A Framework for the Human-Centered Design of Service Processes Enabled by Medical Devices: A Case Study of Wearable Devices for Parkinson’s Disease
Abstract
1. Introduction
2. Materials and Methods
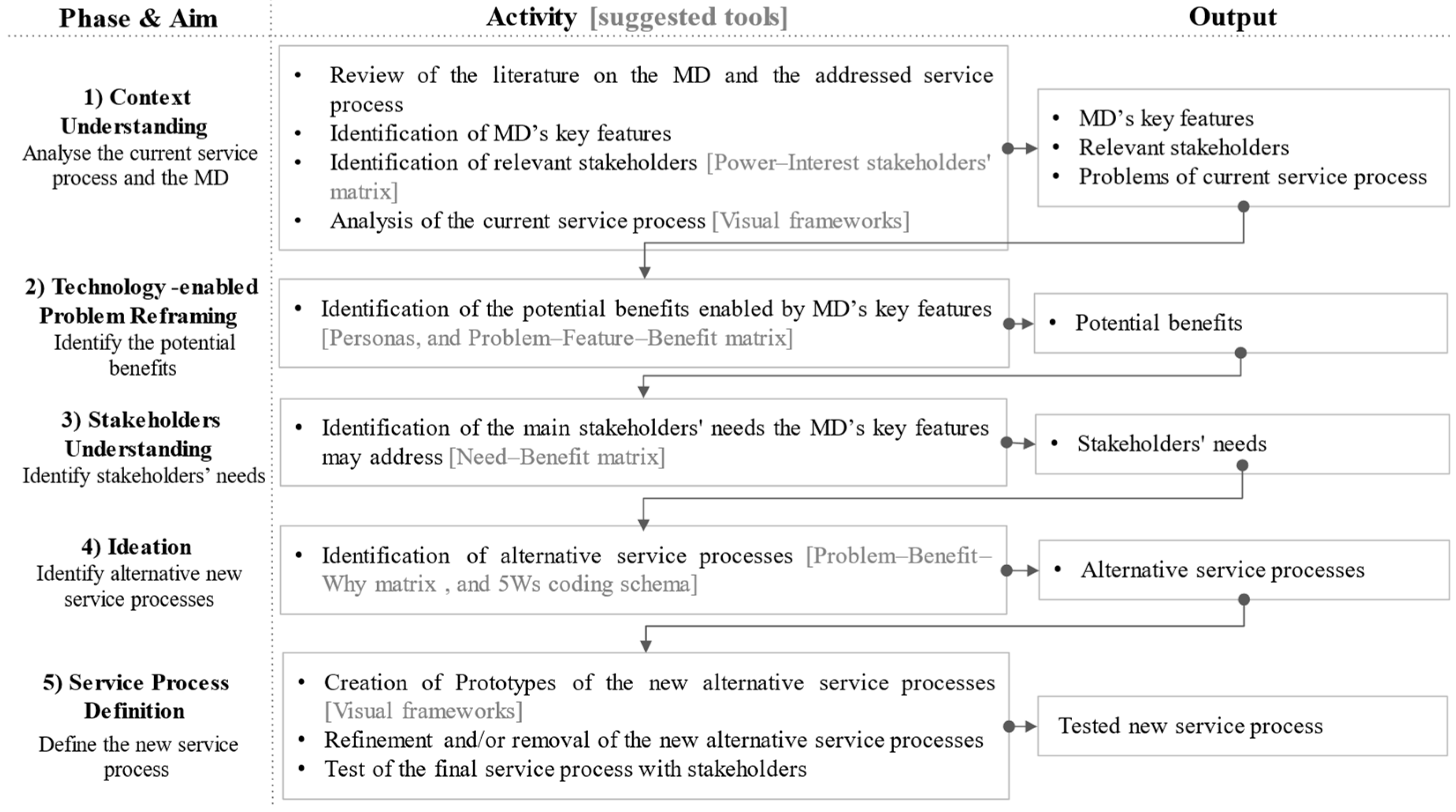
2.1. A Framework for the Design of New Service Processes Enabled by MDs
2.1.1. Phase 1: Context Understanding
2.1.2. Phase 2: Technology-Enabled Problem Reframing
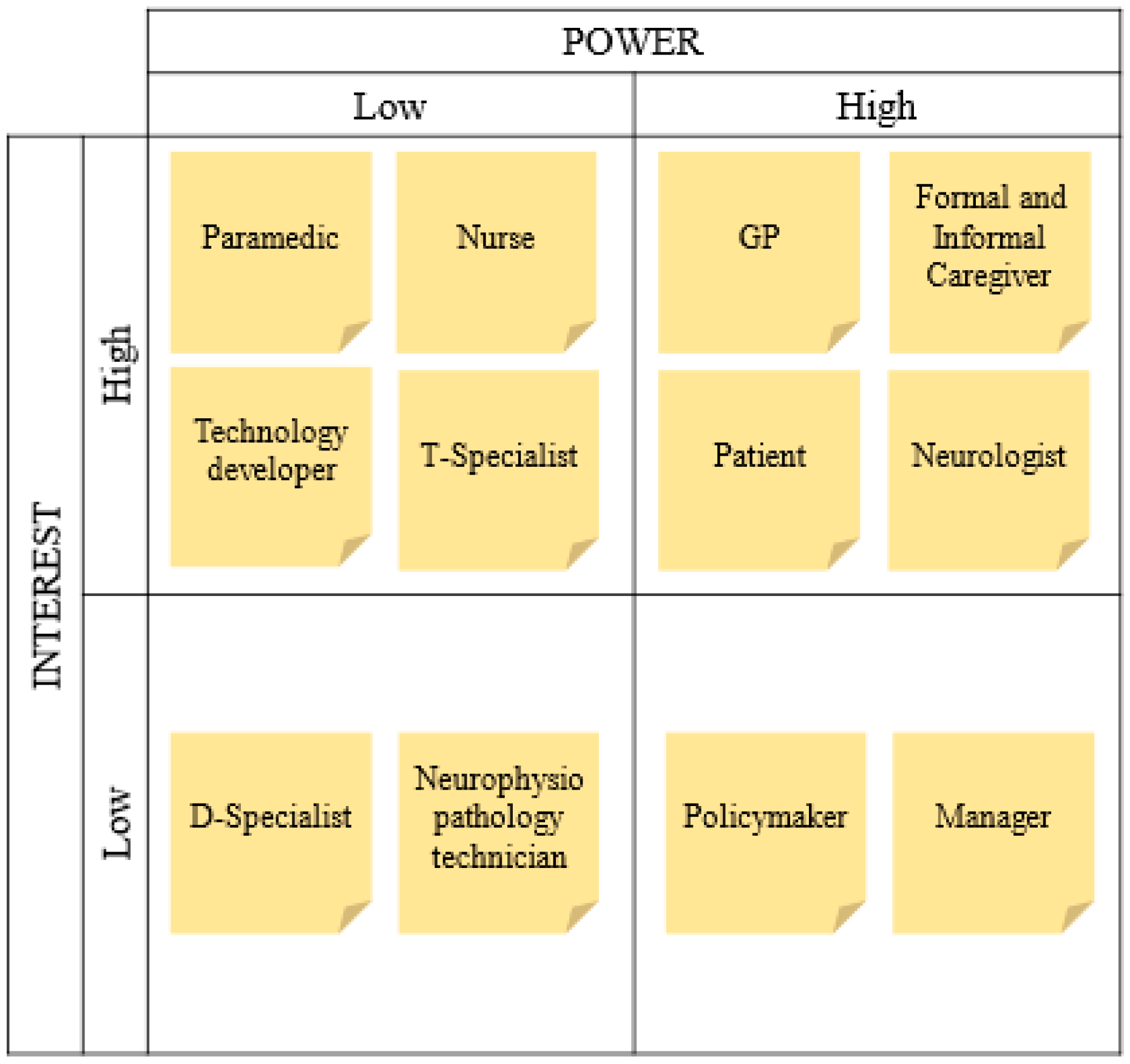
2.1.3. Phase 3: Stakeholders Understanding
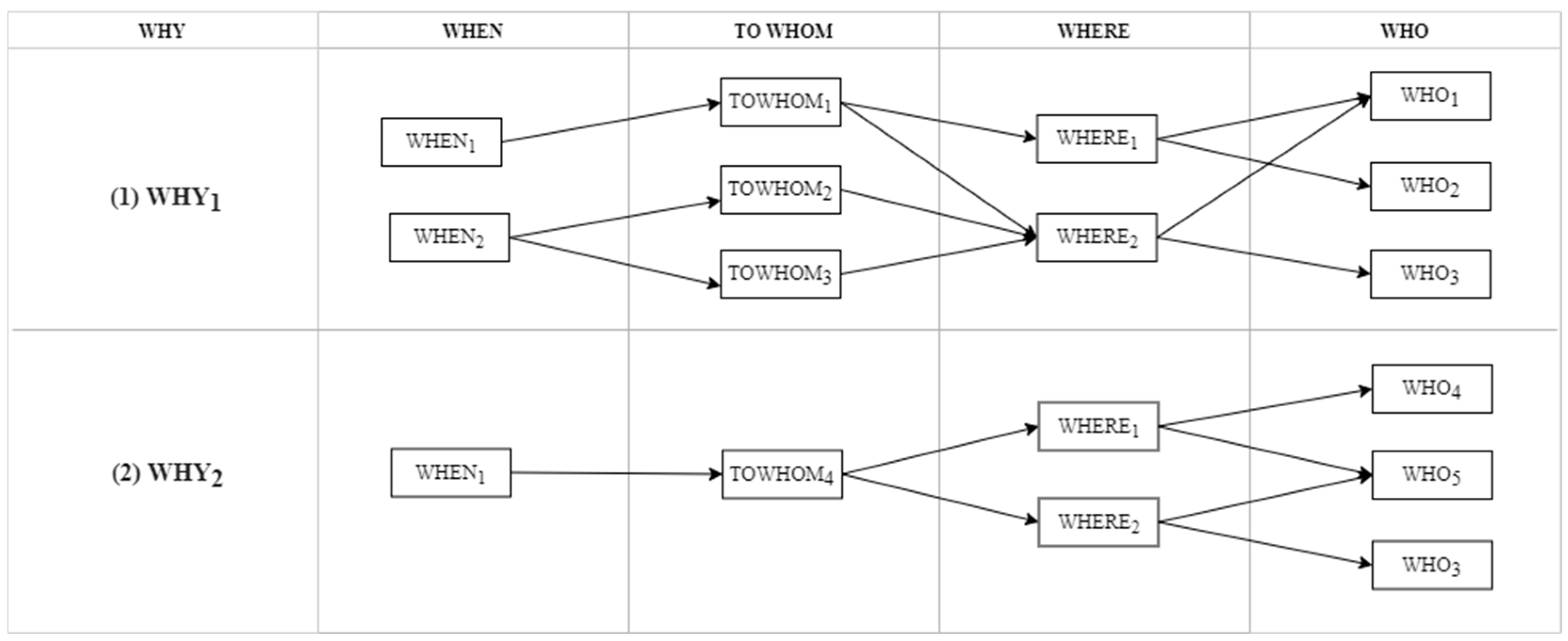
2.1.4. Phase 4: Ideation
2.1.5. Phase 5: Service Process Definition
| Approaches | TED Approaches | HCD Approaches |
|---|---|---|
| Constraints and objectives | Constraints: the MD and the service process are given at the beginning of the design process. Objectives: enhance the service processes by integrating the MD into them (e.g., improving customer experience). | Constraints: the MD is not given at the beginning of the design process, but the targeted service process might be given. Objectives: design an MD that addresses stakeholders’ needs and/or redefine the service to address the stakeholders’ needs. |
| Primary focus | MD functions. | Stakeholders’ needs. |
