Psychosocial Processes in Healthcare Workers: How Individuals’ Perceptions of Interpersonal Communication Is Related to Patient Safety Threats and Higher-Quality Care
Abstract
1. Introduction
- Doctor–patient communication: One of the most important forms of interpersonal communication in hospitals is the interaction between medical doctors/physicians and patients. Effective communication between doctors and patients can help build trust, alleviate anxiety, and improve patient outcomes. For example, a physician might explain a medical diagnosis or treatment plan to a patient clearly and empathetically, which can help the patient feel more comfortable and confident in their care, help compliance, and help them be satisfied with the treatment outcomes [23,24,25].
- Nurse–patient communication: Nurses also play a critical role in patient care, and effective communication between nurses and patients is essential for providing high-quality care. Nurses might use interpersonal communication skills to listen to patients’ concerns, explain medications or treatments, or provide emotional support during difficult times [23,24,25].
- Interdisciplinary team communication: In hospitals, interdisciplinary teams of healthcare professionals often work together to provide coordinated care to patients. Effective communication between team members can help ensure patients receive appropriate care and avoid unnecessary complications and confusion [23,24,26].
- Communication with accompanying persons such as partners and family members: Hospitalization can be a stressful and emotional experience for patients and their families. Effective communication between healthcare providers and accompanying persons can help ease anxiety and improve patient outcomes. For example, a HCW might communicate with a patient’s family about their loved one’s condition, treatment plan, or discharge instructions [24,25,27].
- Prenatal care provider–patient communication: Effective communication between the obstetric care provider and the patient is essential to ensure the health and well-being of the mother and baby. During prenatal visits, the obstetrician or midwife might use interpersonal communication skills to discuss the pregnancy’s progress, address any concerns, and explain what to expect during the next stages of pregnancy [24,27].
- Labor and delivery communication: Communication between the obstetric care provider and the patient is crucial during labor and delivery. Effective communication can help the patient feel supported and informed throughout the delivery process. The obstetrician or midwife might use interpersonal communication skills to explain the different stages of labor, provide pain management options, and help the patient make informed decisions about the delivery [24,25,27].
- Postpartum care provider–patient communication: Communication between the obstetric care provider and the patient is still important after delivery. The care provider might use interpersonal communication skills to provide instructions on postpartum care, discuss breastfeeding or formula feeding options, and address any concerns or complications that arise [24,25,27].
- Obstetrician–midwife communication: Often, an obstetrician and a midwife work together to provide care to a patient during pregnancy, labor, and delivery. Effective communication between the two professionals ensures that the patient receives consistent and coordinated care. The obstetrician and midwife might use interpersonal communication skills to discuss the patient’s medical history, provide updates on the pregnancy´s progress, and collaborate on decisions regarding the delivery [24,26,27].
