Assessing the Impact of Workforce Nutrition Programmes on Nutrition, Health and Business Outcomes: A Review of the Global Evidence and Future Research Agenda
Abstract
1. Introduction
- Access to healthy food interventions, which consist of the employer increasing access to nutritious foods for free or at subsidised costs, and/or making changes to the workplace food environment (e.g., healthier canteen menus, healthier snacks and beverages in vending machines, more balanced portion sizes and meal composition).
- Nutrition education programmes that aim to change employees’ dietary and/or lifestyle behaviours by increasing their nutritional knowledge and health literacy. Examples of interventions are cooperative menu planning, cooking demonstrations, dissemination of educational materials, interactive information sessions/workshops, and interpersonal communication.
- Nutrition-focused health checks (and counselling), which are periodic one-to-one consultations with a health or nutrition professional to assess and discuss the employee’s nutritional and health status. Health checks help employees gain a better understanding of their nutritional and health risk factors, for example, through cholesterol and blood-pressure screenings, or weight monitoring and classification (Body Mass Index, BMI). Follow-up counselling can be provided in addition to health checks, to advise employees on potential dietary and lifestyle changes.
- Breastfeeding support interventions, which include programmes and/or policies aiming to enable working mothers to breastfeed their child exclusively for 6 months (i.e., providing only breastmilk to a child as per World Health Organization (WHO) recommendations) and continually up to 2 years [7]. Examples of policies and interventions are respecting or exceeding national laws on the duration of paid maternity leave, providing breastfeeding rooms and onsite childcare (where relevant), breastfeeding or breastmilk expression breaks, and flexible work schedules for mothers. In addition, breastfeeding support programmes can include awareness-raising or nutrition education campaigns for mothers and co-workers on the importance and benefits of breastfeeding.
2. Methods
- Having a clear focus on workforce nutrition, either as a stand-alone subject or as a principal component of broader workforce health and wellness (for example, records focusing solely on workplace physical activity interventions were excluded, while articles focusing both on worksite nutrition and physical activity programmes were included).
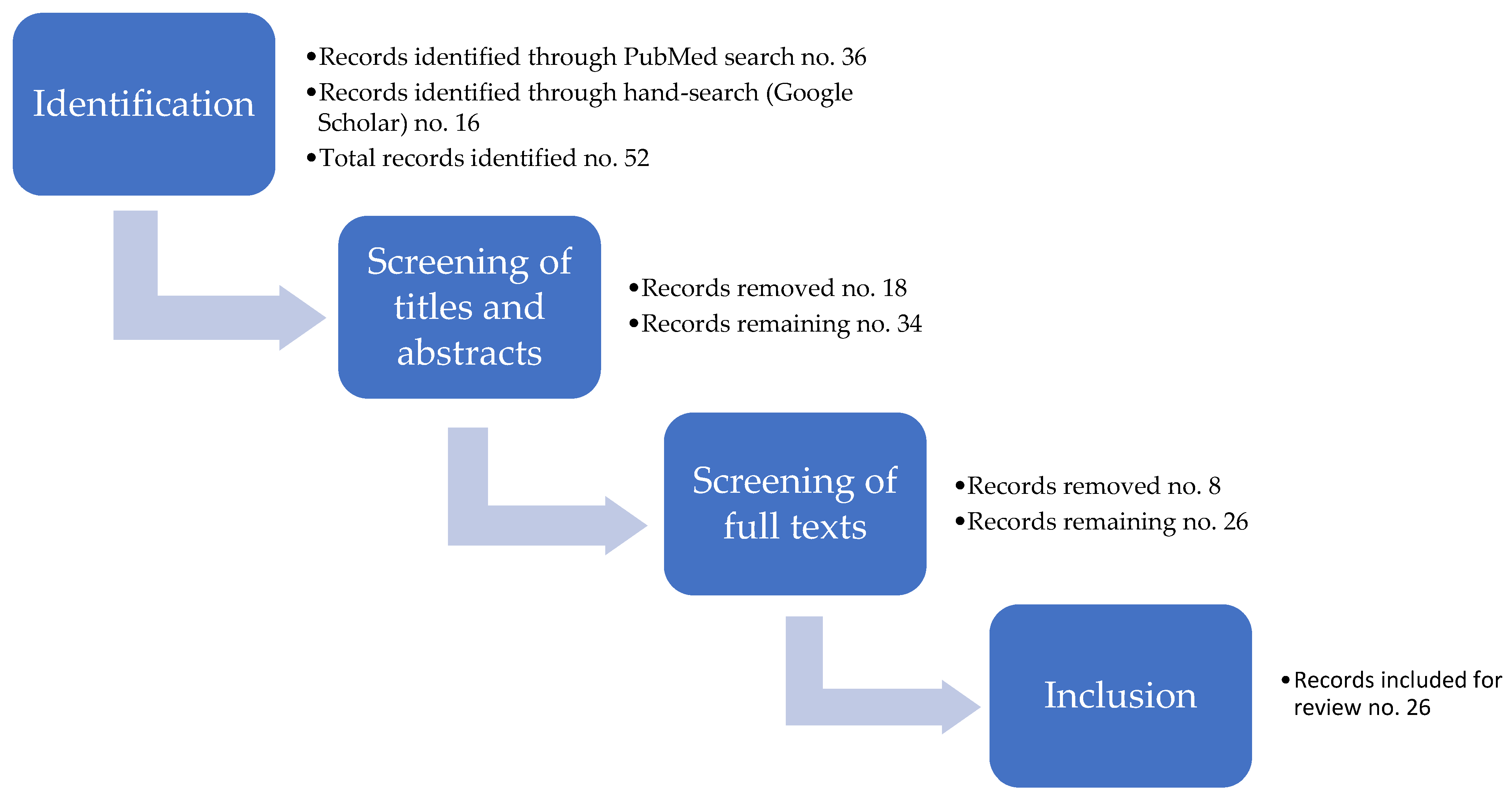
