body and trunk flexion as global measures for assessing the retraction of the anterior and posterior chains. For vertical alignment and for trunk flexion, the values obtained by us are in accordance with the study by Krawczky et al. [52], which identified a reference value of 1.73 ± 0.94°, and with the study by Tulli et al. [79], which reported values of 20 ± 13.3 cm. Nevertheless, the observed values suggest a flexibility deficit, possibly indicative of posterior chain retraction. In this study, no statistically significant results were found between groups for any of the variables studied, namely postural changes, vertical alignment of the body, trunk anterior flexion, and center of pressure displacement (Table 5 and Table 6). Similar results regarding postural changes were reported by Cavalcanti et al. [80], who found that the ten GPR sessions were not sufficient to promote statistically significant improvements in the postural variables studied related to the body segments of the head, shoulders, thoracic kyphosis, and lumbar lordosis, either in the experimental group or in the control group, which did not undergo any intervention. In contrast to this, the study by Basso et al. [81] reported improvements in most of the postural variables assessed after ten GPR sessions, each lasting 45 min, conducted once a week with two postures per session. Similarly, Júnior and Tomaz [82] found that treatment with the RPG method was effective in postural correction, with improvements in head alignment and thoracic and lumbar scoliosis in nearly 50% of the 48 participants who underwent five GPR sessions over five consecutive days. Regarding trunk flexion, measured by the finger-to-floor distance, the results from the studies by Cavalcanti et al. [80] and Rosário et al. [83] differ from those found in this study. Both studies reported improvements in flexibility in GPR intervention programs conducted over 4 and 5 weeks, with the application of two postures per session. As for the results obtained in this study, the explanation for the discrepancies with other studies may lie in the number, duration, and frequency of the sessions, as well as the specificities of the intervention. Additionally, our sample consisted of young, healthy individuals with mild postural changes, which may have influenced the results. The same explanation can be applied to the results when comparing within the same group. We expected that, at least for the experimental group, there would have been some improvement in certain variables from T0 to T1 (Table 7 and Table 8). Although we found a statistically significant difference in the experimental group for the anteroposterior velocity variable (Table 8), this difference does not seem sufficient to guarantee the effectiveness of the intervention.
However, in the reviewed literature, studies by Lozano-Quijada et al. [8] and Fernandes et al. [34] were identified, which evaluated the effect of GPR on postural sway measured by the center of pressure (COP). In the first study, a single GPR session was conducted with university students, resulting in some modifications in postural sway, according to the authors. However, these should not be interpreted as improvements or changes in postural stability. The second study assessed the effects of GPR on women with chronic non-specific neck pain, focusing on pain, disability, and postural control. Eight biweekly sessions lasting 40 min over a 4-week period were conducted. The results of this study were statistically significant in all outcome measures except for postural stability. The anteroposterior velocity parameter in stabilometry can be considered, according to Massani et al. [84], an indicator of the efficiency of the postural control system and stands out as the most sensitive parameter. Lower values of the mean COP velocity are associated with better performance in postural control. Finally, the result with statistically significant differences observed in the control group for the postural variable left knee valgus (Table 7) does not seem particularly meaningful, especially considering that the values of evolution (from 176.37 ± 4.38 to 177.63 ± 3.10°) are not significantly divergent from the evolution observed in the experimental group (from 175.71 ± 3.44 to 176.53 ± 3.44°). This difference could be influenced by the sample size in each group. For the results obtained in the temporal evolution from T0 to T1 within each group (Table 7 and Table 8), in addition to the justification presented for the between-group comparison (Table 5 and Table 6), it seems that the fact that the intervention was conducted in a group setting, and therefore with less specificity and rigor in corrections tailored to each individual, may have contributed to the outcomes observed.
