Validating Constructs of the Depression, Anxiety, and Stress Scale-21 and Exploring Health Indicators to Predict the Psychological Outcomes of Students Enrolled in the Pacific Islands Cohort of College Students
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedures
2.2. Participants
2.3. Measures
- Diet: The diet questionnaire was adapted from the 2013 Behavioral Risk Factor Surveillance System (BRFSS) survey [89]. This survey is a U.S. national self-report survey that collects and provides prevalence data about health-related risk behaviors, chronic health conditions, and the use of preventive services. The diet questionnaire selected for this study from the PICCS focused on the frequency of consuming fruits, vegetables, and fast foods. The respondents indicated how often they consumed the selected food types, and the responses for fruits and vegetables were scored as Daily = 3, Weekly = 2, Monthly = 1, and Seldom = 0. The fast-food responses were categorized as Daily = 0, Weekly = 1, Monthly = 2, and Seldom = 3. The scores for the frequency of each food type were summed up and ranged from 0 to 9, where 9 indicated a high frequency of fruit and vegetable consumption and a low frequency of fast-food consumption. In contrast, 0 indicated a low frequency of fruit and vegetable consumption and a high frequency of fast-food consumption;
- Sleep: The quantity and quality of sleep were assessed by the questions adapted from the Pittsburgh Sleep Quality Index (PSQI) [90]. As for the quantity of sleep, the question asked was, “How many hours of actual sleep do you get at night?” The participants were asked to provide a numerical response, and if answered in ranges (e.g., 6–7 h), the