| Problem emerging when you want to redesign the service given an MD | Starting by identifying the functions and requirements of the MD without considering stakeholders’ needs could forbid the identification of not-easily-foreseeable uses of the MD and could limit the acceptability and desirability of the solutions for stakeholders. | They typically start with identifying stakeholders’ needs. Doing this might lead to identifying needs that cannot be met with the chosen MD. |
| What the proposed five-phase framework inherits | In Phase 1, the MD’s key features and requirements are investigated, and the current service process is analyzed to identify its main problems. |
|
| What the proposed five-phase framework changes |
| Stakeholders’ needs are investigated only in Phase 3 (and not at the beginning of the design process), and the needs analysis focuses only on needs that are linked to the potential benefits offered by the MD’s key features (see the “Need–Benefit matrix” in Appendix C). |
2.2. Case Informants
3. Results
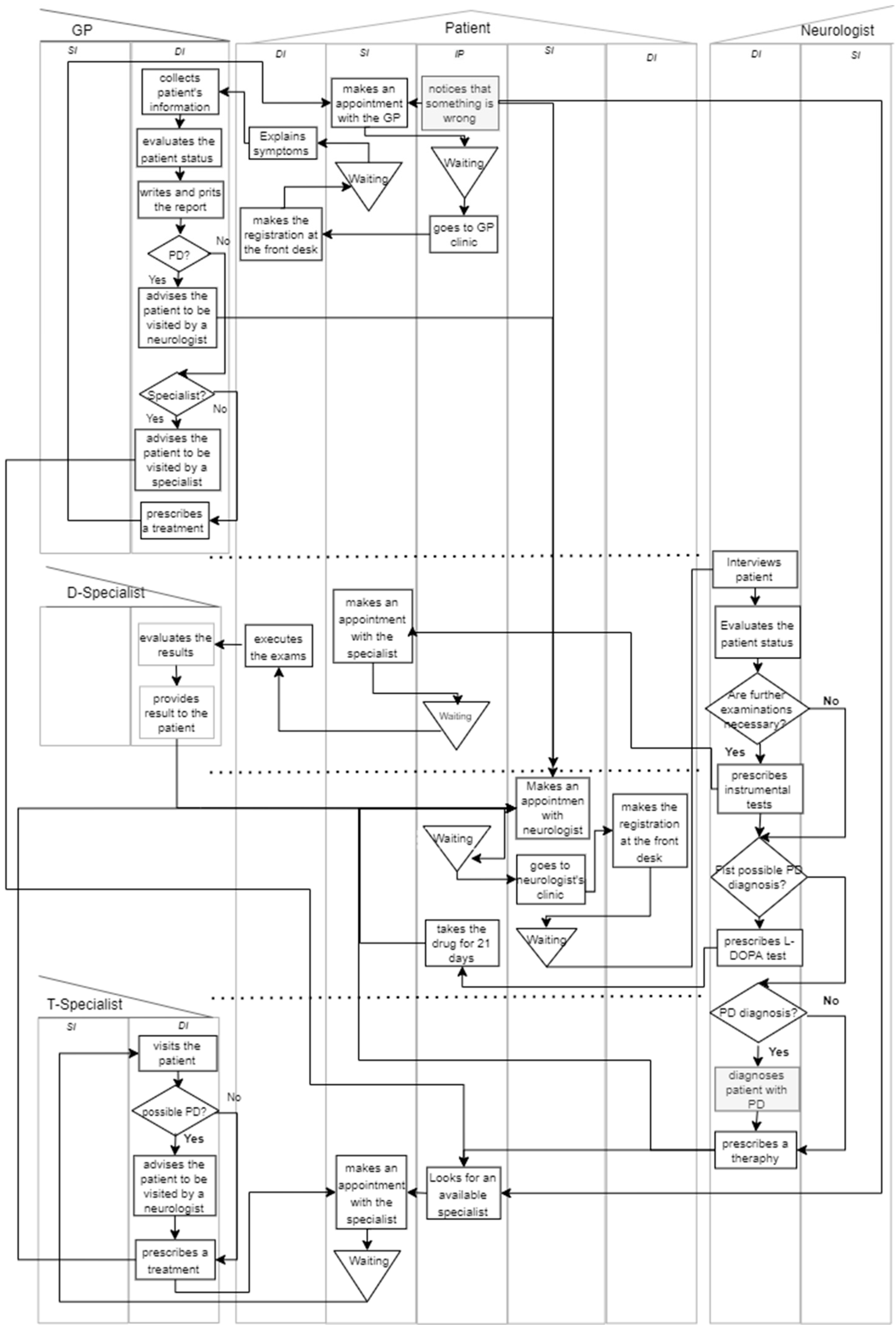
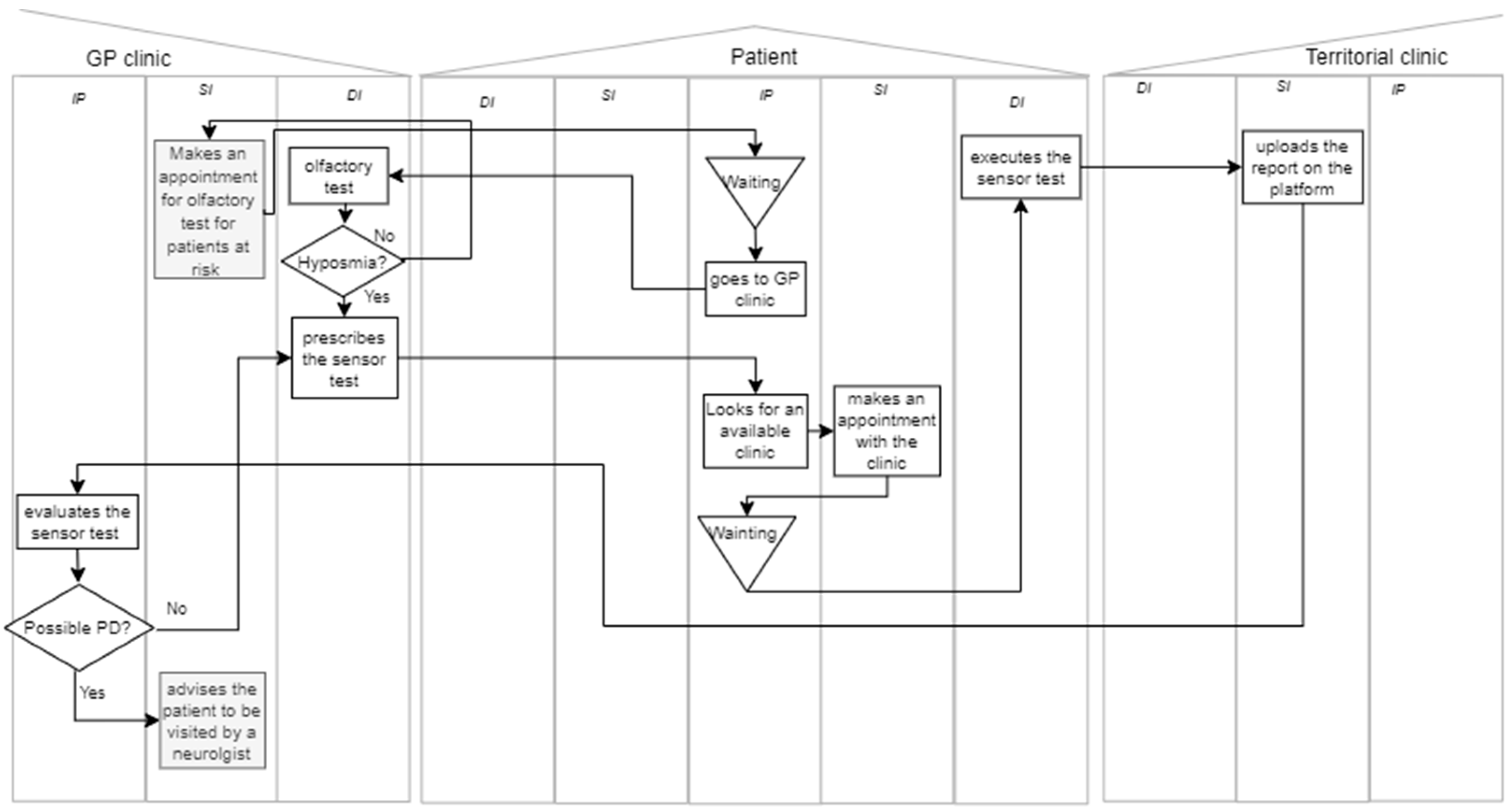
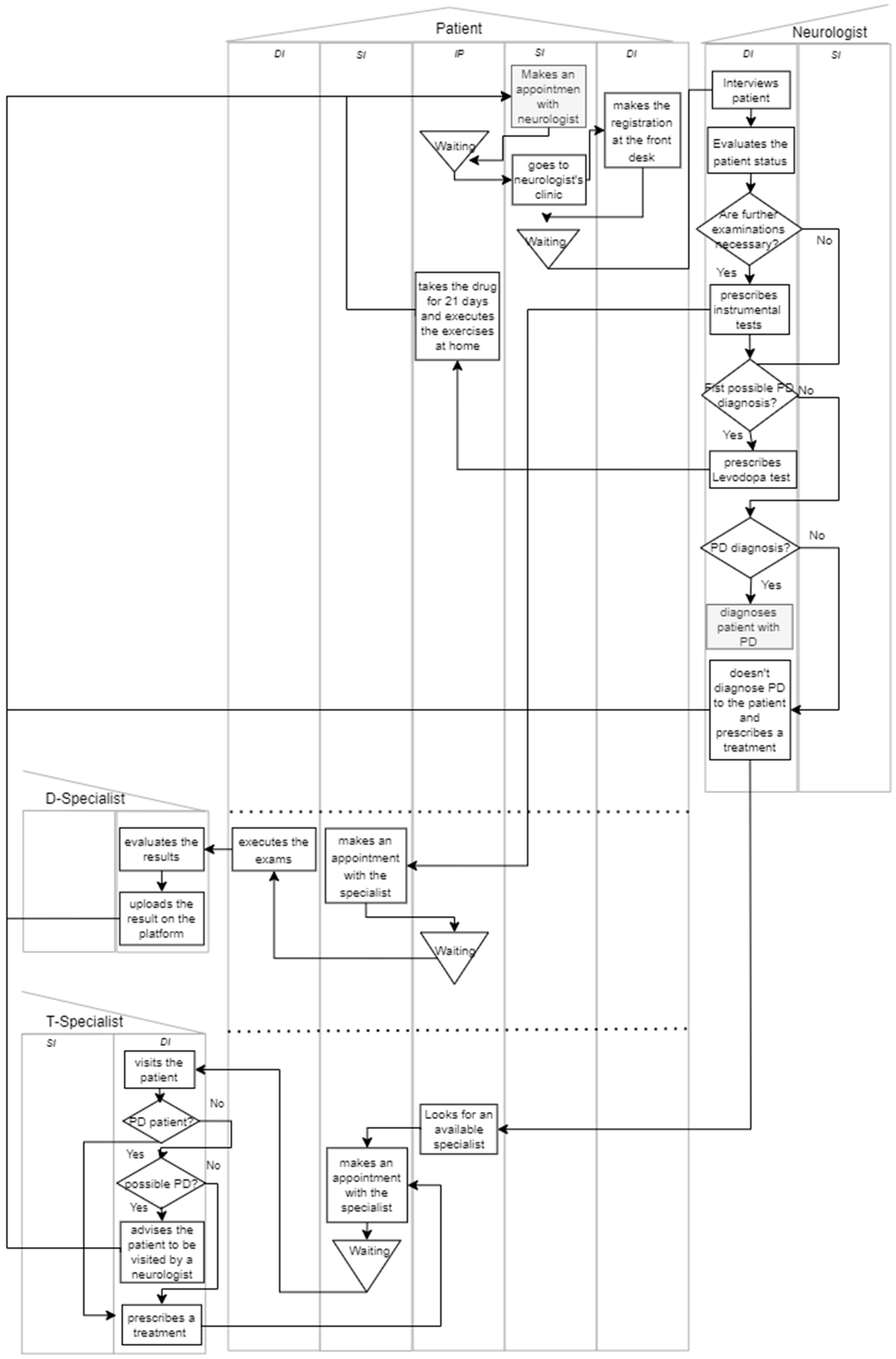
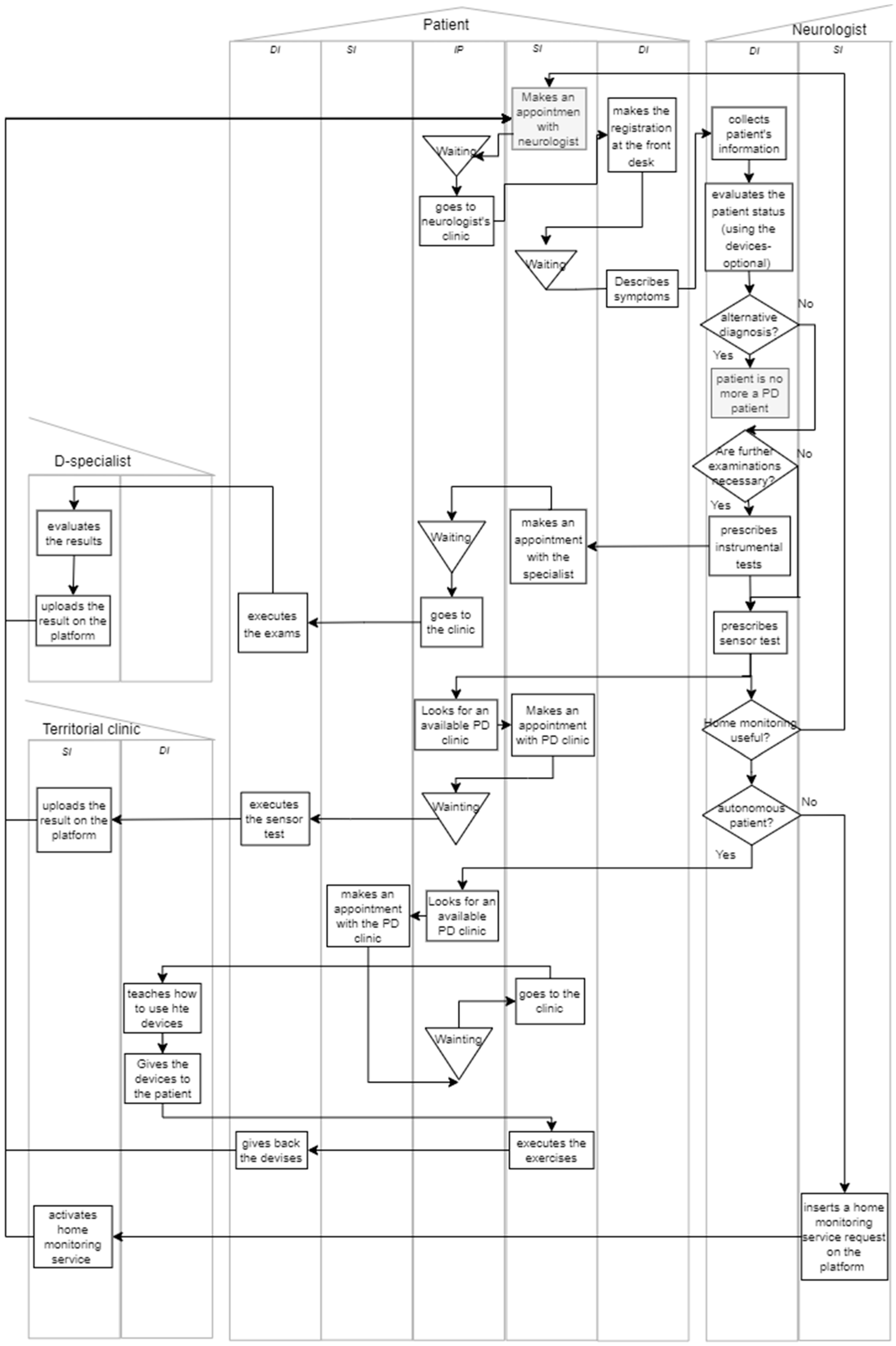
3.1. Phase 1—Context Understanding
3.2. Phase 2—Technology-Enabled Problem Reframing
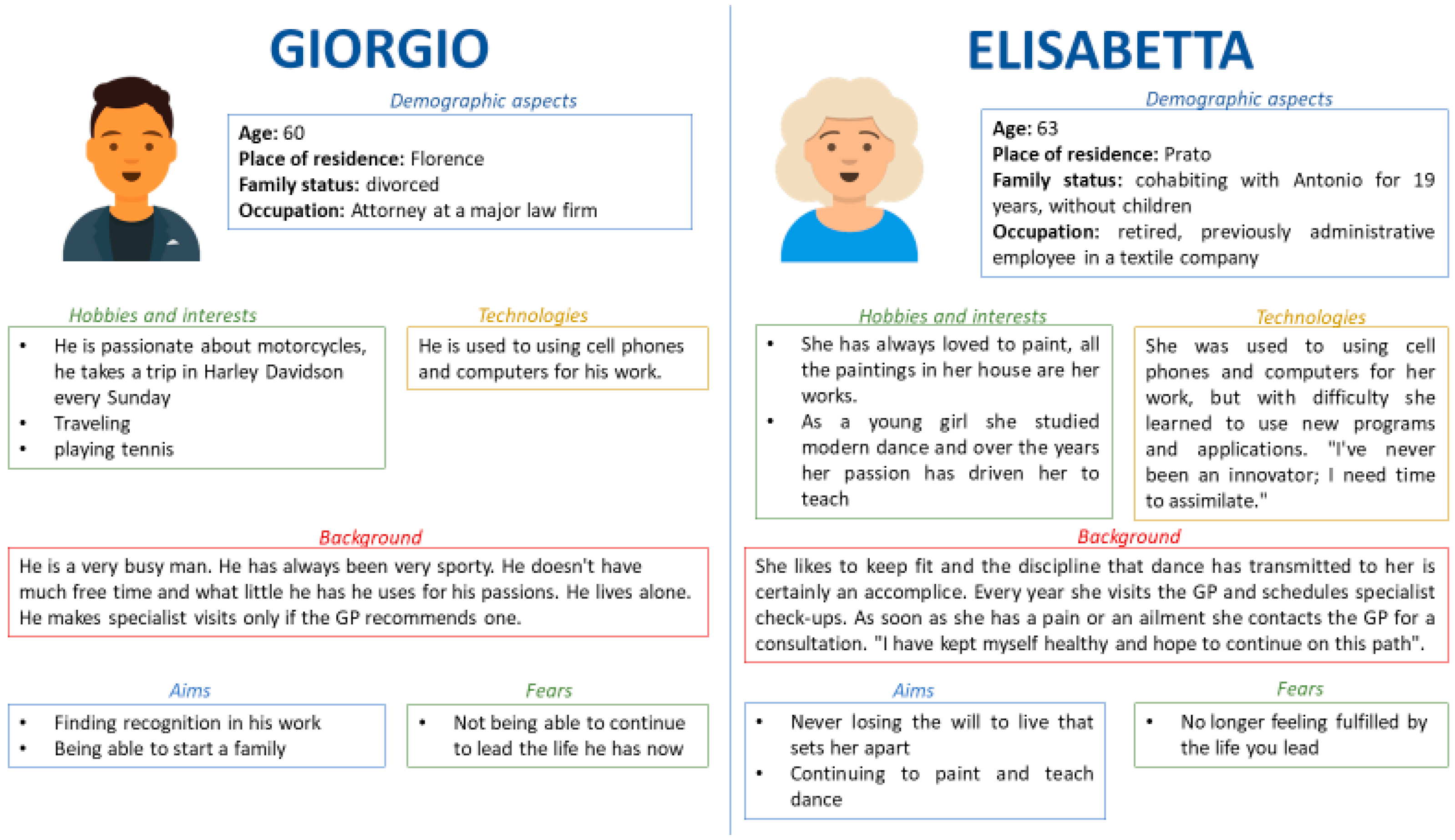
3.3. Phase 3—Stakeholders Understanding
3.4. Phase 4—Ideation
- “How could we diagnose Giorgio with the disease?” (N1)
- “How could we assess Simona’s status accurately and continuously?” (N3, N4)