- Peer-reviewed articles with high strength of evidence (i.e., systematic reviews, meta-analyses and RCTs) (Figure 1). The main rationale for this choice is that the body of literature on workforce nutrition is increasing rapidly. However, only a small subset of it presents high strength of evidence.
- Touching on one or more of the four pillars of workforce nutrition policies and programmes described in the Introduction.
- Discussing the effects of workforce nutrition policies and programmes on nutrition, health and/or business (financial) outcomes.
3. Results
3.1. Descriptive (Numerical) Analysis of Included Records
3.2. Content (Thematic) Analysis of Included Records
3.2.1. Records Focusing on Access to Healthy Food as a Stand-Alone Intervention (One Pillar)
3.2.2. Records Focusing on Nutrition Education as a Stand-Alone Intervention (One Pillar)
3.2.3. Records Focusing on Health Checks and Counselling as a Stand-Alone Intervention (One Pillar)
3.2.4. Records Focusing on Breastfeeding Support as Stand-Alone Interventions (One Pillar)
3.2.5. Records including Health Checks and Counselling Combined with Nutrition Education Interventions (Two Pillars)
3.2.6. Records including Access to Healthy Food Combined with Nutrition Education Interventions (Two Pillars)
3.2.7. Records including Access to Healthy Food, Health Checks and Counselling, and Nutrition Education Interventions Combined (Three Pillars)
4. Discussion
4.1. Identified Literature Gaps and Recommendations for Programmes and Research
4.2. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stevens, G.A.; Beal, T.; Mbuya, M.N.N.; Luo, H.; Neufeld, L.M.; Addo, O.Y.; Adu-Afarwuah, S.; Alayón, S.; Bhutta, Z.; Brown, K.H.; et al. Identified literature gaps and recommendations for programmes and research. Lancet Glob. Health 2022, 10, e1590–e1599. [Google Scholar] [CrossRef] [PubMed]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- Wellesley, L.; Eis, J.; Marijs, C.; Vexler, C.; Waites, F.; Benton, T.G. The Business Case for Investment in Nutrition; Chatham House: London, UK, 2020. [Google Scholar]
- Wanjek, C. Food at Work: Workplace Solutions for Malnutrition, Obesity and Chronic Diseases; International Labour Office: Geneva, Switzerland, 2005. [Google Scholar]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2022. Repurposing Food and Agricultural Policies to Make Healthy Diets More Affordable; FAO: Rome, Italy, 2022. [Google Scholar]
- Workforce Nutrition Alliance Our Pillars: Four Themes for Enhancing Workforce Nutrition. Available online: http://www.wnatest.lucidleaps.com/about/ (accessed on 14 December 2022).
