Models of Care in Providing Comprehensive Healthcare on Cancer Survivors: A Scoping Review with a TIDieR Checklist Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
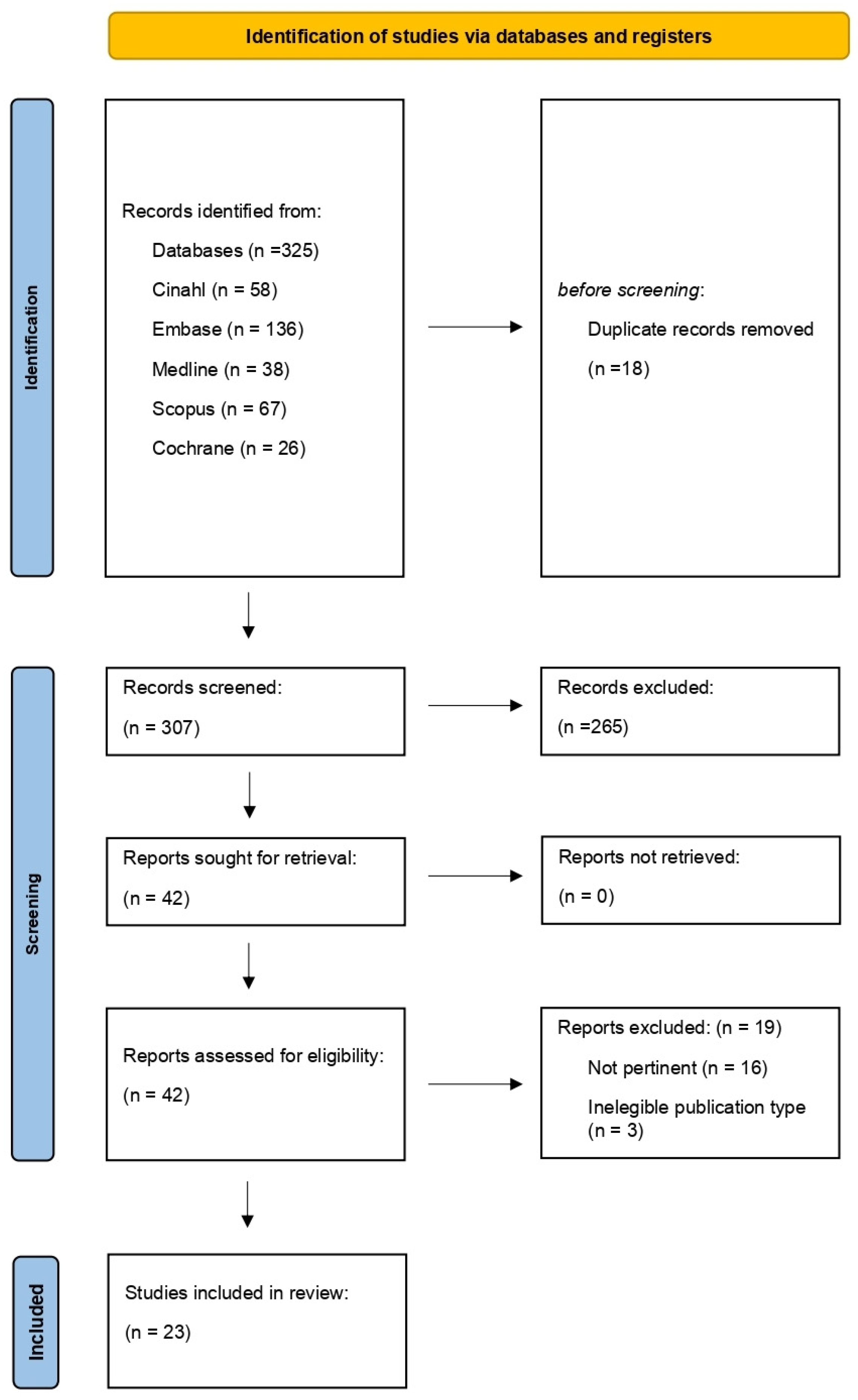
2.3. Study Selection
2.4. Data Extraction
2.5. TIDieR Checklist
2.6. Critical Appraisal of the Evidence
3. Results
3.1. Literature Search Results
3.2. Characteristics of the Included Literature
3.3. Critical Appraisal with the Sources of Evidence
3.4. Results of the Individual Sources of Evidence
3.5. Synthesis of the Results
3.5.1. Professionals Involved in Providing the SCP
3.5.2. Setting and Duration of the SCP Interventions
- shared care with discharge to a general practitioner (GP), with one or two appointments supporting health promotion;
- specialist care with GP support through multidisciplinary visits;
- self-support or community services referral.
3.5.3. Models of Care
- SCP standardization in hospital care: the SCP was used to collect information about specific survivorship issues [35] or for quality-improvement projects aiming to (1) improve the efficacy with the EHR integration of the SCP document [38,40]; (2) improve the accuracy of the SCP document [36]; (3) improve the knowledge and consciousness about specific survivorship issues [41]; (4) improve the complete comprehension of the SCP document [29].
- Consultation-based: several studies reported similar experiences. The SCP intervention was created and completed with the patient during a hospital visit. The SCP document was recorded within the patient chart, and a summary of the indications were given to the patient and sent to the PCP. Clinicians managed the follow-up remotely [22,24,26,28,30,39,42]. Two studies reported a project where a specific computer program was built [37] and used [40]: this integrated information between the EHR, MO, and patients, and was used to create the SCP. One study organized telehealth consultations [25]. In two studies, the ON managed the intervention [21,36].
- PCP direct referral [34].
- Specialist direct referral [23].
- Integration between specialist and primary care: the key elements of the integration were multimodal resources, dedicated clinics, and a shared-care model. One study used different resources (visits, summaries, and a phoneline) to catalyze the passage from active treatment to follow-up care [21]. Glaser et al. [32] reported the experience of a survivorship clinic linked with external services concerning wellness and nutrition. A transition clinic within one of the cancer centers involved in the study of Grant et al. helped transition survivors back to their PCPs [34]. A shared-care model was applied in coresponsibility between the MO and PCP [34], as in Fok et al. [31], where the approach was risk-stratified. In Jefford et al. [23], the patient was discharged to the PCP, with one or two survivorship appointments supporting health promotion.
