The Application of Systems Thinking to the Prevention and Control of Sexually Transmissible Infections among Adolescents and Adults: A Scoping Review
Abstract
1. Introduction
- (1)
- Which specific STIs have been studied from a systems thinking perspective?
- (2)
- In which populations were the studies conducted (i.e., country, age group, gender, sexuality, and ethnic/Indigenous identity)?
- (3)
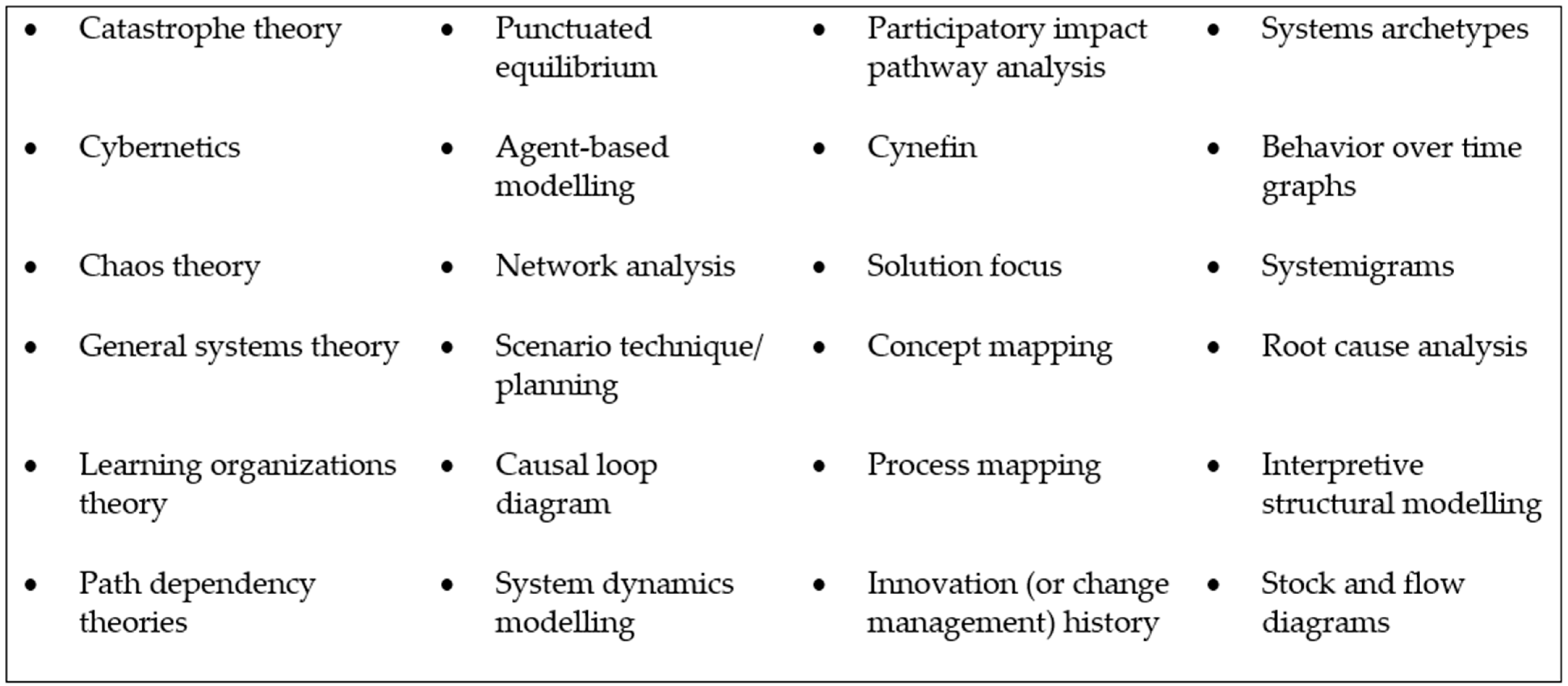
- Which systems thinking concepts and/or tools have been utilized or referenced?
2. Materials and Methods
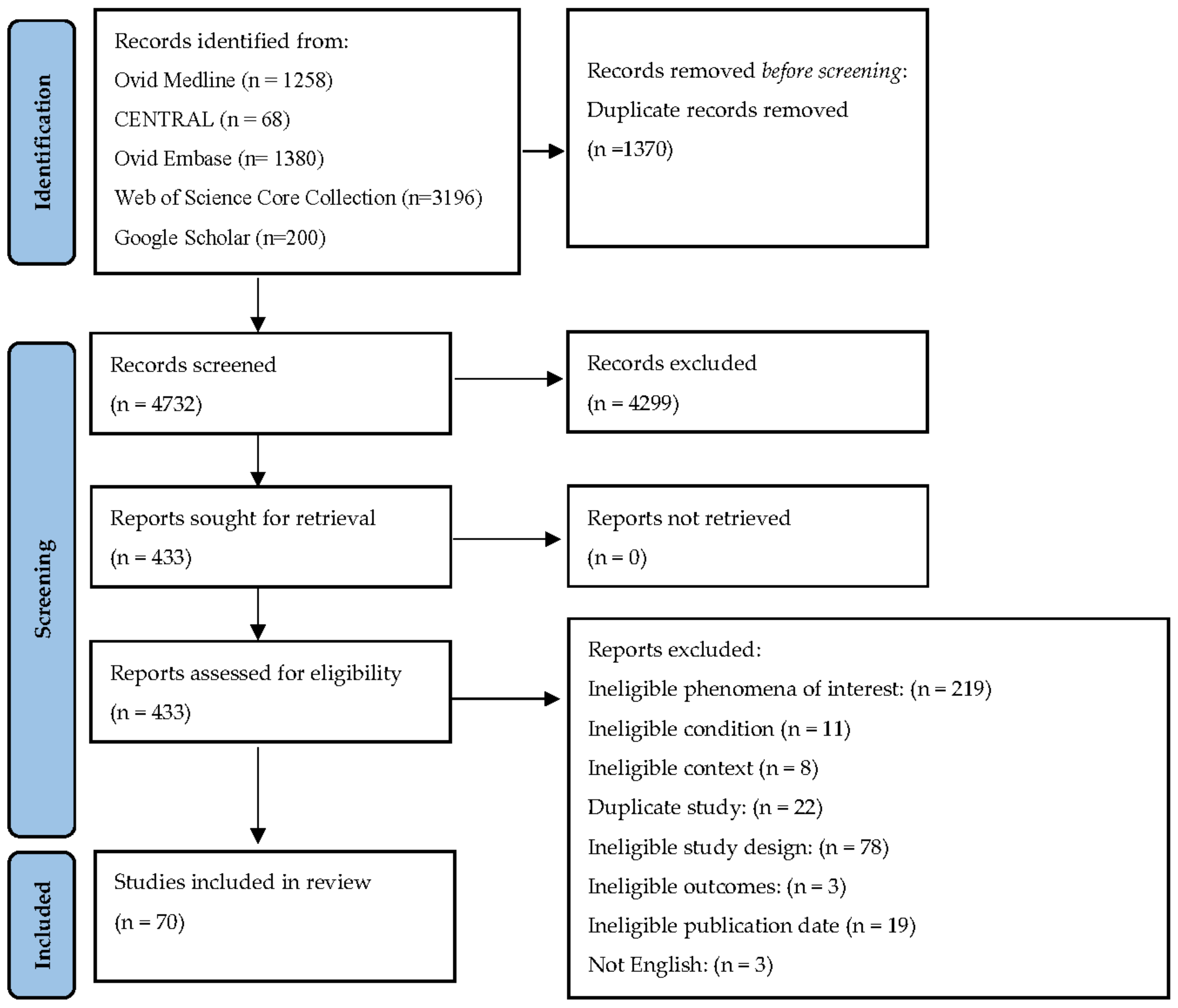
2.1. Search Strategy
2.2. Title and Abstract Screening
2.2.1. Participants
2.2.2. Concept
Systems thinking is a set of synergistic analytic skills used to improve the capability of identifying and understanding systems (i.e., groups or combinations of interrelated, interdependent, or interacting elements forming collective entities), predicting their behaviours, and devising modifications to them in order to produce desired effects.[24] (p. 675)
- Recognizing interconnections: recognizing key connections between system parts.