- “Please, think of other MDs employed in supporting the diagnosis of complex diseases. How might we take inspiration from them to achieve an early diagnosis of PD?” (B1)
- “Please, think of other contexts in which the patients’ status assessment is achieved by performing individual, pre-defined exercises that are the same for each session; can we take inspiration from them?” (B4)
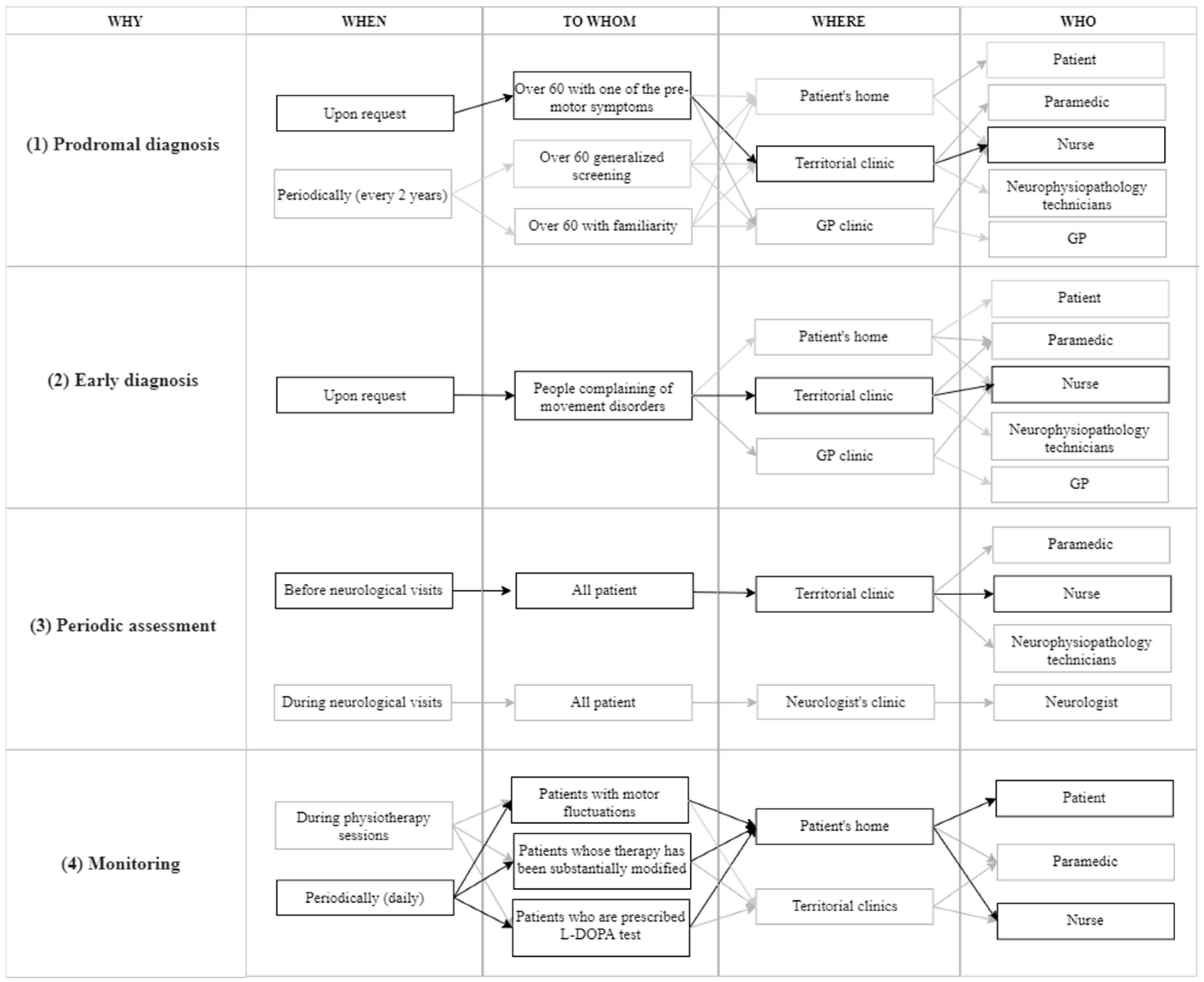
3.5. Phase 5—Service Process Definition
| Why | Decision | Motivation |
|---|---|---|
| [WHY1] Prodromal diagnosis | SensH&F tests are administered to patients over 60 with hyposmia (reduced olfactory sensitivity). |
|
| Olfactory tests are administered by nurses at GP clinics | Olfactory tests are cheap, fast, and easy to perform [80,81]. | |
| Nurses in territorial clinics administer SensH&F tests. |
| |
GP is the care coordinator of this macro-stage:
| The GP is the only one with the opportunity and information to play this role. | |
| [WHY2] Early diagnosis | GPs would prescribe the SensH&F test to people complaining of motor symptoms. | Patients typically go to the GP when they realize they have motor disorders. |
| Nurses in territorial clinics would administer SensH&F tests for patients with motor symptoms. | All reasons given for prodromal diagnosis remain valid. |
| Why | Decision | Motivation |
|---|---|---|
| [WHY3] Periodic assessment | SensH&F test is decoupled from neurological examination:
| The decoupling would reduce the workload for the neurologist (a resource with very limited capacity) while allowing for more frequent monitoring of motor performance. |
| Neurologists would be equipped with SensH&F if they want to double-check the motor performance. | Disagreement among neurologists on trusting the results of SensH&F test administered by others:
| |
| [WHY4] Monitoring | SensH&F tests are administered to patients with motor fluctuations, patients undergoing the L-DOPA test, or patients whose therapy has been substantially changed. | Having the opportunity to monitor motor symptoms of patients undergoing the L-DOPA test or patients whose therapy has been substantially changed would give neurologists essential information [43] |
| Patients (with their caregivers) would self-administer SensH&F tests at home. |
| |
| If patients cannot self-administer the SensH&F test, nurses from territorial clinics would go to patients’ houses to administer it. |
| |
| Data acquired through SensH&F would be saved directly in the patient’s Electronic Health Record. |
|
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

Appendix B

Appendix C
- (1)
- Problem. This column lists the problems within the service process.
