Enhancing Emotion Regulation Skills in High-Risk Adolescents Due to the Existence of Psychopathology in the Family: Feasibility and Uncontrolled Pilot Study of a Group Intervention in a Naturalistic School Setting
Abstract
1. Introduction
Current Study
2. Materials and Methods
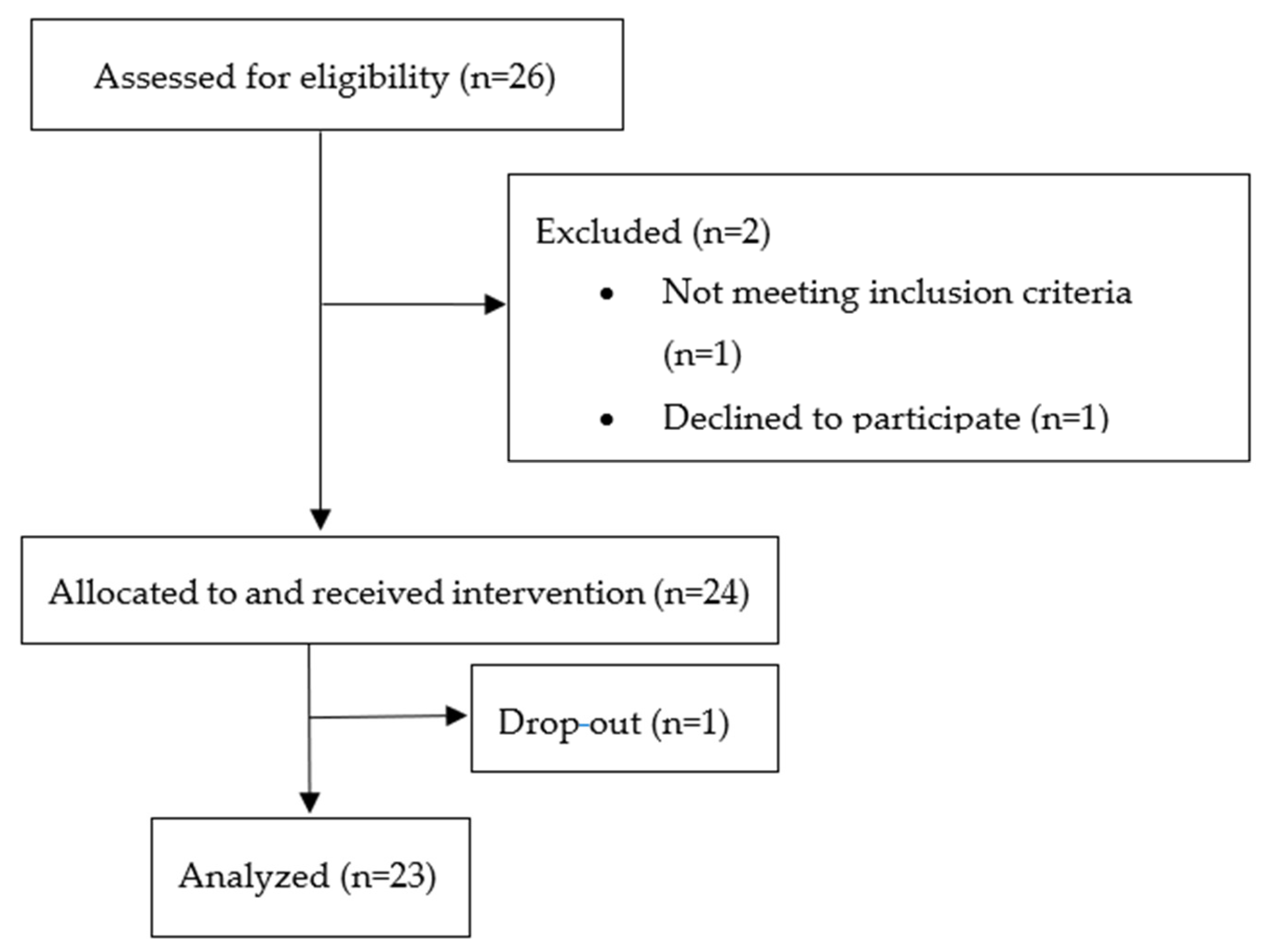
2.1. Participants
2.2. Measures
2.3. Procedure
3. Results
3.1. Feasibility and Acceptability
3.2. Comparison of Pre- and Post-Intervention Status
3.2.1. Emotion Regulation
3.2.2. Symptom Reduction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Hashmi, S. Adolescence: An Age of Storm and Stress. Rev. Arts Humanit. 2013, 2, 19–33. [Google Scholar]
- Romeo, R.D. The Teenage Brain: The Stress Response and the Adolescent Brain. Curr. Dir. Psychol. Sci. 2013, 22, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Seiffge-Krenke, I. Coping with Relationship Stressors: A Decade Review. J. Res. Adolesc. 2011, 21, 196–210. [Google Scholar] [CrossRef]
- Keenan, K. Emotion dysregulation as a risk factor for child psychopathology. Clin. Psychol. Sci. Pract. 2000, 7, 418–434. [Google Scholar] [CrossRef]
- Otterpohl, N.; Schwinger, M.; Wild, E. Exploring the interplay of adaptive and maladaptive strategies: Prevalence and functionality of anger regulation profiles in early adolescence. J. Early Adolesc. 2016, 36, 1042–1069. [Google Scholar] [CrossRef]
- Southam-Gerow, M.A.; Kendall, P.C. Emotion regulation and understanding: Implications for child psychopathology and therapy. Clin. Psychol. Rev. 2002, 22, 189–222. [Google Scholar] [CrossRef] [PubMed]
- Southam-Gerow, M.A.; Kendall, P.C. A preliminary study of the emotional understanding of youth referred for treatment of anxiety disorders. J. Clin. Child Psychol. 2000, 29, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Suveg, C.; Zeman, J. Emotion regulation in children with anxiety disorders. J. Clin. Child Adolesc. Psychol. 2004, 33, 750–759. [Google Scholar] [CrossRef] [PubMed]
- Silk, J.S.; Steinberg, L.; Morris, A.S. Adolescents’ emotion regulation in daily life: Links to depressive symptoms and problem behaviors. Child Dev. 2003, 74, 1869–1880. [Google Scholar] [CrossRef]
- Bohnert, A.M.; Crnic, K.A.; Lim, K.G. Emotional competence and aggressive behavior in school-age children. J. Abnorm. Child Psychol. 2003, 31, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Dearing, K.F.; Hubbard, J.A.; Ramsden, S.R.; Parker, E.H.; Relyea, N.; Smithmyer, C.M.; Flanagan, K.D. Children’s self-reports about anger regulation: Direct and indirect links to social preference and aggression. Merrill-Palmer Q. 2002, 48, 308–336. [Google Scholar] [CrossRef]
- Eisenberg, N.; Guthrie, I.K.; Fabes, R.A.; Shepard, S.; Losoya, S.; Murphy, B.; Jones, S.; Poulin, R.; Reiser, M. Prediction of elementary school children’s externalizing problem behaviors from attentional and behavioral regulation and negative emotionality. Child Dev. 2000, 71, 1367–1382. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, K.A.; Hatzenbuehler, M.L.; Mennin, D.S.; Nolen-Hoeksema, S. Emotion dysregulation and adolescent psychopathology: A prospective study. Behav. Res. Ther. 2011, 49, 544–554. [Google Scholar] [CrossRef] [PubMed]
- Gilliom, M.; Shaw, D.S.; Beck, J.E.; Schonberg, M.A.; Lukon, J.L. Anger regulation in disadvantaged preschool boys: Strategies, antecedents, and the development of self-control. Dev. Psychol. 2002, 38, 222–235. [Google Scholar] [CrossRef]