- Identifying and understanding feedback: identifying cause-and-effect feedback loops and their impact on the system.
- Understanding system structure: understanding the elements of a system, how they are connected, and how they contribute to the way a system behaves.
- Differentiating types of stocks, flows, and variables: identifying pools of resources (stocks) in a system, changes in the amounts of those resources (flows), and the factors (variables) that contribute to those changes in both linear and non-linear ways.
- Understanding dynamic behaviour: understanding how feedback loops both influence and are influenced by stocks, flows, and variables.
- Reducing complexity by modelling systems conceptually: using methods such as reduction, transformation, abstraction, and homogenization to conceptually model a complex system in a more simplified and accessible manner.
- Understanding systems at different scales: recognizing that systems can be examined in different levels of detail and can be embedded within larger systems [24].
2.2.3. Context
2.3. Full-Text Screening
2.4. Data Extraction and Analysis
3. Results
- Local context and other implementation factors affect intervention outcomes [85].
| Study Citation | Region (Country) | Population | STI or BBV Focus | Aspects of Prevention and Control | Level of System | Systems Thinking Tools and Approaches |
|---|---|---|---|---|---|---|
| Adams et al. [59] | USA |
| HIV |
|
|
|
| Adams et al. [60] | USA |
| HIV |
|
|
|
| Adekola et al. [73] | Africa (South Africa) |
| Sexual health generally |
|
|
|
| Annadurai et al. [80] | Asia and Pacific (India) |
| Syphilis |
|
|
|
| Batchelder et al. [61] | USA |
| HIV |
|
|
|
| Beima-Sofie et al. [74] | Africa (Kenya) |
| HIV |
|
|
|
| Beltran et al. [81] | USA |
| HIV |
|
|
|
| Bezemer et al. [34] | Western European (Netherlands) |
| HIV |
|
|
|
| Bond et al. [84] | Africa (Zambia, South Africa) |
| HIV |
|
|
|
| Boruett et al. [35] | Africa (Kenya) |
| HIV |
|
|
|
| Bouchard et al. [54] | Canada |
| HIV Hepatitis B |
|
|
|
| Bousmah et al. [85] | Africa (South Africa) |
| HIV |
|
|
|
| Brown et al. [86] | Australia |
| HIV |
|
|
|
| Burman et al. [75] | Africa (South Africa) |
| HIV |
|
|
|
| Burman et al. [87] | Africa (South Africa) |
| HIV |
|
|
|
| Burman et al. [88] | Africa (South Africa) |
| HIV |
|
|
|
| Burman et al. [76] | Africa (South Africa) |
| HIV |
|
|
|
| Burman [89] | Africa (South Africa) |
| HIV |
|
|
|
| Burman et al. [90] | Africa (South Africa) |
| HIV |
|
|
|
| Caplon et al. [62] | USA |
| HIV |
|
|
|
| Czaja et al. [77] | USA |
| HIV Sexual health generally |
|
|
|
| De Boer and Lutscher [63] | Other (not specified) |
| HIV |
|
|
|
| du Toit and Craig [36] | General International |
| HIV |
|
|
|
| Dickson-Gomez et al. [37] | Latin American and Caribbean (El Salvador) |
| HIV |
|
|
|
| Eastment et al. [64] | Africa (Kenya) |
| HIV |
|
|
|
| Eastment et al. [65] | Africa (Kenya) |
| HIV |
|
|
|
| Eaton et al. [91] | Africa (South Africa) |
| HIV |
|
|
|
| Fujimoto et al. [82] | USA |
| HIV |
|
|
|
| Goncalves and Kamdem [38] | Africa (Cote d’Ivoire) |
| HIV |
|
|
|
| Gupta et al. [39] | General international |
| HIV |
|
|
|
| Harper et al. [78] | Africa (Kenya) |
| HIV |
|
|
|
| Khan et al. [55] | USA |
| HIV |
|
|
|
| Kiekens et al. [92] | Africa (Sub-Saharan Africa, countries not specified) |
| HIV |
|
|
|
| Kiekens et al. [93] | Africa (Sub-Saharan Africa, countries not specified) |
| HIV |
|
|
|
| Kiekens et al. [40] | Africa (Tanzania) |
| HIV |
|
|
|
| Kok et al. [94] | Canada |
| HIV |
|
|
|
| Levy et al. [41] | Africa (Kenya) |
| HIV |
|
|
|
| Long et al. [95] | Africa (Kenya) |
| HIV |
|
|
|
| Lopez-Entrambasaguas et al. [66] | Latin American and Caribbean (Bolivia) |
| HIV |
|
|
|
| Lounsbury et al. [67] | USA |
| HIV |
|
|
|
| Lutete et al. [42] | USA |
| HIV |
|
|
|
| Mabey et al. [68] | Africa (Tanzania, Uganda, Zambia) Asia and Pacific (China) Latin America and Caribbean (Peru, Brazil) |
| Syphilis |
|
|
|
| Marshall et al. [56] | USA |
| HIV |
|
|
|
| Martin et al. [96] | USA |
| HIV |
|
|
|
| Martin et al. [97] | USA |
| HIV |
|
|
|
| Mayhew et al. [69] | Africa (Kenya) |
| HIV Sexual health |
|
|
|
| McKay et al. [43] | USA |
| HIV |
|
|
|
| Omondi et al. [98] | Africa (Kenya) |
| HIV |
|
|
|
| Orievulu and Iwuji [44] | Africa (South Africa) |
| HIV |
|
|
|
| Orievulu et al. [45] | Africa (South Africa) |
| HIV |
|
|
|
| Palk et al. [83] | Western Europe (Denmark) |
| HIV |
|
|
|
| Pedamallu et al. [9] | Other (unspecified) |
| HIV |
|
|
|
| Riou et al. [46] | Africa (Botswana, Eswatini, Malawi, Mozambique, Namibia, South Africa, Zimbabwe, Lesotho) |
| HIV |
|
|
|
| Rustagi et al. [70] | Africa (Côte d’Ivoire, Kenya, Mozambique) |
| HIV |
|
|
|
| Sherr et al. [71] | Africa (Kenya, Cote d’Ivoire and Mozambique) |
| HIV |
|
|
|
| Stevens et al. [79] | USA |
| HIV |
|
|
|
| Sturmberg et al. [47] | Africa (Kenya) |
| HIV |
|
|
|
| Teng et al. [72] | USA |
| Chlamydia |
|
|
|
| Topp and Chipukuma [48] | Africa (Zambia) |
| HIV |
|
|
|
| Tuan [99] | Africa (South Africa) |
| HIV |
|
|
|
| Tulloch et al. [57] | Asia and Pacific (Thailand) |
| HIV |
|
|
|
| Viana et al. [10] | Western Europe (UK) |
| Chlamydia |
|
|
|
| Wagner et al. [49] | Africa (Kenya) |
| HIV |
|
|
|
| Wai et al. [50] | Canada |
| HIV |
|
|
|
| Weeks et al. [11] | Asia and Pacific (China) |
| HIV |
|
|
|
| Weeks et al. [53] | USA |
| HIV |
|
|
|
| Weeks et al. [51] | USA |
| HIV |
|
|
|
| Weeks et al. [52] | USA |
| HIV |
|
|
|
| Yaya Bocoum et al. [5] | Africa (Burkina Faso) |
| HIV |
|
|
|
| Zou et al. [58] | Asia and Pacific (China) |
| HIV |
|
|
|
4. Discussion