Limitations
The main limitations of this study include certain characteristics of the sample, namely its relatively small size, as well as the fact that it consisted primarily of individuals without pain or identified pathology and with only mild postural changes. Although the primary objective was related to evaluating the effect of GPR on postural changes and considering, retrospectively, similar studies with different outcomes, we question whether the number of postures used (six), the session frequency (twice a week), and the intervention duration (four weeks) were optimal for achieving the intended goal. Additionally, the fact that the intervention was conducted in a group setting and thus was less personalized may have also contributed as a limitation. On the other hand, the normative data used to identify the presence of postural changes, which are not universally agreed upon in the literature, may represent another limitation. These norms, primarily determined through photogrammetric approaches or various measurement instruments, might not concretely reflect the differentiation between the presence or absence of postural changes. Secondarily, the identification of anatomical landmarks for applying markers in the use of the 3D motion analysis system, as well as the complex data processing required by this system, may introduce bias in data collection. This is particularly relevant as the procedure relies heavily on the training and anatomical knowledge of the evaluator(s). And the scarcity of studies evaluating the benefits of GPR in postural changes. In this context, there is a clear need for further research in this area involving larger, more diverse, and well-controlled samples across different populations, as well as more targeted and potentially more personalized interventions.
5. Conclusions
From the work conducted, we can conclude that, in our sample, it is possible to identify the presence of a pattern that indicates a tendency to a postural change in healthy young students, primarily characterized by anteriorization of the head and pelvis, rolled shoulders, cervical hyperlordosis, and valgus knees and calcaneus. Global Postural education does not appear to be effective in improving postural changes and center of pressure displacement in healthy young students. More studies will have to be carried out to better understand this theme.
Author Contributions
Conceptualization, M.P.P., F.S. and S.M.; data curation, S.M.; software, S.M.; methodology, M.P.P., P.J.C., F.S. and S.M.; formal analysis, S.M. and L.C.; investigation, M.P.P.; resources, M.P.P.; writing—original draft preparation, M.P.P. and L.C.; writing—review and editing, P.J.C., S.M., F.S. and L.C.; supervision, P.J.C. and F.S.; project administration, M.P.P.; funding acquisition, M.P.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Faculty of Sports of the University of Porto (CEFADE 17.2019) from 17 July 2019.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy and ethical restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Pastorelli, F.; Pasquetti, P. Biomechanical analysis and rehabilitation in athletes. Clin. Cases Clin. Cases Min. Bone Metab. 2013, 10, 96. [Google Scholar]
- Huxham, F.E.; Goldie, P.A.; Patla, A.E. Theoretical considerations in balance assessment. Aust. J. Physiother. 2001, 47, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Rougier, P.R.; Genthon, N. Dynamical assessment of weight-bearing asymmetry during upright quiet stance in humans. Gait Posture 2009, 29, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Roggio, F.; Ravalli, S.; Maugeri, G.; Bianco, A.; Palma, A.; Di Rosa, M.; Musumeci, G. Technological advancements in the analysis of human motion and posture management through digital devices. World J. Orthop. 2021, 12, 467–484. [Google Scholar] [CrossRef] [PubMed]
