Impact of Weight Status on Hemodynamic Parameters and Aerobic Fitness in School-Aged Children: A Study in a Rural School Community
Abstract
1. Introduction
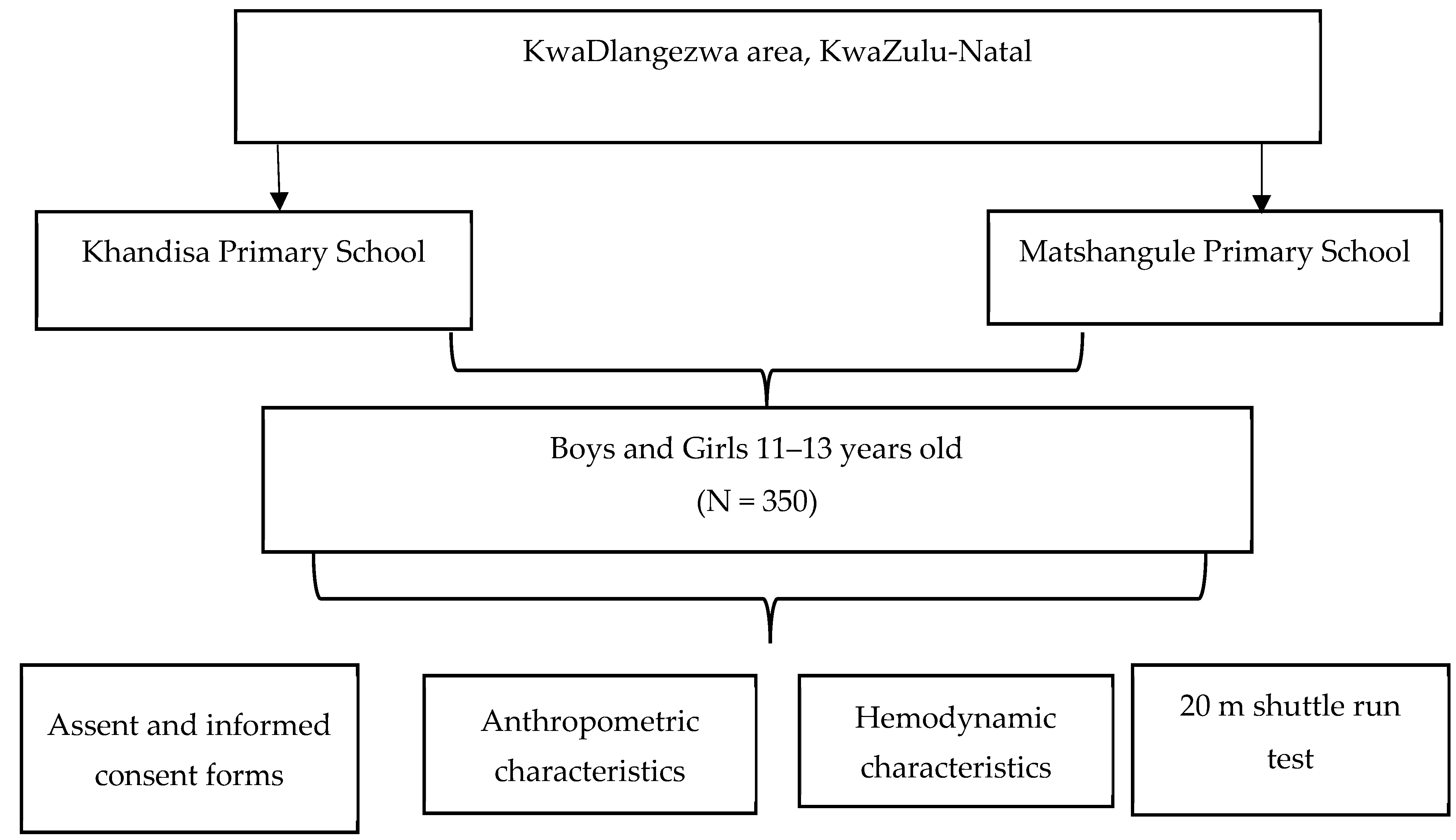
2. Materials and Methods
2.1. Participants and Procedures
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Data Collection Process
Anthropometric Measurements
- Height and Weight
- b.