4. Discussion
4.1. Limitations
4.2. Implication for Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Author Year | Country | Setting | Professionals | Type of Study | Population | Endpoint | Results |
|---|---|---|---|---|---|---|---|
| Rosenberg et al. (2016) [21] | America | Hospitals | Nurse and MO | Observational study | Different types of cancer | Evaluating RAVs in promoting individualized healthcare and self-management during survivorship transition. | A total of 1615 questionnaires were completed. For the strongly agree/agree ratings, 94% felt more confident in communicating their treatment issues to other healthcare providers; 90% felt more comfortable recognizing symptoms to report; 98% had a better appreciation for community programs. |
| Rosales et al. (2014) [22] | America | Outpatient private clinics | Nurse | Observational study | Different types of cancer | Implementing a successful SCP. | For a total of 118 medical record reviews and follow-up telephone calls, the concerns were weight management (35%), fatigue (30%), sexuality (27%), anxiety (23%), caregiver stress (17%), and depression (16%). |
| Jefford et al. (2015) [23] | Oceania | Hospitals and primary care | Multidisciplinary | Pilot study | Different types of cancer | Synthesizing key themes, enablers, and challenges about six 2-year projects of the VCSP. | The lack of tool validity, the limited evidence, the workforce redesign, and the issues around the SCP terminology were challenging factors. |
| Dulko et al. (2013) [24] | America | Hospitals | Nurse | Observational study | Breast and colorectal cancer | Evaluating the SCP completion and surveying oncology staff and PCPs regarding the challenges of implementing the SCP. | The patient response rate: 73%. The oncology staff response rate: 94%. The PCP response rate: 71%. Creation time may be a barrier to SCP implementation. CSs find SCPs useful, but PCPs had insufficient knowledge of the CS issues. Incorporating SCPs in EHR may facilitate the SCP implementation. |
| Patt et al. (2013) [28] | America | Cancer centers | Multidisciplinary | Observational study | Different types of cancer | Implementing an SCP within a suburban oncology practice. | Offering these services to patients in their communities means that we will provide a higher quality of care and help them. |
| Downs-Holmes et al. (2014) [33] | America | Cancer center | Multidisciplinary | Implementation projects | Breast cancer | Describing the steps for the development and implementation of an institution-specific SCP to fulfill the new standards for SCPs. | The steps provided within the context can be adapted to any cancer type with minor modifications. |
| Grant et al. (2015) [34] | America | Cancer centers | Multidisciplinary | Observational study | Breast cancer | Implementation of sustainable models of follow-up care across 14 Canadian Regional Cancer Centers. | All regions used the SCP and patient education materials, direct-to-primary care, transition clinics, and shared care. A total of 85% of the 752 patients reported that they felt prepared for the passage to primary care. |
| Berman et al. (2016) [35] | America | Tele-health | Nurses and PCPs | Observational study | Lung cancer | Generating SCPs using patient-reported outcomes and web-based programs. | Neurocognitive adverse effects (e.g., fatigue and cognitive changes) were the most common (48.8%), especially among those receiving chemotherapy. |
| Tevaarwerk et al. (2017) [36] | America | Cancer centers | Nurse | Observational study | Breast cancer | Describing the change in survivor knowledge after the receipt of TSs delivered as part of the SCPs. | A significant proportion of SCPs prepared for CSs enrolled in a clinical trial contained at least one error (25%) or omission (22%). |
| O’Hea et al. (2016) [37] | America | Outpatient private clinics | Nurses and MOs | Pilot study | Breast cancer | Development and field test of a web-based BC SCP system. | The POST computerized assessment and a tailored SCP were provided for 25 women ending treatment in the past year. A total of 70% of the 23 responders rated the SCP as satisfactory. |
| Jefford et al. (2016) [42] | Oceania | Hospitals | Nurse | RCT | Colorectal cancer | SCP + UC (N = 107) vs. UC (N = 110) to improve psychological distress, SCNs, and the QOL of patients with CRC. | Between-group differences in the SCNs and the QOL at 2 and 6 months were small and nonsignificant. Patients in the SCP group were more satisfied with the SCP than those in the UC group. |
| Runowicz et al. (2016) [43] | America | NA | NA | Guideline | Breast cancer | The purpose of the ACS/ASCO BC SCP was to provide recommendations to assist clinicians in the care of female adult survivors. | Surveillance for BC recurrence, screening for second primary cancers, the assessment and management of the physical and psychosocial LLTEs of BC and its treatment, health promotion, and care coordination. |
Appendix B
| Author Year | Country | Setting | Professionals | Type of Study | Population | Endpoint | Results |
|---|---|---|---|---|---|---|---|
| Lai- Kwon et al. (2022) [25] | Oceania | Tele-health | Nurse | Pilot study | Metastatic melanoma | Verification of the feasibility, acceptability, and utility of a novel model of nurse-led, telehealth-delivered SCP. | The participation rate was 57%; 97% completed the program, demonstrating its utility and acceptability. |
| Lee C.T. et al. (2020) [26] | America | Outpatient private clinic | Nurse and MO | Mixed-methods | Bladder cancer | Acceptability and feasibility of a BC-specific SCP. | A total of 59 SCPs were completed by the providers. Clinical resources were required to ensure the appropriate implementation of the BC SCPs. |
| Ivanics et al. (2019) [27] | America | Outpatient private clinic | Oncological staff | Pilot study | Breast cancer | Evaluating two different SCP programs implemented with a quality-improvement Plan–Do–Study–Act model. | System II (TS by multidisciplinary breast specialists) had fewer inaccuracies than System I (TS by nonspecialist breast clinic staff) (33.78% vs. 51.67%, respectively; p = 0.05). |
| Nàpoles et al. (2019) [29] | America | Telehealth/Home visits | Nurses and MOs | Mixed-methods | Breast cancer | Evaluating the feasibility of an SCP for Spanish-speaking patients approaching the end of active treatment. | A total of 83% of women completed all 5 coaching calls. A total of 81% rated the quality of the app as “very good” or “excellent”. |
| Glaser et al. (2019) [32] | America | Cancer center | Oncological staff | Implementation projects | Breast and gynecologic cancer | Development of an SCP, a network of support services, and an integrative medicine program. | A total of 908 people accessed the survivorship clinic, receiving a complete clinical assessment and an SCP. |
| McGrath et al. (2019) [38] | America | Cancer center | Nurse teams | Quality-improvement projects | Different types of cancer | Standardizing how SCPs are integrated into the EHR. | Standardization of the SCP increased both the participation of the other specialists and increased the rate of completion from 10% to 34%. |
| Lee L.Y. et al. (2023) [39] | Asia | Cancer centers | Nurse | RCT | Head and neck cancer | Nurse-led SCP vs. usual care on physical/mental health emotional distress, social support, and resilience in 100 dyads. | In the IG, the endpoints enhanced after 6 months, with statistical significance. |
| Williamson- Butler et al. (2022) [40] | America | Hospital | Nurse | RCT | Breast cancer | POST (N = 100) vs. UC (N = 100) on patient ratings of quality and the content of discussion with providers at the end of their BC treatment. | The POST women endorsed 20 out of the 29 topics compared to 14 topics endorsed by the UC. The POST women reported a better QOD across all subscales. |
| Su et al. (2019) [41] | America | Tele-health | MO and PCP | RCT | Breast cancer | Web-based BC patient SCP (N = 61) vs. UC (N = 55) to improve on hot flashes, fertility-related concerns, contraception, and vaginal symptoms. | For the IG (70.9%) vs. UC (57.3%): fertility-related concerns (27.9% vs. 14.6%; OR 2.3); hot flashes (58.5% vs. 55.8%; OR 1.1); vaginal symptoms (42.5% vs. 40.7%; OR 1.1); contraception (50% vs. 42.6%; OR 1.4) |