- (2)
- Key Feature. This column identifies the MD key features that can mitigate or resolve the listed problems in the first column.
- (3)
- Potential Benefits. This column outlines the anticipated benefits that can be realized when the MD’s key features address specific problems.
| Problem | Key Feature | Potential Benefit |
|---|---|---|
| P1 | K1 | B1 |
| P2 | Kk | |
| … | … | … |
| Pp | K1 | Bb |
| Stakeholders | Needs | Potential Benefits | ||||
|---|---|---|---|---|---|---|
| B1 | B2 | B3 | …. | Bb | ||
| S1 | N1 | X | ||||
| … | … | |||||
| Ss | Nn−1 | X | X | X | ||
| Nn | X | |||||
| Problem | Potential Benefit | Why |
|---|---|---|
| P1 | B1 | WHY1 |
| WHY2s | ||
| P2 | WHY2s | |
| … | … | … |
| Pp | Bb | WHYw |
- (1)
- Why (what could be the aim of the MD in the new service process?);
- (2)
- When (when and how often may the MD be used?);
- (3)
- To Whom (who may be the target population?);
- (4)
- Where (in which setting may the MD be used?);
- (5)
- Who (who may use the MD?).
Appendix D

References
- Foglia, E.; Garagiola, E.; Bellavia, D.; Rossetto, F.; Baglio, F. Digital technology and COVID-19 pandemic: Feasibility and acceptance of an innovative telemedicine platform. Technovation 2024, 130, 102941. [Google Scholar] [CrossRef]
- Pinelli, M.; Manetti, S.; Lettieri, E. Assessing the Social and Environmental Impact of Healthcare Technologies: Towards an Extended Social Return on Investment. Int. J. Environ. Res. Public Health 2023, 20, 5224. [Google Scholar] [CrossRef] [PubMed]
- Cresswell, K.; Sheikh, A. Organizational issues in the implementation and adoption of health information technology innovations: An interpretative review. Int. J. Med. Inform. 2013, 82, e73–e86. [Google Scholar] [CrossRef] [PubMed]
- van Gemert-Pijnen, J.E.; Nijland, N.; van Limburg, M.; Ossebaard, H.C.; Kelders, S.M.; Eysenbach, G.; Seydel, E.R. A Holistic Framework to Improve the Uptake and Impact of eHealth Technologies. J. Med. Internet Res. 2011, 13, e111. [Google Scholar] [CrossRef]
- Bhatia, M.; Sood, S.K. A comprehensive health assessment framework to facilitate IoT-assisted smart workouts: A predictive healthcare perspective. Comput. Ind. 2017, 92–93, 50–66. [Google Scholar] [CrossRef]
- Luis-Martínez, R.; Monje, M.H.G.; Antonini, A.; Sánchez-Ferro, Á.; Mestre, T.A. Technology-Enabled Care: Integrating Multidisciplinary Care in Parkinson’s Disease Through Digital Technology. Front. Neurol. 2020, 11, 575975. [Google Scholar] [CrossRef]
- Alberts, J.L.; Koop, M.M.; McGinley, M.P.; Penko, A.L.; Fernandez, H.H.; Shook, S.; Bermel, R.A.; Machado, A.; Rosenfeldt, A.B. Use of a Smartphone to Gather Parkinson’s Disease Neurological Vital Signs during the COVID-19 Pandemic. Mir, P.; editor. Parkinsons Dis. 2021, 2021, 5534282. [Google Scholar]
- Stara, V.; Vera, B.; Bolliger, D.; Paolini, S.; de Jong, M.; Felici, E.; Koenderink, S.; Rossi, L.; Von Doellen, V.; di Rosa, M. Toward the Integration of Technology-Based Interventions in the Care Pathway for People with Dementia: A Cross-National Study. Int. J. Environ. Res. Public Health 2021, 18, 10405. [Google Scholar] [CrossRef]
- LaMonica, H.M.; Davenport, T.A.; Ottavio, A.; Rowe, S.C.; Cross, S.P.; Iorfino, F.; Jackson, T.A.; Easton, M.A.; Melsness, J.; Hickie, I.B. Optimising the integration of technology-enabled solutions to enhance primary mental health care: A service mapping study. BMC Health Serv. Res. 2021, 21, 68. [Google Scholar] [CrossRef]
- Patrício, L.; Grenha Teixeira, J.; Vink, J. A service design approach to healthcare innovation: From decision-making to sense-making and institutional change. AMS Rev. 2019, 9, 115–120. [Google Scholar] [CrossRef]
- Rampioni, M.; Moșoi, A.A.; Rossi, L.; Moraru, S.A.; Rosenberg, D.; Stara, V. A Qualitative Study toward Technologies for Active and Healthy Aging: A Thematic Analysis of Perspectives among Primary, Secondary, and Tertiary End Users. Int. J. Environ. Res. Public Health 2021, 18, 7489. [Google Scholar] [CrossRef] [PubMed]
- Edvardsson, D.; Innes, A. Measuring Person-centered Care: A Critical Comparative Review of Published Tools. Gerontologist 2010, 50, 834–846. [Google Scholar] [CrossRef] [PubMed]
- Beach, M.C.; Inui, T. Relationship-centered Care. A Constructive Reframing. J. Gen. Intern. Med. 2006, 21, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, T.S.J.; Ekman, I.; Olsson, L.E.; Dudas, K.; Carlström, E. Organizational culture and the implementation of person centered care: Results from a change process in Swedish hospital care. Health Policy 2012, 108, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Dosi, C.; Mattarelli, E.; Vignoli, M. Prototypes as identity markers: The double-edged role of prototypes in multidisciplinary innovation teams. Creat. Innov. Manag. 2020, 29, 648–666. [Google Scholar] [CrossRef]
- Wannheden, C.; Revenäs, Å. How People with Parkinson’s Disease and Health Care Professionals Wish to Partner in Care Using eHealth: Co-Design Study. J. Med. Internet Res. 2020, 22, e19195. [Google Scholar] [CrossRef]
- Flores, E.J.; Mull, N.K.; Lavenberg, J.G.; Mitchell, M.D.; Leas, B.F.; Williams, A.; Brennan, P.J.; A Umscheid, C. Using a 10-step framework to support the implementation of an evidence-based clinical pathways programme. BMJ Qual. Saf. 2019, 28, 476–485. [Google Scholar] [CrossRef]
- Patrício, L.; Sangiorgi, D.; Mahr, D.; Čaić, M.; Kalantari, S.; Sundar, S. Leveraging service design for healthcare transformation: Toward people-centered, integrated, and technology-enabled healthcare systems. J. Serv. Manag. 2020, 31, 889–909. [Google Scholar] [CrossRef]
- Bertolotti, F.; Tagliaventi, M.R.; Dosi, C. From lone wolves to members of the pack: Exploring interpersonal identity work within identity workspaces. J. Organ. Behav. 2022, 43, 620–642. [Google Scholar] [CrossRef]
- Lebovitz, S.; Lifshitz-Assaf, H.; Levina, N. To Engage or Not to Engage with AI for Critical Judgments: How Professionals Deal with Opacity When Using AI for Medical Diagnosis. Organ. Sci. 2022, 33, 126–148. [Google Scholar] [CrossRef]
- Steen, M.; Manschot, M.; de Koning, N. Benefits of co-design in service design projects. Int. J. Des. 2011, 5, 53–60. [Google Scholar]
- Vignoli, M.; Dosi, C.; Balboni, B. Design thinking mindset: Scale development and validation. Stud. High. Educ. 2023, 48, 926–940. [Google Scholar] [CrossRef]
- Vaisson, G.; Provencher, T.; Dugas, M.; Trottier, M.; Dansokho, S.C.; Colquhoun, H.; Fagerlin, A.; Giguere, A.M.C.; Hakim, H.; Haslett, L.; et al. User Involvement in the Design and Development of Patient Decision Aids and Other Personal Health Tools: A Systematic Review. Med. Decis. Mak. 2021, 41, 261–274. [Google Scholar] [CrossRef]
- Elbers, S.; van Gessel, C.; Renes, R.J.; van der Lugt, R.; Wittink, H.; Hermsen, S. Innovation in Pain Rehabilitation Using Co-Design Methods During the Development of a Relapse Prevention Intervention: Case Study. J. Med. Internet Res. 2021, 23, e18462. [Google Scholar] [CrossRef]
- Micheli, P.; Wilner, S.J.S.; Bhatti, S.H.; Mura, M.; Beverland, M.B. Doing Design Thinking: Conceptual Review, Synthesis, and Research Agenda. J. Prod. Innov. Manag. 2019, 36, 124–148. [Google Scholar] [CrossRef]
- Panwar, T.; Khan, K. Integrating Design Thinking in Service Design Process: A Conceptual Review. J. Des. Think. 2021, 2, 23–36. [Google Scholar]
- Breeman, L.D.; Keesman, M.; Atsma, D.E.; Chavannes, N.H.; Janssen, V.; van Gemert-Pijnen, L.; Kemps, H.; Kraaij, W.; Rauwers, F.; Reijnders, T.; et al. A multi-stakeholder approach to eHealth development: Promoting sustained healthy living among cardiovascular patients. Int. J. Med. Inform. 2021, 147, 104364. [Google Scholar] [CrossRef]
- Bacchin, D.; Pernice, G.F.A.; Pierobon, L.; Zanella, E.; Sardena, M.; Malvestio, M.; Gamberini, L. Co-Design in Electrical Medical Beds with Caregivers. Int. J. Environ. Res. Public Health 2022, 19, 16353. [Google Scholar] [CrossRef]
