IEUBK Modeling of Children’s Blood Lead Levels in Homes Served by Private Domestic Wells in Three Illinois Counties
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Questionnaire
2.3. Blood Lead Level Modeling
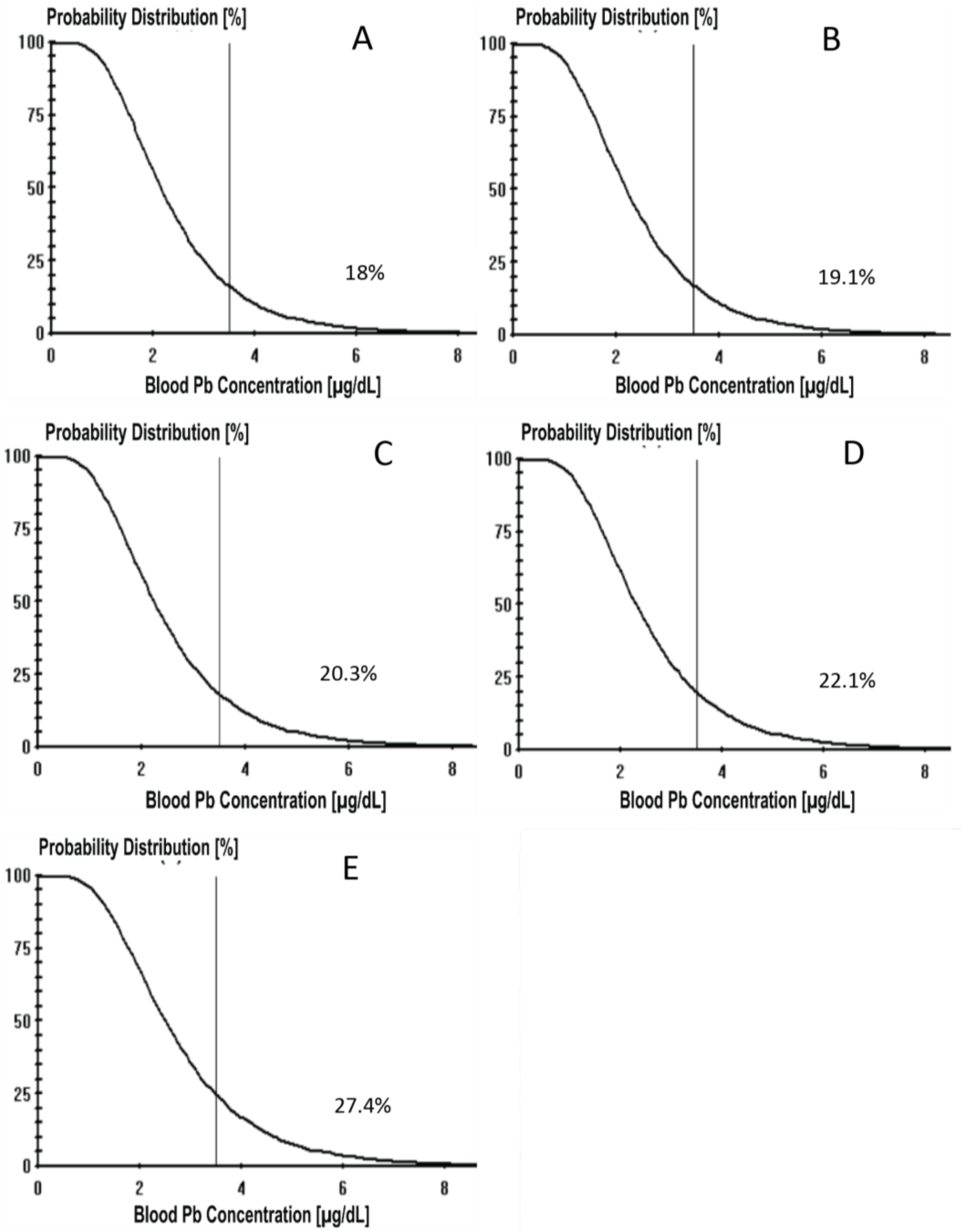
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, J.; Li, L.; Wang, Y.; Yan, C.; Liu, X. Impact of Low Blood Lead Concentrations on IQ and School Performance in Chinese Children. PLoS ONE 2013, 8, e65230. [Google Scholar] [CrossRef]
- Liu, J.; Liu, X.; Wang, W.; McCauley, L.; Pinto-Martin, J.; Wang, Y.; Li, L.; Yan, C.; Rogan, W.J. Blood Lead Concentrations and Children’s Behavioral and Emotional Problems: A Cohort Study. JAMA Pediatr. 2014, 168, 737. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services. National Toxicology Program. NTP monograph on health effects of low-level lead. NTP Monogr. 2012, xiii, xv-148. [Google Scholar]
- Min, J.-Y.; Min, K.-B.; Cho, S.-I.; Kim, R.; Sakong, J.; Paek, D. Neurobehavioral function in children with low blood lead concentrations. Neurotoxicology 2007, 28, 421–425. [Google Scholar] [CrossRef]
- Mason, L.H.; Harp, J.P.; Han, D.Y. Pb Neurotoxicity: Neuropsychological Effects of Lead Toxicity. BioMed Res. Int. 2014, 2014, 1–8. [Google Scholar] [CrossRef]
- Gleason, K.M.; Valeri, L.; Shankar, A.H.; Hasan, M.O.S.I.; Quamruzzaman, Q.; Rodrigues, E.G.; Christiani, D.C.; Wright, R.O.; Bellinger, D.C.; Mazumdar, M. Stunting is associated with blood lead concentration among Bangladeshi children aged 2-3 years. Environ. Health 2016, 15, 103. [Google Scholar] [CrossRef] [PubMed]