Appendix C
| Brief Name | Why | What Materials | What Procedures | Who Provided | How | Where | When and How Much | Tailoring | Modifications | How Well Planned | How Well Actual | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rosenberg et al. (2016) [21] | LIFE SCP | RAVs: (1) placing post-treatment CSs into the primary care setting; (2) diagnosis and treatments for CSs; (3) the active role of CSs in pursuing wellness; (4) linking CSs to community resources that will assist them in their recovery. | Face-to-face visit: 1 h for the provision and discussion of a personalized SCP, which was entered into the patient’s EPIC, EMR, and was also printed as a patient-friendly portable summary. | The LIFE entry point is a CS consulting RAV for those that have completed active treatment and are directed to the program within 1 year of the completion of medical treatment. | The LIFE program is directed by a physician; a certified oncology nurse is the clinical coordinator and conducts the RAV. | Referrals to the LIFE RAV: (1) sending an EPIC in-basket message with the patient’s chart attached to the LIFE clinical coordinator; (2) calling the LIFE line; (3) placing a CS outpatient order in EPIC. | Visits take place 5/7 days in any of the 3 hospital locations and depend on patient preference and provider availability as to the location, time, and date of the appointment. | LIFE participants are anonymously surveyed in two ways: immediately after their RAV and then at least 1 year after. | ||||
| Rosales et al. (2014) [22] | MSTI, with support from the NCCCP and ASCO | MSTI: the patient’s SCP is prepared in the EHR by a registered health information technician. This document is reviewed during an appointment with a nurse practitioner and social worker. | Medical record audit and follow-up telephone call. | When patients at the MSTI complete chemotherapy and/or radiation therapy, they are referred for a survivorship follow-up visit. | The visit lasts 1 h and consists of a joint visit with a nurse oncologist and oncological social worker of the MSTI clinic. | The nurse conducts an examination to the physical LLTE of the treatment, surveillance, and health promotion, discusses the importance of care coordination, and explains how this document will be shared with the PCP. | The social worker assists the nurse practitioner with the discussion of the SCP. | A total of 90 min of social work time, 75 min of nurse practitioner time, and 60 min of registered health information technician time. | The RHIT sends a copy of the patient’s treatment summary and care plan with the provider’s dictation to the PCP and referring physician. | |||
| Jefford et al. (2015) [23] | VCSP | Pilot projects: (1) the post-treatment assistance of CSs in acute and primary care; (2) focus of the specific care needs of different groups of CSs; (3) assessing the VMS (effectiveness and transferability); (4) recommendations for better follow-up assistance. | Semistructured interviews were conducted with VCSP pilot project managers, clinicians, stakeholders, and family doctors. Motivational interviews of nurses (training/experience) were also conducted. | Telephone information and support lines are well-positioned to deliver SCP well-being coaching in an ongoing and economically sustainable way. | The VCSP has had difficulty involving MOs for the self-management of patients in SCPs; this may reflect the traditional follow- up, in which there is limited space for the integration of support for self-management. | |||||||
| Dulko et al. (2013) [24] | JF | The SCPs used to survey oncology staff and PCPs regarding challenges of implementing SCPs were evaluated. | The JF packet was downloaded and given to each staff member, which was available to the APPs through the JF toolkit on the website. | Telephone interviews were conducted with patients about two months after the care plan visit. | The nurse is well positioned to create and deliver SCPs, transitioning patients from oncology care to a PCP in a shared-care model of optimal wellness. | The nurse presented and discussed the SCP with the CS at that appointment. Several days prior to the visit, patients at both sites received a telephone call to remind them of the upcoming appointment. | Accessing complete medical records is an obstacle to completing the SCPs. A 3–6-month window to develop and deliver the SCPs may be ideal. | SCP: (a) patient diagnosis and treatment, (b) follow-up care and secondary prevention, (c) information on the LLTEs of cancer treatments received, and (d) a list of national and local health promotion resources. | ||||
| Patt et al. (2013) [28] | IOM, COC | No universal model for CS delivery exists today, and program models vary significantly. | 1° A survivorship visit 2–3 months after the initial therapy was complete, as this is a time when patients may be more receptive to these issues (1 h). There was also an additional 30–60 min in preparation for the midlevel provider before the visit to complete the initial SCP document. | In addition, there was a general assessment of the triage and referral needs for nutrition, exercise, physical therapy, counseling, and other services, as well as a decision to have the patient follow up for survivorship issues in 3–6 months for higher acuity issues, or 1 year if minimally active issues were identified. | The longitudinal model, however, disseminates the survivorship plan early on, but continues to follow the patient. Some survivorship programs are also integrated with long-term follow-up clinics and are merged with expected follow-up visits. | Texas Oncology Cancer Center, Austin. | Within community practice, the development of a survivorship program could be independent or in collaboration with a local hospital program. | The AYA Healthy Survivorship mobile app, with evidence-based self-assessment, a BMI calculator, children’s oncology group health links, resource links, a survivorship plan links; right, the ASCO’s Cancer Net tumor-specific mobile application showing some of the app’s educational content. | ||||
| Downs-Holmes et al. (2014) [33] | Survivorship care, including the IOM, NCCN, ASCO, LiveStrong, and the ONS | Symptom assessment and collaboration of care in follow-up excelled; documentation supporting the other efforts in survivorship care were lacking. Survivorship education focused on community resources, diet, exercise, lymphedema, and recurrence. | An interdisciplinary team, include representation from the APRN, social workers, nurse navigators, and a survivorship coordinator or designated administrative support, as well as surgical, medical, and radiation oncologists. | ASCO guidelines for follow-up survivorship care with examinations every 3 months for the first 3 years, every 6–12 months for the 4th and 5th years, and annually thereafter. The goal of the program was to alternate visits among the BC team specialists to fulfill the guidelines set by the NCCN and ASCO for the coordination of care. The program has been successfully implemented, ensuring survivors that their providers are communicating in their ongoing care. | Many implications exist for nursing staff in an SCP, including the evaluation and documentation of distress, coping, fatigue, lymphedema, sleep disturbance, and menopausal symptoms. In addition, the reinforcement and encouragement of established patient goals for healthy lifestyle are crucial for change to occur. Education on symptom management, community, and hospital-based resources are also crucial. | Instrumental to the collaboration of care among providers and the documentation of the SCP is the responsibility of the nurse. | ||||||