average of the two numbers (e.g., 6.5 h) was taken. As for the quality of sleep, the question asked was, “How would you rate your sleep quality overall?” The participants were asked to choose one of the following four options: “Very good”, “Fairly good”, “Fairly bad”, or “Very bad”. Here, the component score for the responses was coded 0–3, where 0 indicated “Very bad”, and 3 “Very good”;
- Physical activity: The physical activity in this study was evaluated using the Physical Activity Rating Questionnaire (PAR-Q) [91]. The participants were asked to use a number 0–7 to best describe their general activity level for the previous month. Zero indicated “avoid physical assertion”, while seven indicated running over 10 miles per week or spending over 3 h per week participating in comparable physical activity;
- Depression, anxiety, and stress: The constructs of depression, anxiety, and stress were measured by the 21-item short-form of the Depression, Anxiety, and Stress Scale (DASS-21) [51]. Participants rated how often they experienced the symptoms associated with depression, anxiety, and stress. “Never” was scored 0, “Sometimes” was scored 1, “Often” was scored 2, and “Almost always” was scored 3. The scores were added and multiplied by 2 to calculate the final score;
- Covariates: some possible covariates suggested by the literature that were accounted for in this study were gender, BMI, ethnicity, SES, and the year of data collection.
2.4. Data Analysis
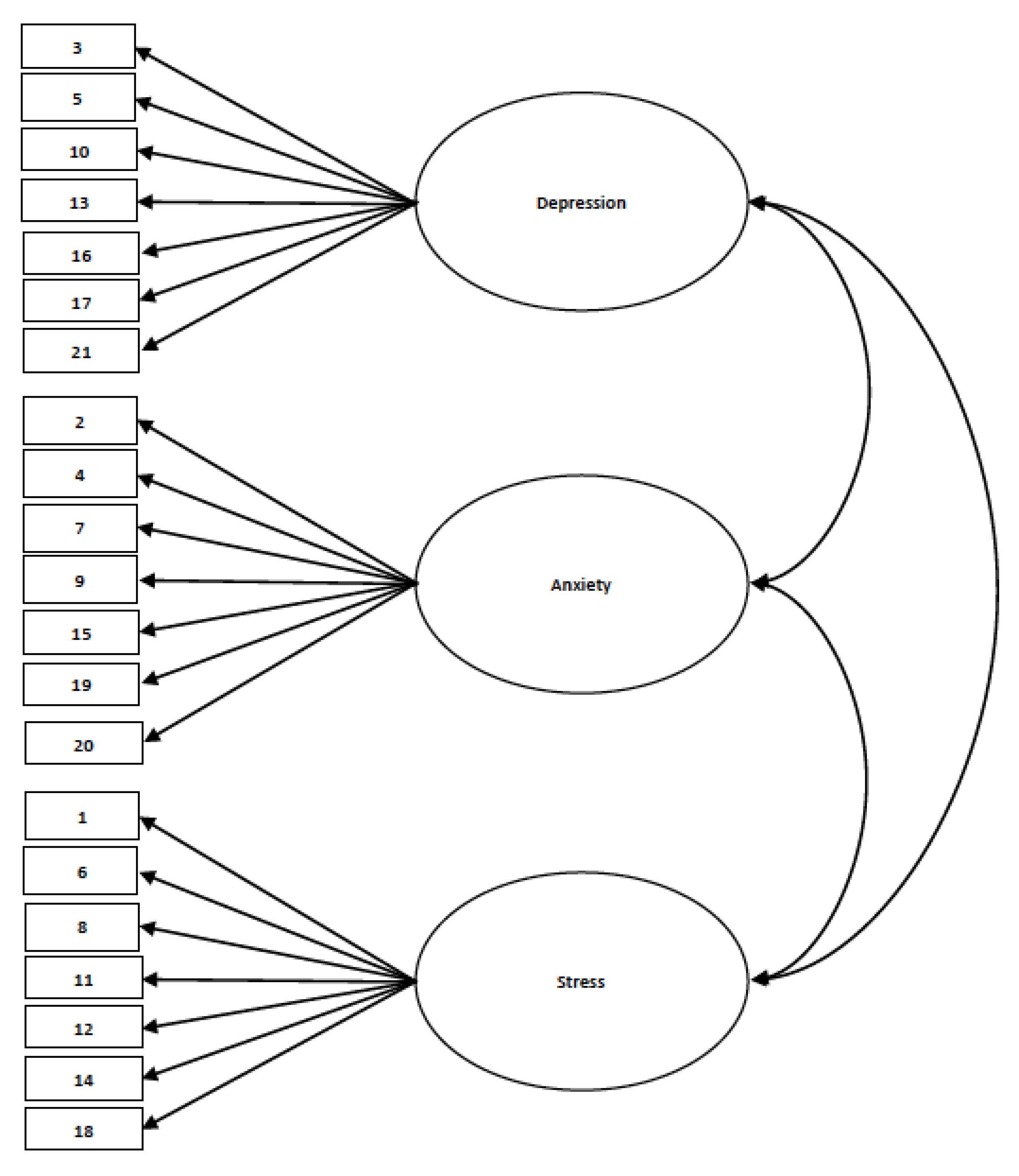
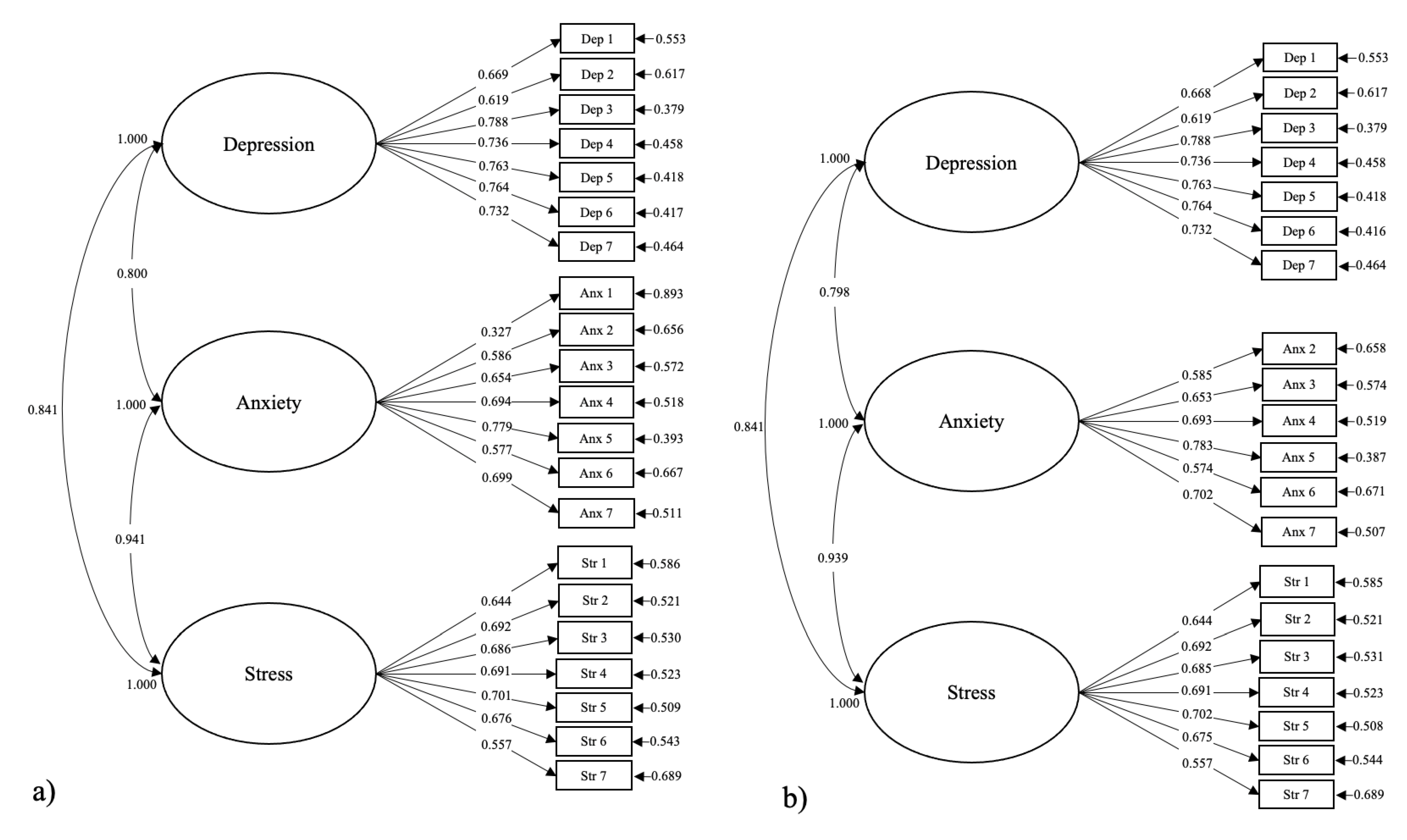
2.4.1. For Objective 1: Construct Validation and Reliability Test of DASS-21
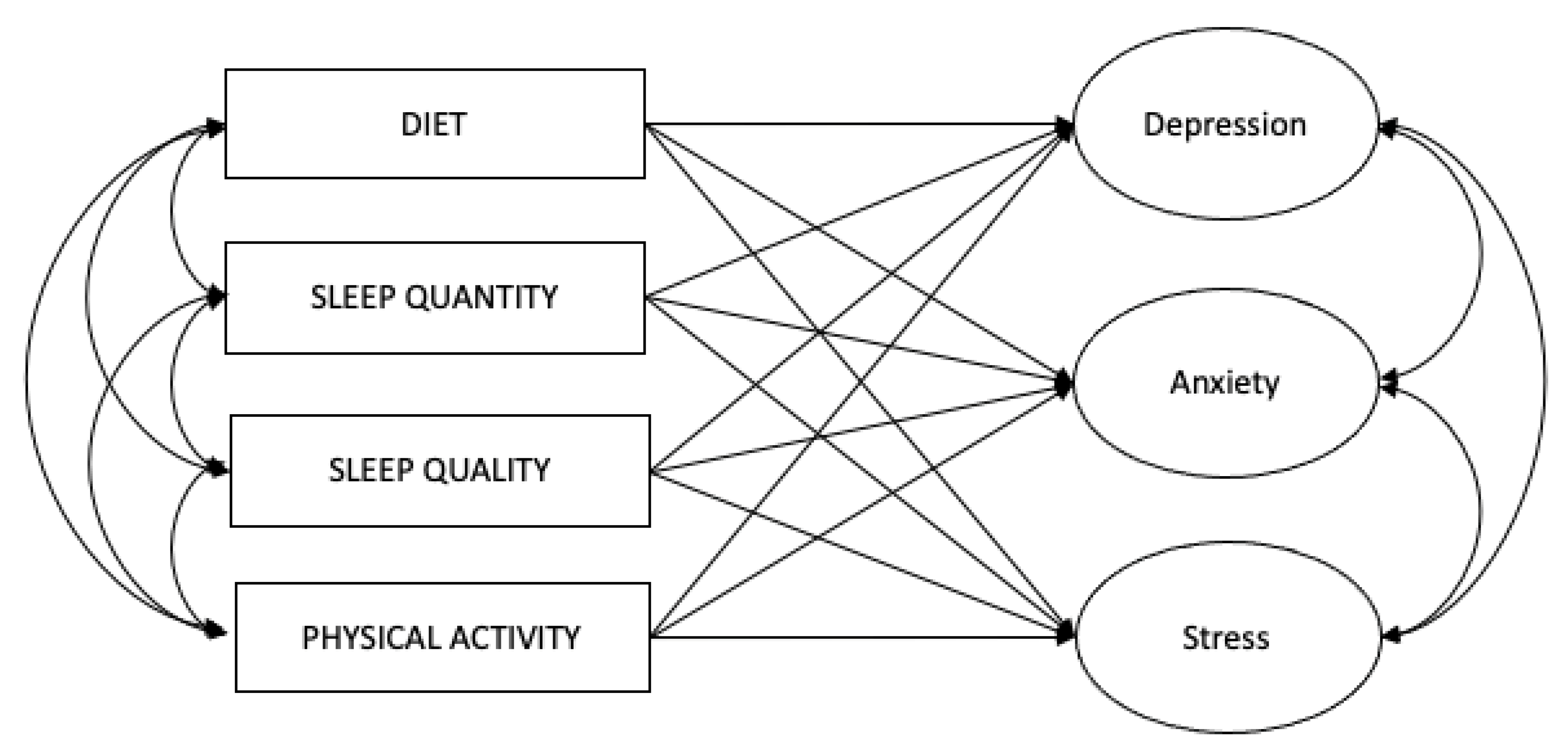
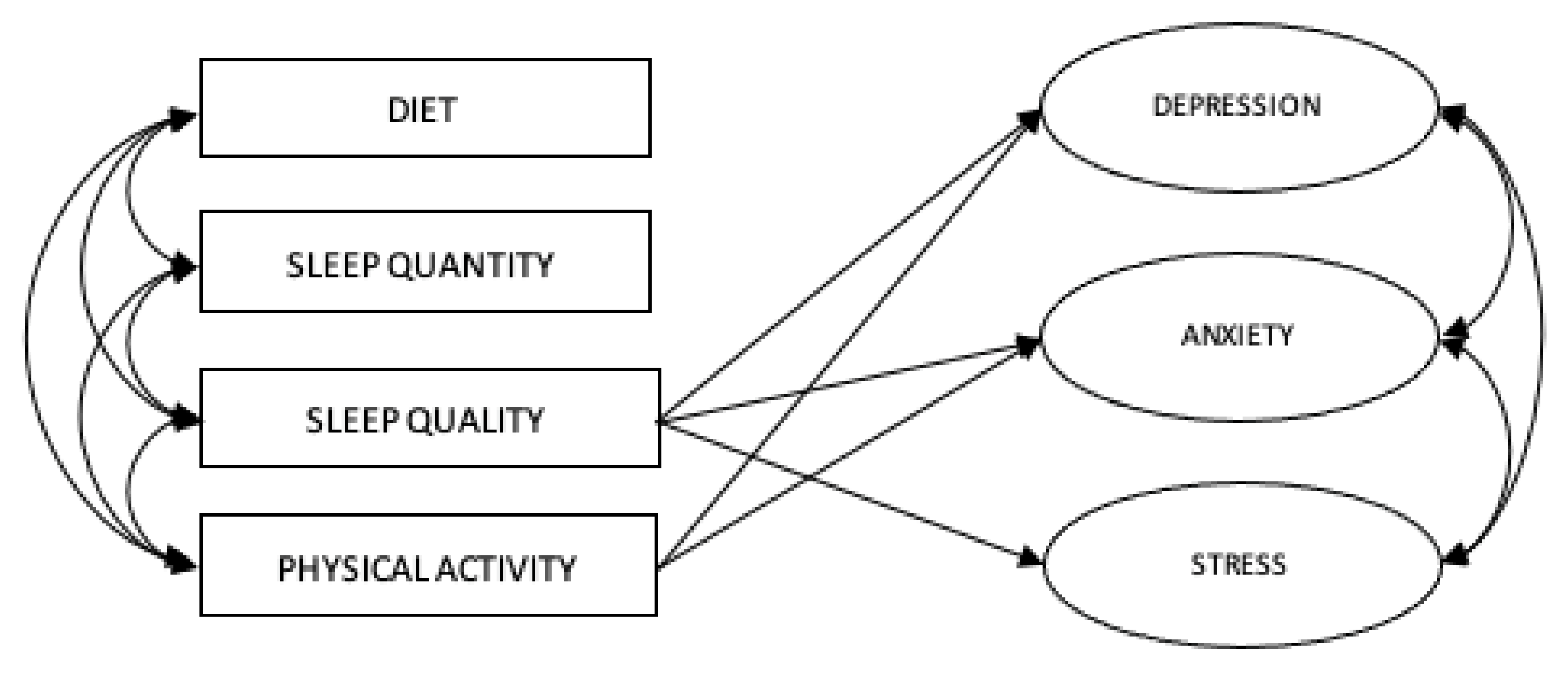
