The Effectiveness of Online Mental Health First Aid Training in Community Rugby: A Mixed-Methods Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Survey Details
2.3. MHFA Training
2.4. Analysis
2.4.1. Statistical Analysis
2.4.2. Qualitative Analysis
3. Results
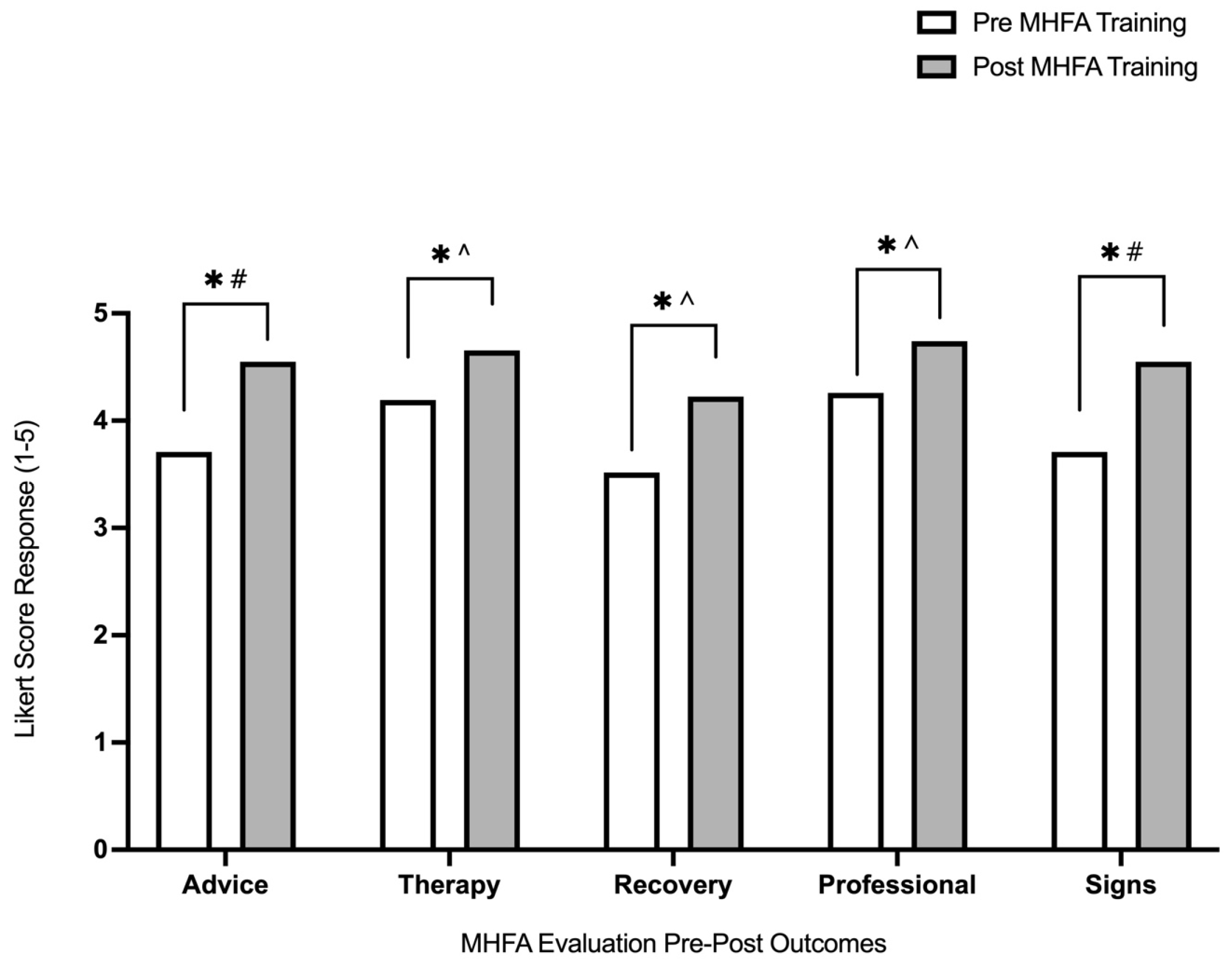