- Szewczenko, A.; Lach, E.; Bursiewicz, N.; Chuchnowska, I.; Widzisz-Pronobis, S.; Sanigórska, M.; Elsner, K.; Bal, D.; Sutor, M.; Włodarz, J.; et al. Urban Therapy—Urban Health Path as an Innovative Urban Function to Strengthen the Psycho-Physical Condition of the Elderly. Int. J. Environ. Res. Public Health 2023, 20, 6081. [Google Scholar] [CrossRef]
- Pousada García, T.; Garabal-Barbeira, J.; Porto Trillo, P.; Vilar Figueira, O.; Novo Díaz, C.; Pereira Loureiro, J. A Framework for a New Approach to Empower Users Through Low-Cost and Do-It-Yourself Assistive Technology. Int. J. Environ. Res. Public Health 2021, 18, 3039. [Google Scholar] [CrossRef]
- Cocchi, N.; Dosi, C.; Vignoli, M. Tech to Organization. Assessing and designing technology adoption with design thinking. Cern. IDEASQUARE J. Exp. Innov. 2023, 3, 20–31. [Google Scholar] [CrossRef]
- Solem, I.K.L.; Varsi, C.; Eide, H.; Kristjansdottir, O.B.; Børøsund, E.; Schreurs, K.M.G.; Waxenberg, L.B.; E Weiss, K.; Morrison, E.J.; Haaland-Øverby, M.; et al. A User-Centered Approach to an Evidence-Based Electronic Health Pain Management Intervention for People With Chronic Pain: Design and Development of EPIO. J. Med. Internet Res. 2020, 22, e15889. [Google Scholar] [CrossRef] [PubMed]
- Harte, R.; Glynn, L.; Rodríguez-Molinero, A.; Baker, P.M.; Scharf, T.; Quinlan, L.R.; ÓLaighin, G. A Human-Centered Design Methodology to Enhance the Usability, Human Factors, and User Experience of Connected Health Systems: A Three-Phase Methodology. JMIR Hum. Factors 2017, 4, e8. [Google Scholar] [CrossRef] [PubMed]
- Cantamessa, M.; Montagna, F.; Cascini, G. Design for innovation-A methodology to engineer the innovation diffusion into the development process. Comput. Ind. 2016, 75, 46–57. [Google Scholar] [CrossRef]
- Milton, A.C.; Hambleton, A.; Dowling, M.; Roberts, A.E.; Davenport, T.; Hickie, I. Technology-Enabled Reform in a Nontraditional Mental Health Service for Eating Disorders: Participatory Design Study. J. Med. Internet Res. 2021, 23, e19532. [Google Scholar] [CrossRef]
- Korpershoek, Y.J.G.; Hermsen, S.; Schoonhoven, L.; Schuurmans, M.J.; Trappenburg, J.C.A. User-Centered Design of a Mobile Health Intervention to Enhance Exacerbation-Related Self-Management in Patients With Chronic Obstructive Pulmonary Disease (Copilot): Mixed Methods Study. J. Med. Internet Res. 2020, 22, e15449. [Google Scholar] [CrossRef]
- van Limburg, M.; van Gemert-Pijnen, J.E.W.C.; Nijland, N.; Ossebaard, H.C.; Hendrix, R.M.G.; Seydel, E.R. Why Business Modeling is Crucial in the Development of eHealth Technologies. J. Med. Internet Res. 2011, 13, e124. [Google Scholar] [CrossRef]
- Maremmani, C.; Rovini, E.; Salvadori, S.; Pecori, A.; Pasquini, J.; Ciammola, A.; Rossi, S.; Berchina, G.; Monastero, R.; Cavallo, F. Hands–feet wireless devices: Test–retest reliability and discriminant validity of motor measures in Parkinson’s disease telemonitoring. Acta Neurol. Scand. 2022, 146, 304–317. [Google Scholar] [CrossRef]
- Ou, Z.; Pan, J.; Tang, S.; Duan, D.; Yu, D.; Nong, H.; Wang, Z. Global Trends in the Incidence, Prevalence, and Years Lived With Disability of Parkinson’s Disease in 204 Countries/Territories From 1990 to 2019. Front. Public Health 2021, 9, 776847. [Google Scholar] [CrossRef]
- Martínez-Martín, P.; Forjaz, M.J.; Frades-Payo, B.; Rusiñol, A.B.; Fernández-García, J.M.; Benito-León, J.; Arillo, V.C.; Barberá, M.A.; Sordo, M.P.; Catalán, M.J. Caregiver burden in Parkinson’s disease. Mov. Disord. 2007, 22, 924–931. [Google Scholar] [CrossRef]
- Roger, K.S.; Medved, M. Living with Parkinson’s disease—Managing identity together. Int. J. Qual. Stud. Health Well-Being 2010, 5, 5129. [Google Scholar] [CrossRef] [PubMed]
- Del Din, S.; Elshehabi, M.; Galna, B.; Hobert, M.A.; Warmerdam, E.; Suenkel, U.; Brockmann, K.; Metzger, F.; Hansen, C.; Berg, D.; et al. Gait analysis with wearables predicts conversion to Parkinson disease. Ann. Neurol. 2019, 86, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Rovini, E.; Maremmani, C.; Cavallo, F. How Wearable Sensors Can Support Parkinson’s Disease Diagnosis and Treatment: A Systematic Review. Front. Neurosci. 2017, 11, 555. [Google Scholar] [CrossRef]
- Dominey, T.; Kehagia, A.A.; Gorst, T.; Pearson, E.; Murphy, F.; King, E.; Carroll, C. Introducing the Parkinson’s KinetiGraph into Routine Parkinson’s Disease Care: A 3-Year Single Centre Experience. J. Parkinsons Dis. 2020, 10, 1827–1832. [Google Scholar] [CrossRef]
- Evans, L.; Mohamed, B.; Thomas, E.C. Using telemedicine and wearable technology to establish a virtual clinic for people with Parkinson’s disease. BMJ Open Qual. 2020, 9, e001000. [Google Scholar] [CrossRef]
- Roberts, J.P.; Fisher, T.R.; Trowbridge, M.J.; Bent, C. A design thinking framework for healthcare management and innovation. Healthcare 2016, 4, 11–14. [Google Scholar] [CrossRef]
- Liedtka, J.; Ogilvie, T. Designing for Growth: A Design Thinking Toolkit for Managers; Psychological Science; Columbia Business School Publishing: New York, NY, USA, 2011; Volume 25, pp. 1682–1690. [Google Scholar]
- Sampson, S.E. Essentials of Service Design and Innovation-Developing High-Value Service Business with PCN Analysis, 4th ed.; CreateSpace Independent Publishing Platform: Provo, UT, USA, 2015. [Google Scholar]
- Sampson, S.E. Visualizing Service Operations. J. Serv. Res. 2012, 15, 182–198. [Google Scholar] [CrossRef]
- Sampson, S.E.; Schmidt, G.; Gardner, J.W.; Van Orden, J. Process Coordination Within a Health Care Service Supply Network. J. Bus. Logist. 2015, 36, 355–373. [Google Scholar] [CrossRef]
- Reed, M.S.; Curzon, R. Stakeholder mapping for the governance of biosecurity: A literature review. J. Integr. Environ. Sci. 2015, 12, 15–38. [Google Scholar] [CrossRef]
- Brugha, R. Stakeholder analysis: A review. Health Policy Plan. 2000, 15, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Dosi, C.; Iori, M.; Kramer, A.; Vignoli, M. Successful implementation of discrete event simulation: Integrating design thinking and simulation approach in an emergency department. Prod. Plan. Control. 2021, 34, 1233–1247. [Google Scholar] [CrossRef]
- Karpathakis, K.; Libow, G.; Potts, H.W.W.; Dixon, S.; Greaves, F.; Murray, E. An Evaluation Service for Digital Public Health Interventions: User-Centered Design Approach. J. Med. Internet Res. 2021, 23, e28356. [Google Scholar] [CrossRef]
- Yu, F.; Pasinelli, M.; Brem, A. Prototyping in theory and in practice: A study of the similarities and differences between engineers and designers. Creat. Innov. Manag. 2018, 27, 121–132. [Google Scholar] [CrossRef]
- Donati, C.; Vignoli, M. How tangible is your prototype? Designing the user and expert interaction. Int. J. Interact. Des. Manuf. 2015, 9, 107–114. [Google Scholar] [CrossRef]
- Dai, H.; Cai, G.; Lin, Z.; Wang, Z.; Ye, Q. Validation of Inertial Sensing-Based Wearable Device for Tremor and Bradykinesia Quantification. IEEE J. Biomed. Health Inform. 2021, 25, 997–1005. [Google Scholar] [CrossRef]
- Ozanne, A.; Johansson, D.; Hällgren Graneheim, U.; Malmgren, K.; Bergquist, F.; Alt Murphy, M. Wearables in epilepsy and Parkinson’s disease—A focus group study. Acta Neurol. Scand. 2018, 137, 188–194. [Google Scholar] [CrossRef]
- Mancini, M.; Shah, V.V.; Stuart, S.; Curtze, C.; Horak, F.B.; Safarpour, D.; Nutt, J.G. Measuring freezing of gait during daily-life: An open-source, wearable sensors approach. J. Neuroeng. Rehabil. 2021, 18, 1. [Google Scholar] [CrossRef]
- Rovini, E.; Galperti, G.; Lorenzon, L.; Radi, L.; Fiorini, L.; Cianchetti, M.; Cavallo, F. Design of a novel wearable system for healthcare applications: Applying the user-centred design approach to SensHand device. Int. J. Interact. Des. Manuf. 2023, 18, 591–607. [Google Scholar] [CrossRef]
- Goetz, C.G.; Fahn, S.; Martinez-Martin, P.; Poewe, W.; Sampaio, C.; Stebbins, G.T.; Stern, M.B.; Tilley, B.C.; Dodel, R.; Dubois, B.; et al. The MDS-sponsored Revision of the Unified Parkinson’s Disease Rating Scale. 2008. Available online: https://www.movementdisorders.org/MDS-Files1/PDFs/Rating-Scales/MDS-UPDRS_English_FINAL.pdf (accessed on 8 October 2024).