- Das, K.; de Paula Oliveira, T.; Newell, J. Comparison of markerless and marker-based motion capture systems using 95% functional limits of agreement in a linear mixed-effects modelling framework. Sci. Rep. 2023, 13, 22880. [Google Scholar] [CrossRef]
- Blaszczyk, J.W.; Fredyk, A.; Blaszczyk, P.M.; Ashtiani, M. Step Response of Human Motor System as a Measure of Postural Stability in Children. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 895–903. [Google Scholar] [CrossRef]
- Richmond, S.B.; Otto, G.; Dames, K.D. Characterization of trial duration in traditional and emerging postural control measures. J. Biomech. 2023, 147, 111438. [Google Scholar] [CrossRef]
- Lozano-Quijada, C.; Poveda-Pagan, E.J.; Segura-Heras, J.V.; Hernandez-Sanchez, S.; Prieto-Castello, M.J. Changes in Postural Sway After a Single Global Postural Reeducation Session in University Students: A Randomized Controlled Trial. J. Manip. Physiol. Ther. 2017, 40, 467–476. [Google Scholar] [CrossRef]
- Blois, C.R.; Specht, L.; Paiz Rodrigues, B.L.; Moraes, M. Efeitos do método Pilates no tratamento das alterações posturais em universitários. Mov. Saúde Revistainspirar. 2016, 9, 31–36. [Google Scholar]
- Duarte, M.; Freitas, S.M. Revision of posturography based on force plate for balance evaluation. Rev. Bras. Fisioter. 2010, 14, 183–192. [Google Scholar] [CrossRef]
- Richmond, S.B.; Dames, K.D.; Goble, D.J.; Fling, B.W. Leveling the playing field: Evaluation of a portable instrument for quantifying balance performance. J. Biomech. 2018, 75, 102–107. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, M.; Kinel, E.; Roncoletta, P. Normative 3D opto-electronic stereo-photogrammetric posture and spine morphology data in young healthy adult population. PLoS ONE 2017, 12, e0179619. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, O. Interrelationship between postural balance and body posture in children and adolescents. J. Phys. Ther. Sci. 2017, 29, 1154–1158. [Google Scholar] [CrossRef]
- Ludwig, O.; Frohlich, M.; Schmitt, E. Therapy of poor posture in adolescents: Sensorimotor training increases the effectiveness of strength training to reduce increased anterior pelvic tilt. Cogent Med. 2016, 3, 1262094. [Google Scholar] [CrossRef]
- Alsalameh, A.M.; Harisi, M.; Alduayji, M.A.; Almutham, A.A.; Mahmood, F.M. Evaluating the relationship between smartphone addiction/overuse and musculoskeletal pain among medical students at Qassim University. J. Fam. Med. Prim. Care 2019, 8, 2953–2959. [Google Scholar] [CrossRef]
- Pacheco, M.P.; Carvalho, P.J.; Cavalheiro, L.; Sousa, F.M. Prevalence of Postural Changes and Musculoskeletal Disorders in Young Adults. Int. J. Environ. Res. Public Health 2023, 20, 7191. [Google Scholar] [CrossRef]
- Gonzalez-Galvez, N.; Marcos-Pardo, P.J.; Trejo-Alfaro, H.; Vaquero-Cristobal, R. Effect of 9-month Pilates program on sagittal spinal curvatures and hamstring extensibility in adolescents: Randomised controlled trial. Sci. Rep. 2020, 10, 9977. [Google Scholar] [CrossRef]
- Hesarikia, H.; Rahimnia, A.; Emami Meybodi, M.K. Differences between male and female sagittal spinopelvic parameters and alignment in asymptomatic pediatric and young adults. Minerva Orthop. Trauma 2018, 69, 44–48. [Google Scholar] [CrossRef]
- Ciric, A.; Causevic, D.; Bejdic, A. Differences in posture status between boys and girls 6 to 9 years of age. Homosporticus 2015, 17, 15–20. [Google Scholar]
- dos Santos, A.M.C.D.; do Amaral, C.P.; Oliveira, M.R.T.O.; de Souza Bastos, V.C.; do Nascimento, L.S.G.; da Cunha, E.F.; de Araújo, M.D.G.R. Alterações posturais da coluna vertebral em indivíduos jovens Universitários: Análise por biofotogrametria computadorizada. Rev. Saúde E Pesqui. 2014, 7, 191–198. [Google Scholar]