2.4.2. For Objective 2: Predicting Psychological Outcomes with Health-Related Variables
2.4.3. Adjustments for Missing Data
2.4.4. Adjustments for Non-Normal Data
3. Results
3.1. For Objective 1: Construct Validation and Reliability Test of DASS-21
3.2. For Objective 2: Predicting Psychological Outcomes with Health-Related Variables
4. Discussion
4.1. Objective 1: Construct Validation and Reliability Test of DASS-21
4.2. Objective 2: Predicting Psychological Outcomes with Health-Related Variables
4.2.1. Sleep Quality and Mental Health
4.2.2. Physical Activity and Mental Health
4.2.3. Other Non-Significant Predictors
4.2.4. Other Factors
4.3. Limitations
4.4. Suggestions for Future Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Mental Health Disorders Affect One in Four People. In World Health Report 2001. 2001. Available online: https://www.who.int/news-room/detail/28-09-2001-the-world-health-report-2001-mental-disorders-affect-one-in-four-people (accessed on 19 February 2024).
- World Health Organization. World Mental Health Report: Transforming Mental Health for All. 2022. Available online: https://iris.who.int/bitstream/handle/10665/356119/9789240049338-eng.pdf?sequence=1 (accessed on 19 February 2024).
- Institute for Health Metrics and Evaluation. Findings from the Global Burden of Disease Study 2017. 2018. Available online: https://www.healthdata.org/sites/default/files/files/policy_report/2019/GBD_2017_Booklet.pdf (accessed on 19 February 2024).
- American Foundation for Suicide Prevention. Risk Factors, Protective Factors, and Warning Signs. 2024. Available online: https://afsp.org/risk-factors-protective-factors-and-warning-signs/ (accessed on 19 February 2024).