- Levallois, P.; St-Laurent, J.; Gauvin, D.; Courteau, M.; Prévost, M.; Campagna, C.; Lemieux, F.; Nour, S.; D’Amour, M.; Rasmussen, P.E. The impact of drinking water, indoor dust and paint on blood lead levels of children aged 1–5 years in Montréal (Québec, Canada). J. Expo. Sci. Environ. Epidemiol. 2014, 24, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, C.; Yard, E.; Dignam, T.; Buchanan, S.; Condon, S.; Brown, M.J.; Raymond, J.; Rogers, H.S.; Sarisky, J.; De Castro, R.; et al. Blood Lead Levels Among Children Aged <6 Years—Flint, Michigan, 2013–2016. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 650–654. [Google Scholar]
- U.S. EPA. Basic Information about Lead in Drinking Water. Available online: https://www.epa.gov/ground-water-and-drinking-water/basic-information-about-lead-drinking-water (accessed on 27 January 2023).
- US EPA. Lead and Copper Rule. 28 November 2023. Available online: https://www.epa.gov/dwreginfo/lead-and-copper-rule (accessed on 16 February 2024).
- Rhode Island Department of State. Private Drinking Water Systems (216-RICR-50-05-2.12). Available online: https://casetext.com/regulation/rhode-island-administrative-code/title-216-department-of-health/chapter-50-environmental-health/subchapter-05-water-quality/part-2-private-drinking-water-systems-216-ricr-50-05-2/section-216-ricr-50-05-212-mandatory-testing-requirements-for-private-water-supplies (accessed on 21 November 2023).
- Gibson, J.M.; Fisher, M.; Clonch, A.; MacDonald, J.M.; Cook, P.J. Children drinking private well water have higher blood lead than those with city water. Proc. Natl. Acad. Sci. USA 2020, 117, 16898–16907. [Google Scholar] [CrossRef] [PubMed]
- U.S. Census Bureau. American Housing Survey (AHS)—AHS Table Creator. Available online: https://www.census.gov/programs-surveys/ahs/data/interactive/ahstablecreator.html?s_areas=00000&s_year=2019&s_tablename=TABLE4&s_bygroup1=1&s_bygroup2=1&s_filtergroup1=1&s_filtergroup2=1&s_show=SO (accessed on 6 April 2022).