- Regione Toscana. Percorso per pazienti affetti da Parkinson. 2013. Available online: https://www.regione.toscana.it/documents/10180/12143253/Allegato+Parere+n.+23-2013+ (accessed on 8 October 2024).
- Giunta Regionale della regione Puglia. DGR n.740/2019. Patto per la Puglia Azioni “Infrastrutture per la Sanità”. 2019. Available online: https://burp.regione.puglia.it/documents/20135/1344245/DEL_2041_2019.pdf/52847e3a-229d-a999-c55a-549f7f0540a2?t=1623053965570 (accessed on 8 October 2024).
- Tenison, E.; Smink, A.; Redwood, S.; Darweesh, S.; Cottle, H.; van Halteren, A.; Haak, P.v.D.; Hamlin, R.; Ypinga, J.; Bloem, B.R.; et al. Proactive and Integrated Management and Empowerment in Parkinson’s Disease: Designing a New Model of Care. Parkinsons Dis. 2020, 2020, 8673087. [Google Scholar] [CrossRef]
- van Halteren, A.D.; Munneke, M.; Smit, E.; Thomas, S.; Bloem, B.R.; Darweesh, S.K.L. Personalized Care Management for Persons with Parkinson’s Disease. Bloem, B.R.; Brundin, P.; editors. J. Park. Dis. 2020, 10, S11–S20. [Google Scholar]
- Candiani, G.; Villa, R. Diagnosi e Terapia Della Malattia di Parkinson. 2013. Available online: https://www.sigg.it/wp-content/uploads/2018/09/Linee-guida-Diagnosi-e-terapia-della-malattia-di-Parkinson.pdf (accessed on 8 October 2024).
- Bloem, B.R.; Henderson, E.J.; Dorsey, E.R.; Okun, M.S.; Okubadejo, N.; Chan, P.; Andrejack, J.; Darweesh, S.K.L.; Munneke, M. Integrated and patient-centred management of Parkinson’s disease: A network model for reshaping chronic neurological care. Lancet Neurol. 2020, 19, 623–634. [Google Scholar] [CrossRef] [PubMed]
- Hatano, T.; Kubo, S.I.; Shimo, Y.; Nishioka, K.; Hattori, N. Unmet Needs of Patients with Parkinson’s Disease: Interview Survey of Patients and Caregivers. J. Int. Med. Res. 2009, 37, 717–726. [Google Scholar] [CrossRef] [PubMed]
- Plouvier, A.O.A.; Hartman, T.C.O.; de Bont, O.A.; Maandag, S.; Bloem, B.R.; van Weel, C.; Lagro-Janssen, A.L.M. The diagnostic pathway of Parkinson’s disease: A cross-sectional survey study of factors influencing patient dissatisfaction. BMC Fam. Pract. 2017, 18, 83. [Google Scholar] [CrossRef] [PubMed]
- Sampson, S.E. A Strategic Framework for Task Automation in Professional Services. J. Serv. Res. 2021, 24, 122–140. [Google Scholar] [CrossRef]
- Wärnestål, P.; Svedberg, P.; Lindberg, S.; Nygren, J.M. Effects of Using Child Personas in the Development of a Digital Peer Support Service for Childhood Cancer Survivors. J. Med. Internet Res. 2017, 19, e161. [Google Scholar] [CrossRef]
- Aronoff-Spencer, E.; McComsey, M.; Chih, M.-Y.; Hubenko, A.; Baker, C.; Kim, J.; Ahern, D.K.; Gibbons, M.C.; A Cafazzo, J.; Nyakairu, P.; et al. Designing a Framework for Remote Cancer Care Through Community Co-design: Participatory Development Study. J. Med. Internet Res. 2022, 24, e29492. [Google Scholar] [CrossRef]
- Berry, L.L.; Attai, D.J.; Scammon, D.L.; Awdish, R.L.A. When the Aims and the Ends of Health Care Misalign. J. Serv. Res. 2022, 25, 160–184. [Google Scholar] [CrossRef]
- Jiang, S.; Hu, J.; Wood, K.L.; Luo, J. Data-Driven Design-By-Analogy: State-of-the-Art and Future Directions. J. Mech. Des. 2022, 144, 020801. [Google Scholar] [CrossRef]
- Liedtka, J.; Ogilvie, T.; Brozenske, R. The Designing for Growth-Field Book (a Step-by-Step Project Guide); Columbia Business School Pub.: New York, NY, USA, 2019. [Google Scholar]
- Rovini, E.; Maremmani, C.; Cavallo, F. A Wearable System to Objectify Assessment of Motor Tasks for Supporting Parkinson’s Disease Diagnosis. Sensors 2020, 20, 2630. [Google Scholar] [CrossRef]
- Maremmani, C.; Cavallo, F.; Purcaro, C.; Rossi, G.; Salvadori, S.; Rovini, E.; Esposito, D.; Pieroni, A.; Ramat, S.; Vanni, P.; et al. Combining olfactory test and motion analysis sensors in Parkinson’s disease preclinical diagnosis: A pilot study. Acta Neurol. Scand. 2018, 137, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Postuma, R.B.; Berg, D. Advances in markers of prodromal Parkinson’s disease. Nat. Rev. Neurol. 2016, 12, 622–634. [Google Scholar] [CrossRef] [PubMed]
- Neikrug, A.B.; Ancoli-Israel, S. Diagnostic tools for REM sleep behavior disorder. Sleep. Med. Rev. 2012, 16, 415–429. [Google Scholar] [CrossRef] [PubMed]
- Maremmani, C.; Rossi, G.; Tambasco, N.; Fattori, B.; Pieroni, A.; Ramat, S.; Napolitano, A.; Vanni, P.; Serra, P.; Piersanti, P.; et al. The validity and reliability of the Italian Olfactory Identification Test (IOIT) in healthy subjects and in Parkinson’s disease patients. Park. Relat. Disord. 2012, 18, 788–793. [Google Scholar] [CrossRef]
- Hummel, T.; Kobal, G.; Gudziol, H.; Mackay-Sim, A. Normative data for the “Sniffin’ Sticks” including tests of odor identification, odor discrimination, and olfactory thresholds: An upgrade based on a group of more than 3,000 subjects. Eur. Arch. Oto-Rhino-Laryngol. 2007, 264, 237–243. [Google Scholar] [CrossRef]
- Presidenza del Consiglio dei Ministri. Piano Nazionale di Ripresa e Resilienza [Internet]. 2021. Available online: https://www.governo.it/sites/governo.it/files/PNRR.pdf (accessed on 8 October 2024).
- Ministero della Salute. Piano Nazionale della Cronicità. 2016. Available online: http://www.salute.gov.it/imgs/C_17_pubblicazioni_2584_allegato.pdf (accessed on 8 October 2024).