If there is a jungle of terminology used to describe scientific endeavor, it becomes even thicker in the area of systems thinking, perhaps because of its diverse heritage… It is based on a wide variety of scientific methods… It uses an even larger array of instruments or tools… The use of these terms is not consistent across or within scientific fields, including systems sciences, and the continuum from tool to method to theory and framework is often blurry.[2]
“the “fuzzy” boundary between [systems thinking] and other fields of focus like socio-ecological frameworks, network science, action research, participatory research, quality/implementation/improvement science, health services research, team science, and realist reviews, amongst others, reflects not only a key limitation of [their] review but also a challenge to those in health in trying to understand and apply these ideas”.[4] (p. 604)
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hossain, N.U.I.; Dayarathna, V.L.; Nagahi, M.; Jaradat, R. Systems Thinking: A review and bibliometric analysis. Systems 2020, 8, 23. [Google Scholar] [CrossRef]
- Peters, D.H. The application of systems thinking in health: Why use systems thinking? Health Res. Policy Syst. 2014, 12, 51. [Google Scholar] [CrossRef]
- Carey, G.; Malbon, E.; Carey, N.; Joyce, A.; Crammond, B.; Carey, A. Systems science and systems thinking for public health: A systematic review of the field. BMJ Open 2015, 5, e009002. [Google Scholar] [CrossRef] [PubMed]
- Rusoja, E.; Haynie, D.; Sievers, J.; Mustafee, N.; Nelson, F.; Reynolds, M.; Sarriot, E.; Swanson, R.C.; Williams, B. Thinking about complexity in health: A systematic review of the key systems thinking and complexity ideas in health. J. Eval. Clin. Pract. 2018, 24, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Yaya Bocoum, F.; Kouanda, S.; Kouyaté, B.; Hounton, S.; Adam, T. Exploring the effects of task shifting for HIV through a systems thinking lens: The case of Burkina Faso. BMC Public Health 2013, 13, 997. [Google Scholar] [CrossRef]
- Aral, S.O.; Leichliter, J.S.; Blanchard, J.F. Overview: The role of emergent properties of complex systems in the epidemiology and prevention of sexually transmitted infections including HIV infection. Sex. Transm. Infect. 2010, 86 (Suppl. 3), iii1-3. [Google Scholar] [CrossRef]
- Traeger, M.W.; Cornelisse, V.J.; Asselin, J.; Price, B.; Roth, N.J.; Willcox, J.; Tee, B.K.; Fairley, C.K.; Chang, C.C.; Armishaw, J.; et al. Association of HIV Preexposure Prophylaxis with incidence of sexually transmitted infections among individuals at high risk of HIV infection. JAMA 2019, 321, 1380–1390. [Google Scholar] [CrossRef] [PubMed]
- Latkin, C.; Weeks, M.R.; Glasman, L.; Galletly, C.; Albarracin, D. A dynamic social systems model for considering structural factors in HIV prevention and detection. AIDS Behav. 2010, 14 (Suppl. 2), 222–238. [Google Scholar] [CrossRef]
- Pedamallu, C.S.; Ozdamar, L.; Kropat, E.; Weber, G.-W. A system dynamics model for intentional transmission of HIV/AIDS using cross impact analysis. Cent. Eur. J. Oper. Res. 2012, 20, 319–336. [Google Scholar] [CrossRef]
- Viana, J.; Brailsford, S.C.; Harindra, V.; Harper, P.R. Combining discrete-event simulation and system dynamics in a healthcare setting: A composite model for Chlamydia infection. Eur. J. Oper. Res. 2014, 237, 196–206. [Google Scholar] [CrossRef]
- Weeks, M.R.; Li, J.; Liao, S.; Zhang, Q.; Dunn, J.; Wang, Y.; Jiang, J. Multilevel dynamic systems affecting introduction of HIV/STI prevention innovations among Chinese women in sex work establishments. Health Educ. Behav. 2013, 40 (Suppl. 1), 111s–122s. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health & Human Services. A Timeline of HIV and AIDS. Available online: https://www.hiv.gov/hiv-basics/overview/history/hiv-and-aids-timeline/ (accessed on 8 March 2023).
- Globerman, J.; Mitra, S.; Gogolishvili, D.; Rueda, S.; Schoffel, L.; Gangbar, K.; Shi, Q.; Rourke, S.B. HIV/STI prevention interventions: A systematic review and meta-analysis. Open Med. (Wars) 2017, 12, 450–467. [Google Scholar] [CrossRef] [PubMed]
- Clifford Astbury, C.; McGill, E.; Egan, M.; Penney, T.L. Systems thinking and complexity science methods and the policy process in non-communicable disease prevention: A systematic scoping review protocol. BMJ Open 2021, 11, e049878. [Google Scholar] [CrossRef]
- Bramer, W.M.; Rethlefsen, M.L.; Kleijnen, J.; Franco, O.H. Optimal database combinations for literature searches in systematic reviews: A prospective exploratory study. Syst. Rev. 2017, 6, 245. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Collins, A.M.; Coughlin, D.; Kirk, S. The role of Google Scholar in evidence reviews and its applicability to grey literature searching. PLoS ONE 2015, 10, e0138237. [Google Scholar] [CrossRef]
- Paez, A. Grey literature: An important resource in systematic reviews. J. Evid. Based Med. 2017, 10, 233. [Google Scholar] [CrossRef]
- The Endnote Team. Endnote, Endnote X20; Clarivate: Philadelphia, PA, USA, 2013. [Google Scholar]
- Bramer, W.M.; Giustini, D.; de Jonge, G.B.; Holland, L.; Bekhuis, T. De-duplication of database search results for systematic reviews in EndNote. J. Med. Libr. Assoc. 2016, 104, 240–243. [Google Scholar] [CrossRef]
- Munn, Z.; Aromataris, E.; Tufanaru, C.; Stern, C.; Porritt, K.; Farrow, J.; Lockwood, C.; Stephenson, M.; Moola, S.; Lizarondo, L.; et al. The development of software to support multiple systematic review types: The Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI SUMARI). Int. J. Evid. Based Healthc. 2019, 17, 36–43. [Google Scholar] [CrossRef]
- World Health Organization. Adolescent Health. Available online: https://www.who.int/health-topics/adolescent-health#tab=tab_1 (accessed on 4 January 2023).