- Dieter, C.A.; Maupin, M.A.; Caldwell, R.R.; Harris, M.A.; Ivahnenko, T.I.; Lovelace, J.K.; Barber, N.L.; Linsey, K.S. Estimated Use of Water in the United States in 2015; U.S. Geological Survey: Reston, VA, USA, 2018; p. 76. [Google Scholar] [CrossRef]
- Johnson, T.D.; Belitz, K.; Lombard, M.A. Estimating domestic well locations and populations served in the contiguous U.S. for years 2000 and 2010. Sci. Total Environ. 2019, 687, 1261–1273. [Google Scholar] [CrossRef] [PubMed]
- Kamai, E.M.; Daniels, J.L.; Delamater, P.L.; Lanphear, B.P.; MacDonald Gibson, J.; Richardson, D.B. Patterns of Children’s Blood Lead Screening and Blood Lead Levels in North Carolina, 2011–2018—Who Is Tested, Who Is Missed? Environ. Health Perspect. 2022, 130, 067002. [Google Scholar] [CrossRef]
- Deshommes, E.; Laroche, L.; Nour, S.; Cartier, C.; Prévost, M. Source and occurrence of particulate lead in tap water. Water Res. 2010, 44, 3734–3744. [Google Scholar] [CrossRef] [PubMed]
- Hou, S.; Yuan, L.; Jin, P.; Ding, B.; Qin, N.; Li, L.; Liu, X.; Wu, Z.; Zhao, G.; Deng, Y. A clinical study of the effects of lead poisoning on the intelligence and neurobehavioral abilities of children. Theor. Biol. Med. Model 2013, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- Needleman, H.L.; Gunnoe, C.; Leviton, A.; Reed, R.; Peresie, H.; Maher, C.; Barrett, P. Deficits in Psychologic and Classroom Performance of Children with Elevated Dentine Lead Levels. N. Engl. J. Med. 1979, 300, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Miranda, M.L.; Kim, D.; Galeano, M.A.O.; Paul, C.J.; Hull, A.P.; Morgan, S.P. The Relationship between Early Childhood Blood Lead Levels and Performance on End-of-Grade Tests. Environ. Health Perspect. 2007, 115, 1242–1247. [Google Scholar] [CrossRef]
- Nicolescu, R.; Petcu, C.; Cordeanu, A.; Fabritius, K.; Schlumpf, M.; Krebs, R.; Krämer, U.; Winneke, G. Environmental exposure to lead, but not other neurotoxic metals, relates to core elements of ADHD in Romanian children: Performance and questionnaire data. Environ. Res. 2010, 110, 476–483. [Google Scholar] [CrossRef]
- Needleman, H.L.; Schell, A.; Bellinger, D.; Leviton, A.; Allred, E.N. The Long-Term Effects of Exposure to Low Doses of Lead in Childhood: An 11-Year Follow-up Report. N. Engl. J. Med. 1990, 322, 83–88. [Google Scholar] [CrossRef]
- Needleman, H.L. Lead at low dose and the behavior of children. Acta Psychiatr Scand. 1983, 67, 26–37. [Google Scholar] [CrossRef]
- Needleman, H.L.; McFarland, C.; Ness, R.B.; Fienberg, S.E.; Tobin, M.J. Bone lead levels in adjudicated delinquents: A case control study. Neurotoxicology Teratol. 2002, 24, 711–717. [Google Scholar] [CrossRef]
- Jakubowski, M. Low-level environmental lead exposure and intellectual impairment in children—The current concepts of risk assessment. Int. J. Occup. Med. Environ. Health 2011, 24, 1–7. [Google Scholar] [CrossRef]
- Long, A.S.; Hanlon, A.L.; Pellegrin, K.L. Socioeconomic variables explain rural disparities in US mortality rates: Implications for rural health research and policy. SSM Popul. Health 2018, 6, 72–74. [Google Scholar] [CrossRef]
- Geiger, S.D.; Bressler, J.; Kelly, W.; Jacobs, D.E.; Awadalla, S.S.; Hagston, B.; Onwuta, U.; Panier, C.; Dorevitch, S. Predictors of Water Lead Levels in Drinking Water of Homes With Domestic Wells in 3 Illinois Counties. J. Public Health Manag. Pract. 2021, 27, 567–576. [Google Scholar] [CrossRef]
- US EPA R 08. Lead and Copper-Suggested Directions for Homeowner Tap Sample Collection Procedures. 29 May 2019. Available online: https://www.epa.gov/region8-waterops/lead-and-copper-suggested-directions-homeowner-tap-sample-collection-procedures (accessed on 10 July 2023).