- American Psychological Association. Psychology Topics: Stress. 2019. Available online: https://www.apa.org/topics/stress (accessed on 19 February 2024).
- American Psychological Association. Stress. 2018. Available online: https://dictionary.apa.org/stress (accessed on 19 February 2024).
- Mayo Clinic. Chronic Stress Puts Your Health at Risk. 2021. Available online: https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/stress/art-20046037 (accessed on 19 February 2024).
- Farreras, I.G. History of mental illness. In Noba Textbook Series: Psychology; Biswas-Diener, R., Diener, E., Eds.; DEF Publishers: Champaign, IL, USA, 2019; Available online: http://noba.to/65w3s7ex (accessed on 19 February 2024).
- Mullins, N.; Lewis, C.M. Genetics of Depression: Progress at Last. Curr. Psychiatry Rep. 2017, 19, 43. [Google Scholar] [CrossRef] [PubMed]
- Faravelli, C.; Scarpato, M.A.; Castellini, G.; Sauro, C.L. Gender differences in depression and anxiety: The role of age. Psychiatry Res. 2013, 210, 1301–1303. [Google Scholar] [CrossRef]
- Zhao, K.-X.; Huang, C.-Q.; Xiao, Q.; Gao, Y.; Liu, Q.-X.; Wang, Z.-R.; Li, Y.-H.; Xie, Y.-Z. Age and risk for depression among the elderly: A meta-analysis of the published literature. CNS Spectrums 2012, 17, 142–154. [Google Scholar] [CrossRef] [PubMed]
- Gravely-Witte, S.; Stewart, D.E.; Suskin, N.; Grace, S.L. The association among depressive symptoms, smoking status and antidepressant use in cardiac outpatients. J. Behav. Med. 2009, 32, 478–490. [Google Scholar] [CrossRef][Green Version]
- Pavkovic, B.; Zaric, M.; Markovic, M.; Klacar, M.; Huljic, A.; Caricic, A. Double screening for dual disorder, alcoholism and depression. Psychiatry Res. 2018, 270, 483–489. [Google Scholar] [CrossRef]
- Li, L.; Wu, C.; Gan, Y.; Qu, X.; Lu, Z. Insomnia and the risk of depression: A meta-analysis of prospective cohort studies. BMC Psychiatry 2016, 16, 375. [Google Scholar] [CrossRef]
- Caspi, A.; Sugden, K.; Moffitt, T.E.; Taylor, A.; Craig, I.W.; Harrington, H.; McClay, J.; Mill, J.; Martin, J.; Braithwaite, A.; et al. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science 2003, 301, 386–389. [Google Scholar] [CrossRef] [PubMed]
- Gibb, B.E. Depression in children. In Handbook of Depression, 3rd ed.; Gotlib, I.H., Hammen, C.L., Eds.; Guildford Press: New York, NY, USA, 2014; pp. 374–390. [Google Scholar]
- McLeod, B.D.; Weisz, J.R.; Wood, J.J. Examining the association between parenting and childhood depression: A meta-analysis. Clin. Psychol. Rev. 2007, 27, 986–1003. [Google Scholar] [CrossRef]
- Yap, M.B.H.; Jorm, A.F. Parental factors associated with childhood anxiety, depression, and internalizing problems: A systematic review and meta-analysis. J. Affect. Disord. 2015, 175, 424–440. [Google Scholar] [CrossRef]
- Ryder, A.G.; Sun, J.; Zhu, X.; Yao, S.; Chentsova-Dutton, Y.E. Depression in China: Integrating Developmental Psychopathology and Cultural-Clinical Psychology. J. Clin. Child Adolesc. Psychol. 2012, 41, 682–694. [Google Scholar] [CrossRef]
- Eley, T.C. Contributions of behavioral genetics research: Quantifying genetic, shared environmental, and nonshared environmental influences. In The Developmental Psychopathology of Anxiety; Vasey., M.W., Dadds, M.R., Eds.; Oxford University Press: London, UK, 2001; pp. 45–49. [Google Scholar]
- Gregory, A.M.; Eley, T.C. The genetic basis of child and adolescent anxiety. In Anxiety Disorders in Children and Adolescents: Research, Assessment, and Intervention, 2nd ed.; Silverman, W.K., Fields, A., Eds.; Cambridge University Press: Cambridge, UK, 2011; pp. 161–178. [Google Scholar]
- Gordon, J.A.; Hen, R. Genetic approaches to the study of anxiety. Annu. Rev. Neurosci. 2004, 27, 193–222. [Google Scholar] [CrossRef] [PubMed]
- Fox, N.A.; Nichols, K.E.; Henderson, H.A.; Rubin, K.; Schmidt, L.; Hamer, D.; Ernst, M.; Pine, D.S. Evidence for a gene-environment interaction in predicting behavioral inhibition in middle childhood. Psychol. Sci. 2005, 16, 921–926. [Google Scholar] [CrossRef] [PubMed]
- Biederman, J.; Rosenbaum, J.F.; Hirshfeld, D.R.; Faraone, S.V.; Bolduc, E.A.; Gersten, M.; Meminger, S.R.; Kagan, J.; Snidman, N.; Reznick, J.S. Psychiatric correlates of behavioral inhibition in young children of parents with and without psychiatric disorders. Arch. Gen. Psychiatry 1990, 47, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Biederman, J.; Rosenbaum, J.F.; Bolduc-Murphy, E.A.; Faraone, S.V.; Chaloff, J.; Hirshfeld, D.R.; Kagan, J. behavioral inhibition as a temperamental risk factor for anxiety disorders. Child Adolesc. Psychiatr. Clin. N. Am. 1993, 2, 667–684. [Google Scholar] [CrossRef]
- Kagan, J.; Reznick, J.S.; Snidman, N. The physiology and psychology of behavioral inhibition. Child Dev. 1987, 58, 1459–1473. Available online: https://www.jstor.org/stable/pdf/1130685.pdf?refreqid=excelsior%3A1f55ad7493810175c7e8d03eb194c2fe (accessed on 19 February 2024). [CrossRef] [PubMed]
- Kagan, J.; Reznick, J.S.; Snidman, N. Biological Bases of Childhood Shyness. Science 1988, 240, 167–171. [Google Scholar] [CrossRef]
- Kagan, J.; Reznick, J.S.; Gibbons, J. Inhibited and uninhibited types of children. Child Dev. 1989, 60, 838–845. Available online: https://www.jstor.org/stable/pdf/1131025.pdf?refreqid=excelsior%3A4e886fad067acb091f9d1c0f14a93076 (accessed on 19 February 2024). [CrossRef] [PubMed]
