Food Insecurity among International Migrants during the COVID-19 Pandemic: A Scoping Review
Abstract
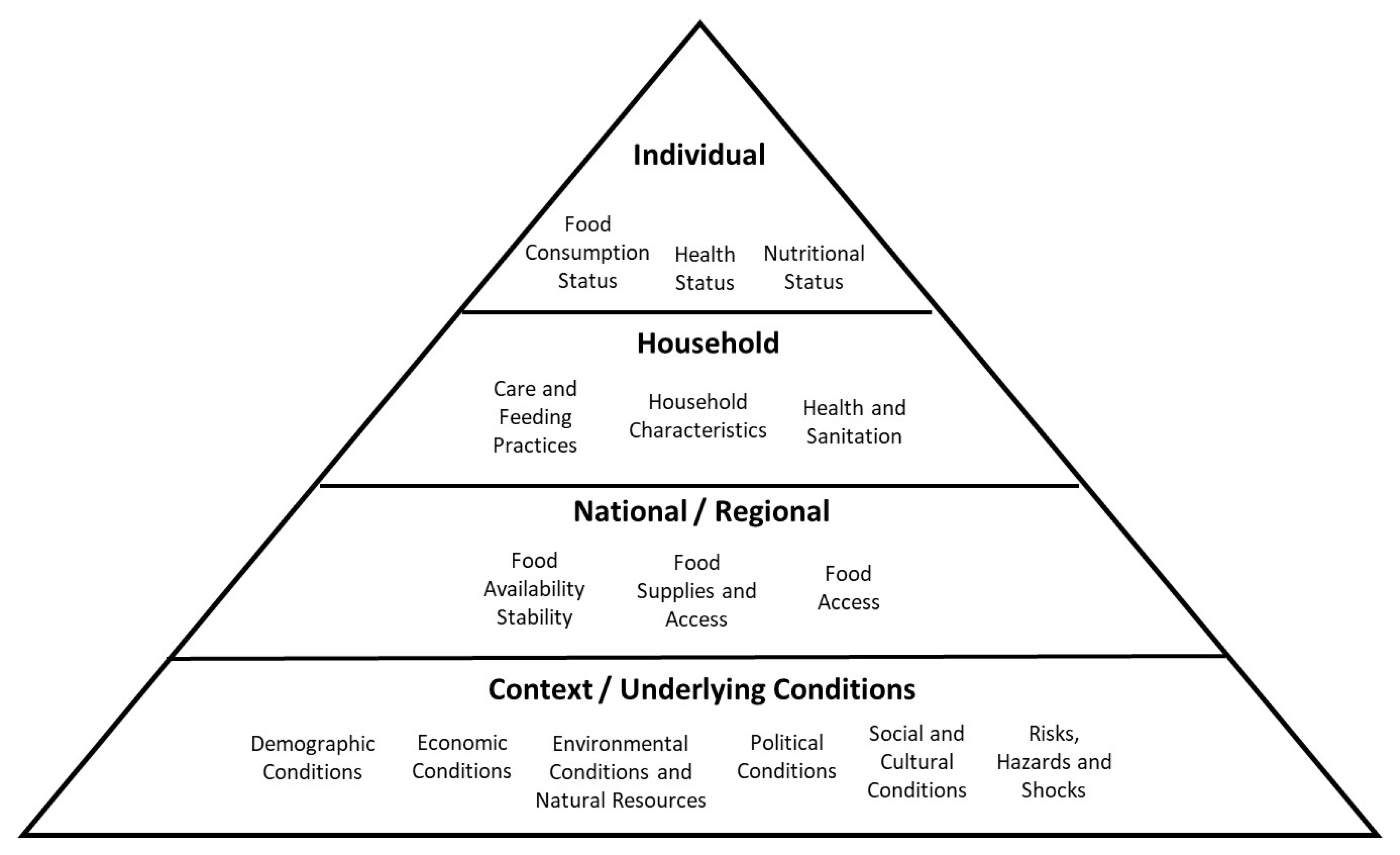