- Nurse–physician communication: Nurses and physicians often work together in obstetric care to provide comprehensive care to patients. Effective communication between nurses and physicians is important to ensure that the patient’s needs are met and that the care provided is safe and effective. For example, a nurse might communicate with a physician about a patient’s vital signs or symptoms, or a physician might collaborate with a nurse on the patient’s care plan [24,26,27].
2. Study 1 Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Data Analysis
3. Study 1 Results
3.1. Testing H1: Better Interpersonal Communication Is Associated with Fewer Patient Safety Threats (H1a) and Higher-Quality Care (H1b)
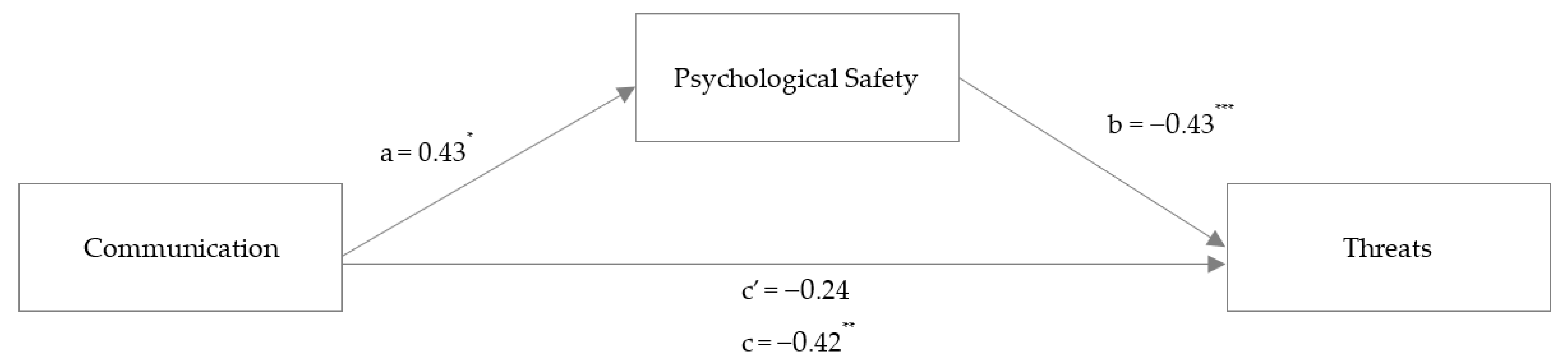
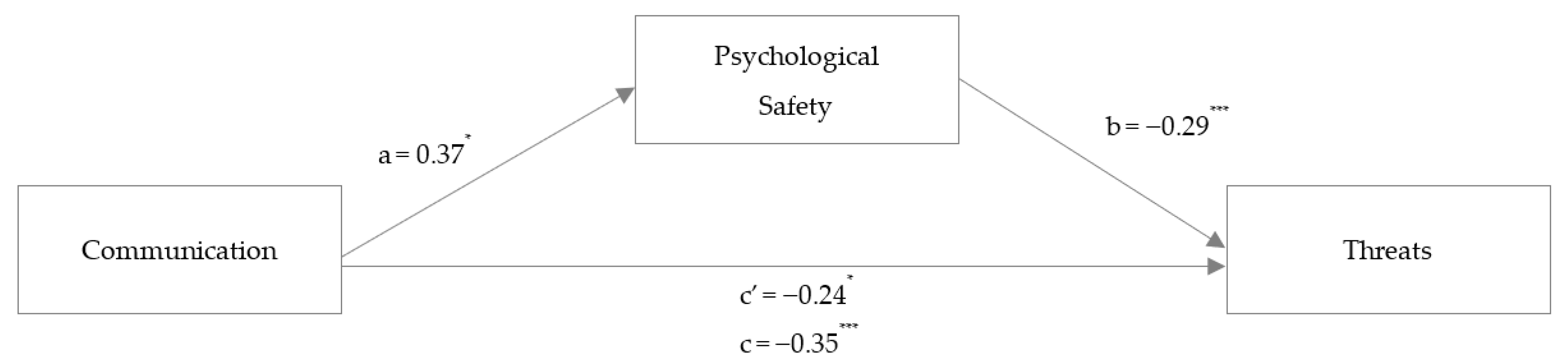
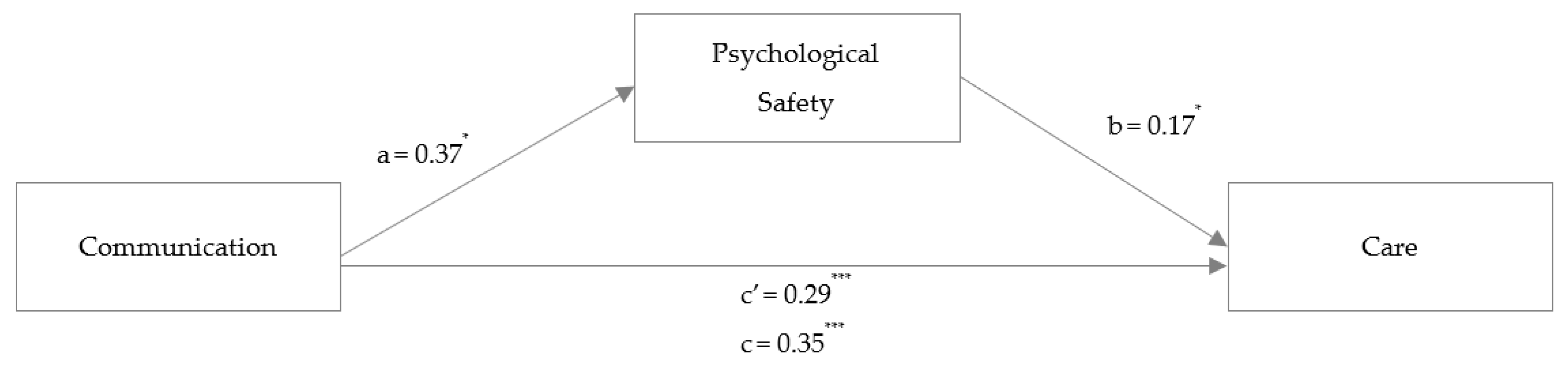
3.2. Testing H2: The Associations between Interpersonal Communication and Patient Safety Threats (H2a) as Well as Higher-Quality Care (H2b) Are Both Mediated by Psychological Safety
4. Study 2 Materials and Methods
4.1. Participants and Procedure
4.2. Measures
4.3. Data Analysis
5. Study 2 Results
5.1. Testing H1: Better Interpersonal Communication Is Associated with Fewer Patient Safety Threats (H1a) and Higher-Quality Care (H1b)
5.2. Testing H2: The Associations between Interpersonal Communication and Patient Safety Threats (H2a) as Well as Higher-Quality Care (H2b) Are Both Mediated by Psychological Safety
6. Discussion
6.1. Integration of Results
6.2. Limitations of the Current Research and Suggestions for Future Studies
6.3. Implications for Practice
- Interpersonal communication skills training to communicate effectively. Such training can include learning active listening techniques, closed-loop communication, and speaking up or training clear, concise, and sufficient information exchange: Improved interpersonal communication competencies can help individuals and teams develop the skills needed to communicate openly and honestly with each other to create a shared understanding. This can lead to increased trust and respect within the team, which in turn can help create a safe and supportive environment where team members feel comfortable sharing their thoughts, feelings, and concerns [29,30,78]
- Standardized communication protocols can help reduce the risk of errors and misunderstandings in healthcare: Examples include standardized communication tools such as the SBAR (situation, background, assessment, recommendation) technique or implementing checklists to ensure important information is communicated effectively and consistently [31]. This is especially important in the face of the findings of the current research demonstrating that psychological safety is a key mediator.
- Feedback and debriefing sessions: Regular feedback and debriefing sessions can help individuals and teams reflect on their communication and identify areas for improvement [28,32]. This can be done through individual feedback sessions, team debriefs, or anonymous surveys to gather feedback from patients and colleagues.
- Creating a culture of learning and improvement: Team exercises can help create a culture of learning and improvement, where mistakes are viewed as opportunities for growth rather than failures. When team members feel safe making mistakes and learning from them, they are more likely to take risks and contribute their ideas [10,33,43].