- Been, E.; Shefi, S.; Soudack, M. Cervical lordosis: The effect of age and gender. Spine J. 2017, 17, 880–888. [Google Scholar] [CrossRef] [PubMed]
- Dudko, M.V. Characteristic of biogeometric profile of students’ posture and physical fitness in process of physical education. Phys. Educ. Stud. 2015, 19, 10–16. [Google Scholar] [CrossRef]
- Liu, H.; Garrett, W.E.; Moorman, C.T.; Yu, B. Injury rate, mechanism, and risk factors of hamstring strain injuries in sports: A review of the literature. J. Sport Health Sci. 2012, 1, 92–101. [Google Scholar] [CrossRef]
- Cejudo, A.; Centenera-Centenera, J.M.; Santonja-Medina, F. The Potential Role of Hamstring Extensibility on Sagittal Pelvic Tilt, Sagittal Spinal Curves and Recurrent Low Back Pain in Team Sports Players: A Gender Perspective Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8654. [Google Scholar] [CrossRef] [PubMed]
- Senthil, S.P.; Vinodhini, R.; Vinosh Kumar, P.; Ambusam, S.; Rajkumar Krishnan, V. Effectiveness of Global Posture Re-education and McKenzie technique in Non-Specific Low Back Pain. Inti J. 2022, 2022, 39. [Google Scholar]
- Paillard, T. Relationship between Muscle Function, Muscle Typology and Postural Performance According to Different Postural Conditions in Young and Older Adults. Front. Physiol. 2017, 8, 585. [Google Scholar] [CrossRef]
- Souchard, P. Reeducação Postural Global: O Método; Elsevier: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Taylor, D.C.; Dalton, J.D., Jr.; Seaber, A.V.; Garrett, W.E., Jr. Viscoelastic properties of muscle-tendon units. The biomechanical effects of stretching. Am. J. Sports Med. 1990, 18, 300–309. [Google Scholar] [CrossRef]
- Bonetti, F.; Curti, S.; Mattioli, S.; Mugnai, R.; Vanti, C.; Violante, F.S.; Pillastrini, P. Effectiveness of a ‘Global Postural Reeducation’ program for persistent low back pain: A non-randomized controlled trial. BMC Musculoskelet. Disord. 2010, 11, 285. [Google Scholar] [CrossRef]
- Ferreira, G.E.; Barreto, R.G.; Robinson, C.C.; Plentz, R.D.; Silva, M.F. Global Postural Reeducation for patients with musculoskeletal conditions: A systematic review of randomized controlled trials. Braz. J. Phys. Ther. 2016, 20, 194–205. [Google Scholar] [CrossRef]
- Mendes-Fernandes, T.; Puente-Gonzalez, A.S.; Marquez-Vera, M.A.; Vila-Cha, C.; Mendez-Sanchez, R. Effects of Global Postural Reeducation versus Specific Therapeutic Neck Exercises on Pain, Disability, Postural Control, and Neuromuscular Efficiency in Women with Chronic Nonspecific Neck Pain: Study Protocol for a Randomized, Parallel, Clinical Trial. Int. J. Environ. Res. Public Health 2021, 18, 10704. [Google Scholar] [CrossRef]
- Castagnoli, C.; Cecchi, F.; Del Canto, A.; Paperini, A.; Boni, R.; Pasquini, G.; Vannetti, F.; Macchi, C. Effects in Short and Long Term of Global Postural Reeducation (GPR) on Chronic Low Back Pain: A Controlled Study with One-Year Follow-Up. Sci. World J. 2015, 2015, 271436. [Google Scholar] [CrossRef] [PubMed]
- Lawand, P.; Lombardi Junior, I.; Jones, A.; Sardim, C.; Ribeiro, L.H.; Natour, J. Effect of a muscle stretching program using the global postural reeducation method for patients with chronic low back pain: A randomized controlled trial. Jt. Bone Spine 2015, 82, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Mendes Fernandes, T.; Mendez-Sanchez, R.; Puente-Gonzalez, A.S.; Martin-Vallejo, F.J.; Falla, D.; Vila-Cha, C. A randomized controlled trial on the effects of “Global Postural Re-education” versus neck specific exercise on pain, disability, postural control, and neuromuscular features in women with chronic non-specific neck pain. Eur. J. Phys. Rehabil. Med. 2023, 59, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Souchard, P.E.; Meli, O.; Sgamma, D.; Pillastrini, P. Reeducação Postural Global. A tradição, o Presente e o Futuro; Summus Editorial: São Paulo, Brazil, 2022. [Google Scholar]