- World Health Organization (WHO). Health Topics: Breastfeeding. Available online: https://www.who.int/health-topics/breastfeeding (accessed on 14 December 2022).
- Cochrane. Trusted Evidence. Informed Decisions. Better Health. Available online: https://www.cochrane.org/welcome (accessed on 14 December 2022).
- Feuerstein-Simon, R.; Dupuis, R.; Schumacher, R.; Cannuscio, C.C. A randomized trial to encourage healthy eating through workplace delivery of fresh food. Am. J. Health Promot. 2020, 34, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Sawada, K.; Wada, K.; Shahrook, S.; Ota, E.; Takemi, Y.; Mori, R. Social marketing including financial incentive programs at worksite cafeterias for preventing obesity: A systematic review. Syst. Rev. 2019, 8, 66. [Google Scholar] [CrossRef]
- Hassani, B.; Amani, R.; Haghighizadeh, M.H.; Araban, M. A priority oriented nutrition education program to improve nutritional and cardiometabolic status in the workplace: A randomized field trial. J. Occup. Med. Toxicol. 2020, 15, 2. [Google Scholar] [CrossRef]
- Vasiljevic, M.; Cartwright, E.; Pilling, M.; Lee, M.-M.; Bignardi, G.; Pechey, R.; Hollands, G.J.; Jebb, S.A.; Marteau, T.M. Impact of calorie labelling in worksite cafeterias: A stepped wedge randomised controlled pilot trial. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 41. [Google Scholar] [CrossRef]
- Dinour, L.M.; Szaro, J.M. Employer-based programs to support breastfeeding among working mothers: A systematic review. Breastfeed. Med. 2017, 12, 131–141. [Google Scholar] [CrossRef]
- Tang, X.; Patterson, P.; MacKenzie-Shalders, K.; van Herwerden, L.A.; Bishop, J.; Rathbone, E.; Honeyman, D.; Reidlinger, D.P. Workplace programmes for supporting breast-feeding: A systematic review and meta-analysis. Public Health Nutr. 2021, 24, 1501–1513. [Google Scholar] [CrossRef]
- Taylor, Y.J.; Scott, V.C.; Danielle Connor, C. Perceptions, experiences, and outcomes of lactation support in the workplace: A systematic literature review. J. Hum. Lact. 2020, 36, 657–672. [Google Scholar] [CrossRef]
- Kim, J.H.; Shin, J.C.; Donovan, S.M. Effectiveness of workplace lactation interventions on breastfeeding outcomes in the United States: An updated systematic review. J. Hum. Lact. 2019, 35, 100–113. [Google Scholar] [CrossRef]
- Miller, C.K.; Weinhold, K.R.; Nagaraja, H.N. Impact of a worksite diabetes prevention intervention on diet quality and social cognitive influences of health behavior: A randomized controlled trial. J. Nutr. Educ. Behav. 2016, 48, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.; Baicker, K. Effect of a workplace wellness program on employee health and economic outcomes: A randomized clinical trial. JAMA 2019, 321, 1491–1501. [Google Scholar] [CrossRef] [PubMed]
- Tarro, L.; Llauradó, E.; Ulldemolins, G.; Hermoso, P.; Solà, R. Effectiveness of workplace interventions for improving absenteeism, productivity, and work ability of employees: A systematic review and meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health 2020, 17, 1901. [Google Scholar] [CrossRef] [PubMed]
- Weerasekara, Y.K.; Roberts, S.B.; Kahn, M.A.; LaVertu, A.E.; Hoffman, B.; Das, S.K. Effectiveness of workplace weight management interventions: A systematic review. Curr. Obes. Rep. 2016, 5, 298–306. [Google Scholar] [CrossRef]