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gori, A.; Arcioni, A.; Topino, E.; Palazzeschi, L.; Di Fabio, A. Constructing well-being in organizations: First empirical results on job crafting, personality traits, and insight. Int. J. Environ. Res. Public Health 2021, 18, 6661. [Google Scholar] [CrossRef]
- Umberson, D.; Karas Montez, J. Social relationships and health: A flashpoint for health policy. J. Health Soc. Behav. 2010, 51 (Suppl. S1), S54–S66. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Yang, M.; Quade, M.J.; Chen, W. Is the bottom line reached? An exploration of supervisor bottom-line mentality, team performance avoidance goal orientation and team performance. Hum. Relat. 2022, 75, 349–372. [Google Scholar] [CrossRef]
- Knox, G.E.; Simpson, K.R. Perinatal high reliability. Am. J. Obstet. Gynecol. 2011, 204, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Neuhaus, C.; Lutnæs, D.E.; Bergström, J. Emergence of power and complexity in obstetric teamwork. PLoS ONE 2022, 17, e0269711. [Google Scholar] [CrossRef] [PubMed]
- Lyndon, A.; Zlatnik, M.G.; Wachter, R.M. Effective physician-nurse communication: A patient safety essential for labor and delivery. Am. J. Obstet. Gynecol. 2011, 205, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Malterud, K.; Aamland, A.; Fosse, A. How can task shifting put patient safety at risk? A qualitative study of experiences among general practitioners in Norway. Scand. J. Prim. Health Care 2020, 38, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Weller, J.; Boyd, M.; Cumin, D. Teams, tribes and patient safety: Overcoming barriers to effective teamwork in healthcare. Postgrad. Med. J. 2014, 90, 149–154. [Google Scholar] [CrossRef]
- Leonard, M.; Graham, S.; Bonacum, D. The human factor: The critical importance of effective teamwork and communication in providing safe care. BMJ Qual. Saf. 2004, 13, i85–i90. [Google Scholar] [CrossRef]
- Edmondson, A.C.; Lei, Z. Psychological safety: The history, renaissance, and future of an interpersonal construct. Annu. Rev. Organ. Psychol. Organ. Behav. 2014, 1, 23–43. [Google Scholar] [CrossRef]
- Jain, A.K.; Fennell, M.L.; Chagpar, A.B.; Connolly, H.K.; Nembhard, I.M. Moving toward improved teamwork in cancer care: The role of psychological safety in team communication. J. Oncol. Pract. 2016, 12, 1000–1011. [Google Scholar] [CrossRef]
- Yanchus, N.J.; Derickson, R.; Moore, S.C.; Bologna, D.; Osatuke, K. Communication and psychological safety in veterans health administration work environments. J. Health Organ. Manag. 2014, 28, 754–776. [Google Scholar] [CrossRef] [PubMed]
- Rhaiem, K.; Amara, N. Learning from innovation failures: A systematic review of the literature and research agenda. Rev. Manag. Sci. 2021, 15, 189–234. [Google Scholar] [CrossRef]
- Lysova, E.I.; Fletcher, L.; El Baroudi, S. What enables us to better experience our work as meaningful? The importance of awareness and the social context. Hum. Relat. 2022. [Google Scholar] [CrossRef]
- Echterhoff, G.; Higgins, E.T.; Levine, J.M. Shared Reality. Experiencing Commonality with others’ Inner States about the World. Perspect. Psychol. Sci. 2009, 4, 496–521. [Google Scholar] [CrossRef]
- Beukeboom, C.J.; Burgers, C. How Stereotypes Become Shared Knowledge: An Integrative Review on the Role of Biased Language Use in Communication about Categorized Individuals. Rev. Commun. Res. 2019, 7, 1–37. [Google Scholar] [CrossRef]