- Waist to Hip (WHR)
- c.
- Skinfolds
- d.
- Hemodynamic Measurements
- e.
- Aerobic Fitness Test (20 m Shuttle Run Test)
- f.
- Data Analysis
3. Results
3.1. Anthropometric Characteristics
3.2. Hemodynamic Characteristics
3.3. Aerobic Characteristics
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Carnethon, M.R.; Gulati, M.; Greenland, P. Prevalence and cardiovascular disease correlates of low cardiorespiratory fitness in adolescents and adults. JAMA 2005, 294, 2981–2988. [Google Scholar] [CrossRef] [PubMed]
- Dobosz, J.; Mayorga-Vega, D.; Viciana, J. Percentile values of physical fitness levels among polish children aged 7 to 19 years—A population-based study. Cent. Eur. J. Public. Health 2015, 23, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Amusa, L.O.; Goon, D.T.; Amey, A.K.; Toriola, A.L. Health-related physical fitness among rural primary school children in Tshannda, South Africa. Sci. Res. Essays 2011, 6, 4665–4680. [Google Scholar] [CrossRef]
- World Health Organization. Adolescent Obesity and Related Behaviours: Trends and Inequalities in the WHO European Region, 2002–2014: Observations from the Health Behavior in School-Aged Children (HBSC) WHO Collaborative Cross-National Study; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Ruiz, J.R.; Castro-Piñero, J.; Artero, E.G.; Ortega, F.B.; Sjöström, M.; Suni, J.; Castillo, M.J. Predictive validity of health-related fitness in youth: A systematic review. Br. J. Sports Med. 2009, 43, 909–923. [Google Scholar] [CrossRef]
- Ogden, C.L.; Freedman, D.S.; Hales, C.M. CDC extended BMI-for-age percentiles versus percent of the 95th percentile. Pediatr. 2023, 1152, e2023062285. [Google Scholar] [CrossRef]
- Pepera, G.; Hadjiandrea, S.; Iliadis, I.; Sandercock, G.R.; Batalik, L. Associations between cardiorespiratory fitness, fatness, hemodynamic characteristics, and sedentary behaviour in primary school-aged children. BMC Sports Sci. Med. Rehabil. 2022, 14, 16. [Google Scholar] [CrossRef]
- Prathap, S.; Nagel, B.J.; Herting, M.M. Understanding the role of aerobic fitness, spatial learning, and hippocampal subfields in adolescent males. Sci. Rep. 2021, 11, 9311. [Google Scholar] [CrossRef] [PubMed]
- Corbin, C.B.; Pangrazi, R.P.; Franks, B.D. Definitions: Health, fitness, and physical activity. Pres. Coun Phys. Fit. Sports Res. Dig. 2000, 3, 1–11. [Google Scholar]
- Men, J.; Zou, S.; Ma, J.; Xiang, C.; Li, S.; Wang, J. Effects of high-intensity interval training on physical morphology, cardiorespiratory fitness and metabolic risk factors of cardiovascular disease in children and adolescents: A systematic review and meta-analysis. PLoS ONE 2023, 18, e0271845. [Google Scholar] [CrossRef]
- Pojskic, H.; Eslami, B. Relationship between obesity, physical activity, and cardiorespiratory fitness levels in children and adolescents in Bosnia and Herzegovina: An analysis of gender differences. Front. Physiol. 2018, 9, 418967. [Google Scholar] [CrossRef]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Franks, P.W.; Hanson, R.L.; Knowler, W.C.; Sievers, M.L.; Bennett, P.H.; Looker, H.C. Childhood obesity, other cardiovascular risk factors, and premature death. N. Engl. J. Med. 2010, 362, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, C.C.; Li, J.; Cooper, M.N.; Hopkins, K.D.; Farrant, B.M. The impact of racial discrimination on the health of Australian Indigenous children aged 5–10 years: Analysis of national longitudinal data. Int. J. Equity Health 2017, 16, 116. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Ahn, J.; Kim, H.K.; and Kim, J.H. Obese children experience more extremity fractures than nonobese children and are significantly more likely to die from traumatic injuries. Acta Paediatr. 2016, 105, 1152–1157. [Google Scholar] [CrossRef]