| Grant et al. (2015) [34] | Survivorship Program at CCO | Many BCSs continue to be seen by specialists for routine follow-up care, despite growing evidence that transitioning appropriate BCSs to primary care is safe and effective. | Software development and IT support. | Three main models of follow-up care were developed: (1) direct-to-primary care, (2) transition clinics, and (3) shared care. | The SCP was directed by a nurse, FHT, GPO, MO, and PCP. | Fourteen RCCs in Ontario, Canada. | An environmental scan after 1 year. | Analysis of the models described in the final reports submitted by each RCC identified three main models of follow-up care: (1) direct to the PCP, (2) the transition clinics, and (3) shared care. | All 14 RCCs developed an SCP, a transition letter, and patient education material. The SCP, in most cases, was populated by a nurse at the cancer center and was sent by fax or mail to the survivor’s PCP in the community. All SCPs included an up-to-date list of local resources for survivors. | CSs and their PCPs in these regions were offered direct access to a nurse via telephone. Transitioned survivors and their PCPs were provided direct access to a contact within the RCC who would be able to triage questions about follow-up care or recurrence. | ||
| Berman et al. (2016) [35] | OncoLife and the LIVESTRONG (Internet-based) | Patients were asked about symptoms, disease characteristics, and previous and LLTEs. The characteristics of the PCF users were analyzed, and the PROs were related to the treatments provided. | Internet-based programs, publicly accessible via OncoLink, were created to design individualized SCPs for patients treated previously for cancer. | Nurses and physicians. | PROs have been shown to be prognostic for survival. Emerged patterns of longitudinal PROs were collected in the development of the SCP. | |||||||
| Tevaarwerk et al. (2017) [36] | Treatment summaries prepared as part of the SCP should correctly and thoroughly report diagnosis and treatment information. | The EMR, external software program, and manual clinic record. | The EHR or using manual data entry into an external software program to create the summary. | A nurse reviewed each survivor’s medical records to abstract the necessary diagnosis and treatment data. The nurse then provided the document, typically as part of an SCP visit (either in person or telephone-based). | Two midwestern cancer centers. | As part of a clinical trial. | ||||||
| Jefford et al. (2016) [42] | Nurse-led supportive care package for CRC | The improvement of the SCNs and QOL of patients with CRC. The intervention comprised of educational materials, needs assessments, SCPs, end-of-treatment sessions, and 3 follow-up telephone calls. | (a) Information package, (b) nurse-led, face-to-face end-of-treatment session; (c) a tailored SCP; (d) telephone follow-up. | Nurses received training in all aspects of the protocol into usual care. | Private hospital clinic room. | These sessions occurred 1, 3, and 7 weeks after the first intervention. The sessions revisited issues discussed during the end-of-treatment and addressed any other CS issues in 60 min. |
Appendix D
| Brief Name | Why | What Materials | What Procedures | Who Provided | How | Where | When and How Much | Tailoring | Modifications | How Well Planned | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lai- Kwon et al. (2022) [25] | Nurse-led MELCARE | Telehealth-delivered: electronic survey after the follow-up consultation assessing the overall utility of MELCARE. | MELCARE was designed by a multidisciplinary team of healthcare professionals and consumers from the MIA and MPA. It consisted of two, 1 h, melanoma nurse-led consultations conducted via telephone 3 months apart. | All participants received MELCARE, a nurse-led survivorship program involving two telehealth consultations 3 months apart, a needs assessment using the DT and problem list, and the creation of an SCP. | Specialist melanoma center in Australia. | Administration of the DT and problem list in the initial nurse-led telehealth consultation of 60 min. Within 2 weeks of the initial consultation: produce an SCP (shared with participants, PCPs, and MOs). Three months after initial consultation: administer the DT and problem list follow-up in the nurse-led telehealth consultation of 60 min. After follow-up consultation: participants complete the utility survey. | |||||
| Lee et al. (2020) [26] | A bladder cancer SCP (ASCO, NCCN, IOM, and CoC) | A nurse and physicians. | Focus groups: 60 and 120 min with physicians (e.g., urologists and oncologists) and nonphysician providers (e.g., physician assistants, PAs, nurse practitioners, and social workers). | Twelve high academic health-centers in the US and Canada, and one private practice group enrolled patients in this prospective clinical pilot. | A mixed-method model in III phases; a 12.3 min SCP. | ||||||
| Ivanics et al. (2019) [27] | Healthcare improvement’s Plan–Do–Study–Act model | System I involved TSs drafted by nonspecialist breast clinic staff; System II involved TSs vetted through a multidisciplinary breast specialist conference approach. The accuracy of the basic documentation entries related to dates and the components of the treatment were compared for the two approaches. | The EHR of these patients for the monitoring of the timeline regarding when each patient is due to receive the SCP–TS document. | The Breast Program Leadership Committee convenes monthly and includes representatives from surgery, MO, radiation, pathology, radiology, as well as nurses and physical therapy/rehabilitation medicine. | Breast oncology personnel or nurses. | A nurse and physician maintain an EHR of these patients for the monitoring of the timeline regarding when each patient is due to receive the SCP–TS document. | Patients requiring chemotherapy are assigned to have their SCP–TS drafted by a member of medical oncology; patients requiring surgery and no chemo/radiotherapy are assigned to a surgical team; patients receiving radiation as a component of their care, but no chemotherapy, are assigned to a radiation oncologist. | ||||
| Nápoles et al. (2019) [29] | Mobile phone app “Nuevo Amanecer (New Dawn)” and telephone coaching for the SCP | Spanish-speaking Latina BCSs’ experience disparities in the knowledge of BC survivorship care, psychosocial health, lifestyle risk factors, and symptoms compared with their white counterparts. The SCP could help these women receive optimal follow-up care and manage their conditions. | Instructions on the use of the SCP; a booklet; the app installed; an unmasked activity tracker; an illustrated guide. | Completed SCPs were reviewed by the project director and the patient’s oncologist or oncology nurse, and scanned into the patient’s EHR. | A 2-month intervention. Home visit 1: a 45–60 min visit. Home visit 2: in this 1 h visit, participants received instructions. | The mobile app home page contained: daily walks, treatment, follow-up care, and managing symptoms. | Coaching consisted of 5 weekly phone calls with the following structure: daily steps goal and working through any barriers; 5 health topics: (1) walking and nutrition, (2) BC follow-up care, (3) signs of recurrence, (4) treatment LLTEs, and (5) resources and review of content from the first 4 calls. | Home visit 1: The RA conducted the visit at the clinic site or the participant’s home. Home visit 2: participants received materials and verbal instructions on the use of the written SCP. Home visit 3: At this visit, the RA conducted the final assessment and a brief satisfaction survey, synchronized the activity tracker, and collected the mobile phone and charger. | |||
| Corsini et al. (2020) [30] | SA CS framework | The framework was developed to identify and recommend the minimum level of care CSs should receive following the completion of treatment. Key components of the framework include the provision of a cancer TS and the development of a CP. | The NCCN DT and Problem checklist was utilized during individual consultations with the survivors to identify the key needs and priorities, and to establish goals to address these within the CP. | The time to TS and CP was 154 min (median 165 min) per person: for medical records, it was 20–90 min (median 50 min); for needs assessment, it was 45–90 min (median 60 min); for the delivery to survivors of the letter from GPs, it was 30–75 min (median 50 min). | Four self-selected teams consisting of a nurse candidate and an MO. | Face-to-face consultation with one nurse. | Four medical oncology clinics in South Australia participated (three metropolitan and one regional). | A 3-month pilot study; 165 min per person. | The CP template was revised to list resources at the bottom with reference to relevant websites. As a result of the early discussions at the debrief sessions, a list of key phrases and examples of common issues being identified within the CP were developed. | ||