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Data Extraction
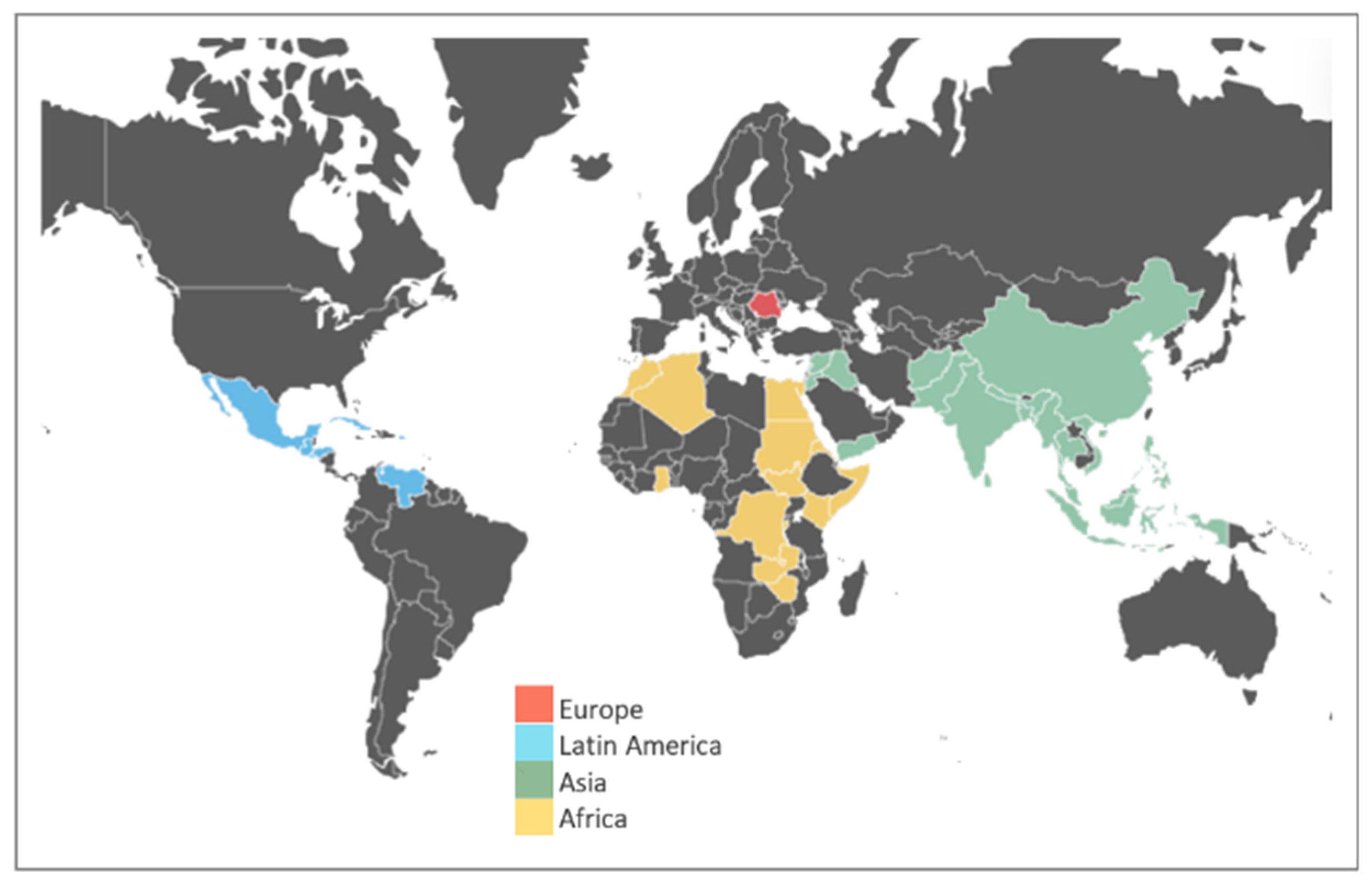
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 15 December 2022).