- Lonigan, C.J.; Phillips, B.M.; Wilson, S.B.; Allan, N.P. Temperament and anxiety in children and adolescents. In Anxiety Disorders in Children and Adolescents: Research, Assessment, and Intervention, 2nd ed.; Silverman, W.K., Fields, A., Eds.; Cambridge University Press: Cambridge, UK, 2011; pp. 198–226. [Google Scholar]
- Wolpe, J.; Rachman, S. Psychoanalytic “evidence”: A critique based on Freud’s case of Little Hans. J. Nerv. Ment. Dis. 1960, 131, 135–148. [Google Scholar] [CrossRef] [PubMed]
- Gray, J.A.; McNaughton, N. The Neuropsychology of Anxiety, 2nd ed.; Oxford University Press: New York, NY, USA, 2000. [Google Scholar]
- Davis, M. Are different parts of the extended amygdala involved in fear versus anxiety? Biol. Psychiatry 1998, 44, 1239–1247. [Google Scholar] [CrossRef]
- LeDoux, J.E. Emotion circuits in the brain. Annu. Rev. Neurosci. 2000, 23, 155–184. [Google Scholar] [CrossRef]
- Beidel, D.C. Determining the reliability of psychophysiological assessment in childhood anxiety. J. Anxiety Disord. 1991, 5, 139–150. [Google Scholar] [CrossRef]
- Carrion, V.G.; Weems, C.F.; Ray, R.D.; Glaser, B.; Hessl, D.; Reiss, A.L. Diurnal salivary cortisol in pediatric posttraumatic stress disorder. Biol. Psychiatry 2002, 51, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Field, A.P.; Hadwin, J.A.; Lester, K.J. Information processing biases in child and adolescent anxiety: A developmental perspective. In Anxiety Disorders in Children and Adolescents: Research, Assessment, and Intervention, 2nd ed.; Silverman, W.K., Fields, A., Eds.; Cambridge University Press: Cambridge, UK, 2011; pp. 103–128. [Google Scholar]
- Vasey, M.W.; MacLeod, C. Information-processing factors in childhood anxiety: A review and developmental perspective. In The Developmental Psychopathology of Anxiety; Vasey, M.W., Dadds, M.R., Eds.; Oxford University Press: London, UK, 2001; pp. 253–277. [Google Scholar]
- Weems, C.F.; Watts, S.E. Cognitive models of childhood anxiety. In Anxiety Disorder Research; Velotis, C.M., Ed.; Nova Science Publishers, Inc.: Hauppauge, NY, USA, 2005; pp. 205–232. [Google Scholar]
- Weisz, J.R.; Suwanlert, S.; Chaiyasit, W.; Walter, B.R. Over- and under-controlled referral problems among children and adolescents from Thailand and the United States: The Wat and Wai of cultural differences. J. Consult. Clin. Psychol. 1987, 55, 719–726. [Google Scholar] [CrossRef] [PubMed]
- Varela, R.E.; Vernberg, E.M.; Sanchez-Sosa, J.J.; Riveros, A.; Mitchell, M.; Mashunkashey, J. Anxiety Reporting and Culturally Associated Interpretation Biases and Cognitive Schemas: A Comparison of Mexican, Mexican American, and European American Families. J. Clin. Child Adolesc. Psychol. 2004, 33, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Varela, R.E.; Vernberg, E.M.; Sanchez-Sosa, J.J.; Riveros, A.; Mitchell, M.; Mashunkashey, J. Parenting practices of Mexican, Mexican American, and European American families: Social context and cultural influences. J. Fam. Psychol. 2004, 18, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Silverman, W.K.; Carter, R. Anxiety disturbance in girls and women. In Handbook of Girls’ and Women’s Psychological Health; Worell, J., Goodheart, C., Eds.; Oxford University Press: New York, NY, USA, 2006; pp. 60–68. [Google Scholar]
- Costello, E.J.; Egger, H.L.; Angold, A. Developmental epidemiology of anxiety disorders. In Phobic and Anxiety Disorders in Children and Adolescents: A Clinician’s Guide to Effective Psychosocial and Pharmacological Interventions; Ollendick, T.H., March, J.S., Eds.; Oxford University Press: New York, NY, USA, 2004; pp. 61–91. [Google Scholar] [CrossRef]
- Ginsburg, G.S.; Silverman, W.K. Gender role orientation and fearfulness in children with anxiety disorders. J. Anxiety Disord. 2000, 14, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Ollendick, T.H.; King, N.J.; Frary, R.B. Fears in children and adolescents: Reliability and generalizability across gender, age and nationality. Behav. Res. Ther. 1989, 27, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Ollendick, T.H.; Langley, A.K.; Jones, R.T.; Kephart, C. Fear in children and adolescents: Relations with negative life events, attributional style, and avoidant coping. J. Child Psychol. Psychiatry 2001, 42, 1029–1034. [Google Scholar] [CrossRef] [PubMed]
- Melchior, M.; Caspi, A.; Milne, B.J.; Danese, A.; Poulton, R.; Moffitt, T.E. Work stress precipitates depression and anxiety in young, working women and men. Psychol. Med. 2007, 37, 1119–1129. [Google Scholar] [CrossRef]
- Calkins, A.W.; Otto, M.W.; Cohen, L.S.; Soares, C.N.; Vitonis, A.F.; Hearon, B.A.; Harlow, B.L. Psychosocial predictors of the onset of anxiety disorders in women: Results from a prospective 3-year longitudinal study. J. Anxiety Disord. 2009, 23, 1165–1169. [Google Scholar] [CrossRef][Green Version]
- Ediz, B.; Ozcakir, A.; Bilgel, N. Depression and anxiety among medical students: Examining scores of the Beck Depression and Anxiety Inventory and the Depression Anxiety and Stress Scale with Student Characteristics. Cogent Psychol. 2017, 4, 1283829. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety Stress Scale, 4th ed.; Psychology Foundation Monograph: Sydney, Australia, 2004. Original work published 1995. [Google Scholar]
- Tran, T.D.; Tran, T.; Fisher, J. Validation of the depression anxiety stress scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC Psychiatry 2013, 13, 24. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım, A.; Boysan, M.; Kefeli, M.C. Psychometric properties of the Turkish version of the Depression Anxiety Stress Scale-21 (DASS-21). Br. J. Guid. Couns. 2018, 46, 582–595. [Google Scholar] [CrossRef]