- Brown, S.A.; García, A.A.; Zuñiga, J.A.; Lewis, K.A. Effectiveness of workplace diabetes prevention programs: A systematic review of the evidence. Patient Educ. Couns. 2018, 101, 1036–1050. [Google Scholar] [CrossRef]
- Park, S.-H.; Kim, S.-Y. Effectiveness of worksite-based dietary interventions on employees’ obesity: A systematic review and meta-analysis. Nutr. Res. Pract. 2019, 13, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Sandercock, V.; Andrade, J. Evaluation of worksite wellness nutrition and physical activity programs and their subsequent impact on participants’ body composition. J. Obes. 2018, 2018, e1035871. [Google Scholar] [CrossRef]
- Torquati, L.; Pavey, T.; Kolbe-Alexander, T.; Leveritt, M. Promoting diet and physical activity in nurses: A systematic review. Am. J. Health Promot. 2017, 31, 19–27. [Google Scholar] [CrossRef]
- Geaney, F.; Kelly, C.; Greiner, B.A.; Harrington, J.M.; Perry, I.J.; Beirne, P. The effectiveness of workplace dietary modification interventions: A systematic review. Prev. Med. 2013, 57, 438–447. [Google Scholar] [CrossRef]
- Maes, L.; van Cauwenberghe, E.; van Lippevelde, W.; Spittaels, H.; de Pauw, E.; Oppert, J.-M.; van Lenthe, F.J.; Brug, J.; de Bourdeaudhuij, I. Effectiveness of workplace interventions in Europe promoting healthy eating: A systematic review. Eur. J. Public Health 2012, 22, 677–683. [Google Scholar] [CrossRef]
- Robroek, S.J.W.; Oude Hengel, K.M.; van der Beek, A.J.; Boot, C.R.L.; van Lenthe, F.J.; Burdorf, A.; Coenen, P. Socio-economic inequalities in the effectiveness of workplace health promotion programmes on body mass index: An individual participant data meta-analysis. Obes. Rev. 2020, 21, e13101. [Google Scholar] [CrossRef] [PubMed]
- Van Dongen, J.M.; Proper, K.I.; van Wier, M.F.; van der Beek, A.J.; Bongers, P.M.; van Mechelen, W.; van Tulder, M.W. A systematic review of the cost-effectiveness of worksite physical activity and/or nutrition programs. Scand. J. Work Environ. Health 2012, 38, 393–408. [Google Scholar] [CrossRef] [PubMed]
- Grimani, A.; Aboagye, E.; Kwak, L. The effectiveness of workplace nutrition and physical activity interventions in improving productivity, work performance and workability: A systematic review. BMC Public Health 2019, 19, 1676. [Google Scholar] [CrossRef] [PubMed]
- Plotnikoff, R.; Collins, C.E.; Williams, R.; Germov, J.; Callister, R. Effectiveness of interventions targeting health behaviors in university and college staff: A systematic review. Am. J. Health Promot. 2015, 29, e169–e187. [Google Scholar] [CrossRef]
- Lassen, A.D.; Fagt, S.; Lennernäs, M.; Nyberg, M.; Haapalar, I.; Thorsen, A.V.; Møbjerg, A.C.M.; Beck, A.M. The impact of worksite interventions promoting healthier food and/or physical activity habits among employees working “around the clock” hours: A systematic review. Food Nutr. Res. 2018, 62, 1115. [Google Scholar] [CrossRef]
- Van Dongen, J.M.; Proper, K.I.; van Wier, M.F.; van der Beek, A.J.; Bongers, P.M.; van Mechelen, W.; van Tulder, M.W. Systematic review on the financial return of worksite health promotion programmes aimed at improving nutrition and/or increasing physical activity. Obes. Rev. 2011, 12, 1031–1049. [Google Scholar] [CrossRef]