- Simon, J.; Helter, T.M.; White, R.G.; van der Boor, C.; Łaszewska, A. Impacts of the COVID-19 lockdown and relevant vulnerabilities on capability well-being, mental health and social support: An Austrian survey study. BMC Public Health 2021, 21, 314. [Google Scholar] [CrossRef] [PubMed]
- Oliva-Arocas, A.; Benavente, P.; Ronda, E.; Diaz, E. Health of International Migrant Workers During the COVID-19 Pandemic: A Scoping Review. Front. Public Health 2022, 10, 816597. [Google Scholar] [CrossRef] [PubMed]
- Egger, D.; Miguel, E.; Warren, S.S.; Shenoy, A.; Collins, E.; Karlan, D.; Parkerson, D.; Mobarak, A.M.; Fink, G.; Udry, C.; et al. Falling living standards during the COVID-19 crisis: Quantitative evidence from nine developing countries. Sci. Adv. 2021, 7, eabe0997. [Google Scholar] [CrossRef] [PubMed]
- OECD. Social Economy and the COVID-19 Crisis: Current and Future Roles. Available online: https://read.oecd-ilibrary.org/view/?ref=135_135367-031kjiq7v4&title=Social-economy-and-the-COVID-19-crisis-current-and-future-roles (accessed on 17 December 2022).
- Barron, G.C.; Laryea-Adjei, G.; Vike-Freiberga, V.; Abubakar, I.; Dakkak, H.; Devakumar, D.; Johnsson, A.; Karabey, S.; Labonté, R.; Legido-Quigley, H.; et al. Safeguarding people living in vulnerable conditions in the COVID-19 era through universal health coverage and social protection. Lancet Public Health 2022, 7, e86–e92. [Google Scholar] [CrossRef]
- FHI. COVID-19 Blant Innvandrere i Norge, Vurdering av Tiltak og Erfaringer Fra Felt, Delrapport 1; Folkehelseinstituttet: Oslo, Norway, 2021. [Google Scholar]
- WHO. Apart Together Survey; WHO: Rome, Italy, 2020. [Google Scholar]
- Rosario, O.M.M.; Shaaban, A.N.; Abecasis, A.; Muggli, Z.; Amado, R.; Vaz, D.; Dias, S.S.; Silva, A.C.; Fronteira, I. Are immigrants more vulnerable to the socioeconomic impact of COVID-19? A cross-sectional study in Amadora Municipality, Lisbon metropolitan area. Front. Public Health 2022, 10, 920308. [Google Scholar] [CrossRef]
- Mena, G.E.; Martinez, P.P.; Mahmud, A.S.; Marquet, P.A.; Buckee, C.O.; Santillana, M. Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile. Science 2021, 372, eabg5298. [Google Scholar] [CrossRef]
- FAO. An Introduction to the Basic Concepts of Food Security. Available online: https://www.fao.org/3/al936e/al936e00.pdf (accessed on 20 October 2021).
- Pérez-Escamilla, R. Food Security and the 2015–2030 Sustainable Development Goals: From Human to Planetary Health: Perspectives and Opinions. Curr. Dev. Nutr. 2017, 1, e000513. [Google Scholar] [CrossRef]
- Laraia, B.A. Food insecurity and chronic disease. Adv. Nutr. 2013, 4, 203–212. [Google Scholar] [CrossRef]
- Chilton, M.; Black, M.M.; Berkowitz, C.; Casey, P.H.; Cook, J.; Cutts, D.; Jacobs, R.R.; Heeren, T.; de Cuba, S.E.; Coleman, S.; et al. Food insecurity and risk of poor health among US-born children of immigrants. Am. J. Public Health 2009, 99, 556–562. [Google Scholar] [CrossRef]
- Frongillo, E.A.; Nguyen, H.T.; Smith, M.D.; Coleman-Jensen, A. Food Insecurity Is Associated with Subjective Well-Being among Individuals from 138 Countries in the 2014 Gallup World Poll. J. Nutr. 2017, 147, 680–687. [Google Scholar] [CrossRef]
- Maharaj, V.; Tomita, A.; Thela, L.; Mhlongo, M.; Burns, J.K. Food Insecurity and Risk of Depression Among Refugees and Immigrants in South Africa. J. Immigr. Minor Health 2017, 19, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Gibson, M. Food Security-A Commentary: What Is It and Why Is It So Complicated? Foods 2012, 1, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada. Household Food Insecurity in Canada. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/household-food-insecurity-canada-overview.html (accessed on 4 November 2022).