- Tuan, S.; Su, H.; Chen, Y.; Li, M.; Tsai, Y.; Yang, C.; Lin, K. Fat mass index and body mass index affect peak metabolic equivalent negatively during exercise test among children and adolescents in Taiwan. Int. J. Env. Res. Public. Health 2018, 15, 263. [Google Scholar] [CrossRef] [PubMed]
- Pahkala, K.; Hernelahti, M.; Heinonen, O.J.; Raittinen, P.; Hakanen, M.; Lagström, H.; Viikari, J.S.; Rönnemaa, T.; Raitakari, O.T.; Simell, O. Body mass index, fitness and physical activity from childhood through adolescence. Br. J. Sports Med. 2013, 47, 71–77. [Google Scholar] [CrossRef]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012, 307, 483–490. [Google Scholar] [CrossRef]
- Bacopoulou, F.; Efthymiou, V.; Landis, G.; Rentoumis, A.; Chrousos, G.P. Waist circumference, waist-to-hip ratio and waist-to-height ratio reference percentiles for abdominal obesity among Greek adolescents. BMC Pediatr. 2015, 15, 50. [Google Scholar] [CrossRef]
- Scicali, R.; Rosenbaum, D.; Di Pino, A.; Giral, P.; Cluzel, P.; Redheuil, A.; Piro, S.; Rabuazzo, A.M.; Purrello, F.; Bruckert, E.; et al. An increased waist-to-hip ratio is a key determinant of atherosclerotic burden in overweight subjects. Acta Diabetol. 2018, 55, 741–749. [Google Scholar] [CrossRef]
- Radetti, G.; Grugni, G.; Lupi, F.; Fanolla, A.; Caroli, D.; Bondesan, A.; Sartorio, A. High Tg/HDL-cholesterol ratio highlights a higher risk of metabolic syndrome in children and adolescents with severe obesity. J. Clin. Med. 2022, 11, 4488. [Google Scholar] [CrossRef]
- Jakobsson, J.; Malm, C.; Furberg, M.; Ekelund, U.; Svensson, M. Physical activity during the coronavirus (COVID-19) pandemic: Prevention of a decline in metabolic and immunological functions. Front. Sports Act. Living 2020, 2, 57. [Google Scholar] [CrossRef]
- Posadzki, P.; Pieper, D.; Bajpai, R.; Makaruk, H.; Könsgen, N.; Neuhaus, A.L.; Semwal, M. Exercise/physical activity and health outcomes: An overview of Cochrane systematic reviews. BMC Public. Health 2020, 20, 1724. [Google Scholar] [CrossRef]
- Ostojic, S.M.; Stojanovic, M.D.; Stojanovic, V.; Maric, J.; Njaradi, N. Correlation between fitness and fatness in 6–14-year old Serbian school children. J. Health Popul. Nutr. 2011, 29, 53–60. [Google Scholar] [CrossRef]
- Clemente, F.M.; Ardigò, L.P.; Song, W.; Lenoir, M.E.M.; Rodrigues, L.P.; Sigmundsson, H. Editorial: Children's Exercise Physiology. Front. Physiol. 2020, 11, 269. [Google Scholar] [CrossRef]
- Freeney Wright, T.; Rivero, C.M.; Barlow, S.E. Updates in the treatment of pediatric obesity. Curr. Treat. 2023, 9, 93–105. [Google Scholar] [CrossRef]
- Breukelman, G.J.; Millard, L.; De Klerk, G. The effects of BMI on health-related physical fitness components in secondary school children (15–17 years). HealthMED 2018, 19, 43. [Google Scholar]
- Kansra, A.R.; Lakkunarajah, S.; Jay, M.S. Childhood and adolescent obesity: A review. Front. Pediatr. 2021, 8, 581461. [Google Scholar] [CrossRef]
- Skelton, J.A.; Beech, B.M. Attrition in paediatric weight management: A review of the literature and new directions. Obes. Rev. 2011, 12, e273–e281. [Google Scholar] [CrossRef]