- Wolfenden, L.; Goldman, S.; Stacey, F.G.; Grady, A.; Kingsland, M.; Williams, C.M.; Wiggers, J.; Milat, A.; Rissel, C.; Bauman, A.; et al. Strategies to improve the implementation of workplace-based policies or practices targeting tobacco, alcohol, diet, physical activity and obesity. Cochrane Database Syst. Rev. 2018, 11, CD012439. [Google Scholar] [CrossRef]
- Vargas-Martínez, A.M.; Romero-Saldaña, M.; de Diego-Cordero, R. Economic Evaluation of Workplace Health Promotion Interventions Focused on Lifestyle: Systematic Review and Meta-Analysis. J. Adv. Nurs. 2021, 77, 3657–3691. [Google Scholar] [CrossRef]
- Drewnowski, A. Impact of nutrition interventions and dietary nutrient density on productivity in the workplace. Nutr. Rev. 2019, 78, 215–224. [Google Scholar] [CrossRef]
- Berry, L.L.; Mirabito, A.M.; Baun, W.B. What’s the hard return on employee wellness programs? Harv. Bus. Rev. 2010, 88, 104–112. [Google Scholar]
- Yeung, O.; Johnston, K. The Future of Wellness at Work; The Global Wellness Institute: Miami, FL, USA, 2016. [Google Scholar]
- NCD Alliance. Realising the Potential of Workplaces to Prevent and Control NCDs: How Public Policy Can Encourage Businesses and Governments to Work Together to Address NCDs through the Workplace; NCD Alliance: Geneva, Switzerland, 2016. [Google Scholar]
- UN. Transforming Our World: The 2030 Agenda for Sustainable Development. Available online: https://sdgs.un.org/publications/transforming-our-world-2030-agenda-sustainable-development-17981 (accessed on 31 December 2015).

| Aspect Considered | No. of Identified Records | ||||||
|---|---|---|---|---|---|---|---|
| Type of publication | Systematic review | RCT | |||||
| 21 | 5 | ||||||
| Countries’ income level | HICs | HICs and UMICs | HICs and LMICs | LMICs | |||
| 18 | 5 | 2 | 1 | ||||
| Workforce nutrition pillar(s) | AHF a | NE b | HCC c | BF d | AHF + NE | HCC + NE | AHF + HCC + NE |
| 2 | 2 | 0 | 4 | 2 | 8 | 8 | |
| Outcomes measured | Nutrition and/or health | Breastfeeding | Business | ||||
| 20 | 4 | 12 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nyhus Dhillon, C.; Ortenzi, F. Assessing the Impact of Workforce Nutrition Programmes on Nutrition, Health and Business Outcomes: A Review of the Global Evidence and Future Research Agenda. Int. J. Environ. Res. Public Health 2023, 20, 5733. https://doi.org/10.3390/ijerph20095733
Nyhus Dhillon C, Ortenzi F. Assessing the Impact of Workforce Nutrition Programmes on Nutrition, Health and Business Outcomes: A Review of the Global Evidence and Future Research Agenda. International Journal of Environmental Research and Public Health. 2023; 20(9):5733. https://doi.org/10.3390/ijerph20095733
Chicago/Turabian StyleNyhus Dhillon, Christina, and Flaminia Ortenzi. 2023. "Assessing the Impact of Workforce Nutrition Programmes on Nutrition, Health and Business Outcomes: A Review of the Global Evidence and Future Research Agenda" International Journal of Environmental Research and Public Health 20, no. 9: 5733. https://doi.org/10.3390/ijerph20095733
APA StyleNyhus Dhillon, C., & Ortenzi, F. (2023). Assessing the Impact of Workforce Nutrition Programmes on Nutrition, Health and Business Outcomes: A Review of the Global Evidence and Future Research Agenda. International Journal of Environmental Research and Public Health, 20(9), 5733. https://doi.org/10.3390/ijerph20095733