- Arnold, R.D.; Wade, J.P. A definition of systems thinking: A systems approach. Procedia Comput. Sci. 2015, 44, 669–678. [Google Scholar] [CrossRef]
- National Cancer Institute NCI Dictionary of Cancer Terms. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/sti (accessed on 4 January 2023).
- Van Seventer, J.M.; Hochberg, N.S. Principles of infectious diseases: Transmission, diagnosis, prevention, and control. Int. Encycl. Public Health 2017, volume, 22–39. [Google Scholar]
- Dowdle, W.R. The principles of disease elimination and eradication. Bull World Health Organ 1998, 76 (Suppl. 2), 22–25. [Google Scholar]
- Abdullah, M.A.; Shaikh, B.T.; Ghazanfar, H. Curing or causing? HIV/AIDS in health care system of Punjab, Pakistan. PLoS ONE 2021, 16, e0254476. [Google Scholar] [CrossRef]
- Adam, P.C.G.; de Wit, J.B.F.; Bourne, C.P.; Knox, D.; Purchas, J. Promoting regular testing: An examination of HIV and STI testing routines and associated socio-demographic, behavioral and social-cognitive factors among men who have sex with men in New South Wales, Australia. AIDS Behav. 2014, 18, 921–932. [Google Scholar] [CrossRef] [PubMed]
- Farel, C.E.; Parker, S.D.; Muessig, K.E.; Grodensky, C.A.; Jones, C.; Golin, C.E.; Fogel, C.I.; Wohl, D.A. Sexuality, sexual practices, and HIV risk among incarcerated African-American women in North Carolina. Women’s Health Issues 2013, 23, e357–e364. [Google Scholar] [CrossRef] [PubMed]
- Joore, I.K.; van Roosmalen, S.L.; van Bergen, J.E.; van Dijk, N. General practitioners’ barriers and facilitators towards new provider-initiated HIV testing strategies: A qualitative study. Int. J. STD AIDS 2017, 28, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Govender, K.; Cowden, R.G.; Asante, K.O.; George, G.; Reardon, C. Sexual risk behavior: A multi-system model of risk and protective factors in South African adolescents. Prev. Sci. 2019, 20, 1054–1065. [Google Scholar] [CrossRef]
- Monat, J.P.; Gannon, T.F. What is systems thinking? A review of selected literature plus recommendations. Am. J. Syst. Sci. 2015, 4, 11–26. [Google Scholar]
- Bezemer, D.; Cori, A.; Ratmann, O.; van Sighem, A.; Hermanides, H.S.; Dutilh, B.E.; Gras, L.; Rodrigues Faria, N.; van den Hengel, R.; Duits, A.J.; et al. Dispersion of the HIV-1 epidemic in men who have sex with men in the Netherlands: A combined mathematical model and phylogenetic analysis. PLoS Med. 2015, 12, e1001898. [Google Scholar] [CrossRef]
- Boruett, P.; Kagai, D.; Njogo, S.; Nguhiu, P.; Awuor, C.; Gitau, L.; Chalker, J.; Ross-Degnan, D.; Wahlström, R.; Tomson, G. Facility-level intervention to improve attendance and adherence among patients on anti-retroviral treatment in Kenya—A quasi-experimental study using time series analysis. BMC Health Serv. Res. 2013, 13, 242. [Google Scholar] [CrossRef] [PubMed]
- Du Toit, E.F.; Craig, I.K. Selective pinning control of the average disease transmissibility in an HIV contact network. Phys. Rev. E 2015, 92, 012810. [Google Scholar] [CrossRef] [PubMed]
- Dickson-Gomez, J.; Glasman, L.A.; Bodnar, G.; Murphy, M. A social systems analysis of implementation of El Salvador’s national HIV combination prevention: A research agenda for evaluating Global Health Initiatives. BMC Health Serv. Res. 2018, 18, 848. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, P.; Kamdem, S.T. Reaching an AIDS-free generation in Côte d’Ivoire-Data driven policy design for HIV/AIDS response programs: Evidence-based policy design for HIV/AIDS response programs in Côte d’Ivoire. Int. J. Syst. Dyn. Appl. 2016, 5, 43–62. [Google Scholar] [CrossRef]
- Gupta, C.; Tuncer, N.; Martcheva, M. A network immuno-epidemiological HIV model. Bull. Math. Biol. 2021, 83, 18. [Google Scholar] [CrossRef] [PubMed]
- Kiekens, A.; Mosha, I.H.; Zlatić, L.; Bwire, G.M.; Mangara, A.; Dierckx de Casterlé, B.; Decouttere, C.; Vandaele, N.; Sangeda, R.Z.; Swalehe, O.; et al. Factors associated with HIV drug resistance in Dar es Salaam, Tanzania: Analysis of a complex adaptive system. Pathogens 2021, 10, 1535. [Google Scholar] [CrossRef]
- Levy, B.; Correia, H.E.; Chirove, F.; Ronoh, M.; Abebe, A.; Kgosimore, M.; Chimbola, O.; Machingauta, M.H.; Lenhart, S.; White, K.A.J. Modeling the effect of HIV/AIDS stigma on HIV infection dynamics in Kenya. Bull. Math. Biol. 2021, 83, 55. [Google Scholar] [CrossRef]
- Lutete, P.; Matthews, D.W.; Sabounchi, N.S.; Paige, M.Q.; Lounsbury, D.W.; Rodriguez, N.; Echevarria, N.; Usher, D.; Walker, J.J.; Dickerson, A.; et al. Intersectional stigma and prevention among gay, bisexual, and same gender-loving men in New York City, 2020: System Dynamics Models. Am. J. Public Health 2022, 112 (Suppl. 4), S444–S451. [Google Scholar] [CrossRef]
- McKay, V.R.; Cambey, C.L.; Combs, T.B.; Stubbs, A.W.; Pichon, L.C.; Gaur, A.H. Using a modeling-based approach to assess and optimize HIV linkage to care services. AIDS Behav. 2021, 25, 886–896. [Google Scholar] [CrossRef]
- Orievulu, K.; Ayeb-Karlsson, S.; Ngwenya, N.; Ngema, S.; McGregor, H.; Adeagbo, O.; Siedner, M.J.; Hanekom, W.; Kniveton, D.; Seeley, J.; et al. Economic, social and demographic impacts of drought on treatment adherence among people living with HIV in rural South Africa: A qualitative analysis. Clim. Risk Manag. 2022, 36, 100423. [Google Scholar] [CrossRef]
- Orievulu, K.S.; Iwuji, C.C. Institutional Responses to Drought in a High HIV Prevalence Setting in Rural South Africa. Int. J. Environ. Res. Public Health 2021, 19, 434. [Google Scholar] [CrossRef] [PubMed]
- Riou, J.; Dupont, C.; Bertagnolio, S.; Gupta, R.K.; Kouyos, R.D.; Egger, M.; L. Althaus, C. Drivers of HIV-1 drug resistance to non-nucleoside reverse-transcriptase inhibitors (NNRTIs) in nine southern African countries: A modelling study. BMC Infect. Dis. 2021, 21, 1042. [Google Scholar]