3.1. Pre- and Post-MHFA Training Responses
3.2. MHFA Outcome Evaluation
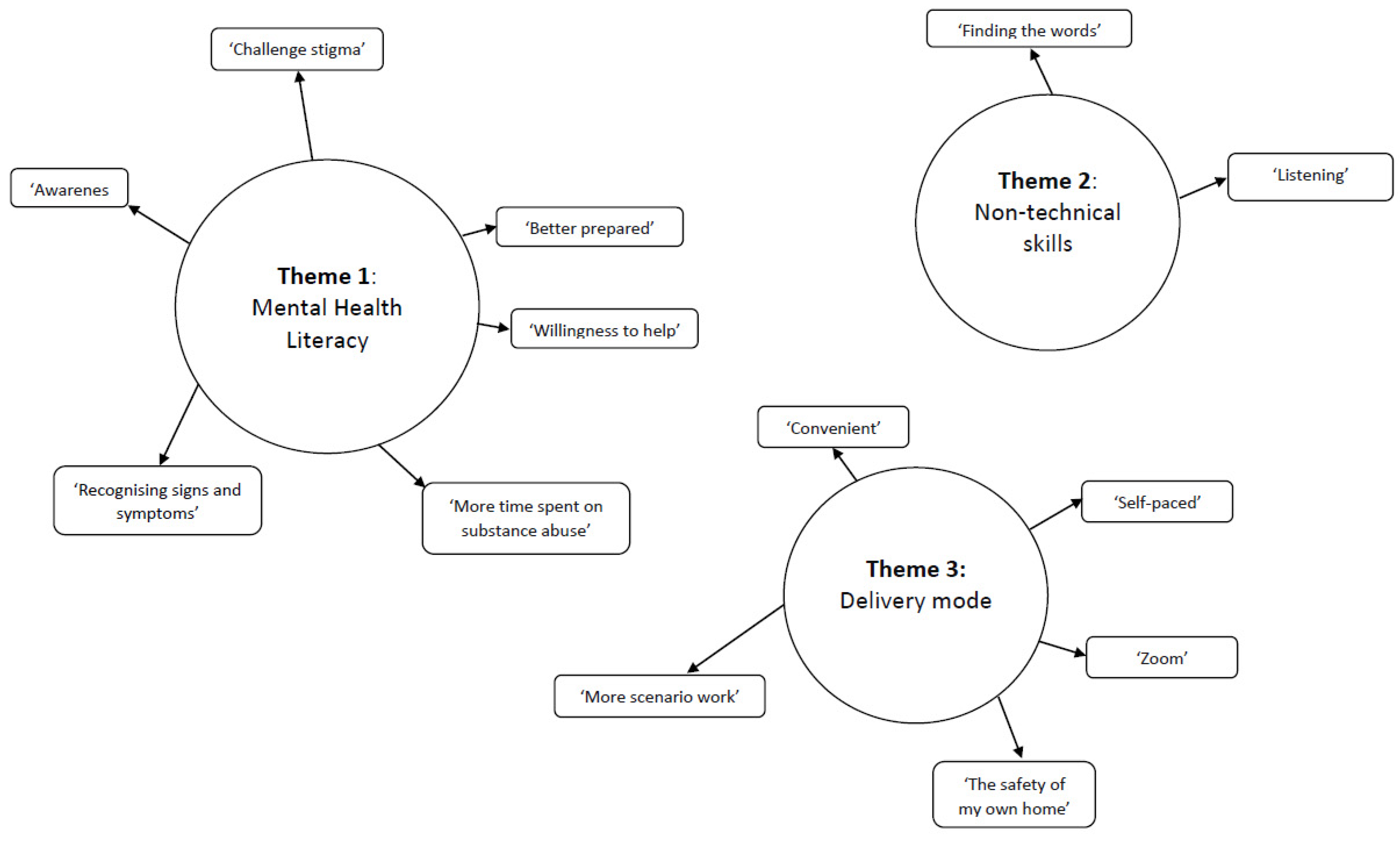
3.3. Mental Health Literacy
“I gained more. I thought it would be another ‘flick through’ online course but it was very interactive, and I now feel like I have the tools to open up these conversations.”