- Okuyama, A.; Wagner, C.; Bijnen, B. Speaking up for patient safety by hospital-based health care professionals: A literature review. BMC Health Serv. Res. 2014, 14, 61. [Google Scholar] [CrossRef] [PubMed]
- Petriglieri, G.; Petriglieri, J.L. The work is alive! Hum. Relat. 2022, 75, 1431–1460. [Google Scholar] [CrossRef]
- Van Swol, L.M.; Kane, A.A. Language and group processes: An integrative, interdisciplinary review. Small Group Res. 2019, 50, 3–38. [Google Scholar] [CrossRef]
- Holtgraves, T.M.; Kashima, Y. Language, meaning, and social cognition. Personal. Soc. Psychol. Rev. 2008, 12, 73–94. [Google Scholar] [CrossRef]
- Echterhoff, G. Achieving commonality in interpersonal communication: Shared reality and memory processes. Asian J. Soc. Psychol. 2014, 17, 104–107. [Google Scholar] [CrossRef]
- Hannawa, A.F. “SACCIA Safe Communication”: Five core competencies for safe and high-quality care. J. Patient Saf. Risk Manag. 2018, 23, 99–107. [Google Scholar] [CrossRef]
- Hüner, B.; Derksen, C.; Schmiedhofer, M.; Lippke, S.; Riedmüller, S.; Janni, W.; Reister, F.; Scholz, C. Reducing preventable adverse events in obstetrics by improving interprofessional communication skills–Results of an intervention study. BMC Pregnancy Childbirth 2023, 23, 55. [Google Scholar] [CrossRef]
- Schmiedhofer, M.; Derksen, C.; Dietl, J.E.; Häussler, F.; Louwen, F.; Hüner, B.; Reister, F.; Strametz, R.; Lippke, S. Birthing under the condition of the COVID-19 pandemic in Germany: Interviews with mothers, partners, and obstetric health care workers. Int. J. Environ. Res. Public Health 2022, 19, 1486. [Google Scholar] [CrossRef]
- Hüner, B.; Schmiedhofer, M.; Derksen, C.; Polasik, A.; Janni, W.; Reister, F.; Lippke, S. “Hilflosigkeit, das Abgeben jeglicher Selbstverantwortung und Selbstbestimmtheit”—Eine qualitative Auswertung von traumatisierenden Geburtserlebnissen in Relation zum Geburtsmodus/“Helplessness, giving up of any self-responsibility and self-determination”—A qualitative evaluation of traumatizing birth experiences in relation to birth mode. Z. Geburtshilfe Neonatol. 2023. [Google Scholar] [CrossRef]
- Schmiedhofer, M.; Derksen, C.; Keller, F.M.; Dietl, J.E.; Häussler, F.; Strametz, R.; Koester-Steinebach, I.; Lippke, S. Barriers and facilitators of safe communication in obstetrics: Results from qualitative interviews with physicians, midwives and nurses. Int. J. Environ. Res. Public Health 2021, 18, 915. [Google Scholar] [CrossRef] [PubMed]
- Schmiedhofer, M.; Derksen, C.; Dietl, J.E.; Haeussler, F.; Strametz, R.; Huener, B.; Lippke, S. The impact of a communication training on the birth experience: Qualitative interviews with mothers after giving birth at obstetric university departments in Germany. Int. J. Environ. Res. Public Health 2022, 19, 11481. [Google Scholar] [CrossRef]
- Kolbe, M.; Weiss, M.; Grote, G.; Knauth, A.; Dambach, M.; Spahn, D.R.; Grande, B. TeamGAINS: A tool for structured debriefings for simulation-based team trainings. BMJ Qual. Saf. 2013, 22, 541–553. [Google Scholar] [CrossRef] [PubMed]
- Kolbe, M.; Burtscher, M.J.; Wacker, J.; Grande, B.; Nohynkova, R.; Manser, T.; Spahn, D.R.; Grote, G. Speaking up is related to better team performance in simulated anesthesia inductions: An observational study. Anesth. Analg. 2012, 115, 1099–1108. [Google Scholar] [CrossRef] [PubMed]
- Raemer, D.B.; Kolbe, M.; Minehart, R.D.; Rudolph, J.W.; Pian-Smith, M. Improving anesthesiologists’ ability to speak up in the operating room: A randomized controlled experiment of a simulation-based intervention and a qualitative analysis of hurdles and enablers. Acad. Med. 2016, 91, 530–539. [Google Scholar] [CrossRef]