- Marfell-Jones, M.J.; Stewart, A.D.; De Ridder, J.H. International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry: Potchefstroom, South Africa, 2011. [Google Scholar]
- Fryar, C.D.; Carroll, M.D.; Gu, Q.; Afful, J.; and Ogden, C.L. Anthropometric reference data for children and adults: United States, 2015–2018. National Center for Health Statistics. Vital Health Stat. 2021, 3, 1–44. [Google Scholar]
- Silva, V.S.; Vieira, M.F. International Society for the Advancement of Kinanthropometry (ISAK) Global: International accreditation scheme of the competent anthropometrist. Rev. Bras. Cineantropom Desempenho Hum. 2020, 22, e70517. [Google Scholar] [CrossRef]
- Bojanic, D.; Ljubojevic, M.; Krivokapic, D.; Gontarev, S. Waist circumference, waist-to-hip ratio, and waist-to-height ratio reference percentiles for abdominal obesity among Macedonian adolescents. Nutr. Hosp. 2020, 37, 786–793. [Google Scholar] [CrossRef] [PubMed]
- Slaughter, M.H.; Lohman, T.G.; Boileau, R.A.; Horwill, C.A.; Stillman, R.J.; Van Loan, M.D.; Bemben, D.A. Skinfold equation for estimation of body fatness in children and youth. Hum. Biol. 1988, 60, 709–723. [Google Scholar] [PubMed]
- Ekelund, U.; Poortvliet, E.; Nilsson, A.; Yngve, A.; Holmberg, A.; Sjöström, M. Physical activity in relation to aerobic fitness and body fat in 14-to 15-year-old boys and girls. Eur. J. Appl. Physiol. 2001, 85, 195–201. [Google Scholar] [CrossRef]
- Bing, S.; Chen, K.; Hou, H.; Zhang, W.; LiLWei, J.; Shu, C.; Wan, Y. Validation of the Microlife BP A200 Comfort and W2 Slim automated blood pressure monitors in a general adult population according to the European Society of Hypertension and the ANSI/AAMI/ISO 81060-2:2013 protocols. Blood Press Monit. 2016, 21, 118–123. [Google Scholar] [CrossRef]
- Cohen, D.D.; Lopez-Jaramillo, P.; Fernández-Santos, J.D.; Castro-Piñero, J.; Sandercock, G.R. Muscle strength is associated with lower diastolic blood pressure in schoolchildren. Prev. Med. 2017, 95, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Silva, D.A.; Lima, T.R.; Tremblay, M.S. Association between resting heart rate and health-related physical fitness in Brazilian adolescents. Biomed. Res. Int. 2018, 2018, 3812197. [Google Scholar] [CrossRef]
- Flynn, J.T.; Kaelber, D.C.; Baker-Smith, C.M.; Blowey, D.; Carroll, A.E.; Daniels, S.R.; De Ferranti, S.D.; Dionne, J.M.; Falkner, B.; Flinn, S.K.; et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatr. 2017, 140, e20171904. [Google Scholar] [CrossRef]
- Fleming, S.; Thompson, M.; Stevens, R.; Heneghan, C.; Plüddemann, A.; Maconochie, I.; Tarassenko, L.; Mant, D. Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: A systematic review of observational studies. Lancet 2011, 377, 1011–1018. [Google Scholar] [CrossRef]
- Tomkinson, G.R.; Lang, J.J.; Blanchard, J.; Léger, L.A.; Tremblay, M.S. The 20-m shuttle run: Assessment and interpretation of data in relation to youth aerobic fitness and health. Pediatr. Exerc. Sci. 2019, 31, 152–163. [Google Scholar] [CrossRef]
- Léger, L.; Lambert, J.; Goulet, A.; Rowan, C.; Dinelle, Y. Aerobic capacity of 6 to 17-year-old Quebecois—20 meter shuttle run. Can. J. Appl. Sport. Sci. 1984, 9, 64–69. [Google Scholar]
- Kolimechkov, S.; Petrov, L.; Alexandrova, A.; Cholakov, K. BeepShuttle junior: Software for the administration of the 20m shuttle run test in children and adolescents. J. Adv. Sport. Technol. 2018, 2, 35–40. [Google Scholar]