- Hinshaw, S.P. Impulsivity, emotion regulation, and developmental psychopathology: Specificity versus generality of linkages. Ann. N. Y. Acad. Sci. 2003, 1008, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Aldao, A.; Dixon-Gordon, K.L. Broadening the scope of research on emotion regulation strategies and psychopathology. Cogn. Behav. Ther. 2014, 43, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Orobio de Castro, B.; Merk, W.; Koops, W.; Veerman, J.W.; Bosch, J.D. Emotions in social information processing and their relations with reactive and proactive aggression in referred aggressive boys. J. Clin. Child Adolesc. Psychol. 2005, 34, 105–116. [Google Scholar] [CrossRef] [PubMed]
- Reupert, A.; Maybery, D. What do we know about families where parents have a mental illness? A systematic review. Child Youth Serv. 2016, 37, 98–111. [Google Scholar] [CrossRef]
- Schafer, J.O.; Naumann, E.; Holmes, E.A.; Tuschen-Caffier, B.; Samson, A.C. Emotion regulation strategies in depressive and anxiety symptoms in youth: A meta analytic review. J. Youth Adolesc. 2017, 46, 261–276. [Google Scholar] [CrossRef]
- Bridges, L.J.; Denham, S.A.; Ganiban, J.M. Definitional issues in emotion regulation research. Child Dev. 2004, 75, 340–345. [Google Scholar] [CrossRef]
- Panayiotou, G.; Panteli, M.; Vlemincx, E. Adaptive and maladaptive emotion processing and regulation, and the case of alexithymia. Cogn. Emot. 2019, 35, 488–499. [Google Scholar] [CrossRef] [PubMed]
- Aldao, A.; Nolen-Hoeksema, S. When are adaptive strategies most predictive of psychopathology? J. Abnorm. Psychol. 2012, 121, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Aldao, A.; Nolen-Hoeksema, S.; Schweizer, S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef] [PubMed]
- Gross, J.J. The emerging field of emotion regulation: An integrative review. Rev. Gen. Psychol. 1998, 2, 271–299. [Google Scholar] [CrossRef]
- Gross, J.J. Emotion regulation: Taking stock and moving forward. Emotion 2013, 13, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Barrett, P.M.; Turner, C. Prevention of anxiety symptoms in primary school children: Preliminary results from a universal school-based trial. Br. J. Clin. Psychol. 2001, 40, 399–410. [Google Scholar] [CrossRef] [PubMed]
- Dadds, M.R.; Spence, S.H.; Holland, D.E.; Barrett, P.M.; Laurens, K.R. Prevention and early intervention for anxiety disorders: A controlled trial. J. Consult. Clin. Psychol. 1997, 65, 627–635. [Google Scholar] [CrossRef] [PubMed]
- Dawe, S.; Seinen, A.; Kavanagh, D. An examination of the utility of the AUDIT in people with schizophrenia. J. Stud. Alcohol Drugs 2000, 61, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Lyneham, H.J.; Abbott, M.J.; Wignall, A.; Rapee, R.M. The Cool Kids Anxiety Treatment Program; MUARU, Macqaurie University: Sydney, Australia, 2003. [Google Scholar]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C. The Fagerstrom Test for Nicotine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. Br. J. Addict. 1991, 86, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Hirshfeld-Becker, D.R.; Masek, B.; Henin, A.; Blakely, L.R.; Rettew, D.C.; Dufton, L.; Segool, N.; Biederman, J. Cognitive-behavioral intervention with young anxious children. Harv. Rev. Psychiatry 2008, 16, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Hudson, J.L.; Rapee, R.M.; Deveney, C.; Schniering, C.A.; Lyneham, H.J.; Bovopoulos, N. Cognitive-behavioral treatment versus an active control for children and adolescents with anxiety disorders: A randomized trial. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Shaw, H.; Bohon, C.; Marti, C.N.; Rohde, P. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. J. Consult. Clin. Psychol. 2009, 77, 486–503. [Google Scholar] [CrossRef] [PubMed]