“recognising signs and symptoms and knowing what hope and resources I can give them.”
“I think it will be great for the rugby community to be able to identify when someone might [be] struggling but also goes a long way to challenging the stigma around mental health.”
“……it allows people to reflect on how we can implement MHFA as a coach, …… and break down some of the barriers and views that are held.”
“Awareness—that in itself can help exponentially. Sharing information with parents in the club.”
“For the context of rugby in high performance maybe substance abuse and also the fact that the supplement industry isn’t regulated and may have banned substances.”
“More time spent on substance abuse.”
3.4. Non-Technical Skills
“gaining a better understanding of the framework for understanding and listening to people.”
“listen—ask open questions, leave space.”
“better prepared to have the conversation.”
“to be brave enough to say something.”
“More people being equipped with the knowledge and a willingness to help.”
“…to not be afraid to approach any given situation and not be frightened by the idea of mental health issues.”
“young males are an at risk group and I feel more confident to assist them if needed.”
“I think this will help in my club, which is predominantly teenage girls in minority groups, in identifying girls who are struggling and help intervene early and help them get professional help.”
3.5. Delivery Mode
“I would have liked more time working through scenarios putting the work into practice.”
“really good via zoom (and our only option at present).”
“I was surprised how effective the zoom meetings could be with the breakout rooms etc.”
“it was convenient and practical to go through mental health issues in the safety of your own home was comforting.”; “very good to be able to learn something whilst still in your home environment.”
“I liked this as I could do the e-learning at my own pace and the face to face was broken up over a few days so wasn’t a huge info dump.”
4. Discussion
Proposed Integration of MHFA into Sporting Communities
- Establishment of a culture that endorses mental health and wellbeing for everyone within the sporting organisation community.
- Facilitation of an environment that positions periodisation of mental health as an integral part of achievement of sporting excellence.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Australian Bureau of Statistics (ABS). National Study of Mental Health and Wellbeing. Available online: https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/latest-release (accessed on 11 November 2022).
- Australian Institute of Health and Welfare (AIHW). Mental Health: Prevalence and Impact. Available online: https://www.aihw.gov.au/reports/mental-health-services/mental-health (accessed on 11 November 2022).
- Purcell, R.; Henderson, J.; Tamminen, K.A.; Frost, J.; Gwyther, K.; Kerr, G.; Kim, J.; Pilkington, V.; Rice, S.M.; Walton, C.C. Starting young to protect elite athletes’ mental health. Br. J. Sport. Med. 2023, 57, 439–440. [Google Scholar] [CrossRef] [PubMed]
- Mazzer, K.R.; Rickwood, D.J. Mental health in sport: Coaches’ views of their role and efficacy in supporting young people’s mental health. Int. J. Health Promot. Educ. 2015, 53, 102–114. [Google Scholar] [CrossRef]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Barriers and facilitators to mental health help-seeking for young elite athletes: A qualitative study. BMC Psychiatry 2012, 12, 157. [Google Scholar] [CrossRef] [PubMed]
- Hurley, D.; Swann, C.; Allen, M.S.; Okely, A.D.; Vella, S.A. The role of community sports clubs in adolescent mental health: The perspectives of adolescent males’ parents. Qual. Res. Sport Exerc. Health 2017, 9, 372–388. [Google Scholar] [CrossRef]
- Breslin, G.; Haughey, T.J.; Donnelly, P.; Kearney, C.; Prentice, G. Promoting mental health awareness in sport clubs. J. Public Ment. Health 2017, 16, 55–62. [Google Scholar] [CrossRef]
- Liddle, S.K.; Deane, F.P.; Vella, S.A. Addressing mental health through sport: A review of sporting organizations’ websites. Early Interv. Psychiatry 2016, 11, 93–103. [Google Scholar] [CrossRef]