- Sturmberg, J.P.; Njoroge, A. People-centred health systems, a bottom-up approach: Where theory meets empery. J. Eval. Clin. Pract. 2017, 23, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Topp, S.M.; Chipukuma, J.M. How did rapid scale-up of HIV services impact on workplace and interpersonal trust in Zambian primary health centres: A case-based health systems analysis. BMJ Glob. Health 2016, 1, e000179. [Google Scholar] [CrossRef]
- Wagner, A.D.; Augusto, O.; Njuguna, I.N.; Gaitho, D.; Mburu, N.; Oluoch, G.; Carimo, N.; Mwaura, P.; Cherutich, P.; Oyiengo, L.; et al. Systems analysis and improvement approach to optimize the pediatric and adolescent HIV Cascade (SAIA-PEDS): A pilot study. Implement. Sci. Commun. 2022, 3, 49. [Google Scholar] [CrossRef]
- Wai, B.; Vasarhelyi, K.; Rutherford, A.R.; Buchner, C.; Gustafson, R.; Compton, M.; Hull, M.; Williams, J.; Barrios, R. A qualitative model of the HIV care continuum in Vancouver, Canada. Heal. Syst. 2021, 11, 84–97. [Google Scholar] [CrossRef]
- Weeks, M.R.; Green Montaque, H.D.; Lounsbury, D.W.; Li, J.; Ferguson, A.; Warren-Dias, D. Using participatory system dynamics learning to support Ryan White Planning Council priority setting and resource allocations. Eval. Program Plan. 2022, 93, 102104. [Google Scholar] [CrossRef]
- Weeks, M.R.; Lounsbury, D.W.; Li, J.; Hirsch, G.; Berman, M.; Green, H.D.; Rohena, L.; Gonzalez, R.; Montezuma-Rusca, J.M.; Jackson, S. Simulating system dynamics of the HIV care continuum to achieve treatment as prevention. PLoS ONE 2020, 15, e0230568. [Google Scholar] [CrossRef]
- Weeks, M.R.; Li, J.; Lounsbury, D.; Green, H.D.; Abbott, M.; Berman, M.; Rohena, L.; Gonzalez, R.; Lang, S.; Mosher, H. Using Participatory System Dynamics Modeling to Examine the Local HIV Test and Treatment Care Continuum in Order to Reduce Community Viral Load. Am. J. Community Psychol. 2017, 60, 584–598. [Google Scholar] [CrossRef]
- Bouchard, M.; Hashimi, S.; Tsai, K.; Lampkin, H.; Jozaghi, E. Back to the core: A network approach to bolster harm reduction among persons who inject drugs. Int. J. Drug Policy 2018, 51, 95–104. [Google Scholar] [CrossRef]
- Khan, B.; Dombrowski, K.; Saad, M.; McLean, K.; Friedman, S. Network firewall dynamics and the subsaturation stabilization of HIV. Discret. Dyn. Nat. Soc. 2013, 2013, 720818. [Google Scholar] [CrossRef] [PubMed]
- Marshall, B.D.L.; Paczkowski, M.M.; Seemann, L.; Tempalski, B.; Pouget, E.R.; Galea, S.; Friedman, S.R. A Complex Systems Approach to Evaluate HIV Prevention in Metropolitan Areas: Preliminary Implications for Combination Intervention Strategies. PLoS ONE 2012, 7, e44833. [Google Scholar] [CrossRef] [PubMed]
- Tulloch, O.; Taegtmeyer, M.; Ananworanich, J.; Chasombat, S.; Kosalaraksa, P.; Theobald, S. What can volunteer co-providers contribute to health systems? The role of people living with HIV in the Thai paediatric HIV programme. Soc. Sci. Med. 2015, 145, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Zou, X.; Xu, Y.; Chen, W.; Xia, Y.; Liu, Y.; Gong, C.; Ling, L. Strategies to control HIV and HCV in methadone maintenance treatment in Guangdong Province, China: A system dynamic modeling study. Subst. Abus. Treat. Prev. Policy 2018, 13, 1. [Google Scholar] [CrossRef]
- Adams, J.W.; Lurie, M.N.; King, M.R.F.; Brady, K.A.; Galea, S.; Friedman, S.R.; Khan, M.R.; Marshall, B.D.L. Potential drivers of HIV acquisition in African-American women related to mass incarceration: An agent-based modelling study. BMC Public Health 2018, 18, 1387. [Google Scholar] [CrossRef]
- Adams, J.W.; Lurie, M.N.; King, M.R.F.; Brady, K.A.; Galea, S.; Friedman, S.R.; Khan, M.R.; Marshall, B.D.L. Decreasing HIV transmissions to African American women through interventions for men living with HIV post-incarceration: An agent-based modeling study. PLoS ONE 2019, 14, e0219361. [Google Scholar] [CrossRef]
- Batchelder, A.W.; Gonzalez, J.S.; Palma, A.; Schoenbaum, E.; Lounsbury, D.W. A social ecological model of syndemic risk affecting women with and at-risk for HIV in impoverished urban communities. Am. J. Community Psychol. 2015, 56, 229–240. [Google Scholar] [CrossRef]
- Caplon, A.; Alexander, K.A.; Kershaw, T.; Willie, T.C. Assessing provider-, clinic-, and structural-level barriers and recommendations to Pre-Exposure Prophylaxis (PrEP) uptake: A qualitative investigation among women experiencing intimate partner violence, intimate partner violence service providers, and healthcare providers. AIDS Behav. 2021, 25, 3425–3436. [Google Scholar]
- De Boer, R.; Lutscher, F. Choice disability as a target for non-medical HIV intervention. Math. Biosci. 2018, 299, 127–137. [Google Scholar] [CrossRef]
- Eastment, M.C.; Long, J.E.; Wanje, G.; Richardson, B.A.; Mwaringa, E.; Sherr, K.; Barnabas, R.V.; Mandaliya, K.; Jaoko, W.; McClelland, R.S. Qualitative evaluation of the Systems Analysis and Improvement Approach as a strategy to increase HIV testing in family planning clinics using the Consolidated Framework for Implementation Research and the Implementation Outcomes Framework. Implement. Sci. Commun. 2022, 3, 97. [Google Scholar] [CrossRef]
- Eastment, M.C.; Wanje, G.; Richardson, B.A.; Mwaringa, E.; Sherr, K.; Barnabas, R.V.; Perla, M.; Mandaliya, K.; Jaoko, W.; McClelland, R.S. Results of a cluster randomized trial testing the systems analysis and improvement approach to increase HIV testing in family planning clinics. Aids 2022, 36, 225–235. [Google Scholar] [CrossRef] [PubMed]
- López-Entrambasaguas, O.M.; Granero-Molina, J.; Fernández-Sola, C. An ethnographic study of HIV/AIDS among Ayoreo sex workers: Cultural factors and risk perception. J. Clin. Nurs. 2013, 22, 3337–3348. [Google Scholar] [CrossRef]