| Fok et al. (2020) [31] | PCPs towards managing low-risk BCSs in a shared-care model with specialists | To explore the perspectives of PCPs towards managing BCSs in a community-based shared-care model. | For a shared-care model involving PCPs, an MO assumes the responsibility for cancer-related care, with the PCP focusing on the primary care. This model adopts a risk-stratified approach, where low-risk BCSs are managed by alternating visits with oncologists and PCPs. | Expanding PCPs’ role in survivorship care must go beyond relieving the MO to allow them to focus on active cancer treatment. | PCPs are best placed to address unmet needs in the psychosocial domains, optimize comorbidities, and ensure adherence to lifestyle modifications. | Singapore, which included private PCPs and public PCPs. | Qualitative study. | Recommendations from the PCP included risk stratification, role definition, focused training, timely communication, and sustainable funding to equip them for this expanded role. However, the successful implementation must be centered around instilling in the BCS the belief that her PCP is a valued partner in her cancer journey. | |||
| Glaser et al. (2019) [32] | Survivorship program at Roswell Park Comprehensive Cancer Center (Roswell Park) | An SCP at an urban National Cancer Institute-designated comprehensive cancer center with three closely linked components: an SCP with a dedicated staff, a network of support services, including wellness, and an integrative medicine program. | (1) Patients’ complete treatment (one-time visit to survivorship provides the patient and family with a complete assessment at the start of the post-treatment period). (2) An avenue to survivorship is a transfer from oncology for long-term surveillance. (3) A way to access survivorship is through self-referral. | The SCP should not be solely contingent on the preferences of the oncology team. | Roswell Park Comprehensive Cancer Center (Buffalo, NY) | A 1-year pilot study. | These services would transfer patients to the centralized SCP, whereas others would prefer to provide an SCP within the oncology practices. The M.R. met with the other oncology disease sites to define a workable SCP pathway and to determine the optimal timeframe for transitioning these patients from the oncology service to the survivorship service. | ||||
| McGrath et al. (2019) [38] | LIVESTRONG, JF, and ASCO guidelines | (1) Develop an EHR; (2) evaluate an SCP within 3 to 6 months of the completion of therapy for survival visits; (3) develop site-specific treatment plans that meet ASCO standards; (4) pilot the implementation of an SCP using EMR functions; (5) assess the process. | Oncology DMGs created flow sheets that included information about CS treatments and LLTEs. These flowsheets and models are live documents for a disease-specific flow sheet. | The NP entered the data into the flow sheet, and this information was then easily uploaded into the hardened SCP document. Using the disease-specific flow sheet and the tempered SCP document, including the patient’s “smart text” education, it was validated that the completion of a treatment plan took less than 15 min for patients. | Research suggests that nurse survivorship clinics have been successful in providing quality SCPs in accordance with the IOM recommendations and demonstrate improvement in patient satisfaction, QOL, and process efficiency. | Nurse group evaluation: the audit was performed by a chart review using an EPIC/Beacon-generated list that utilized “curative intent” and the completion of a Beacon plan to create an eligible patient list. This list was then reviewed by the nurse group to assess the number of eligible patients who had completed the SCP. | NCI-designated academic medical center. | The timing of the delivery of the SCP was targeted between 3 and 6 months after completion of therapy to comply with the Commission on Cancer standards. Then, there was a 3- and 6-month evaluation of the project efficacy. | The SCP identifies medical oncology as the provider responsible for all combined modality patients. Radiation oncology is responsible for patients receiving definitive radiation therapy only. | The NP group responsible for delivering the treatment plans has met several times to reach a consensus on the “intelligent text” used in the model for the patient education. The “smart text” could be loaded into a patient’s SCP and easily edited for CSs. | |
| Lee et al. (2023) [39] | A nurse-led SCP on the health and resilience of primary caregivers of patients with advanced head and neck cancer | Evaluate the effects of a nurse-led SCP on emotional distress, social support, physical health, mental health, and resilience in primary caregivers of patients with advanced head and neck cancer. | Five domains: (1) problems of primary caregivers; (2) cancer risk factors, the side-effects of treatment, caregiving burden, and possible contraindications; (3) caregiving skills and psychological supportive care; (4) health promotion and surveillance for cancer recurrence; (5) primary caregivers’ feedback on the effectiveness of the program. | The nurse with the dyads in the IG had monthly meetings for the first 6 months (1 h visit) to the clinic after the patient had completed the initial HNC treatment. Follow-up calls to discuss the problems and concerns of the primary caregivers were made twice a week. The CG received usual care in the health education room, including caregiving information regarding symptom management, daily care, and medical appointments. | A hospital in northern Taiwan. | A 4-year RCT with parallel, double-blind recruitment. | The nurse-led SCP can be applied before the patients complete the treatment, which may increase the positive effect on physical health and adaptation. | ||||
| Williamson-Butler et al. (2022) [40] | POST | A web-based program: the EHR and from the MO providers generate an individualized SCP that abides by the IOM and ASCO guidelines. | SCP content checklist to examine the patient-reported quality and content of the discussion with their MO. Individualized SCP, which was created by the blinded for review RA and the study nurse, using both the patients’ EHR and their responses to the POST assessment. | The final SCP consisted of 10 patient-centered questions; every plan contained sections that included information on follow-ups, general recommendations for BCSs, possible LLTEs, screening and surveillance tips, etc. Finally, at the research visit, the TAU women received the affiliated hospital’s standard care planning procedure. Like the POST protocol, the TAU women also completed the final baseline assessments at this visit. | The nurse provides the POST to women ending treatment for BC: it may help women transition into survivorship feeling more knowledgeable about important survivorship topics and satisfied with their oncology care. | In person visit, follow-up via phone or e-mail at 1-, 3-, and 6-months postbaseline, which measured the psychological, physical, and emotional outcomes. On average, it took about 30 min for the study nurse to review the SCP with the POST women. | Last treatment visit in hospital oncology care. | The TAU women received an SCP. For these women, the nurse spent approximately 20 to 30 min reviewing the care plan with them. | |||
| Su et al. (2019) [41] | BC SCP | BCSs who received a web-based, women’s health SCP were more likely to improve on at least one of four targeted issues compared to the attention controls. | (1) A 2-page SCP framed in a question-and-answer format; (2) a detailed summary of the systematic review results; (3) a description of the relevant clinical guidelines with hyperlinks to them; (4) curated web-based resources for CSs and providers. | The SCP was accessible to both survivors and the provider of their choice, as survivors actively seek health information from their providers and on the Internet. | MOs and PCPs. |
References
- World Health Organization. Who.int. Available online: https://www.who.int/health-topics/cancer (accessed on 4 January 2024).