- Henjum, S.; Morseth, M.S.; Arnold, C.D.; Mauno, D.; Terragni, L. “I worry if I will have food tomorrow”: A study on food insecurity among asylum seekers living in Norway. BMC Public Health 2019, 19, 592. [Google Scholar] [CrossRef]
- Idzerda, L.; Gariépy, G.; Corrin, T.; Tarasuk, V.; McIntyre, L.; Neil-Sztramko, S.; Dobbins, M.; Snelling, S.; Jaramillo Garcia, A. What is known about the prevalence of household food insecurity in Canada during the COVID-19 pandemic: A systematic review. Health Promot. Chronic. Dis. Prev. Can. 2022, 42, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Pryor, S.; Dietz, W. The COVID-19, Obesity, and Food Insecurity Syndemic. Curr. Obes. Rep. 2022, 11, 70–79. [Google Scholar] [CrossRef]
- FAO. The State of Food Security and Nutrition in the World. Available online: https://www.fao.org/publications/sofi/2022/en/ (accessed on 20 November 2022).
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Attal, J.H.; Lurie, I.; Neumark, Y. A rapid assessment of migrant careworkers’ psychosocial status during Israel’s COVID-19 lockdown. Isr. J. Health Policy Res. 2020, 9, 61. [Google Scholar] [CrossRef]
- Ayande, R.E.A.; Chilufya, J. Two african immigrant graduate students reflect on food access, food (in)security, and community during the pandemic. Food Foodways 2021, 29, 391–402. [Google Scholar] [CrossRef]
- Burton-Jeangros, C.; Duvoisin, A.; Lachat, S.; Consoli, L.; Fakhoury, J.; Jackson, Y. The Impact of the COVID-19 Pandemic and the Lockdown on the Health and Living Conditions of Undocumented Migrants and Migrants Undergoing Legal Status Regularization. Front. Public Health 2020, 8, 596887. [Google Scholar] [CrossRef]
- Duh-Leong, C.; Yin, H.S.; Yi, S.S.; Chen, S.L.; Mui, A.; Perrin, E.M.; Zhao, Q.; Gross, R.S. Material Hardship and Stress from COVID-19 in Immigrant Chinese American Families with Infants. J. Immigr. Minor. Health 2022, 24, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Dutta, M.J. COVID-19, Authoritarian Neoliberalism, and Precarious Migrant Work in Singapore: Structural Violence and Communicative Inequality. Front. Commun. 2020, 5, 58. [Google Scholar] [CrossRef]
- Eshareturi, C.; Wareham, A.; Rattray, M.; Haith-Cooper, M.; McCarthy, R. An exploration of the impact of SARS-CoV-2 (COVID-19) restrictions on marginalised groups in the UK. Public Health 2021, 197, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Guglielmi, S.; Seager, J.; Mitu, K.; Baird, S.; Jones, N. Exploring the impacts of COVID-19 on Rohingya adolescents in Cox’s Bazar: A mixed-methods study. J. Migr. Health 2020, 1–2, 100031. [Google Scholar] [CrossRef] [PubMed]
- Khayyam, M.; Shuai, C.M.; Qasim, H.; Ihtisham, M.; Anjum, R.; Li, J.X.; Tikhomirova, A.; Khan, N. Food Consumption Behavior of Pakistani Students Living in China: The Role of Food Safety and Health Consciousness in the Wake of Coronavirus Disease 2019 Pandemic. Front. Psychol. 2021, 12, 673771. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, D.; Obure, R.; Billingsley, K.; Inks, M.; Umurutasate, E.; Baer, R.D. Evaluating understandings of state and federal pandemic policies: The situation of refugees from the Congo wars in Tampa, Florida. Hum. Organ. 2020, 79, 271–280. [Google Scholar] [CrossRef]