- Lounsbury, D.W.; Schwartz, B.; Palma, A.; Blank, A. Simulating patterns of patient engagement, treatment adherence, and viral suppression: A system dynamics approach to evaluating HIV care management. AIDS Patient Care STDS 2015, 29 (Suppl. 1), S55–S63. [Google Scholar] [CrossRef] [PubMed]
- Mabey, D.C.; Sollis, K.A.; Kelly, H.A.; Benzaken, A.S.; Bitarakwate, E.; Changalucha, J.; Chen, X.-S.; Yin, Y.-P.; Garcia, P.J.; Strasser, S.; et al. Point-of-Care Tests to Strengthen Health Systems and Save Newborn Lives: The Case of Syphilis. PLoS Med. 2012, 9, e1001233. [Google Scholar] [CrossRef]
- Mayhew, S.H.; Sweeney, S.; E Warren, C.; Collumbien, M.; Ndwiga, C.; Mutemwa, R.; Lut, I.; Colombini, M.; Vassall, A.; Initiative, I. Numbers, systems, people: How interactions influence integration. Insights from case studies of HIV and reproductive health services delivery in Kenya. Health Policy Plan. 2017, 32 (Suppl. 4), iv67–iv81. [Google Scholar] [CrossRef]
- Rustagi, A.S.; Gimbel, S.; Nduati, R.; Cuembelo Mde, F.; Wasserheit, J.N.; Farquhar, C.; Gloyd, S.; Sherr, K. Implementation and operational research: Impact of a systems engineering *intervention on PMTCT service delivery in Côte d’Ivoire, Kenya, Mozambique: A cluster randomized trial. J. Acquir. Immune Defic. Syndr. 2016, 72, e68–e76. [Google Scholar] [CrossRef] [PubMed]
- Sherr, K.; Gimbel, S.; Rustagi, A.; Nduati, R.; Cuembelo, F.; Farquhar, C.; Wasserheit, J.; Gloyd, S. With input from the, S. S. T. Systems analysis and improvement to optimize pMTCT (SAIA): A cluster randomized trial. Implement. Sci. 2014, 9, 55. [Google Scholar] [CrossRef]
- Teng, Y.; Kong, N.; Tu, W. Optimizing strategies for population-based chlamydia infection screening among young women: An age-structured system dynamics approach. BMC Public Health 2015, 15, 639. [Google Scholar] [CrossRef] [PubMed]
- Adekola, A.P.; Mavhandu-Mudzusi, A.H. Advancing sexual and reproductive health outcomes in rural schools with the use of a sexuality education enhancement model: Learners’ perspectives. Heliyon 2022, 8, e11189. [Google Scholar] [CrossRef] [PubMed]
- Beima-Sofie, K.; Wagner, A.D.; Soi, C.; Liu, W.; Tollefson, D.; Njuguna, I.N.; Ogutu, E.; Gaitho, D.; Mburu, N.; Oluoch, G.; et al. Providing “a beam of light to see the gaps”: Determinants of implementation of the Systems Analysis and Improvement Approach applied to the pediatric and adolescent HIV cascade in Kenya. Implement. Sci. Commun. 2022, 3, 73. [Google Scholar] [CrossRef]
- Burman, C.; Aphane, M.; Mamabolo, R.; Mtapuri, O.; Delobelle, P. The process of developing distributed-efficacy and social practice in the context of ‘ending AIDS’. J. Transdiscipl. Res. South. Afr. 2015, 11, 25. [Google Scholar] [CrossRef]
- Burman, C.; Moerschell, L.; Mamabolo, R.; Aphane, M.; Delobelle, P. Re-imagining decision making: Addressing a discrete social driver of HIV/AIDS through the lens of complexity science. Afr. J. AIDS Res. 2015, 14, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Czaja, S.J.; Valente, T.W.; Nair, S.N.; Villamar, J.A.; Brown, C.H. Characterizing implementation strategies using a systems engineering survey and interview tool: A comparison across 10 prevention programs for drug abuse and HIV sexual risk behavior. Implement. Sci. 2016, 11, 70. [Google Scholar] [CrossRef] [PubMed]
- Harper, G.W.; Riplinger, A.J.; Neubauer, L.C.; Murphy, A.G.; Velcoff, J.; Bangi, A.K. Ecological factors influencing HIV sexual risk and resilience among young people in rural Kenya: Implications for prevention. Health Educ. Res. 2013, 29, 131–146. [Google Scholar] [CrossRef] [PubMed]
- Stevens, R.; Bernadini, S.; Jemmott, J.B. Social environment and sexual risk-taking among gay and transgender African American youth. Cult. Health Sex. 2013, 15, 1148–1161. [Google Scholar] [CrossRef]
- Annadurai, K.; Bagavandas, M. A systematic approach for early identification of syphilis infection among mwn having sex with men in Chennai City: A page rank based approach. Indian J. Community Health 2017, 29, 389–395. [Google Scholar] [CrossRef]
- Beltran, R.M.; Schuyler, A.C.; Blair, C.S.; Goldbach, J.T.; Castro, C.A.; Holloway, I. “That’s kind of like the big struggle right now is can we get PrEP?”: Facilitators and barriers to PrEP uptake among active duty gay and bisexual men. Sex. Res. Soc. Policy 2021. [Google Scholar] [CrossRef]
- Fujimoto, K.; Wang, P.; Flash, C.A.; Kuhns, L.M.; Zhao, Y.; Amith, M.; Schneider, J.A. Network Modeling of PrEP uptake on referral networks and health venue utilization among young men who have sex with men. AIDS Behav. 2019, 23, 1698–1707. [Google Scholar] [CrossRef]
- Palk, L.; Gerstoft, J.; Obel, N.; Blower, S. A modeling study of the Danish HIV epidemic in men who have sex with men: Travel, pre-exposure prophylaxis and elimination. Sci. Rep. 2018, 8, 16003. [Google Scholar] [CrossRef]
- Bond, V.; Hoddinott, G.; Viljoen, L.; Ngwenya, F.; Simuyaba, M.; Chiti, B.; Ndubani, R.; Makola, N.; Donnell, D.; Schaap, A.; et al. How ‘place’ matters for addressing the HIV epidemic: Evidence from the HPTN 071 (PopART) cluster-randomised controlled trial in Zambia and South Africa. Trials 2021, 22, 251. [Google Scholar] [CrossRef]
- Bousmah, M.A.; Iwuji, C.; Okesola, N.; Orne-Gliemann, J.; Pillay, D.; Dabis, F.; Larmarange, J.; Boyer, S. Costs and economies of scale in repeated home-based HIV counselling and testing: Evidence from the ANRS 12249 treatment as prevention trial in South Africa. Soc. Sci. Med. 2022, 305, 115068. [Google Scholar] [CrossRef] [PubMed]