- Dimitrova, E.; Rohleva, M. Global Postural Reeducation in the treatment of postural impairments. Research Kinesiol. 2014, 4, 72–75. [Google Scholar]
- Amorim, C.S.; Gracitelli, M.E.; Marques, A.P.; Alves, V.L. Effectiveness of global postural reeducation compared to segmental exercises on function, pain, and quality of life of patients with scapular dyskinesis associated with neck pain: A preliminary clinical trial. J. Manip. Physiol. Ther. 2014, 37, 441–447. [Google Scholar] [CrossRef]
- Di Ciaccio, E.; Polastri, M.; Bianchini, E.; Gasbarrini, A. Herniated lumbar disc treated with Global Postural Reeducation. A middle-term evaluation. Eur. Rev. Med. Pharmacol. Sci. 2012, 16, 1072–1077. [Google Scholar]
- Lomas-Vega, R.; Garrido-Jaut, M.V.; Rus, A.; Del-Pino-Casado, R. Effectiveness of Global Postural Re-education for Treatment of Spinal Disorders: A Meta-analysis. Am. J. Phys. Med. Rehabil. 2017, 96, 124–130. [Google Scholar] [CrossRef]
- Agosti, V.; Vitale, C.; Avella, D.; Rucco, R.; Santangelo, G.; Sorrentino, P.; Varriale, P.; Sorrentino, G. Effects of Global Postural Reeducation on gait kinematics in parkinsonian patients: A pilot randomized three-dimensional motion analysis study. Neurol. Sci. 2016, 37, 515–522. [Google Scholar] [CrossRef]
- Corwell, B.N.; Davis, N.L. The Emergent Evaluation and Treatment of Neck and Back Pain. Emerg. Med. Clin. N. Am. 2020, 38, 167–191. [Google Scholar] [CrossRef]
- Adorno, M.L.; Brasil-Neto, J.P. Assessment of the quality of life through the SF-36 questionnaire in patients with chronic nonspecific low back pain. Acta Ortop. Bras. 2013, 21, 202–207. [Google Scholar] [CrossRef]
- Beynon, A.M.; Hebert, J.J.; Lebouef-Yde, C.; Walker, B.F. Potential risk factors and triggers for back pain in children and young adults. A scoping review, part I: Incident and episodic back pain. Chiropr. Man Therap. 2019, 27, 58. [Google Scholar] [CrossRef] [PubMed]
- Guastala, F.A.M.G.M.; Klein, P.F.; Leite, V.C.; Cappellazzo, R.; Facci, L.M. Efeitos da reeducação postural global e do isostretching em pacientes com lombalgia crônica não-específi ca: Ensaio clínico aleatório. Fisioter. Mov. Curitiba. 2016, 29, 515–525. [Google Scholar] [CrossRef]
- Soares, P.; Cabral, V.; Mendes, M.; Vieira, R.; Aviolo, G.; de Souza Vale, R.G. Efeitos do Programa Escola de Postura e Reeducacão Postural Global sobre a amplitude de movimento e níveis de dor em pacientes com lombalgia crónica. Rev. Andal. Med. Deporte 2016, 9, 23–28. [Google Scholar] [CrossRef]
- Longo, C.A.; Ferrari, S.; Lanza, A.; Vanti, C.; Stradiotti, P.; Ausenda, C.D. Effects of the “standing posture with flexion of the trunk” on the lumbar multifidus tropism in patients with chronic low back pain. A randomized, controlled pilot study. Sci. Riabil. 2016, 18, 5–12. [Google Scholar]
- O’Sullivan, P. It’s time for change with the management of non-specific chronic low back pain. Br. J. Sports Med. 2012, 46, 224–227. [Google Scholar] [CrossRef]
- Tomkinson, G.R.S.L. An anthropometric method of measuring standing posture with 3D analysis. In Kinanthropometry X; Marfell-Jones, M., Olds, T., Eds.; Routledge: London, UK, 2008; pp. 56–77. [Google Scholar]
- Dimitriadis, Z.; Podogyros, G.; Polyviou, D.; Tasopoulos, I.; Passa, K. The Reliability of Lateral Photography for the Assessment of the Forward Head Posture Through Four Different Angle-Based Analysis Methods in Healthy Individuals. Musculoskelet. Care 2015, 13, 179–186. [Google Scholar] [CrossRef]