- Garland, A.F.; Hawley, M.K.; Brookman-Frazee, L.; Hurlburt, M.S. Identifying common elements of evidence-based psychosocial treatments for children’s disruptive behavior problems. J. Am. Acad. Child Adolesc. Psychiatry 2008, 47, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Menting, A.T.; Albrecht, G.; De Castro, B.O. Effective Elements of Interventions for Externalizing Problem Behavior in Youth; Universiteit Utrecht: Utrecht, The Netherlands, 2015. [Google Scholar]
- Te Brinke, L.W.; Schuiringa, H.D.; Menting, A.T.A.; Deković, M.; de Castro, B.O. A cognitive versus behavioral approach to emotion regulation training for externalizing behavior problems in adolescence: Study protocol of a randomized controlled trial. BMC Psychol. 2018, 6, 49. [Google Scholar] [CrossRef] [PubMed]
- McCart, M.R.; Priester, P.E.; Davies, W.H.; Azen, R. Differential effectiveness of behavioral parent-training and cognitive-behavioral therapy for antisocial youth: A meta-analysis. J. Abnorm. Child Psychol. 2006, 34, 527–543. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.J.; Lipsey, M.W. School-based interventions for aggressive and disruptive behavior: Update of a meta-analysis. Am. J. Prev. Med. 2007, 33, S130–S143. [Google Scholar] [CrossRef] [PubMed]
- Hans, E.; Hiller, W. Effectiveness of and dropout from outpatient cognitive behavioral therapy for adult unipolar depression: A meta-analysis of nonrandomized effectiveness studies. J. Consult. Clin. Psychol. 2013, 81, 75. [Google Scholar] [CrossRef]
- Karekla, M.; Konstantinou, P.; Ioannou, M.; Kareklas, I.; Gloster, A.T. The Phenomenon of Treatment Dropout, Reasons and Moderators in Acceptance and Commitment Therapy and Other Active Treatments: A Meta-Analytic Review. Clin. Psychol. Eur. 2019, 1, 1–36. [Google Scholar] [CrossRef]
- Zhou, X.; Hetrick, S.E.; Cuijpers, P.; Qin, B.; Barth, J.; Whittington, C.J.; Cohen, D.; Del Giovane, C.; Liu, Y.; Michael, K.D.; et al. Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: A systematic review and network meta-analysis. World Psychiatr. Assoc. 2015, 14, 207–222. [Google Scholar] [CrossRef]
- Prinz, R.J.; Miller, G.E. Family-based treatment for childhood antisocial behavior: Experimental influences on dropout and engagement. J. Consult. Clin. Psychol. 1994, 62, 645–650. [Google Scholar] [CrossRef]
- Luk, E.S.; Staiger, P.K.; Mathai, J.; Wong, L.; Birleson, P.; Adler, R. Children with persistent conduct problems who dropout of treatment. Eur. Child Adolesc. Psychiatry 2001, 10, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Chin, F.; Hayes, S.C. Acceptance and Commitment Therapy and the Cognitive Behavioral Tradition: Assumptions, Model, Methods, and Outcomes. In The Science of Cognitive Behavioral Therapy; Hofmann, S.G., Asmundson, G.J.G., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 155–173. [Google Scholar]