- Brown, G.; Reeders, D.; Cogle, A.; Madden, A.; Kim, J.; O’Donnell, D. A Systems thinking approach to understanding and demonstrating the role of peer-led programs and leadership in the response to HIV and hepatitis C: Findings from the W3 Project. Front. Public Health 2018, 6, 231. [Google Scholar] [CrossRef]
- Burman, C.J.; Aphane, M.; Delobelle, P. Weak signal detection: A discrete window of opportunity for achieving ‘Vision 90:90:90’? SAHARA J. 2016, 13, 17–34. [Google Scholar] [CrossRef] [PubMed]
- Burman, C.J.; Aphane, M.; Mtapuri, O.; Delobelle, P. Expanding the prevention armamentarium portfolio: A framework for promoting HIV-Conversant Communities within a complex, adaptive epidemiological landscape. SAHARA J. 2015, 12, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Burman, C.J. The Taming Wicked Problems Framework: A plausible biosocial contribution to ‘ending AIDS by 2030’. J. Transdiscipl. Res. South. Afr. 2018, 14, 1–12. [Google Scholar] [CrossRef]
- Burman, C.J.; Aphane, M.; Delobelle, P. Reducing the overall HIV-burden in South Africa: Is ‘reviving ABC’ an appropriate fit for a complex, adaptive epidemiological HIV landscape? Afr. J. AIDS Res. 2015, 14, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Eaton, J.W.; Johnson, L.F.; Salomon, J.A.; Bärnighausen, T.; Bendavid, E.; Bershteyn, A.; Bloom, D.E.; Cambiano, V.; Fraser, C.; Hontelez, J.A.C.; et al. HIV Treatment as Prevention: Systematic Comparison of Mathematical Models of the Potential Impact of Antiretroviral Therapy on HIV Incidence in South Africa. PLoS Med. 2012, 9, e1001245. [Google Scholar] [CrossRef] [PubMed]
- Kiekens, A.; de Casterlé, B.D.; Vandamme, A.-M. Qualitative systems mapping for complex public health problems: A practical guide. PLoS ONE 2022, 17, e0264463. [Google Scholar] [CrossRef]
- Kiekens, A.; de Casterlé, B.D.; Pellizzer, G.; Mosha, I.H.; Mosha, F.; de Wit, T.F.R.; Sangeda, R.Z.; Surian, A.; Vandaele, N.; Vranken, L.; et al. Exploring the mechanisms behind HIV drug resistance in sub-Saharan Africa: Conceptual mapping of a complex adaptive system based on multi-disciplinary expert insights. BMC Public Health 2022, 22, 455. [Google Scholar] [CrossRef]
- Kok, S.; Vancouver HIV Testing Program Modelling Group; Rutherford, A.R.; Gustafson, R.; Barrios, R.; Montaner, J.S.G.; Vasarhelyi, K. Optimizing an HIV testing program using a system dynamics model of the continuum of care. Heal. Care Manag. Sci. 2015, 18, 334–362. [Google Scholar] [CrossRef]
- Long, J.E.; Eastment, M.C.; Wanje, G.; Richardson, B.A.; Mwaringa, E.; Mohamed, M.A.; Sherr, K.; Barnabas, R.V.; Mandaliya, K.; Jaoko, W.; et al. Assessing the sustainability of the Systems Analysis and Improvement Approach to increase HIV testing in family planning clinics in Mombasa, Kenya: Results of a cluster randomized trial. Implement. Sci. 2022, 17, 70. [Google Scholar] [CrossRef] [PubMed]
- Martin, E.G.; MacDonald, R.H.; Smith, L.C.; Gordon, D.E.; Tesoriero, J.M.; Laufer, F.N.; Leung, S.-Y.J.; O’Connell, D.A. Policy Modeling to Support Administrative Decisionmaking on the New York State Hiv Testing Law. J. Policy Anal. Manag. 2015, 34, 403–423. [Google Scholar] [CrossRef] [PubMed]
- Martin, E.G.; MacDonald, R.H.; Smith, L.C.; Gordon, D.E.; Tesoriero, J.M.; Laufer, F.N.; Leung, S.Y.; Rowe, K.A.; O’Connell, D.A. Mandating the offer of HIV testing in New York: Simulating the epidemic impact and resource needs. J Acquir. Immune Defic. Syndr. 2015, 68 (Suppl. 1), S59–S67. [Google Scholar] [CrossRef]
- Omondi, E.O.; Mbogo, R.W.; Luboobi, L.S. Mathematical modelling of the impact of testing, treatment and control of HIV transmission in Kenya. Cogent Math. Stat. 2018, 5, 1475590. [Google Scholar] [CrossRef]
- Tuan, N.-T. A Systemic Inquiry into the AIDS Epidemic in the Western Cape of South Africa through Interactive Management. Syst. Pract. Action Res. 2018, 31, 421–435. [Google Scholar] [CrossRef]
- Amagoh, F. Systems and Complexity Theories of Organizations. In Global Encyclopedia of Public Administration, Public Policy, and Governance; Farazmand, A., Ed.; Springer International Publishing: Cham, Switzerland, 2016; pp. 1–7. [Google Scholar]
- Favaretto, M.; De Clercq, E.; Schneble, C.O.; Elger, B.S. What is your definition of Big Data? Researchers’ understanding of the phenomenon of the decade. PLoS ONE 2020, 15, e0228987. [Google Scholar] [CrossRef]
- Ayala, R.A. Thinking of conceptual reviews and systematic reviews. Nurs. Inq. 2018, 25, e12264. [Google Scholar] [CrossRef]
- Richardson, M.; Ramsay, L.C.; Bielecki, J.M.; Berta, W.; Sander, B. Systems thinking in health technology assessment: A scoping review. Int. J. Technol. Assess. Health Care 2021, 37, e71. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Yu, Q.; Lin, Y.; Zhou, Y.; Lan, L.; Yang, S.; Wu, J. Global burden and trends of sexually transmitted infections from 1990 to 2019: An observational trend study. Lancet Infect. Dis. 2022, 22, 541–551. [Google Scholar] [CrossRef]
- Srivastava, S.; Nambiar, D. Pivoting from systems “thinking” to systems “doing” in health systems—Documenting stakeholder perspectives from Southeast Asia. Front. Public Health 2022, 10, 2521. [Google Scholar] [CrossRef]
- Minichiello, V.; Rahman, S.; Hussain, R. Epidemiology of sexually transmitted infections in global indigenous populations: Data availability and gaps. Int. J. STD AIDS 2013, 24, 759–768. [Google Scholar] [CrossRef]
- Santoso, D.; Asfia, S.K.B.M.; Mello, M.B.; Baggaley, R.C.; Johnson, C.C.; Chow, E.P.F.; Fairley, C.K.; Ong, J.J. HIV prevalence ratio of international migrants compared to their native-born counterparts: A systematic review and meta-analysis. eClinicalMedicine 2022, 53, 101661. [Google Scholar] [CrossRef] [PubMed]