- Erinosho, T.O.; Pinard, C.A.; Nebeling, L.C.; Moser, R.P.; Shaikh, A.R.; Resnicow, K.; Oh, A.Y.; Yaroch, A.L. Development and Implementation of the National Cancer Institute’s Food Attitudes and Behaviors Survey to Assess Correlates of Fruit and Vegetable Intake in Adults. PLoS ONE 2015, 10, e0115017. [Google Scholar] [CrossRef] [PubMed]
- Hargrove, W.; Juárez-Carillo, P.; Korc, M. Healthy Vinton: A Health Impact Assessment Focused on Water and Sanitation in a Small Rural Town on the U.S.-Mexico Border. Int. J. Environ. Res. Public Health 2015, 12, 3864–3888. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.Q.; Dewey, C.E.; Doré, K.; Majowicz, S.E.; McEwen, S.A.; David, W.-T.; Eric, M.; Carr, D.J.; Henson, S.J. Public perceptions of drinking water: A postal survey of residents with private water supplies. BMC Public Health 2006, 6, 94. [Google Scholar] [CrossRef] [PubMed]
- McLeod, L.; Bharadwaj, L.; Waldner, C. Risk Factors Associated with the Choice to Drink Bottled Water and Tap Water in Rural Saskatchewan. Int. J. Environ. Res. Public Health 2014, 11, 1626–1646. [Google Scholar] [CrossRef] [PubMed]
- Merkel, L.; Bicking, C.; Sekhar, D. Parents’ Perceptions of Water Safety and Quality. J. Community Health 2012, 37, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Onufrak, S.J.; Park, S.; Sharkey, J.R.; Sherry, B. The relationship of perceptions of tap water safety with intake of sugar-sweetened beverages and plain water among US adults. Public Health Nutr. 2014, 17, 179–185. [Google Scholar] [CrossRef]
- U.S. Census Bureau. American Community Survey (ACS). Available online: https://www.census.gov/programs-surveys/acs (accessed on 18 December 2021).
- U.S. EPA. Lead at Superfund Sites: Software and Users’ manuals for IEUBK Model. Retrieved 18 December 2021, from U. S. Available online: https://www.epa.gov/superfund/lead-superfund-sites-software-and-users-manuals (accessed on 8 December 2021).
- U.S. CDC. Blood Lead Reference Value | Lead | CDC. Available online: https://www.cdc.gov/nceh/lead/data/blood-lead-reference-value.htm (accessed on 2 December 2022).
- Fokum, F.D.; Entezar, T.; McAfee, K. Effect of the COVID-19 Global Pandemic on Illinois Children Tested for Blood Lead Level and Exposure. Am. J. Public Health 2023, 113, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Aelion, C.M.; Davis, H.T. Blood lead levels in children in urban and rural areas: Using multilevel modeling to investigate impacts of gender, race, poverty, and the environment. Sci. Total Environ. 2019, 694, 133783. [Google Scholar] [CrossRef]
- Akers, D.B.; MacCarthy, M.F.; Cunningham, J.A.; Annis, J.; Mihelcic, J.R. Lead (Pb) Contamination of Self-Supply Groundwater Systems in Coastal Madagascar and Predictions of Blood Lead Levels in Exposed Children. Environ. Sci. Technol. 2015, 49, 2685–2693. [Google Scholar] [CrossRef] [PubMed]