- Biglan, A.; Hayes, S.C.; Pistorello, J. Acceptance and Commitment: Implications for Prevention Science. Prev. Sci. 2008, 9, 139–152. [Google Scholar] [CrossRef] [PubMed]
- Carona, C. The philosophical assumptions across the ‘three waves’ of cognitive–behavioural therapy: How compatible are they? BJPsych Adv. 2023, 29, 213–217. [Google Scholar] [CrossRef]
- Fletcher, L.; Hayes, S.C. Relational Frame Theory, Acceptance and Commitment Therapy, and a functional analytic definition of Mindfulness. J. Ration.-Emotive Cogn.-Behav. Ther. 2005, 23, 315–336. [Google Scholar] [CrossRef]
- Hayes, S.C. Acceptance and Commitment Therapy, Relational Frame Theory, and the Third Wave of Behavioral and Cognitive Therapies. Behav. Ther. 2004, 354, 639–665. [Google Scholar] [CrossRef]
- Karekla, M.; Panayiotou, G. Coping and experiential avoidance: Unique or overlapping constructs? J. Behav. Ther. Exp. Psychiatry 2011, 42, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, C.L.; Puleo, C.M.; Settipani, C.A.; Brodman, D.M.; Edmunds, J.M.; Cummings, C.M.; Kendall, P.C. History of Cognitive-Behavioral Therapy (CBT) in Youth. Child Adolesc. Psychiatr. Clin. N. Am. 2011, 20, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, S.G.; Asu Asnaani, M.A.; Imke, J.J.; Vonk, M.A.; Sawyer, A.T.; Fang, A. The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cogn. Ther. Res. 2012, 36, 427–440. [Google Scholar] [CrossRef] [PubMed]
- Linehan, M.M. DBT Skills Training Manual, 2nd ed.; The Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Rathus, J.H.; Miller, A.L. DBT Skills Manual for Adolescents; Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Yeomans, F.E.; Levy, K.N.; Meehan, K.B. Treatment approaches for borderline personality disorder. Psychiatr. Times 2012, 29, 42–46. [Google Scholar]
- Schleider, J.L.; Burnette, J.L.; Widman, L.; Hoyt, C.; Prinstein, M.J. Randomized trial of a single-session growth mind-set intervention for rural adolescents’ internalizing and externalizing problems. J. Clin. Child Adolesc. Psychol. 2019, 49, 660–672. [Google Scholar] [CrossRef] [PubMed]
- Reupert, A.; Maybery, D. Strategies and issues in supporting children whose parents have a mental illness within the school system. Sch. Psychol. Int. 2007, 28, 195–205. [Google Scholar] [CrossRef]
- Merikangas, K.R.; He, J.P.; Burstein, M.; Swanson, S.A.; Avenevoli, S.; Cui, L.; Benjet, C.; Georgiades, K.; Swendsen, J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 980–989. [Google Scholar] [CrossRef] [PubMed]
- Morrison, N. Cognitive group therapy: Treatment of choice or sub-optimal option? Behav. Cogn. Psychother. 2001, 29, 311–332. [Google Scholar] [CrossRef]
- Yalom, I. Theory and Practice of Group Psychotherapy, 3rd ed.; Basic Books: New York, NY, YSA, 1985. [Google Scholar]
- Gratz, K.L.; Roemer, L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Garnefski, N.; Kraaij, V.; Spinhoven, P.H. Manual for the Use of the Cognitive Emotion Regulation Questionnaire; DATEC: Leiderdorp, The Netherlands, 2002. [Google Scholar]
- Garnefski, N.; Kraaij, V.; Spinhoven, P.H. Negative life events, cognitive emotion regulation and emotional problems. Personal. Individ. Differ. 2001, 30, 1311–1327. [Google Scholar] [CrossRef]
- Achenbach, T.M.; McConaughy, S.H.; Howell, C.T. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychol. Bull. 1987, 101, 213–232. [Google Scholar] [CrossRef] [PubMed]