- Yang, J.J.; Li, J.; Mulder, J.; Wang, Y.; Chen, S.; Wu, H.; Wang, Q.; Pan, H. Emerging information technologies for enhanced healthcare. Comput. Ind. 2015, 69, 3–11. [Google Scholar] [CrossRef]
- Bitner, M.J.; Ostrom, A.L.; Morgan, F.N.; Bitner, M.J.; Ostrom, A.L.; Morgan, F.N. Service Blueprinting: A Practical Technique for Service Innovation. Calif. Manag. Rev. 2008, 50, 66–94. [Google Scholar] [CrossRef]
- Matthias, O.; Brown, S. Implementing operations strategy through Lean processes within health care: The example of NHS in the UK. Int. J. Oper. Prod. Manag. 2016, 36, 1435–1457. [Google Scholar] [CrossRef]
- Vanhaecht, K.; Van Gerven, E.; Deneckere, S.; Lodewijckx, C.; Janssen, I.; van Zelm, V.; Boto, P.; Mendes, R.V.; Panella, M.; Biringer, E.; et al. The 7-phase method to design, implement and evaluate care pathways. Int. J. Pers. Cent. Med. 2012, 2, 341–351. [Google Scholar]
- Visintin, F.; Cappanera, P.; Banditori, C.; Danese, P. Development and implementation of an operating room scheduling tool: An action research study. Prod. Plan. Control 2017, 28, 758–775. [Google Scholar] [CrossRef]
- Visintin, F.; Caprara, C.; Puggelli, F. Experimental design and simulation applied to a paediatric emergency department: A case study. Comput. Ind. Eng. 2019, 128, 755–781. [Google Scholar] [CrossRef]
- Cappanera, P.; Visintin, F.; Banditori, C. Addressing conflicting stakeholders’ priorities in surgical scheduling by goal programming. Flex. Serv. Manuf. J. 2018, 30, 252–271. [Google Scholar] [CrossRef]
- Roshanghalb, A.; Lettieri, E.; Aloini, D.; Cannavacciuolo, L.; Gitto, S.; Visintin, F. What evidence on evidence-based management in healthcare? Manag. Decis. 2018, 56, 2069–2084. [Google Scholar] [CrossRef]
- Aloini, D.; Cannavacciuolo, L.; Gitto, S.; Lettieri, E.; Malighetti, P.; Visintin, F. Evidence-Based Management for Performance Improvement in HealthCare. Manag. Decis. 2018, 56, 2063–2068. [Google Scholar] [CrossRef]
| Informants | N | ID | Phases | Total Meetings | ||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 4 | 5 | |||||
| Interview (I) | Focus Group (FG) | Brainstorming (BRAIN) | Co-Design (DES) | Test (TEST) | ||||
| Neurologists | 8 | NEURO_1 | INT1 | FG1 | DES4 | |||
| NEURO_2 | INT2 | FG1 | ||||||
| NEURO_3 | INT3 | FG1 | BRAIN4 | TEST3 | ||||
| NEURO_4 | FG2 | |||||||
| NEURO_5 | FG2 | |||||||
| NEURO_6 | FG2 | |||||||
| NEURO_7 | DES1 | |||||||
| NEURO_8 | BRAIN4 | |||||||
| PD patients | 4 | PAT_1 | INT4 | |||||
| PAT_2 | DES2 | |||||||
| PAT_3 | DES3 | |||||||
| PAT_4 | TEST1 | |||||||
| Informal caregivers | 3 | ICG_1 | INT4 | |||||
| ICG_2 | DES2 | |||||||
| ICG_3 | DES3 | |||||||
| Neurology department directors | 1 | NEUDIR_1 | DES6 | |||||
| Geriatricians | 1 | GER_1 | BRAIN3 | |||||
| Nuclear medicine specialists | 1 | NUCL_1 | BRAIN3 | |||||
| Neurosurgeons | 1 | NEUROSUR_1 | BRAIN3 | |||||
| General Practitioners | 10 | GP_1 | INT5 | |||||
| GP_2 | INT6 | |||||||
| GP_3 | BRAIN1 | |||||||
| GP_4 | BRAIN1 | |||||||
| GP_5 | TEST2 | |||||||
| GP_6 | TEST2 | |||||||
| GP_7 | TEST2 | |||||||
| GP_8 | TEST2 | |||||||
| GP_9 | TEST2 | |||||||
| GP_10 | TEST2 | |||||||
| Psychologists | 3 | PSY_1 | BRAIN4 | |||||
| PSY_2 | BRAIN4 | |||||||
| PSY_3 | BRAIN4 | |||||||
| Nurses | 2 | NU_1 | DES6 | |||||
| NU_2 | DES6 | |||||||
| Medical directors | 1 | MD_1 | DES5 | |||||
| Physiotherapists | 1 | PHYSIO_1 | BRAIN4 | |||||
| Territorial clinics managers | 1 | TCM_1 | BRAIN4 | TEST2 | ||||
| Heads of the nursing staff | 1 | NURSEHEAD | BRAIN2 | |||||
| Physiatrists | 2 | PHYSI_1 | BRAIN4 | |||||
| PHYSI_2 | BRAIN4 | |||||||
| Nurses with managerial duties | 2 | NURSEMNG_1 | BRAIN2 | DES6 | ||||
| NURSEMNG_2 | BRAIN2 | |||||||
| Total informants | 42 | |||||||
| Meetings per phase | 6 | 2 | 4 | 6 | 3 | 21 | ||
| Problem from Stakeholders’ Perspective (with Evidence from the Field) | Key Feature | Potential Benefit |
|---|---|---|
| [P1] Late diagnosis “It was my son who had the concern because the same had happened to one of his friends”—ICG_1. “I couldn’t move my left foot properly. I thought it was caused by playing soccer. I went to the neurologist because my sister was diagnosed with PD 10 years ago”—PAT_1. “Initially, patients tend to hide problems, and the family calls me”—GP_2. | [KF3] Fine-grained detection | [B1] Early detection |
| [P2] Subjective Assessment “We use qualitative scales (mild, severe, or continuous) to measure tremor, which introduces significant inter- and intra-observer bias”—GP_2. | [KF2] Objective detection | [B2] Objective assessment |
| [P3] Inaccurate Assessment “The guidelines ask us to make judgments with the naked eye, which are, however, very inaccurate”—NEURO_2. | [KF1] Accurate detection | [B3] Accurate assessment |
| [P4] Infrequent Assessment “Patients are at risk of waiting three months or more to hear that therapy is not working”—NEURO_2. “The frequency with which patients are visited quite often does not depend on actual clinical needs but on the resources available”—NEURO_3. | [KF4] Easy to use | [B4] Delegate |
| [KF5] Easy to transport | [B5] Change setting | |
| [P5] Improper Timing “Motor symptoms usually worsen in the evening or early morning, but that’s not when we can visit the patient”—NEURO_3. | [KF4] Easy to use | [B4] Delegate |
| [KF5] Easy to transport | [B5] Change setting |
| Stakeholders | Needs [N] | Potential Benefits | ||||
|---|---|---|---|---|---|---|
| [B1] Early Detection | [B2] Objective Assessment | [B3] Accurate Assessment | [B4] Delegate | [B5] Change Setting | ||
| Persona 1—Giorgio (Main features: prodromal stage, no check-ups) | [N1] Be proactively involved in an early diagnosis process | X | ||||
| Persona 2—Elisabetta (Main features: initial motor symptoms, frequent check-ups) | [N2] Be subjected to the proper check-ups by the right physicians | X | ||||
| Persona 3—Simona (Main features: already diagnosed with PD, autonomous, with informal caregivers, capable of using technologies) | [N3] Continue doing the activities she loves | X | X | X | X | |
| [N4] Manage PD without reducing the quality of life of her family | X | |||||
| Persona 4—Paolo (Main features: already diagnosed with PD, low autonomy, with a formal caregiver, not capable of using technologies) | [N5] Strengthen the collaboration between doctors and caregivers | X | ||||
| [N6] Receive therapies calibrated on the actual status of the disease | X | X | X | X | ||
| GPs | [N7] Activate a proactive diagnosis process | X | ||||
| [N8] Effectively coordinate patient care | X | X | X | X | ||
| Neurologists | [N9] Obtain an early diagnosis | X | ||||
| [N10] Avoid errors in the diagnosis and treatment process | X | X | X | X | ||
| [N11] Facilitate patient’s handover to/from another neurologist | X | X | ||||
| Problem | Potential Benefit | Why |
|---|---|---|
| [P1] Late diagnosis | [B1] Early detection | [WHY1] Prodromal diagnosis |
| [WHY2] Early diagnosis | ||
| [P2] Subjective assessment | [B2] Objective assessment | [WHY3] Periodic assessment |
| [P3] Inaccurate assessment | [B3] Accurate assessment | [WHY3] Periodic assessment |
| [P4] Infrequent assessment | [B4] Delegate | [WHY4] Monitoring |
| [B5] Change setting | [WHY4] Monitoring | |
| [P5] Unproper timing | [B4] Delegate | [WHY4] Monitoring |
| [B5] Change setting | [WHY4] Monitoring |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vannelli, S.; Visintin, F.; Dosi, C.; Fiorini, L.; Rovini, E.; Cavallo, F. A Framework for the Human-Centered Design of Service Processes Enabled by Medical Devices: A Case Study of Wearable Devices for Parkinson’s Disease. Int. J. Environ. Res. Public Health 2024, 21, 1367. https://doi.org/10.3390/ijerph21101367
Vannelli S, Visintin F, Dosi C, Fiorini L, Rovini E, Cavallo F. A Framework for the Human-Centered Design of Service Processes Enabled by Medical Devices: A Case Study of Wearable Devices for Parkinson’s Disease. International Journal of Environmental Research and Public Health. 2024; 21(10):1367. https://doi.org/10.3390/ijerph21101367
Chicago/Turabian StyleVannelli, Sara, Filippo Visintin, Clio Dosi, Laura Fiorini, Erika Rovini, and Filippo Cavallo. 2024. "A Framework for the Human-Centered Design of Service Processes Enabled by Medical Devices: A Case Study of Wearable Devices for Parkinson’s Disease" International Journal of Environmental Research and Public Health 21, no. 10: 1367. https://doi.org/10.3390/ijerph21101367
APA StyleVannelli, S., Visintin, F., Dosi, C., Fiorini, L., Rovini, E., & Cavallo, F. (2024). A Framework for the Human-Centered Design of Service Processes Enabled by Medical Devices: A Case Study of Wearable Devices for Parkinson’s Disease. International Journal of Environmental Research and Public Health, 21(10), 1367. https://doi.org/10.3390/ijerph21101367