- Akin, A.; Cetin, B. The Depression Anxiety and Stress Scale (DASS): The study of validity and reliability. Educ. Sci. Theory Pract. 2007, 7, 260–268. [Google Scholar]
- Pezirkianidis, C.; Karakasidou, E.; Lakioti, A.; Stalikas, A.; Galanakis, M. Psychometric properties of the depression, anxiety, stress scales-21 (DASS-21) in a Greek sample. Psychology 2018, 9, 2933–2950. [Google Scholar] [CrossRef]
- Wang, K.; Shi, H.-S.; Geng, F.-L.; Zou, L.-Q.; Tan, S.-P.; Wang, Y.; Neumann, D.L.; Shum, D.H.K.; Chan, R.C.K. Cross-cultural validation of the Depression Anxiety Stress Scale–21 in China. Psychol. Assess. 2016, 28, e88–e100. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.C.; Xu, T.; Huang, J.; Wang, Y.; Zhao, Q.; Shum, D.H.; O’gorman, J.; Potangaroa, R. Extending the utility of the Depression Anxiety Stress scale by examining its psychometric properties in Chinese settings. Psychiatry Res. 2012, 200, 879–883. [Google Scholar] [CrossRef] [PubMed]
- Vignola, R.C.B.; Tucci, A.M. Adaptation and validation of the depression, anxiety and stress scale (DASS) to Brazilian Portuguese. J. Affect. Disord. 2014, 155, 104–109. [Google Scholar] [CrossRef]
- Bottesi, G.; Ghisi, M.; Altoè, G.; Conforti, E.; Melli, G.; Sica, C. The Italian version of the Depression Anxiety Stress Scales-21: Factor structure and psychometric properties on community and clinical samples. Compr. Psychiatry 2015, 60, 170–181. [Google Scholar] [CrossRef]
- Musa, R.; Ramli, R.; Abdullah, K.; Sarkarsi, R. Concurrent validity of the depression and anxiety in the Bahasa Malaysia version of the Depression Anxiety and Stress Scales (DASS). ASEAN J. Psychiatry 2011, 12. Available online: https://www.aseanjournalofpsychiatry.org/articles/concurrent-validity-of-the-depression-and-anxiety-components-in-the-bahasa-malaysia-version-of-the-depression-anxiety-an.pdf (accessed on 19 February 2024).
- Norton, P.J. Depression Anxiety and Stress Scales (DASS-21): Psychometric analysis across four racial groups. Anxiety, Stress. Coping 2007, 20, 253–265. [Google Scholar] [CrossRef] [PubMed]
- Gomez, R. Depression Anxiety Stress Scales: Factor structure and differential item functioning across women and men. Pers. Individ. Differ. 2013, 54, 687–691. [Google Scholar] [CrossRef]
- Page, A.C.; Hooke, G.R.; Morrison, D.L. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in depressed clinical samples. Br. J. Clin. Psychol. 2007, 46, 283–297. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.R.; Henry, J.D. The Depression Anxiety Stress Scales (DASS): Normative data and latent structure in a large non-clinical sample. Br. J. Clin. Psychol. 2003, 42, 111–131. [Google Scholar] [CrossRef] [PubMed]
- Szabó, M. The short version of the Depression Anxiety Stress Scales (DASS-21): Factor structure in a young adolescent sample. J. Adolesc. 2010, 33, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Le, M.T.H.; Tran, T.D.; Holton, S.; Nguyen, H.T.; Wolfe, R.; Fisher, J. Reliability, convergent validity and factor structure of the DASS-21 in a sample of Vietnamese adolescents. PLoS ONE 2017, 12, e0180557. [Google Scholar] [CrossRef] [PubMed]
- Shaw, T.; Campbell, M.; Runions, K.; Zubrick, S.R. Properties of the DASS-21 in an Australian community adolescent population. J. Clin. Psychol. 2017, 73, 879–892. [Google Scholar] [CrossRef] [PubMed]
- Steinmo, S.; Hagger-Johnson, G.; Shahab, L. Bidirectional association between mental health and physical activity in older adults: Whitehall II prospective cohort study. Prev. Med. 2014, 66, 74–79. [Google Scholar] [CrossRef]
- Buchan, M.C.; Romano, I.; Butler, A.; Laxer, R.E.; Patte, K.A.; Leatherdale, S.T. Bi-directional relationships between physical activity and mental health among a large sample of Canadian youth: A sex-stratified analysis of students in the COMPASS study. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 132. [Google Scholar] [CrossRef]
- Li, Y.; Lv, M.-R.; Wei, Y.-J.; Sun, L.; Zhang, J.-X.; Zhang, H.-G.; Li, B. Dietary patterns and depression risk: A meta-analysis. Psychiatry Res. 2017, 253, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Richard, A.; Rohrmann, S.; Vandeleur, C.L.; Mohler-Kuo, M.; Eichholzer, M. Associations between fruit and vegetable consumption and psychological distress: Results from a population-based study. BMC Psychiatry 2015, 15, 213. [Google Scholar] [CrossRef] [PubMed]
- Jacka, F.N.; Pasco, J.A.; Mykletun, A.; Williams, L.J.; Hodge, A.M.; O’Reilly, S.L.; Nicholson, G.C.; Kotowicz, M.A.; Berk, M. Association of western and traditional diets with depression and anxiety in women. Am. J. Psychiatry 2010, 167, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Jacka, F.N.; Cherbuin, N.; Anstey, K.J.; Sachdev, P.; Butterworth, P. Western diet is associated with a smaller hippocampus: A longitudinal investigation. BMC Med. 2015, 13, 215. [Google Scholar] [CrossRef] [PubMed]
- Roohafza, H.; Sarrafzadegan, N.; Sadeghi, M.; Rafieian-Kopaei, M.; Sajjadi, F.; Khosravi-Boroujeni, H. The association between stress levels and food consumption among Iranian population. Arch. Iran. Med. 2013, 16, 145–148. [Google Scholar] [PubMed]
- Baglioni, C.; Battagliese, G.; Feige, B.; Spiegelhalder, K.; Nissen, C.; Voderholzer, U.; Lombardo, C.; Riemann, D.; Baglioni, C.; Battagliese, G.; et al. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 2011, 135, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Dinis, J.; Bragança, M. Quality of sleep and depression in college students: A systematic review. Sleep Sci. 2018, 11, 290–301. [Google Scholar] [CrossRef]