- Jarvis, P.; Quy, K.; Macadam, J.; Edwards, M.; Smith, M. Intake of lead (Pb) from tap water of homes with leaded and low lead plumbing systems. Sci. Total Environ. 2018, 644, 1346–1356. [Google Scholar] [CrossRef] [PubMed]
- Deshommes, E.; Prévost, M.; Levallois, P.; Lemieux, F.; Nour, S. Application of lead monitoring results to predict 0–7 year old children’s exposure at the tap. Water Res. 2013, 47, 2409–2420. [Google Scholar] [CrossRef]
- Zartarian, V.; Xue, J.; Tornero-Velez, R.; Brown, J. Children’s Lead Exposure: A Multimedia Modeling Analysis to Guide Public Health Decision-Making. Environ. Health Perspect. 2017, 125, 097009. [Google Scholar] [CrossRef]
- Stanek, L.W.; Xue, J.; Lay, C.R.; Helm, E.C.; Schock, M.; Lytle, D.A.; Speth, T.F.; Zartarian, V.G. Modeled Impacts of Drinking Water Pb Reduction Scenarios on Children’s Exposures and Blood Lead Levels. Environ. Sci. Technol. 2020, 54, 9474–9482. [Google Scholar] [CrossRef] [PubMed]
| Jackson | Kane | Peoria | |
|---|---|---|---|
| Population, n (%) | |||
| Under 5 years | 3129 (5.4) | 32,962 (6.2) | 12,555 (7.0) |
| 5 to 9 years | 2544 (4.4) | 32,638 (6.1) | 11,115 (6.2) |
| Under 18 years | 10,646 (18.4) | 132,979 (25.0) | 42,236 (23.6) |
| Total Population | 57,977 | 532,403 | 179,179 |
| Rural Housing, % | 30 | 11 | 17 |
| Housing before 1980, % | 60 | 75 | 50.5 |
| Estimated PDWs, n | 1900 | 7100 | 18,000 |
| Water Pb Concentration (µg/L) | |||||
|---|---|---|---|---|---|
| Samples with Detectable Pb (n) | Minimum Detectable | Maximum | Median | IQR * | |
| 1st Liter | |||||
| Jackson (n = 38) | 20 | 0.83 | 76.2 | 0.85 | 1.62 |
| Kane (n = 62) | 27 | 0.83 | 47.0 | 0.54 | 1.62 |
| Peoria (n = 51) | 26 | 0.79 | 15.4 | 0.79 | 1.12 |
| All (n = 151) | 51 | 0.79 | 76.2 | 0.54 | 1.60 |
| 7th Liter | |||||
| Jackson (n = 38) | 11 | 0.89 | 3.93 | 0.54 | 0.46 |
| Kane (n = 62) | 8 | 0.86 | 3.37 | 0.54 | 0 |
| Peoria (n = 51) | 15 | 0.77 | 5.00 | 0.54 | 0.37 |
| All (n = 151) | 34 | 0.77 | 5.00 | 0.54 | 0 |
| Year House Built | Measurable Pb n (%) | Undetectable Pb n (%) | Total n |
|---|---|---|---|
| Pre-1950 | 10 (71.4) | 4 (28.6) | 14 |
| 1950–1969 | 15 (50.0) | 15 (50.0) | 30 |
| 1970–1979 | 24 (63.2) | 14 (36.8) | 38 |
| 1980–Present | 19 (31.7) | 41 (68.3) | 60 |
| Question/Answer | Measurable Pb n (%) | Undetectable Pb n (%) | Total n (%) |
|---|---|---|---|
| Amount Spent on Well Upkeep Annually (n = 146) | |||
| <$100 | 60 (85.7) | 73 (96.1) | 133 (91.1) |
| >$100 | 10 (14.3) | 3 (3.9) | 13 (8.9) |
| p = 0.028 * | |||
| My tap water is safe to drink (n = 148) | |||
| Strongly agree | 32 (45.7) | 41 (52.6) | 73 (49.3) |
| Agree somewhat | 23 (32.9) | 16 (20.5) | 39 (26.4) |
| Neither agree nor disagree | 10 (14.3) | 10 (12.8) | 20 (13.5) |
| Disagree somewhat | 4 (5.7) | 8 (10.3) | 12 (8.1) |
| Disagree strongly | 1 (1.4) | 3 (3.8) | 4 (2.70) |
| p = 0.370 | |||
| Concern about lead in well water after learning about the Flint water crisis (n = 138) | |||
| Yes | 18 (26.9) | 14(19.7) | 32 (23.2) |