- Ribeiro, A.F.M.; Bergmann, A.; Lemos, T.; Pacheco, A.G.; Russo, M.M.; de Oliveira, L.A.S.; de Carvalho Rodrigues, E. Reference Values for Human Posture Measurements Based on Computerized Photogrammetry: A Systematic Review. J. Manip. Physiol. Ther. 2017, 40, 156–168. [Google Scholar] [CrossRef]
- Trombini-Souza, F.; Ribeiro, A.P.; Iunes, D.H.; Monte-Raso, V.V. Correlações entre as estruturas dos membros inferiores. Fisioter. E Pesqui. 2009, 16, 205–210. [Google Scholar] [CrossRef]
- Krawczky, B.; Pacheco, A.G.; Mainenti, M.R. A systematic review of the angular values obtained by computerized photogrammetry in sagittal plane: A proposal for reference values. J. Manip. Physiol. Ther. 2014, 37, 269–275. [Google Scholar] [CrossRef]
- Carregaro, R.L.S.L.e.G.C.H. Comparação entre dois testes clínicos para avaliar a Flexibilidade dos músculos posteriores da coxa. Rev. Bras. Fisioter. 2007, 11, 139–145. [Google Scholar] [CrossRef]
- de Oliveira, J.M. Statokinesigram normalization method. Behav. Res. Methods 2017, 49, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, L.F.; Simpson, D.M.; Nadal, J. Calculation of area of stabilometric signals using principal component analysis. Physiol. Meas. 1996, 17, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Prieto, T.E.; Myklebust, J.B.; Hoffmann, R.G.; Lovett, E.G.; Myklebust, B.M. Measures of postural steadiness: Differences between healthy young and elderly adults. IEEE Trans. Biomed. Eng. 1996, 43, 956–966. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-de-las-Penas, C.; Alonso-Blanco, C.; Cuadrado, M.L.; Gerwin, R.D.; Pareja, J.A. Trigger points in the suboccipital muscles and forward head posture in tension-type headache. Headache 2006, 46, 454–460. [Google Scholar] [CrossRef]
- Raine, S.; Twomey, L.T. Head and shoulder posture variations in 160 asymptomatic women and men. Arch. Phys. Med. Rehabil. 1997, 78, 1215–1223. [Google Scholar] [CrossRef]
- Ruivo, R.M.; Pezarat-Correia, P.; Carita, A.I. Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain. Braz. J. Phys. Ther. 2014, 18, 364–371. [Google Scholar] [CrossRef]
- Raine, S.; Twomey, L. Posture of the head, shoulders and thoracic spine in comfortable erect standing. Aust. J. Physiother. 1994, 40, 25–32. [Google Scholar] [CrossRef]
- Gadotti, I.C.; Armijo-Olivo, S.; Silveira, A.; Magee, D. Reliability of the craniocervical posture assessment: Visual and angular measurements using photographs and radiographs. J. Manip. Physiol. Ther. 2013, 36, 619–625. [Google Scholar] [CrossRef]
- Nam, S.H.; Son, S.M.; Kwon, J.W.; Lee, N.K. The Intra- and Inter-rater Reliabilities of the Forward Head Posture Assessment of Normal Healthy Subjects. J. Phys. Ther. Sci. 2013, 25, 737–739. [Google Scholar] [CrossRef]
- Harrison, A.L.; Barry-Greb, T.; Wojtowicz, G. Clinical measurement of head and shoulder posture variables. J. Orthop. Sports Phys. Ther. 1996, 23, 353–361. [Google Scholar] [CrossRef]
- Harrison, D.E.; Harrison, D.D.; Troyanovich, S.J.; Harmon, S. A normal spinal position: It’s time to accept the evidence. J. Manip. Physiol. Ther. 2000, 23, 623–644. [Google Scholar] [CrossRef] [PubMed]
- Sacco, I.; Melo, M.; Rojas, G.; Naki, I.; Burgi, K.; Silveira, L.; Guedes, V.; Kanayama, E.; Vasconcelos, A.; Penteado, D.; et al. Análise biomecânica e cinesiológica de posturas mediante fotografia digital: Estudo de casos. Rev. Bras. Ciênc. Mov. 2003, 11, 25–33. [Google Scholar]
- Vaz, G.; Roussouly, P.; Berthonnaud, E.; Dimnet, J. Sagittal morphology and equilibrium of pelvis and spine. Eur. Spine J. 2002, 11, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Been, E.; Kalichman, L. Lumbar lordosis. Spine J. 2014, 14, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Laouissat, F.; Sebaaly, A.; Gehrchen, M.; Roussouly, P. Classification of normal sagittal spine alignment: Refounding the Roussouly classification. Eur. Spine J. 2018, 27, 2002–2011. [Google Scholar] [CrossRef]