- Ojio, Y.; Nishida, A.; Shimodera, S.; Togo, F.; Sasaki, T. Sleep duration associated with the lowest risk of depression/anxiety in adolescents. Sleep 2016, 39, 1555–1562. [Google Scholar] [CrossRef] [PubMed]
- Teker, A.G.; Luleci, N.E. Sleep Quality and Anxiety Level in Employees. North. Clin. Istanb. 2018, 5, 31–36. [Google Scholar] [CrossRef]
- Oh, C.-M.; Kim, H.Y.; Na, H.K.; Cho, K.H.; Chu, M.K. The effect of anxiety and depression on sleep quality of individuals with high risk for insomnia: A population-based study. Front. Neurol. 2019, 10, 849. [Google Scholar] [CrossRef]
- Prather, A.A.; Puterman, E.; Epel, E.S.; Dhabhar, F.S. Poor sleep quality potentiates stress-induced cytokine reactivity in postmenopausal women with high visceral abdominal adiposity. Brain Behav. Immun. 2014, 35, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Almojali, A.I.; Almalki, S.A.; Alothman, A.S.; Masuadi, E.M.; Alaqeel, M.K. The prevalence and association of stress with sleep quality among medical students. J. Epidemiol. Glob. Health 2017, 7, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Dunn, A.L.; Trivedi, M.H.; O’neal, H. Physical activity dose-response effects on outcomes of depression and anxiety. Med. Sci. Sports Exerc. 2001, 33, S587–S597. [Google Scholar] [CrossRef] [PubMed]
- McKercher, C.M.; Schmidt, M.D.; Sanderson, K.A.; Patton, G.C.; Dwyer, T.; Venn, A.J. Physical Activity and Depression in Young Adults. Am. J. Prev. Med. 2009, 36, 161–164. [Google Scholar] [CrossRef] [PubMed]
- De Mello, M.T.; Lemos, V.d.A.; Antunes, H.K.M.; Bittencourt, L.; Santos-Silva, R.; Tufik, S. Relationship between physical activity and depression and anxiety symptoms: A population study. J. Affect. Disord. 2013, 149, 241–246. [Google Scholar] [CrossRef]
- Mochcovitch, M.D.; Deslandes, A.C.; Freire, R.C.; Garcia, R.F.; Nardi, A.E. The effects of regular physical activity on anxiety symptoms in healthy older adults: A systematic review. Rev. Bras. Psiquiatr. 2016, 38, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Salmon, P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: A unifying theory. Clin. Psychol. Rev. 2001, 21, 33–61. [Google Scholar] [CrossRef] [PubMed]
- Aldana, S.G.; Sutton, L.D.; Jacobson, B.H.; Quirk, M.G. Relationships between leisure time physical activity and perceived stress. Percept. Mot. Ski. 1996, 82, 315–321. [Google Scholar] [CrossRef]
- Myers, N.D.; Ahn, S.; Jin, Y. Sample Size and Power Estimates for a Confirmatory Factor Analytic Model in Exercise and Sport. Res. Q. Exerc. Sport 2011, 82, 412–423. [Google Scholar] [CrossRef]
- Behavioral Risk Factor Surveillance System. Behavioral Risk Factor Surveillance System Questionnaire [PDF File]. 2012. Available online: https://www.cdc.gov/brfss/questionnaires/pdf-ques/2013-BRFSS_English.pdf (accessed on 19 February 2024).
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Jackson, A.S.; Blair, S.N.; Mahar, M.T.; Wier, L.T.; Ross, R.M.; Stuteville, J.E. Prediction of functional aerobic capacity without exercise testing. Med. Sci. Sports Exerc. 1990, 22, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Muthén, L.K.; Muthén, B.O. Mplus: Statistical Analysis with Latent Variables: User’s Guide (Version 8.4); Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, version 26.0; IBM Corp.: Armonk, NY, USA, 2019. [Google Scholar]
- Cohen, J.; Cohen, P. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences, 3rd ed.; Routledge: Boca Raton, FL, USA, 2003; pp. 23–28. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Evaluating model fit: A synthesis of the structural equation modelling literature. In Proceedings of the 7th European Conference on Research Methodology for Business and Management Studies, London, UK, 18–20 June 2008; pp. 195–200. [Google Scholar] [CrossRef]
- Cronbach, L.J. Coefficient alpha and internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Schafer, J.L.; Graham, J.W. Missing data: Our view of the state of the art. Psychol. Methods 2002, 7, 147–177. [Google Scholar] [CrossRef] [PubMed]
- Langkamp, D.L.; Lehman, A.; Lemeshow, S. Techniques for handling missing data in secondary analyses of large surveys. Acad. Pediatr. 2010, 10, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Efron, B.; Tibshirani, R. An introduction to the Bootstrap. In Chapman and Hall/CRC eBooks; Taylor & Francis Ltd.: London, UK, 1994. [Google Scholar]
- Antony, M.M.; Bieling, P.J.; Cox, B.J.; Enns, M.W.; Swinson, R.P. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scale in clinical groups and a community sample. Psychol. Assess. 1998, 10, 176. [Google Scholar] [CrossRef]
- Rezaei, M.; Khormali, M.; Akbarpour, S.; Sadeghniiat-Hagighi, K.; Shamsipour, M. Sleep quality and its association with psychological distress and sleep hygiene: A cross-sectional study among pre-clinical medical students. Sleep Sci. 2018, 11, 274–280. [Google Scholar] [CrossRef] [PubMed]
- O’leary, K.; Bylsma, L.M.; Rottenberg, J. Why might poor sleep quality lead to depression? A role for emotion regulation. Cogn. Emot. 2017, 31, 1698–1706. [Google Scholar] [CrossRef] [PubMed]
- Lindwall, M.; Gerber, M.; Jonsdottir, I.H.; Börjesson, M.; Ahlborg, G. The relationships of change in physical activity with change in depression, anxiety, and burnout: A longitudinal study of Swedish healthcare workers. Health Psychol. 2014, 33, 1309–1318. [Google Scholar] [CrossRef]