- Moi, E.B.; Söderhamn, U.; Marthinsen, G.N.; Flateland, S. The ISBAR tool leads to conscious, structured communication by healthcare personnel. Sykepl. Forsk. 2019, 14, 74699. [Google Scholar] [CrossRef]
- Rudolph, J.W.; Simon, R.; Raemer, D.B.; Eppich, W.J. Debriefing as formative assessment: Closing performance gaps in medical education. Acad. Emerg. Med. 2008, 15, 1010–1016. [Google Scholar] [CrossRef] [PubMed]
- Giudici, M.; Filimonau, V. Exploring the linkages between managerial leadership, communication and teamwork in successful event delivery. Tour. Manag. Perspect. 2019, 32, 100558. [Google Scholar] [CrossRef]
- Nembhard, I.M.; Edmondson, A.C. Making it safe: The effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J. Organ. Behav. 2006, 27, 941–966. [Google Scholar] [CrossRef]
- Catchpole, K. Spreading human factors expertise in healthcare: Untangling the knots in people and systems. BMJ Qual. Saf. 2013, 22, 793–797. [Google Scholar] [CrossRef] [PubMed]
- Edmondson, A.C. Psychological safety and learning behavior in work teams. Adm. Sci. Q. 1999, 44, 350–383. [Google Scholar] [CrossRef]
- Newman, A.; Donohue, R.; Eva, N. Psychological safety: A systematic review of the literature. Hum. Resour. Manag. Rev. 2017, 27, 521–535. [Google Scholar] [CrossRef]
- Edmondson, A.C. Speaking up in the operating room: How team leaders promote learning in interdisciplinary action teams. J. Manag. Stud. 2003, 40, 1419–1452. [Google Scholar] [CrossRef]
- Oc, B.; Bashshur, M.R. Followership, leadership and social influence. Leadersh. Q. 2013, 24, 919–934. [Google Scholar] [CrossRef]
- Meneghel, I.; Borgogni, L.; Miraglia, M.; Salanova, M.; Martinez, I.M. From social context and resilience to performance through job satisfaction: A multilevel study over time. Hum. Relat. 2016, 69, 2047–2067. [Google Scholar] [CrossRef]
- Aranzamendez, G.; James, D.; Toms, R. Finding antecedents of psychological safety: A step toward quality improvement. Nurs. Forum 2015, 50, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Frazier, M.L.; Fainshmidt, S.; Klinger, R.L.; Pezeshkan, A.; Vracheva, V. Psychological safety: A meta-analytic review and extension. Pers. Psychol. 2017, 70, 113–165. [Google Scholar] [CrossRef]
- Parker, A.L.; Forsythe, L.L.; Kohlmorgen, I.K. Teamstepps®: An evidence-based approach to reduce clinical errors threatening safety in outpatient settings: An integrative review. J. Healthc. Risk Manag. 2019, 38, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Hughes, A.M.; Gregory, M.E.; Joseph, D.L.; Sonesh, S.C.; Marlow, S.L.; Lacerenza, C.N.; Benishek, L.E.; King, H.B.; Salas, E. Saving lives: A meta-analysis of team training in healthcare. J. Appl. Psychol. 2016, 101, 1266. [Google Scholar] [CrossRef]
- Bateman, A.; Fonagy, P. Mentalization-based treatment. Psychoanal. Inq. 2013, 33, 595–613. [Google Scholar] [CrossRef] [PubMed]
- Di Stefano, G.; Piacentino, B.; Ruvolo, G. Mentalizing in organizations: A psychodynamic model for an understanding of well-being and suffering in the work contexts. World Futures 2017, 73, 216–223. [Google Scholar] [CrossRef]
- Edmondson, A.C. Learning from mistakes is easier said than done. J. Appl. Behav. Sci. 2004, 40, 66–90. [Google Scholar] [CrossRef]
- Akan, O.H.; Jack, E.P.; Mehta, A. Concrescent conversation environment, psychological safety, and team effectiveness: Examining a mediation model. Team Perform. Manag. Int. J. 2020, 26, 29–51. [Google Scholar] [CrossRef]