- Roussos, A.; Francis, K.; Zoubou, V.; Kiprianos, S.; Prokopiou, A.; Richardson, C. The standardization of Achenbach’s Youth Self-Report in Greece in a national sample of high school students. Eur. Child Adolesc. Psychiatry 2001, 10, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Ebesutani, C.; Bernstein, A.; Martinez, J.I.; Chorpita, B.F. The Youth Self Report: Applicability and Validity Across Younger and Older Youths. J. Clin. Child Adolesc. Psychol. 2011, 40, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Babor, T.F.; de la Fuente, J.R.; Saunders, J.; Grant, M. The Alcohol Use Disorders Identification Test. In Guidelines for Use in Primary Health Care; World Health Organization: Geneva, Switzerland, 1992. [Google Scholar]
- Allen, J.P.; Litten, R.Z.; Fertig, J.B.; Babor, T. A review of research on the alcohol use disorders identification test (AUDIT). Alcohol. Clin. Exp. Res. 1997, 21, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Karno, M.; Granholm, E.; Lin, A. Factor structure of the alcohol use disorders identification test (AUDIT) in a mental health clinic sample. J. Stud. Alcohol 2000, 61, 751–758. [Google Scholar] [CrossRef]
- Moussas, G.; Dadouti, G.; Douzenis, A.; Poulis, E.; Tselebis, A.; Bratis, D.; Christodoulou, C.; Lykouras, L. The Alcohol Use Disorders Identification Test (AUDIT): Reliability and validity of the Greek version. Ann. Gen. Psychiatry 2009, 8, 11. [Google Scholar] [CrossRef]
- Stavrinides, P.; Georgiou, S.; Demetriou, A. Longitudinal associations between adolescent alcohol use and parents’ sources of knowledge. Br. J. Dev. Psychol. 2010, 28, 643–655. [Google Scholar] [CrossRef] [PubMed]
- Karekla, M.; Symeou, A.; Tsangari, H.; Kapsou, M.; Constantinou, M. Smoking prevalence and tobacco exposure among adolescents in Cyprus. Eur. J. Public Health 2009, 19, 655–661. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gotzsche, P.C.; Devereaux, P.J. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef] [PubMed]
- Thissen, D.; Steinberg, L.; Kuang, D. Quick and Easy Implementation of the Benjamini-Hochberg Procedure for Controlling the False Positive Rate in Multiple Comparisons. J. Educ. Behav. Stat. 2002, 27, 77–83. [Google Scholar] [CrossRef]
- Kidger, J.; Araya, R.; Donovan, J.; Gunnell, D. The effect of the school environment on the emotional health of adolescents: A systematic review. Pediatrics 2012, 129, 925–949. [Google Scholar] [CrossRef] [PubMed]
- Lewis, T.J.; Jones, S.E.; Horner, R.H.; Sugai, G. School-wide positive behavior support and students with emotional/behavioral disorders: Implications for prevention, identification and intervention. Exceptionality 2010, 18, 82–93. [Google Scholar] [CrossRef]
- Blatch-Jones, A.J.; Pek, W.; Kirkpatrick, E.; Ashton-Key, M. Role of feasibility and pilot studies in randomised controlled trials: A cross-sectional study. BMJ Open 2018, 8, e022233. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, G.A.; Dodd, S.; Williamson, P.R. Design and analysis of pilot studies: Recommendations for good practice. J. Eval. Clin. Pract. 2004, 10, 307–312. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, K.A.; Aldao, A.; Wisco, B.E.; Hilt, L.M. Rumination as a transdiagnostic factor underlying transitions between internalizing symptoms and aggressive behavior in early adolescents. J. Abnorm. Psychol. 2014, 123, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.C.; Ollendick, T.H. The comorbidity of conduct problems and depression in childhood and adolescence. Clin. Child Fam. Psychol. Rev. 2006, 9, 201–220. [Google Scholar] [CrossRef] [PubMed]