- Sarbadhikari, S.N.; Saha, A.K. Moderate exercise and chronic stress produce counteractive effects on different areas of the brain by acting through various neurotransmitter receptor subtypes: A hypothesis. Theor. Biol. Med. Model. 2006, 3, 33. [Google Scholar] [CrossRef]
- Pilcher, J.J.; Ginter, D.R.; Sadowsky, B. Sleep quality versus sleep quantity: Relationships between sleep and measures of health, well-being and sleepiness in college students. J. Psychosom. Res. 1997, 42, 583–596. [Google Scholar] [CrossRef] [PubMed]
- Bassett, S.M.; Lupis, S.B.; Gianferante, D.; Rohleder, N.; Wolf, J.M. Sleep quality but not sleep quantity effects on cortisol responses to acute psychosocial stress. Stress 2015, 18, 638–644. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, V.; Gupta, R.; Grover, S.; Basu, A.; Tripathi, A.; Subramanyam, A.; Nischal, A.; Hussain, A.; Mehra, A.; Ambekar, A.; et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J. Psychiatry 2020, 62, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Marelli, S.; Castelnuovo, A.; Somma, A.; Castronovo, V.; Mombelli, S.; Bottoni, D.; Leitner, C.; Fossati, A.; Ferini-Strambi, L. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J. Neurol. 2020, 268, 8–15. [Google Scholar] [CrossRef]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef]
| Year | 2017 | 2018 | 2019 | Total | |
|---|---|---|---|---|---|
| Participants | 284 | 230 | 212 | 726 | |
| Average Age | 21.73 ± 2.3 | 21.43 ± 2.04 | 22.06 ± 2.56 | 21.7 ± 2.3 | |
| Gender by Frequency (%) | Male: | n = 129, 45.4% | n = 109, 47.4% | n = 91, 42.9% | n = 329, 45.3% |
| Female: | n = 155, 54.6% | n = 121, 54.6% | n = 121, 57.1% | n = 397, 54.7% | |
| Ethnicities by Frequency (%) | Asian: | 43.3% | 43.5% | 49.5% | 45.2% |
| Native Hawaiian/ Other Pacific Islander: | 42.6% | 46.5% | 42.9% | 43.9% | |
| White: | 1.1% | 1.7% | 1.9% | 1.5% | |
| American Indian/Alaskan Native: | 0.4% | 1.3% | 0.5% | 0.7% | |
| African American: | 0.7% | 0.0% | 0.9% | 0.6% | |
| Missing: | 12% | 7% | 4.2% | 8.1% | |
| Model-Fit Indicators | Good Fit [95] | Acceptable Fit [96] | Model-Fit Values | |
|---|---|---|---|---|
| (a) All Items | (b) Without Item 2 | |||
| RMSEA | 0.00 < x < 0.06 | 0.06 < x < 0.08 | 0.073 | 0.076 |
| CFI | 0.95 < x < 1 | 0.90 < x < 0.95 | 0.901 | 0.902 |
| TLI | 0.95 < x < 1 | 0.80 < x < 0.95 | 0.889 | 0.889 |
| SRMR | x < 0.08 | x < 0.08 | 0.044 | 0.045 |
| Variables | N | Min | Max | Mean | SD | Skewness | Kurtosis |
|---|---|---|---|---|---|---|---|
| DIET | 504 | 0 | 9 | 5.42 | 1.47 | −0.470 | 1.167 |
| SLEEPQLT | 723 | 0 | 3 | 1.71 | 0.68 | −0.644 | 0.524 |
| SLEEPQTY | 719 | 1 | 13 | 6.19 | 1.40 | 0.129 | 1.727 |
| PARQ | 585 | 0 | 7 | 3.67 | 2.23 | 0.013 | −1.336 |
| AGE | 726 | 18 | 29 | 21.73 | 2.33 | 0.620 | 0.278 |
| GENDER | 726 | 1 | 2 | 1.55 | 0.50 | −0.189 | −1.970 |
| BMI | 690 | 14.18 | 62.03 | 27.32 | 6.64 | 1.296 | 2.728 |
| Predictors and Covariates | Depression (Latent) | Anxiety (Latent) | Stress (Latent) |
|---|---|---|---|
| Diet | −0.017 | 0.008 | −0.020 |
| Sleep Quality | −0.215 ** | −0.151 ** | −0.204 ** |
| Sleep Quantity | −0.013 | −0.041 | −0.070 |
| PARQ | −0.124 ** | −0.136 ** | −0.054 |
| Age | −0.058 | −0.075 | −0.057 |
| Gender | 0.041 | 0.148 ** | 0.190 ** |
| BMI | 0.029 | 0.007 | −0.015 |
| Standardized Estimates (β) | Two-Tailed p Value | |
|---|---|---|
| DEPRESSION ON | ||
| DIET | −0.015 | 0.744 |
| SLEEPQLT | −0.208 | 0.000 |
| SLEEPQTY | −0.011 | 0.780 |
| PARQ | −0.116 | 0.016 |
| GENDER | 0.039 | 0.349 |
| ANXIETY ON | ||
| DIET | 0.015 | 0.764 |
| SLEEPQLT | −0.143 | 0.002 |
| SLEEPQTY | −0.039 | 0.405 |
| PARQ | −0.127 | 0.007 |
| GENDER | 0.147 | 0.000 |
| STRESS ON | ||
| DIET | −0.015 | 0.743 |
| SLEEPQLT | −0.197 | 0.000 |
| SLEEPQTY | −0.067 | 0.112 |
| PARQ | −0.043 | 0.355 |
| GENDER | 0.193 | 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, R.H.; Paulino, Y.C.; Kawabata, Y. Validating Constructs of the Depression, Anxiety, and Stress Scale-21 and Exploring Health Indicators to Predict the Psychological Outcomes of Students Enrolled in the Pacific Islands Cohort of College Students. Int. J. Environ. Res. Public Health 2024, 21, 509. https://doi.org/10.3390/ijerph21040509
Kim RH, Paulino YC, Kawabata Y. Validating Constructs of the Depression, Anxiety, and Stress Scale-21 and Exploring Health Indicators to Predict the Psychological Outcomes of Students Enrolled in the Pacific Islands Cohort of College Students. International Journal of Environmental Research and Public Health. 2024; 21(4):509. https://doi.org/10.3390/ijerph21040509
Chicago/Turabian StyleKim, Rebecca H., Yvette C. Paulino, and Yoshito Kawabata. 2024. "Validating Constructs of the Depression, Anxiety, and Stress Scale-21 and Exploring Health Indicators to Predict the Psychological Outcomes of Students Enrolled in the Pacific Islands Cohort of College Students" International Journal of Environmental Research and Public Health 21, no. 4: 509. https://doi.org/10.3390/ijerph21040509
APA StyleKim, R. H., Paulino, Y. C., & Kawabata, Y. (2024). Validating Constructs of the Depression, Anxiety, and Stress Scale-21 and Exploring Health Indicators to Predict the Psychological Outcomes of Students Enrolled in the Pacific Islands Cohort of College Students. International Journal of Environmental Research and Public Health, 21(4), 509. https://doi.org/10.3390/ijerph21040509