- Stead, G.B. Culture and career psychology: A social constructionist perspective. J. Vocat. Behav. 2004, 64, 389–406. [Google Scholar] [CrossRef]
- Bekkink, M.O.; Farrell, S.E.; Takayesu, J.K. Interprofessional communication in the emergency department: Residents’ perceptions and implications for medical education. Int. J. Med. Educ. 2018, 9, 262–270. [Google Scholar] [CrossRef]
- Gluyas, H. Effective communication and teamwork promotes patient safety. Nurs. Stand. 2015, 29, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Foronda, C.; MacWilliams, B.; McArthur, E. Interprofessional communication in healthcare: An integrative review. Nurse Educ. Pract. 2016, 19, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Carmeli, A.; Gittell, J.H. High-quality relationships, psychological safety, and learning from failures in work organizations. J. Organ. Behav. 2009, 30, 709–729. [Google Scholar] [CrossRef]
- Stewart, G.L.; Barrick, M.R. Team structure and performance: Assessing the mediating role of intrateam process and the moderating role of task type. Acad. Manag. J. 2000, 43, 135–148. [Google Scholar] [CrossRef]
- Decius, J.; Schaper, N.; Seifert, A. Work characteristics or workers’ characteristics? An input-process-output perspective on informal workplace learning of blue-collar workers. Vocat. Learn. 2021, 14, 285–326. [Google Scholar] [CrossRef]
- Calder, L.A.; Mastoras, G.; Rahimpour, M.; Sohmer, B.; Weitzman, B.; Cwinn, A.A.; Hobin, T.; Parush, A. Team communication patterns in emergency resuscitation: A mixed methods qualitative analysis. Int. J. Emerg. Med. 2017, 10, 24. [Google Scholar] [CrossRef]
- Lippke, S.; Wienert, J.; Keller, F.M.; Derksen, C.; Welp, A.; Kötting, L.; Hofreuter-Gätgens, K.; Müller, H.; Louwen, F.; Weigand, M.; et al. Communication and patient safety in gynecology and obstetrics—Study protocol of an intervention study. BMC Health Serv. Res. 2019, 19, 908. [Google Scholar] [CrossRef]
- Rider, E.A.; Keefer, C.H. Communication skills competencies. definitions and a teaching toolbox. Med. Educ. 2006, 40, 624–629. [Google Scholar] [CrossRef]
- Keller, F.M.; Derksen, C.; Kötting, L.; Schmiedhofer, M.; Lippke, S. Development of the perceptions of preventable adverse events assessment tool (PPAEAT): Measurement properties and patients’ mental health status. Int. J. Qual. Health Care 2021, 33, mzab063. [Google Scholar] [CrossRef]
- Klein, J.; Grosse Frie, K.; Blum, K.; von dem Knesebeck, O. Psychosocial stress at work and perceived quality of care among clinicians in surgery. BMC Health Serv. Res. 2011, 11, 109. [Google Scholar] [CrossRef]
- Winkler, H.; Prinz, A. Zertifizierung von Einrichtungen der Sucht-Rehabilitation—Erwartungen und Erfolge [Certification of addiction rehabilitation facilities—Expectations and successes]. SUCHT 2009, 55, 164–168. [Google Scholar] [CrossRef]
- Ibn El Haj, H.; Lamrini, M.; Rais, N. Quality of care between Donabedian model and ISO9001V2008. Int. J. Qual. Res. 2013, 7, 17–30. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2013. [Google Scholar]
- Petriglieri, G.; Stein, M. The Unwanted Self: Projective Identification in Leaders’ Identity Work. Organ. Stud. 2012, 33, 1217–1235. [Google Scholar] [CrossRef]
- Driver, M. Drawing on the discursive resources from psychological contracts to construct imaginary selves: A psychoanalytic perspective on how identity work drives psychological contracts. Hum. Relat. 2018, 71, 617–639. [Google Scholar] [CrossRef]