- Rickwood, D.J.; Deane, F.P.; Wilson, C.J. When and how do young people seek professional help for mental health problems? Med. J. Aust. 2007, 187, S35–S39. [Google Scholar] [CrossRef]
- Gorczynski, P.; Gibson, K.; Clarke, N.; Mensah, T.; Summers, R. Examining mental health literacy, help-seeking behaviours, distress, and wellbeing in UK coaches. Eur. Phys. Educ. Rev. 2020, 26, 713–726. [Google Scholar] [CrossRef]
- Morgan, A.J.; Ross, A.; Reavley, N.J. Systematic review and meta-analysis of Mental Health First Aid training: Effects on knowledge, stigma, and helping behaviour. PLoS ONE 2018, 13, e0197102. [Google Scholar] [CrossRef]
- Bird, M.; Simons, E.E.; Jackman, P.C. Mental Toughness, Sport-Related Well-Being, and Mental Health Stigma Among National Collegiate Athletic Association Division I Student-Athletes. J. Clin. Sport Psychol. 2021, 15, 306–322. [Google Scholar] [CrossRef]
- Hadlaczky, G.; Hökby, S.; Mkrtchian, A.; Carli, V.; Wasserman, D. Mental Health First Aid is an effective public health intervention for improving knowledge, attitudes, and behaviour: A meta-analysis. J. Int. Rev. Psychiatry 2014, 26, 467–475. [Google Scholar] [CrossRef]
- Pierce, D.; Liaw, S.-T.; Dobell, J.; Anderson, R. Australian rural football club leaders as mental health advocates: An investigation of the impact of the Coach the Coach project. Int. J. Ment. Health Syst. 2010, 4, 10. [Google Scholar] [CrossRef]
- Jorm, A.F.; Kitchener, B.A.; O’Kearney, R.; Dear, K.B. Mental health first aid training of the public in a rural area: A cluster randomized trial. BMC Psychiatry 2004, 4, 33. [Google Scholar] [CrossRef]
- Kitchener, B.A.; Jorm, A.F. Mental health first aid training for the public: Evaluation of effects on knowledge, attitudes and helping behavior. BMC Psychiatry 2002, 2, 10. [Google Scholar] [CrossRef]
- Jorm, A.F.; Kitchener, B.A.; Sawyer, M.G.; Scales, H.; Cvetkovski, S. Mental health first aid training for high school teachers: A cluster randomized trial. BMC Psychiatry 2010, 10, 51. [Google Scholar] [CrossRef]
- Carpini, J.A.; Chandra, J.; Lin, J.; Teo, R.; Truong, N.; Boyne, E.; Wylde, T.; Clifford, R.; Ashoorian, D. Mental health first aid by Australian tertiary staff: Application rates, modes, content, and outcomes. Early Interv. Psychiatry 2021, 15, 1234–1242. [Google Scholar] [CrossRef]
- Reavley, N.J.; Morgan, A.J.; Fischer, J.-A.; Kitchener, B.; Bovopoulos, N.; Jorm, A.F. Effectiveness of eLearning and blended modes of delivery of Mental Health First Aid training in the workplace: Randomised controlled trial. BMC Psychiatry 2018, 18, 312. [Google Scholar] [CrossRef]
- Sparkes, A.C.; Smith, B. Qualitative Research Methods in Sport, Exercise and Health: From Process to Product; Routledge: Abingdon, UK, 2013. [Google Scholar]
- Harper, L.D.; McCunn, R. “Hand in Glove”: Using Qualitative Methods to Connect Research and Practice. Int. J. Sport. Physiol. Perform. 2017, 12, 990–993. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Hossain, D.; Gorman, D.; Eley, R. Enhancing the knowledge and skills of Advisory and Extension Agents in mental health issues of farmers. Australas. Psychiatry 2009, 17, S116–S120. [Google Scholar] [CrossRef]
- Billingham, S.A.; Whitehead, A.L.; Julious, S.A. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Med. Res. Methodol. 2013, 13, 104. [Google Scholar] [CrossRef] [PubMed]
- Evans-Lacko, S.; Little, K.; Meltzer, H.; Rose, D.; Rhydderch, D.; Henderson, C.; Thornicroft, G. Development and psychometric properties of the mental health knowledge schedule. Can. J. Psychiatry 2010, 55, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Kitchener, B.A.; Jorm, A.F. Mental Health First Aid Training: Review of Evaluation Studies. Aust. N. Z. J. Psychiatry 2006, 40, 6–8. [Google Scholar] [CrossRef] [PubMed]
- Australia, M.H.F.A. Standard Mental Health First Aid. Available online: https://mhfa.com.au/courses/public/types/standardedition4 (accessed on 25 March 2022).