| Session | Topic | Session Components | ER Skill |
|---|---|---|---|
| 1 | Introduction |
| |
| 2 | Understanding emotions |
| Emotion recognition |
| 3 | Acceptance of emotions |
| Acceptance skills |
| 4 | Thinking styles |
| Cognitive restructuring |
| 5 | Sadness and anxiety management |
| Behavioral activation |
| 6 | Anger management and problem solving |
| DBT skills |
| F | p | ηp2 | |
|---|---|---|---|
| DERS | |||
| Non-acceptance of emotional responses | 5.67 | 0.03 | 0.25 |
| Difficulties engaging in goal directed behavior | 3.45 | 0.08 | 0.17 |
| Impulse control difficulties | 3.22 | 0.09 | 0.15 |
| Lack of emotional awareness | 0.31 | 0.58 | 0.02 |
| Limited access to emotion regulation strategies | 11.17 | 0.01 | 0.38 |
| Lack of emotional clarity | 2.25 | 0.15 | 0.12 |
| CERQ | |||
| Self-blame | 12.27 | 0.01 | 0.42 |
| Acceptance | 2.15 | 0.160 | 0.11 |
| Rumination | 2.82 | 0.11 | 0.14 |
| Positive refocusing | 0.00 | 0.95 | 0.01 |
| Refocus on planning | 0.83 | 0.37 | 0.05 |
| Positive reappraisal | 0.92 | 0.35 | 0.05 |
| Putting into perspective | 1.56 | 0.23 | 0.08 |
| Catastrophizing | 3.19 | 0.09 | 0.15 |
| Other-blame | 1.17 | 0.29 | 0.06 |
| YSR problems | |||
| Affective problems | 12.97 | 0.01 | 0.37 |
| Anxiety problems | 1.30 | 0.26 | 0.06 |
| Somatic problems | 0.00 | 1.00 | 0.01 |
| ADHD | 6.17 | 0.02 | 0.22 |
| Oppositional defiant problems | 4.52 | 0.05 | 0.17 |
| Conduct problems | 7.56 | 0.01 | 0.26 |
| Nicotine dependence | 15.6 | 0.01 | 0.57 |
| Alcohol dependence | 8.52 | 0.01 | 0.40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Theodorou, C.; Karekla, M.; Panayiotou, G. Enhancing Emotion Regulation Skills in High-Risk Adolescents Due to the Existence of Psychopathology in the Family: Feasibility and Uncontrolled Pilot Study of a Group Intervention in a Naturalistic School Setting. Int. J. Environ. Res. Public Health 2024, 21, 738. https://doi.org/10.3390/ijerph21060738
Theodorou C, Karekla M, Panayiotou G. Enhancing Emotion Regulation Skills in High-Risk Adolescents Due to the Existence of Psychopathology in the Family: Feasibility and Uncontrolled Pilot Study of a Group Intervention in a Naturalistic School Setting. International Journal of Environmental Research and Public Health. 2024; 21(6):738. https://doi.org/10.3390/ijerph21060738
Chicago/Turabian StyleTheodorou, Christiana, Maria Karekla, and Georgia Panayiotou. 2024. "Enhancing Emotion Regulation Skills in High-Risk Adolescents Due to the Existence of Psychopathology in the Family: Feasibility and Uncontrolled Pilot Study of a Group Intervention in a Naturalistic School Setting" International Journal of Environmental Research and Public Health 21, no. 6: 738. https://doi.org/10.3390/ijerph21060738
APA StyleTheodorou, C., Karekla, M., & Panayiotou, G. (2024). Enhancing Emotion Regulation Skills in High-Risk Adolescents Due to the Existence of Psychopathology in the Family: Feasibility and Uncontrolled Pilot Study of a Group Intervention in a Naturalistic School Setting. International Journal of Environmental Research and Public Health, 21(6), 738. https://doi.org/10.3390/ijerph21060738