- Morrison, E.W. Employee voice and silence. Annu. Rev. Organ. Psychol. Organ. Behav. 2014, 1, 173–197. [Google Scholar] [CrossRef]
- Subhakaran, S.E.; Dyaram, L. Interpersonal antecedents to employee upward voice: Mediating role of psychological safety. Int. J. Product. Perform. Manag. 2018, 67, 1510–1525. [Google Scholar] [CrossRef]
- Cohen, L.; Sher-Censor, E.; Oppenheim, D.; Dassa, A.; Liat, A.; Yuval, P. Nursing aides’ mentalization, expressed emotion, and observed interaction with residents with demential: A quasi-experimental study. Geriatr. Nurs. 2022, 45, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Bordoagni, G.; Fino, E.; Agostini, A. Burnout, Attachment and Mentalization in Nursing Students and Nurse Professionals. Healthcare 2021, 9, 1576. [Google Scholar] [CrossRef]
- Lawler, E.J. An affect theory of social exchange. Am. J. Sociol. 2001, 107, 321–352. [Google Scholar] [CrossRef]
- Carmeli, A.; Brueller, D.; Dutton, J.E. Learning behaviours in the workplace: The role of high-quality interpersonal relationships and psychological safety. Syst. Res. 2009, 26, 81–98. [Google Scholar] [CrossRef]
- Patel, R.S.; Bachu, R.; Adikey, A.; Malik, M.; Shah, M. Factors related to physician burnout and its consequences: A review. Behav. Sci. 2018, 8, 98. [Google Scholar] [CrossRef]
- Khamisa, N.; Oldenburg, B.; Peltzer, K.; Ilic, D. Work related stress, burnout, job satisfaction and general health of nurses. Int. J. Environ. Res. Public Health 2015, 12, 652–666. [Google Scholar] [CrossRef]
- Lippke, S.; Derksen, C.; Keller, F.M.; Kötting, L.; Schmiedhofer, M.; Welp, A. Effectiveness of communication interventions in obstetrics—A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 2616. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, R.; Ward, M.; De Brún, A.; McAuliffe, E. Safety culture in health care teams: A narrative review of the literature. J. Nurs. Manag. 2019, 27, 871–883. [Google Scholar] [CrossRef] [PubMed]
- Halvorsrud, K.; Kucharska, J.; Adlington, K.; Rüdell, K.; Hajdukova, E.B.; Nazroo, J.; Haarmans, M.; Rhodes, J.; Bhui, K. Identifying evidence of effectiveness in the co-creation of research: A systematic review and meta-analysis of the international healthcare literature. J. Public Health 2021, 43, 197–208. [Google Scholar] [CrossRef] [PubMed]
- Grindell, C.; Coates, E.; Croot, L.; O’Cathain, A. The use of co-production, co-design and co-creation to mobilise knowledge in the management of health conditions: A systematic review. BMC Health Serv. Res. 2022, 22, 877. [Google Scholar] [CrossRef]
- Verdonik, D. Between understanding and misunderstanding. J. Pragmat. 2010, 42, 1364–1379. [Google Scholar] [CrossRef]
- Leroy, H.; Dierynck, B.; Anseel, F.; Simons, T.; Halbesleben, J.; McCaughey, D.; Savage, G.T.; Sels, L. Behavioral integrity for safety, priority of safety, psychological safety, and patient safety: A team-level study. J. Appl. Psychol. 2012, 97, 1273–1281. [Google Scholar] [CrossRef]

| N = 129 | Physicians (n = 18, 14%) | Midwives (n = 14, 11%) | Nurses (n = 58, 46%) | Other (Specified, e.g., Psychologist or Management, and Unspecified) (n = 24, 19%) | |
|---|---|---|---|---|---|
| Sex | Women (n = 91, 71%) | 9 (10%) | 12 (14%) | 42 (47%) | 19 (21%) |
| Men (n = 34, 26%) | 8 (24%) | 0 (0%) | 16 (47%) | 5 (15%) | |
| Divers (n = 1, 1%) | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Age | <26 years (n = 8, 6%) | 0 (0%) | 1 (13%) | 4 (50%) | 2 (25%) |
| 26–40 years (n = 46, 36%) | 7 (15%) | 4 (9%) | 26 (57%) | 6 (13%) | |