- van Leeuwen, M.; Husson, O.; Alberti, P.; Arraras, J.I.; Chinot, O.L.; Costantini, A.; Darlington, A.-S.; Dirven, L.; Eichler, M.; Hammerlid, E.B.; et al. Understanding the Quality of Life (QOL) Issues in Survivors of Cancer: Towards the Development of an EORTC QOL Cancer Survivorship Questionnaire. Health Qual. Life Outcomes 2018, 16, 114. [Google Scholar] [CrossRef] [PubMed]
- Sanft, T.; Denlinger, C.S.; Armenian, S.; Baker, K.S.; Broderick, G.; Demark-Wahnefried, W.; Friedman, D.L.; Goldman, M.; Hudson, M.; Khakpour, N.; et al. NCCN Guidelines Insights: Survivorship, Version 2.2019. J. Natl. Compr. Cancer Netw. 2019, 17, 784–794. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, A.T.C.; da Silva, R.P.; de Almeida, L.M.; Bosi, M.L.M.; de Menezes, M.d.F.B.; Skaba, M.M.V.F.; Nigenda, G.; Arruda, C.A.M.; Pinheiro, C.P.O.; González-Robledo, M.C.; et al. Cancer Survivorship Needs in Brazil: Patient and Family Perspective. PLoS ONE 2020, 15, e0239811. [Google Scholar] [CrossRef]
- Ross, L.W.; Townsend, J.S.; Rohan, E.A. Still Lost in Transition? Perspectives of Ongoing Cancer Survivorship Care Needs from Comprehensive Cancer Control Programs, Survivors, and Health Care Providers. Int. J. Environ. Res. Public Health 2022, 19, 3037. [Google Scholar] [CrossRef] [PubMed]
- Saiganesh, H.; Duffy, C.; Chrysanthopoulou, S.A.; Dizon, D.S. Predictors and impact of survivorship care plans and survivorship care visits. J. Cancer Surviv. 2023, 24, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hill, R.E.; Wakefield, C.E.; Cohn, R.J.; Fardell, J.E.; Brierley, M.E.; Kothe, E.; Jacobsen, P.B.; Hetherington, K.; Mercieca-Bebber, R. Survivorship Care Plans in Cancer: A Meta-Analysis and Systematic Review of Care Plan Outcomes. Oncologist 2020, 25, e351–e372. [Google Scholar] [CrossRef] [PubMed]
- Vardy, J.L.; Chan, R.J.; Koczwara, B.; Lisy, K.; Cohn, R.J.; Joske, D.; Dhillon, H.M.; Jefford, M. Clinical Oncology Society of Australia Position Statement on Cancer Survivorship Care. Aust. J. Gen. Pract. 2019, 48, 833–836. [Google Scholar] [CrossRef] [PubMed]
- Lorenzi, E.; Morello, L.; Giordano, L.; Agostinetto, E.; Garassino, I.M.G.; Cavina, R.; Mazza, R.; Persico, P.; Simonelli, M.; Carlo-Stella, C.; et al. Quality of Life of Adult Cancer Survivors Enrolled in Humanitas Research Hospital’s Survivorship Care Model. Support Care Cancer 2022, 30, 5561–5564. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Bernardes, R.A.; Cruz, A.; Neves, H.; Parola, V.; Catela, N. Screening Tools Designed to Assess and Evaluate Oropharyngeal Dysphagia in Adult Patients: A Scoping Review. Nurs. Rep. 2022, 12, 245–258. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better Reporting of Interventions: Template for Intervention Description and Replication (TIDieR) Checklist and Guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef]
- Fugazzaro, S.; Denti, M.; Accogli, M.A.; Costi, S.; Pagliacci, D.; Calugi, S.; Cavalli, E.; Taricco, M.; Bardelli, R.; on behalf of Look after Yourself Project. Self-Management in Stroke Survivors: Development and Implementation of the Look after Yourself (LAY) Intervention. Int. J. Environ. Res. Public Health 2021, 18, 5925. [Google Scholar] [CrossRef] [PubMed]
- Noonan, M.; Jomeen, J.; Doody, O. A Review of the Involvement of Partners and Family Members in Psychosocial Interventions for Supporting Women at Risk of or Experiencing Perinatal Depression and Anxiety. Int. J. Environ. Res. Public Health 2021, 18, 5396. [Google Scholar] [CrossRef] [PubMed]
- Armijo-Olivo, S.; Stiles, C.R.; Hagen, N.A.; Biondo, P.D.; Cummings, G.G. Assessment of Study Quality for Systematic Reviews: A Comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological Research. J. Eval. Clin. Pract. 2012, 18, 12–18. [Google Scholar] [CrossRef] [PubMed]
- CASP Checklist: 10 Questions to Help You Make Sense of a Qualitative Research How to Use this Appraisal Tool: Three Broad Issues Need to be Considered when Appraising a Qualitative Study. Casp-uk.net. Available online: https://casp-uk.net/images/checklist/documents/CASP-Qualitative-Studies-Checklist/CASP-Qualitative-Checklist-2018_fillable_form.pdf (accessed on 4 January 2024).