| p = 0.320 | |||
| Primary source of water (n = 149) | |||
| Tap Water | 25 (35.2) | 22 (28.2) | 47 (31.5) |
| Bottled Water | 21 (29.6) | 20 (25.6) | 41 (27.5) |
| Treated Tap Water | 15 (21.1) | 26 (33.3) | 41 (27.5) |
| Multiple Sources | 3 (4.2) | 1 (1.3) | 4 (2.7) |
| Other | 7 (9.9) | 9 (11.5) | 16 (10.7) |
| p = 0.393 | |||
| Water Treatment devices (point of use or point of entry) (n = 106) | |||
| Reverse osmosis | 8 (17.4) | 12 (20.0) | 20 (18.9) |
| Ultraviolet light system | 0 (0) | 1 (1.7) | 1 (0.9) |
| Water Softener | 30 (65.2) | 37 (61.7) | 67 (63.2) |
| Multiple Devices | 8 (17.4) | 10 (16.7) | 18 (17.0) |
| p = 0.820 | |||
| Amount of Tap Water Consumed Daily by Drinking (n = 149) | |||
| 1–3 cups | 12 (16.9) | 9 (11.5) | 21 (14.1) |
| 4–7 cups | 23 (32.4) | 26 (33.3) | 49 (32.9) |
| 8 or more cups | 23 (32.4) | 27 (34.6) | 50 (33.6) |
| None | 13 (18.3) | 16 (20.5) | 29 (19.5) |
| p = 0.822 | |||
| Cooking Water Source (n = 148) | |||
| Unfiltered tap water | 46 (64.8) | 47 (61.0) | 93 (62.8) |
| Filtered tap water | 5 (7.0) | 6 (4.11) | 11 (7.4) |
| Bottled water | 4 (5.6) | 2 (1.0) | 6 (4.1) |
| Other | 16 (22.5) | 22 (14.99) | 38 (25.7) |
| p = 0.688 |
| BLLs in µg/dL by Age Group in Years | |||||||
|---|---|---|---|---|---|---|---|
| WLL µg/L (WLL Percentile) | 0.5–1 | 1–2 | 2–3 | 3–4 | 4–5 | 5–6 | 6–7 |
| 0.54 (10–50th) | 3.0 | 3.0 | 2.4 | 2.1 | 2.1 | 1.9 | 1.7 |
| 1.07 (60th) | 3.0 | 3.0 | 2.4 | 2.1 | 2.1 | 1.9 | 1.8 |
| 1.65 (70th) | 3.1 | 3.1 | 2.5 | 2.2 | 2.1 | 2.0 | 1.8 |
| 2.50 (80th) | 3.2 | 3.1 | 2.5 | 2.3 | 2.2 | 2.0 | 1.9 |
| 4.88 (90th) | 3.4 | 3.3 | 2.7 | 2.5 | 2.4 | 2.2 | 2.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keeley, S.; Dorevitch, S.; Kelly, W.; Jacobs, D.E.; Geiger, S.D. IEUBK Modeling of Children’s Blood Lead Levels in Homes Served by Private Domestic Wells in Three Illinois Counties. Int. J. Environ. Res. Public Health 2024, 21, 337. https://doi.org/10.3390/ijerph21030337
Keeley S, Dorevitch S, Kelly W, Jacobs DE, Geiger SD. IEUBK Modeling of Children’s Blood Lead Levels in Homes Served by Private Domestic Wells in Three Illinois Counties. International Journal of Environmental Research and Public Health. 2024; 21(3):337. https://doi.org/10.3390/ijerph21030337
Chicago/Turabian StyleKeeley, Sarah, Samuel Dorevitch, Walton Kelly, David E. Jacobs, and Sarah D. Geiger. 2024. "IEUBK Modeling of Children’s Blood Lead Levels in Homes Served by Private Domestic Wells in Three Illinois Counties" International Journal of Environmental Research and Public Health 21, no. 3: 337. https://doi.org/10.3390/ijerph21030337
APA StyleKeeley, S., Dorevitch, S., Kelly, W., Jacobs, D. E., & Geiger, S. D. (2024). IEUBK Modeling of Children’s Blood Lead Levels in Homes Served by Private Domestic Wells in Three Illinois Counties. International Journal of Environmental Research and Public Health, 21(3), 337. https://doi.org/10.3390/ijerph21030337