| 41–55 years (n = 46, 36%) | 8 (18%) | 5 (11%) | 17 (38%) | 10 (22%) | |
| >55 years (n = 26, 20%) | 3 (12%) | 2 (8%) | 10 (40%) | 6 (24%) | |
| Experience | <1 year (n = 2, 2%) | 0 (0%) | 1 (50%) | 0 (0%) | 1 (50%) |
| 1–5 years (n = 23, 18%) | 4 (17%) | 4 (17%) | 13 (57%) | 2 (9%) | |
| >5 years (n = 103, 80%) | 14 (14%) | 9 (9%) | 45 (45%) | 21 (21%) |
| Variable | M | SD | 1 | 2 | 3 | 4 | |
|---|---|---|---|---|---|---|---|
| 1. | Communication Behavior | 4.94 | 0.53 | ||||
| 2. | Psychological Safety | 4.12 | 1.06 | 0.21 * | |||
| 3. | Patient Safety Threats | 3.35 | 0.90 | −0.22 * | −0.45 ** | ||
| 4. | Quality of Care | 4.09 | 0.75 | 0.31 ** | 0.51 ** | −0.61 ** | |
| N = 138 | Physicians (n = 45, 33%) | Midwives (n = 45, 33%) | Nurses (n = 24, 18%) | Trainees (to Become Nurses or a Midwives) (n = 11, 8%) | Other (Specified, e.g., Psychologist or Management, and Unspecified) (n = 11, 8%) | |
|---|---|---|---|---|---|---|
| Sex | Women (n = 125, 92%) | 39(32%) | 44 (36%) | 22 (18%) | 10 (8%) | 9 (7%) |
| Men (n = 11, 8%) | 5 (46%) | 1 (9%) | 2 (18%) | 1 (9%) | 2 (18%) | |
| Age | <26 years (n = 29, 22%) | 1 (3%) | 13 (45%) | 3 (10%) | 10 (34%) | 2 (7%) |
| 26–40 years (n = 76, 58%) | 36 (47%) | 21 (28%) | 15 (20%) | 0 (0%) | 4 (5%) | |
| 41–55 years (n = 21, 16%) | 4 (20%) | 9 (45%) | 3 (15%) | 0 (0%) | 4 (20%) | |
| >55 years (n = 6, 5%) | 1 (17%) | 1 (17%) | 3 (50%) | 0 (0%) | 1 (17%) | |
| Experience | <1 year (n = 21, 16%) | 4 (19%) | 7 (33%) | 5 (24%) | 4 (19%) | 1 (5%) |
| 1–5 years (n = 57, 43%) | 20 (35%) | 21 (37%) | 6 (11%) | 6 (11%) | 4 (7%) | |
| >5 years (n = 54, 41%) | 19 (36%) | 16 (30%) | 12 (23%) | 0 (0%) | 6 (11%) |
| Variable | M | SD | 1 | 2 | 3 | 4 | |
|---|---|---|---|---|---|---|---|
| 1. | Communication | 4.55 | 0.65 | ||||
| 2. | Psychological Safety | 4.32 | 0.89 | 0.31 ** | |||
| 3. | Patient Safety Threats | 3.00 | 0.73 | −0.36 ** | −0.43 ** | ||
| 4. | Quality of Care | 4.31 | 0.62 | 0.39 ** | 0.35 ** | −0.45 ** | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dietl, J.E.; Derksen, C.; Keller, F.M.; Schmiedhofer, M.; Lippke, S. Psychosocial Processes in Healthcare Workers: How Individuals’ Perceptions of Interpersonal Communication Is Related to Patient Safety Threats and Higher-Quality Care. Int. J. Environ. Res. Public Health 2023, 20, 5698. https://doi.org/10.3390/ijerph20095698
Dietl JE, Derksen C, Keller FM, Schmiedhofer M, Lippke S. Psychosocial Processes in Healthcare Workers: How Individuals’ Perceptions of Interpersonal Communication Is Related to Patient Safety Threats and Higher-Quality Care. International Journal of Environmental Research and Public Health. 2023; 20(9):5698. https://doi.org/10.3390/ijerph20095698
Chicago/Turabian StyleDietl, Johanna Elisa, Christina Derksen, Franziska Maria Keller, Martina Schmiedhofer, and Sonia Lippke. 2023. "Psychosocial Processes in Healthcare Workers: How Individuals’ Perceptions of Interpersonal Communication Is Related to Patient Safety Threats and Higher-Quality Care" International Journal of Environmental Research and Public Health 20, no. 9: 5698. https://doi.org/10.3390/ijerph20095698
APA StyleDietl, J. E., Derksen, C., Keller, F. M., Schmiedhofer, M., & Lippke, S. (2023). Psychosocial Processes in Healthcare Workers: How Individuals’ Perceptions of Interpersonal Communication Is Related to Patient Safety Threats and Higher-Quality Care. International Journal of Environmental Research and Public Health, 20(9), 5698. https://doi.org/10.3390/ijerph20095698