- Awan, H.; Mughal, F.; Kingstone, T.; Chew-Graham, C.A.; Corp, N. Emotional distress, anxiety, and depression in South Asians with long-term conditions: A qualitative systematic review. Br. J. Gen. Pract. 2022, 72, e179–e189. [Google Scholar] [CrossRef] [PubMed]
- Berian, J.R.; Cuddy, A.; Francescatti, A.B.; O’Dwyer, L.; Nancy You, Y.; Volk, R.J.; Chang, G.J. A systematic review of patient perspectives on surveillance after colorectal cancer treatment. J. Cancer Surviv. 2017, 11, 542–552. [Google Scholar] [CrossRef]
- Okubo, R.; Wada, S.; Shimizu, Y.; Tsuji, K.; Hanai, A.; Imai, K.; Uchitomi, Y.; Fujiwara, Y.; Tsugane, S.; Matsuoka, Y.J. Expectations of and recommendations for a cancer survivorship guideline in Japan: A literature review of guidelines for cancer survivorship. Jpn J. Clin. Oncol. 2019, 49, 812–822. [Google Scholar] [CrossRef]
- Brouwers, M.C.; Kerkvliet, K.; Spithoff, K.; AGREE Next Steps Consortium. The AGREE Reporting Checklist: A Tool to Improve Reporting of Clinical Practice Guidelines. BMJ 2016, 352, i1152. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, C.A.; Flanagan, C.; Brockstein, B.; Obel, J.C.; Dragon, L.H.; Merkel, D.E.; Wade, E.L.; Law, T.M.; Khandekar, J.D.; Hensing, T.A. Promotion of Self-Management for Post Treatment Cancer Survivors: Evaluation of a Risk-Adapted Visit. J. Cancer Surviv. 2016, 10, 206–219. [Google Scholar] [CrossRef]
- Rosales, A.R.; Byrne, D.; Burnham, C.; Watts, L.; Clifford, K.; Zuckerman, D.S.; Beck, T. Comprehensive Survivorship Care with Cost and Revenue Analysis. J. Oncol. Pract. 2014, 10, e81–e85. [Google Scholar] [CrossRef]
- Jefford, M.; Kinnane, N.; Howell, P.; Nolte, L.; Galetakis, S.; Bruce Mann, G.; Naccarella, L.; Lai-Kwon, J.; Simons, K.; Avery, S.; et al. Implementing Novel Models of Posttreatment Care for Cancer Survivors: Enablers, Challenges and Recommendations: Post-Treatment Care of Cancer Survivors. Asia Pac. J. Clin. Oncol. 2015, 11, 319–327. [Google Scholar] [CrossRef]
- Dulko, D.; Pace, C.M.; Dittus, K.L.; Sprague, B.L.; Pollack, L.A.; Hawkins, N.A.; Geller, B.M. Barriers and Facilitators to Implementing Cancer Survivorship Care Plans. Oncol. Nurs. Forum 2013, 40, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Lai-Kwon, J.; Kelly, B.; Lane, S.; Biviano, R.; Bartula, I.; Brennan, F.; Kivikoski, I.; Thompson, J.; Dhillon, H.M.; Menzies, A.; et al. Feasibility, Acceptability, and Utility of a Nurse-Led Survivorship Program for People with Metastatic Melanoma (MELCARE). Support Care Cancer 2022, 30, 9587–9596. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.T.; Mohamed, N.E.; Pisipati, S.; Shah, Q.N.; Agarwal, P.K.; Downs, T.M.; Droller, M.; Gilbert, S.M.; Goltz, H.H.; Hall, S.J.; et al. Development and Evaluation of a Bladder Cancer Specific Survivorship Care Plan by Patients and Clinical Care Providers: A Multi-Methods Approach. BMC Health Serv. Res. 2020, 20, 686. [Google Scholar] [CrossRef] [PubMed]
- Ivanics, T.; Proctor, E.; Chen, Y.; Ali, H.; Severson, D.; Nasser, H.; Colbert, S.; Susick, L.; Walker, E.; Petersen, L.; et al. Evaluation of a Multidisciplinary Team Approach for Generating Survivorship Care Plan Treatment Summaries in Patients with Breast Cancer. J. Oncol. Pract. 2019, 15, e467–e474. [Google Scholar] [CrossRef] [PubMed]
- Patt, D.; Toth, S.; Hennegham, A.; Mikan, S. How to Begin a Survivorship Program in Your Community Oncology Practice. Community Oncol. 2013, 10, 272–276. [Google Scholar] [CrossRef]
- Nápoles, A.M.; Santoyo-Olsson, J.; Chacón, L.; Stewart, A.L.; Dixit, N.; Ortiz, C. Feasibility of a Mobile Phone App and Telephone Coaching Survivorship Care Planning Program among Spanish-Speaking Breast Cancer Survivors. JMIR Cancer 2019, 5, e13543. [Google Scholar] [CrossRef] [PubMed]
- Corsini, N.; Hislop, C.; Doherty, T.; Eckert, M.; Cameron, K.; Fitzgerald, M.; Bessen, T.; Christensen, C.; Loft, N.; Turpin, K.; et al. A Quality Improvement Pilot to Initiate Treatment Summaries and Survivorship Care Plans in Oncology Services in South Australia. Aust. J. Adv. Nurs. 2020, 37, 5–13. [Google Scholar] [CrossRef]
- Fok, R.W.-Y.; Low, L.L.; Quah, H.M.J.; Vasanwala, F.; Low, S.G.; Soh, L.L.; Mohamad, F.; Loh, K.W.-J.; Soong, Y.L.; Ke, Y.; et al. Roles and Recommendations from Primary Care Physicians towards Managing Low-Risk Breast Cancer Survivors in a Shared-Care Model with Specialists in Singapore—A Qualitative Study. Fam. Pract. 2020, 37, 547–553. [Google Scholar] [CrossRef]
- Glaser, K.M.; McDaniel, D.C.; Hess, S.M.; Flores, T.F.; Rokitka, D.A.; Reid, M.E. Implementing an Integrative Survivorship Program at a Comprehensive Cancer Center: A Multimodal Approach to Life after Cancer. J. Altern. Complement. Med. 2019, 25, S106–S111. [Google Scholar] [CrossRef]
- Downs-Holmes, A.; Dracon, A.; Svarovsky, T.; Sustin, M. Development of a Survivorship Program. Clin. J. Oncol. Nurs. 2014, 18, 5. [Google Scholar] [CrossRef]
- Grant, M.; De Rossi, S.; Sussman, J. Supporting Models to Transition Breast Cancer Survivors to Primary Care: Formative Evaluation of a Cancer Care Ontario Initiative. J. Oncol. Pract. 2015, 11, e288–e295. [Google Scholar] [CrossRef] [PubMed]