- Candotti, C.T.; Gelain, G.M.; Antoniolli, A.; Araujo, L.M.; Vieira, A.; Loss, J.F. Repeatability and Reproducibility of Postural Variables by Photogrammetry. J. Manip. Physiol. Ther. 2019, 42, 372–378. [Google Scholar] [CrossRef]
- Siqueira, C.M.; Rossi, A.; Shimamoto, C.; Tanaka, C. Balance highly influences flexibility measured by the toe-touch test. Hum. Mov. Sci. 2018, 62, 116–123. [Google Scholar] [CrossRef]
- Ayala, F.; Sainz de Baranda, P.; De Ste Croix, M.; Santonja, F. Reproducibility and criterion-related validity of the sit and reach test and toe touch test for estimating hamstring flexibility in recreationally active young adults. Phys. Ther. Sport 2012, 13, 219–226. [Google Scholar] [CrossRef]
- Ekedahl, H.; Jonsson, B.; Frobell, R.B. Fingertip-to-floor test and straight leg raising test: Validity, responsiveness, and predictive value in patients with acute/subacute low back pain. Arch. Phys. Med. Rehabil. 2012, 93, 2210–2215. [Google Scholar] [CrossRef]
- Robinson, H.S.; Mengshoel, A.M. Assessments of lumbar flexion range of motion: Intertester reliability and concurrent validity of 2 commonly used clinical tests. Spine 2014, 39, E270–E275. [Google Scholar] [CrossRef]
- Scoppa, F.; Gallamini, M.; Belloni, G.; Messina, G. Clinical stabilometry standardization: Feet position in the static stabilometric assessment of postural stability. Acta Medica Mediterr. 2017, 33, 707. [Google Scholar]
- Magnusson, S.P.; Simonsen, E.B.; Aagaard, P.; Boesen, J.; Johannsen, F.; Kjaer, M. Determinants of musculoskeletal flexibility: Viscoelastic properties, cross-sectional area, EMG and stretch tolerance. Scand. J. Med. Sci. Sports 1997, 7, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Wilken, J.M.; Rodriguez, K.M.; Brawner, M.; Darter, B.J. Reliability and Minimal Detectible Change values for gait kinematics and kinetics in healthy adults. Gait Posture 2012, 35, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Detsch, C.; Luz, A.M.; Candotti, C.T.; de Oliveira, D.S.; Lazaron, F.; Guimarães, L.K.; Schimanoski, P. [Prevalence of postural changes in high school students in a city in southern Brazil]. Rev. Panam Salud Publica 2007, 21, 231–238. [Google Scholar] [CrossRef]
- Ghandhari, H.; Hesarikia, H.; Ameri, E.; Noori, A. Assessment of normal sagittal alignment of the spine and pelvis in children and adolescents. Biomed. Res. Int. 2013, 2013, 842624. [Google Scholar] [CrossRef]
- Tully, E.A.; Stillman, B.C. Computer-aided video analysis of vertebrofemoral motion during toe touching in healthy subjects. Arch. Phys. Med. Rehabil. 1997, 78, 759–766. [Google Scholar] [CrossRef]
- Cavalcanti, I.F.; Antonino, G.B.; Monte-Silva, K.K.D.; Guerino, M.R.; Ferreira, A.P.L.; das Gracas Rodrigues de Araujo, M. Global Postural Re-education in non-specific neck and low back pain treatment: A pilot study. J. Back Musculoskelet. Rehabil. 2020, 33, 823–828. [Google Scholar] [CrossRef]
- Basso, D.; Corrêa, E.; da Silva, A. Efeito da reeducação postural global no alinhamento corporal e nas condições clínicas de indivíduos com disfunção temporomandibular associada a desvios posturais. Fisioter. Pesqui. 2010, 17, 63–68. [Google Scholar] [CrossRef]
- Júnior, V.; Ronaldo, J.; Carlos, T. Efeitos da reeducação postural global pelo método RPG/RFL na correção postural e no reequilíbrio muscular. Fisioter. Mov. 2008, 21, 127–137. [Google Scholar]
- do Rosario, J.L. Photographic analysis of human posture: A literature review. J. Bodyw. Mov. Ther. 2014, 18, 56–61. [Google Scholar] [CrossRef]
- Masani, K.; Vette, A.H.; Abe, M.O.; Nakazawa, K. Center of pressure velocity reflects body acceleration rather than body velocity during quiet standing. Gait Posture 2014, 39, 946–952. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).