- Cumming, G.; Finch, S. A primer on the understanding, use, and calculation of confidence intervals that are based on central and noncentral distributions. Educ. Psychol. Meas. 2001, 61, 532–574. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: Abingdon, UK, 2013. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Arango, C.; Díaz-Caneja, C.M.; McGorry, P.D. Preventive strategies for mental health. Lancet Psychiatry 2018, 5, 591–604. [Google Scholar] [CrossRef]
- Chow, G.M.; Bird, M.D.; Gabana, N.T.; Cooper, B.T.; Becker, M.A.S. A Program to Reduce Stigma toward Mental Illness and Promote Mental Health Literacy and Help-Seeking in National Collegiate Athletic Association Division I Student-Athletes. J. Clin. Sport Psychol. 2021, 15, 185–205. [Google Scholar] [CrossRef]
- Reardon, C.L.; Hainline, B.; Aron, C.M.; Baron, D.; Baum, A.L.; Bindra, A.; Budgett, R.; Campriani, N.; Castaldelli-Maia, J.M.; Currie, A.; et al. Mental health in elite athletes: International Olympic Committee consensus statement. Br. J. Sport. Med. 2019, 53, 667–699. [Google Scholar] [CrossRef]
- Jorm, A.F.; Kitchener, B.A.; Reavley, N. Mental Health First Aid training: Lessons learned from the global spread of a community education program. World Psychiatry 2019, 18, 142–143. [Google Scholar] [CrossRef]
- Kelly, C.M.; Jorm, A.F.; Wright, A. Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Med. J. Aust. 2007, 187, S26–S30. [Google Scholar] [CrossRef]
- Maslowski, A.K.; LaCaille, R.A.; LaCaille, L.J.; Reich, C.M.; Klingner, J. Effectiveness of mental health first aid: A meta-analysis. Ment. Health Rev. J. 2019, 24, 245–261. [Google Scholar] [CrossRef]
| Domain | Mean ± SD Likert Score * |
|---|---|
| Knowledge to refer others to seek support | 4.77 ± 0.43 |
| Knowledge of signs and symptoms | 4.71 ± 0.46 |
| Knowledge about provision of initial help for those struggling with mental health problems | 4.71 ± 0.46 |
| Useful information about depression and anxiety | 4.68 ± 0.48 |
| Knowledge about effectiveness of treatment for mental health problems | 4.61 ± 0.50 |
| Knowledge for provision of MHFA support in a crisis situation | 4.61 ± 0.50 |
| Useful information about substance use | 4.58 ± 0.50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Russell, S.; Kelly, V.; Polman, R.; Warren-James, M. The Effectiveness of Online Mental Health First Aid Training in Community Rugby: A Mixed-Methods Approach. Int. J. Environ. Res. Public Health 2023, 20, 5391. https://doi.org/10.3390/ijerph20075391
Russell S, Kelly V, Polman R, Warren-James M. The Effectiveness of Online Mental Health First Aid Training in Community Rugby: A Mixed-Methods Approach. International Journal of Environmental Research and Public Health. 2023; 20(7):5391. https://doi.org/10.3390/ijerph20075391
Chicago/Turabian StyleRussell, Suzanna, Vincent Kelly, Remco Polman, and Matthew Warren-James. 2023. "The Effectiveness of Online Mental Health First Aid Training in Community Rugby: A Mixed-Methods Approach" International Journal of Environmental Research and Public Health 20, no. 7: 5391. https://doi.org/10.3390/ijerph20075391
APA StyleRussell, S., Kelly, V., Polman, R., & Warren-James, M. (2023). The Effectiveness of Online Mental Health First Aid Training in Community Rugby: A Mixed-Methods Approach. International Journal of Environmental Research and Public Health, 20(7), 5391. https://doi.org/10.3390/ijerph20075391