- Hernández, A.; Ruano, A.L.; Marchal, B.; San Sebastián, M.; Flores, W. Engaging with complexity to improve the health of indigenous people: A call for the use of systems thinking to tackle health inequity. Int. J. Equity Health 2017, 16, 26. [Google Scholar] [CrossRef]
- Roux, A.V.D. Complex systems thinking and current impasses in health disparities research. Am. J. Public Health 2011, 101, 1627–1634. [Google Scholar] [CrossRef] [PubMed]
- Pocock, N.S.; Chan, Z.; Loganathan, T.; Suphanchaimat, R.; Kosiyaporn, H.; Allotey, P.; Chan, W.-K.; Tan, D. Moving towards culturally competent health systems for migrants? Applying systems thinking in a qualitative study in Malaysia and Thailand. PLoS ONE 2020, 15, e0231154. [Google Scholar] [CrossRef]
- Kunpeuk, W.; Teekasap, P.; Kosiyaporn, H.; Julchoo, S.; Phaiyarom, M.; Sinam, P.; Pudpong, N.; Suphanchaimat, R. Understanding the problem of access to public health insurance schemes among cross-border migrants in Thailand through systems thinking. Int. J. Environ. Res. Public Health 2020, 17, 5113. [Google Scholar] [CrossRef] [PubMed]
- Durham, J.; Schubert, L.; Vaughan, L.; Willis, C.D. Using systems thinking and the Intervention Level Framework to analyse public health planning for complex problems: Otitis media in Aboriginal and Torres Strait Islander children. PLoS ONE 2018, 13, e0194275. [Google Scholar] [CrossRef]
- Browne, J.; Walker, T.; Brown, A.; Sherriff, S.; Christidis, R.; Egan, M.; Versace, V.; Allender, S.; Backholer, K. Systems thinking for Aboriginal Health: Understanding the value and acceptability of group model building approaches. SSM Popul. Health 2021, 15, 100874. [Google Scholar] [CrossRef] [PubMed]
- Tsuboi, M.; Evans, J.; Davies, E.P.; Rowley, J.; Korenromp, E.L.; Clayton, T.; Taylor, M.M.; Mabey, D.; Chico, R.M. Prevalence of syphilis among men who have sex with men: A global systematic review and meta-analysis from 2000–2020. Lancet Glob. Health 2021, 9, e1110–e1118. [Google Scholar] [CrossRef]
- Fu, L.; Sun, Y.; Han, M.; Wang, B.; Xiao, F.; Zhou, Y.; Gao, Y.; Fitzpatrick, T.; Yuan, T.; Li, P.; et al. Incidence trends of five common sexually transmitted infections excluding HIV from 1990 to 2019 at the global, regional, and national levels: Results from the Global Burden of Disease Study 2019. Front. Med. 2022, 9, 851635. [Google Scholar] [CrossRef]
- Unemo, M.; Lahra, M.M.; Escher, M.; Eremin, S.; Cole, M.J.; Galarza, P.; Ndowa, F.; Martin, I.; Dillon, J.-A.R.; Galas, M.; et al. WHO global antimicrobial resistance surveillance for Neisseria gonorrhoeae 2017–2018: A retrospective observational study. Lancet Microbe 2021, 2, e627–e636. [Google Scholar] [CrossRef]
- Cohen, M.S.; Council, O.D.; Chen, J.S. Sexually transmitted infections and HIV in the era of antiretroviral treatment and prevention: The biologic basis for epidemiologic synergy. J. Int. AIDS Soc. 2019, 22, e25355. [Google Scholar] [CrossRef] [PubMed]
- Rojas Castro, D.; Delabre, R.M.; Molina, J.-M. Give PrEP a chance: Moving on from the “risk compensation” concept. J. Int. AIDS Soc. 2019, 22, e25351. [Google Scholar] [CrossRef] [PubMed]
- Atun, R. Health systems, systems thinking and innovation. Health Policy Plan. 2012, 27 (Suppl. 4), iv4–iv8. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Consolidated Guidelines on HIV Testing Services for a Changing Epidemic; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Nagai, H.; Tagoe, H.; Tun, W.; Adiibokah, E.; Ankomah, A.; Rahman, Y.A.A.; Addo, S.A.; Atuahene, S.K.; Essandoh, E.; Kowalski, M. Perspectives of policymakers on the introduction and scale-up of HIV self-testing and implication for national HIV programming in Ghana. Front. Public Health 2021, 9, 694836. [Google Scholar] [CrossRef]
- Piltch-Loeb, R.; Kraemer, J.; Nelson, C.; Savoia, E.; Osborn, D.R.; Stoto, M.A. Root-cause analysis for enhancing public health emergency preparedness: A brief report of a Salmonella outbreak in the Alamosa, Colorado, water supply. J. Public Health Manag. Pract. 2018, 24, 542–545. [Google Scholar] [CrossRef]
- Wawrzyniak, K.M.; Sabo, A.; McDonald, A.; Trudeau, J.J.; Poulose, M.; Brown, M.; Katz, N.P. Root cause analysis of prescription opioid overdoses. J. Opioid Manag. 2015, 11, 127–137. [Google Scholar] [CrossRef]
- Simuyemba, M.C.; Bwembya, P.A.; Chola, M.; Michelo, C. A root cause analysis of sub-optimal uptake and compliance to iron and folic acid supplementation in pregnancy in 7 districts of Zambia. BMC Pregnancy Childbirth 2020, 20, 20. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vujcich, D.; Roberts, M.; Selway, T.; Nattabi, B. The Application of Systems Thinking to the Prevention and Control of Sexually Transmissible Infections among Adolescents and Adults: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 5708. https://doi.org/10.3390/ijerph20095708
Vujcich D, Roberts M, Selway T, Nattabi B. The Application of Systems Thinking to the Prevention and Control of Sexually Transmissible Infections among Adolescents and Adults: A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(9):5708. https://doi.org/10.3390/ijerph20095708
Chicago/Turabian StyleVujcich, Daniel, Meagan Roberts, Tyler Selway, and Barbara Nattabi. 2023. "The Application of Systems Thinking to the Prevention and Control of Sexually Transmissible Infections among Adolescents and Adults: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 9: 5708. https://doi.org/10.3390/ijerph20095708
APA StyleVujcich, D., Roberts, M., Selway, T., & Nattabi, B. (2023). The Application of Systems Thinking to the Prevention and Control of Sexually Transmissible Infections among Adolescents and Adults: A Scoping Review. International Journal of Environmental Research and Public Health, 20(9), 5708. https://doi.org/10.3390/ijerph20095708