- Berman, A.T.; DeCesaris, C.M.; Simone, C.B., II.; Vachani, C.; DiLullo, G.; Hampshire, M.K.; Metz, J.; Hill-Kayser, C. Use of Survivorship Care Plans and Analysis of Patient-Reported Outcomes in Multinational Patients with Lung Cancer. J. Oncol. Pract. 2016, 12, e527–e535. [Google Scholar] [CrossRef] [PubMed]
- Tevaarwerk, A.J.; Hocking, W.G.; Zeal, J.L.; Gribble, M.; Seaborne, L.; Buhr, K.A.; Wisinski, K.B.; Burkard, M.E.; Wiegmann, D.A.; Sesto, M.E. Accuracy and Thoroughness of Treatment Summaries Provided as Part of Survivorship Care Plans Prepared by Two Cancer Centers. J. Oncol. Pract. 2017, 13, e486–e495. [Google Scholar] [CrossRef] [PubMed]
- O’Hea, E.; Wu, J.; Dietzen, L.; Harralson, T.; Boudreaux, E.D. The Polaris Oncology Survivorship Transition (POST) System: A Patient- and Provider-Driven Cancer Survivorship Planning Program. J. Oncol. Navig. Surviv. 2016, 7, 11–24. [Google Scholar] [PubMed]
- McGrath, E.B.; Schaal, A.; Pace, C. The Integration of Survivorship Care Planning at a Comprehensive Cancer Center. J. Adv. Pract. Oncol. 2019, 10, 461. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.-Y.; Huang, B.-S.; Lin, C.-Y.; Su, Y.-H.; Chung, C.-F.; Chang, Y.-L.; Chen, S.-C. Effects of a Nurse-Led Survivorship Care Program on the Health and Resilience of Primary Caregivers of Patients with Advanced Head and Neck Cancer: A Randomized Controlled Trial. Semin. Oncol. Nurs. 2023, 39, 151425. [Google Scholar] [CrossRef] [PubMed]
- Williamson-Butler, S.; Creamer, S.; Flahive, J.; Keating, B.; Crocker, C.; Edmiston, K.; Harralson, T.; Boudreaux, E.; O’Hea, E. Impact of Survivorship Care Planning of Oncology Care at the End of Treatment for Breast Cancer: A Randomized Controlled Trial. Arch. Breast Cancer 2022, 9, 109–118. [Google Scholar] [CrossRef]
- Irene Su, H.; Stark, S.; Kwan, B.; Boles, S.; Chingos, D.; Ehren, J.; Gorman, J.R.; Krychman, M.; Romero, S.A.D.; Mao, J.J.; et al. Efficacy of a Web-Based Women’s Health Survivorship Care Plan for Young Breast Cancer Survivors: A Randomized Controlled Trial. Breast Cancer Res. Treat. 2019, 176, 579–589. [Google Scholar] [CrossRef]
- Jefford, M.; Gough, K.; Drosdowsky, A.; Russell, L.; Aranda, S.; Butow, P.; Phipps-Nelson, J.; Young, J.; Krishnasamy, M.; Ugalde, A.; et al. A Randomized Controlled Trial of a Nurse-Led Supportive Care Package (SurvivorCare) for Survivors of Colorectal Cancer. Oncologist 2016, 21, 1014–1023. [Google Scholar] [CrossRef]
- Runowicz, C.D.; Leach, C.R.; Henry, N.L.; Henry, K.S.; Mackey, H.T.; Cowens-Alvarado, R.L.; Cannady, R.S.; Pratt-Chapman, M.L.; Edge, S.B.; Jacobs, L.A.; et al. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. CA Cancer J. Clin. 2016, 66, 43–73. [Google Scholar] [CrossRef]
- Pollock, D.; Peters, M.D.J.; Khalil, H.; McInerney, P.; Alexander, L.; Tricco, A.C.; Evans, C.; de Moraes, É.B.; Godfrey, C.M.; Pieper, D.; et al. Recommendations for the Extraction, Analysis, and Presentation of Results in Scoping Reviews. JBI Evid. Synth. 2023, 21, 520–532. [Google Scholar] [CrossRef]
| Quantitative Study | EPHPP |
|---|---|
| Lee et al. (2023) [39] | Strong |
| Lai-Kwon et al. (2022) [25] | Moderate |
| Williamson-Butler et al. (2022) [40] | Strong |
| Lee et al. (2020) [26] | Moderate |
| Corsini et al. (2020) [30] | Moderate |
| Glaser et al. (2019) [32] | Moderate |
| McGrath et al. (2019) [38] | Weak |
| Su et al. (2019) [41] | Strong |
| Nàpoles et al. (2019) [29] | Moderate |
| Ivanics et al. (2019) [27] | Moderate |
| Tevaarwerk (2017) [36] | Moderate |
| Rosenberg et al. (2016) [21] | Moderate |
| Jefford et al. (2016) [42] | Strong |
| O’Hea et al. (2016) [37] | Moderate |
| Berman et al. (2016) [35] | Weak |
| Grant et al. (2015) [34] | Weak |
| Jefford et al. (2015) [23] | Moderate |
| Rosales et al. (2014) [22] | Weak |
| Downs-Holmes et al. (2014) [33] | Weak |
| Patt et al. (2013) [28] | Weak |
| Dulko et al. (2013) [24] | Moderate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torreggiani, M.; Maselli, D.; Costi, S.; Guberti, M. Models of Care in Providing Comprehensive Healthcare on Cancer Survivors: A Scoping Review with a TIDieR Checklist Analysis. Int. J. Environ. Res. Public Health 2024, 21, 122. https://doi.org/10.3390/ijerph21020122
Torreggiani M, Maselli D, Costi S, Guberti M. Models of Care in Providing Comprehensive Healthcare on Cancer Survivors: A Scoping Review with a TIDieR Checklist Analysis. International Journal of Environmental Research and Public Health. 2024; 21(2):122. https://doi.org/10.3390/ijerph21020122
Chicago/Turabian StyleTorreggiani, Martina, Deborah Maselli, Stefania Costi, and Monica Guberti. 2024. "Models of Care in Providing Comprehensive Healthcare on Cancer Survivors: A Scoping Review with a TIDieR Checklist Analysis" International Journal of Environmental Research and Public Health 21, no. 2: 122. https://doi.org/10.3390/ijerph21020122
APA StyleTorreggiani, M., Maselli, D., Costi, S., & Guberti, M. (2024). Models of Care in Providing Comprehensive Healthcare on Cancer Survivors: A Scoping Review with a TIDieR Checklist Analysis. International Journal of Environmental Research and Public Health, 21(2), 122. https://doi.org/10.3390/ijerph21020122