- Paradisis, G.P.; Zacharogiannis, E.; Mandila, D.; Smirtiotou, A.; Argeitaki, P.; Cooke, C.B. Multi-stage 20-m shuttle run fitness test, maximal oxygen uptake and velocity at maximal oxygen uptake. J. Hum. Kinet. 2014, 41, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.E.; Eleshery, U.M.; Rashwan, N.I.; Abed, E.E. Waist Circumference as an Indicator for Metabolic Syndrome in Children: A Narrative Review. SVU-Int. J. Med. Sci. 2024, 7, 798–808. [Google Scholar] [CrossRef]
- McConnell-Nzunga, J. An Investigation of Body Fat Accrual in an Ethnically Diverse Cohort of British Columbian Children and Youth: Patterns, Obesity Classification, and Determinants. Ph.D. Dissertation, University of Victoria, Victoria, BC, Canada, 2017. [Google Scholar]
- Ruiz, J.R.; Cavero-Redondo, I.; Ortega, F.B.; Welk, G.J.; Andersen, L.B.; Martinez-Vizcaino, V. Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br. J. Sports Med. 2016, 50, 1451–1458. [Google Scholar] [CrossRef] [PubMed]
- He, Q.Q.; Wong, T.W.; Du, L.; Jiang, Z.Q.; Qiu, H.; Gao, Y.; Liu, J.W.; Wu, J.G.; Yu, I.T. Respiratory health in overweight and obese Chinese children. Pediatr. Pulmonol. 2009, 44, 997–1002. [Google Scholar] [CrossRef]
- López-Gil, J.F.; Brazo-Sayavera, J.; Lucas, J.L.Y.; Cavichiolli, F.R. Weight status is related to health-related physical fitness and physical activity but not to sedentary behaviour in children. Int. J. Environ. Res. Public. Health 2020, 17, 4518. [Google Scholar] [CrossRef]
- Brand, C.; Reuter, C.P.; Gaya, A.R.; Mota, J.; Duncan, M.; Borfe, L.; Pollo Renner, J.D. Association between cardiorespiratory fitness and cardiometabolic risk factors in Brazilian children and adolescents: The mediating role of obesity parameters. Paediatr. Int. Child. Health 2021, 41, 93–102. [Google Scholar] [CrossRef]
- Zadarko-Domaradzka, M.; Sobolewski, M.; Zadarko, E. Comparison of Several Anthropometric Indices Related to Body Fat in Predicting Cardiorespiratory Fitness in School-Aged Children-A Single-Center Cross-Sectional Study. J. Clin. Med. 2023, 12, 6226. [Google Scholar] [CrossRef]
- Burgos, M.S.; Reuter, C.P.; Burgos, L.T.; Pohl, H.H.; Pauli, L.T.; Horta, J.A.; Reckziegel, M.B.; Franke, S.I.; Prá, D.; Camargo, M. Comparison analysis of blood pressure, obesity, and cardio-respiratory fitness in schoolchildren. Arq. Bras. Cardio 2010, 94, 788–793. [Google Scholar] [CrossRef][Green Version]
- Sarni, R.S.; Souza, F.I.; Schoeps, D.D.; Catherino, P.; Oliveira, M.C.; Pessotti, C.F.; Kochi, C.; Colugnati, F.A. Relationship between waist circumference and nutritional status, lipid profile and blood pressure in low socioeconomic level pre-school children. Arq. Bras. Cardio 2006, 87, 153–158. [Google Scholar] [CrossRef][Green Version]
- Cauduro, A.; Bergmann, M.; Bergmann, G. Atividade física, sobrepeso e pressão arterial: Associação independente e combinada em adolescentes. Rev. Bras. Ativ. Fís 2015, 20, 483. [Google Scholar] [CrossRef]
- Itagi, A.; Nagaraja, S.; Bondade, S.; Yunus, G.Y. Relationship of resting heart rate with body composition and obesity among young adults in india-a cross sectional study. Nalt. J. Physiol. Pharm. Pharmacol. 2014, 4, 143–148. [Google Scholar] [CrossRef]
- Mazaro, I.A.; de Lurdes Zanolli, M.; Antonio, M.Â.; Morcillo, A.M.; Zambon, M.P. Obesity and cardiovascular risk factors in school children from Sorocaba, SP. Rev. Assoc. Méd. Bras. (Engl. Ed.) 2011, 57, 674–680. [Google Scholar] [CrossRef]
- Melzer, M.R.; Magrini, I.M.; Domene, S.M.; Martins, P.A. Factors associated with abdominal obesity in children. Rev. Paul. Pediatr. 2015, 33, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Riebe, D.; Franklin, B.A.; Thompson, P.D.; Garber, C.E.; Whitfield, G.P.; Magal, M.; Pescatello, L.S. Updating ACSM’s Recommendations for Exercise Preparticipation Health Screening. Med. Sci. Sports Exerc. 2015, 47, 2473–2479. [Google Scholar] [CrossRef]
- Almeida, S.M.; Furtado, J.M.; Mascarenhas, P.; Ferraz, M.E.; Silva, L.R.; Ferreira, J.C.; Monteiro, M.; Vilanova, M.; Ferraz, F.P. Anthropometric predictors of body fat in a large population of 9-year-old school-aged children. Obes. Sci. Pr. 2016, 2, 272–281. [Google Scholar] [CrossRef]
| Variable | Healthy Weight (n = 201) | Overweight (n = 149) | Difference (%) | Significance (p-Value) |
|---|---|---|---|---|
| Age | 11.99 ± 0.77 | 12.04 ± 0.76 | 0.4 | 0.546 |
| Height (m) | 148.36 ± 8.28 | 149.29 ± 8.08 | 0.6 | 0.293 |
| Weight (kg) | 41.02 ± 7.71 | 49.92 ± 12.87 | 18 | <0.001 * |
| Waist circumference (cm) | 62.59 ± 5.17 | 70.85 ± 10.05 | 12 | <0.001 * |
| Hip circumference (cm) | 82.08 ± 7.08 | 87.42 ± 10.82 | 6 | <0.001 * |
| Waist–hip ratio | 0.76 ± 0.04 | 0.81 ± 0.06 | 6 | <0.001 * |
| Body fat | 20.72 ± 4.46 | 24.99 ± 5.16 | 16 | <0.001 * |
| Variable | Healthy Weight (n = 201) | Overweight (n = 149) | Difference (%) | Significance (p-Value) |
|---|---|---|---|---|
| Resting heart rate (bpm) | 83.92 ± 13.45 | 86.92 ± 11.73 | 3 | 0.055 |
| Systolic blood pressure (mmHg) | 113.85 ± 11.11 | 115.81 ± 12.14 | 2 | 0.116 |
| Diastolic blood pressure (mmHg) | 71.32 ± 13.57 | 73.79 ± 12.96 | 3 | 0.08 |
| Variable | Healthy Weight (n = 201) | Overweight (n = 149) | Difference (%) | Significance (p-Value) |
|---|---|---|---|---|
| Beep speed (km/h) | 9.07 ± 0.50 | 8.67 ± 0.55 | 4 | <0.001 * |
| Beep level | 3.81 ± 1.04 | 3.05 ± 1.15 | 20 | <0.001 * |
| VO2max | 38.26 ± 3.09 | 36.07 ± 313 | 6 | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lukhele, N.P.; Millard, L.; Breukelman, G.J. Impact of Weight Status on Hemodynamic Parameters and Aerobic Fitness in School-Aged Children: A Study in a Rural School Community. Int. J. Environ. Res. Public Health 2024, 21, 1340. https://doi.org/10.3390/ijerph21101340
Lukhele NP, Millard L, Breukelman GJ. Impact of Weight Status on Hemodynamic Parameters and Aerobic Fitness in School-Aged Children: A Study in a Rural School Community. International Journal of Environmental Research and Public Health. 2024; 21(10):1340. https://doi.org/10.3390/ijerph21101340
Chicago/Turabian StyleLukhele, Ncomi Primrose, Lourens Millard, and Gerrit Jan Breukelman. 2024. "Impact of Weight Status on Hemodynamic Parameters and Aerobic Fitness in School-Aged Children: A Study in a Rural School Community" International Journal of Environmental Research and Public Health 21, no. 10: 1340. https://doi.org/10.3390/ijerph21101340
APA StyleLukhele, N. P., Millard, L., & Breukelman, G. J. (2024). Impact of Weight Status on Hemodynamic Parameters and Aerobic Fitness in School-Aged Children: A Study in a Rural School Community. International Journal of Environmental Research and Public Health, 21(10), 1340. https://doi.org/10.3390/ijerph21101340