- Mistry, S.K.; Ali, A.R.M.M.; Akther, F.; Peprah, P.; Reza, S.; Prova, S.; Yadav, U.N. Are older adults of Rohingya community (Forcibly Displaced Myanmar Nationals or FDMNs) in Bangladesh fearful of COVID-19? Findings from a cross-sectional study. PLoS ONE 2021, 16, e0253648. [Google Scholar] [CrossRef]
- Partika, A.; Johnson, A.D.; Martin, A.; Castle, S.; Tulsa, S.S.T. Hispanic English language learner families and food insecurity during COVID-19: Risk factors and systems of food support. Fam. Syst. Health 2021, 16, 16. [Google Scholar] [CrossRef]
- Andersen, J.A.; Willis, D.E.; Malhis, J.R.; Long, C.R.; McElfish, P.A. The Association Between Education and Basic Needs Insecurity for Marshallese During the COVID-19 Pandemic. J. Racial Ethn. Health Disparities 2022, 9, 1882–1887. [Google Scholar] [CrossRef]
- Baird, S.; Murphy, M.; Seager, J.; Jones, N.; Malhotra, A.; Alheiwidi, S.; Emirie, G.; Rashid, S.; Sultan, M. Intersecting disadvantages for married adolescents: Life after marriage pre- and post-COVID-19 in contexts of displacement. J. Adolesc. Health 2022, 70, S86–S96. [Google Scholar] [CrossRef]
- Blay Benzaken, Y.; Zohar, S.; Yuval, K.; Aizik-Reebs, A.; Gebremariam, S.G.; Bernstein, A. COVID-19 and Mental Health Among People Who Are Forcibly Displaced: The Role of Socioeconomic Insecurity. Psychiatr. Serv. 2022, 74, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Bovell-Ammon, A.; de Cuba, S.E.; Le-Scherban, F.; Rateau, L.; Heeren, T.; Cantave, C.; Green, K.A.; Frank, D.A.; Cutts, D.; Ochoa, E.; et al. Changes in Economic Hardships Arising during the COVID-19 Pandemic: Differences by Nativity and Race. J. Immigr. Minor. Health 2023, 25, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Cadenas, G.A.; Cerezo, A.; Carlos Chavez, F.L.; Capielo Rosario, C.; Torres, L.; Suro, B.; Fuentes, M.; Sanchez, D. The citizenship shield: Mediated and moderated links between immigration status, discrimination, food insecurity, and negative health outcomes for latinx immigrants during the COVID-19 pandemic. J. Community Psychol. 2022, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Cyrenne-Dussault, M.; Sirois, M.; St-Pierre, J.; Drouin-Chartier, J.P. Food insecurity in households of children receiving care at a paediatric obesity management clinic in Montreal: Overall prevalence and changes associated with the COVID-19 pandemic. Paediatr. Child Health 2022, 27, 396–402. [Google Scholar] [CrossRef]
- Davlantes, E.; Tippins, A.; Espinosa, C.; Lofgren, H.; Leonard, S.; Solis, M.; Young, A.; Sockwell, D.; Ansher, A. Mitigating SARS-CoV-2 Transmission in Hispanic and Latino Communities-Prince William Health District, Virginia, June 2020. J. Racial Ethn. Health Disparities 2022, 9, 390–398. [Google Scholar] [CrossRef]
- Duerto, C.M.B. In Limbo: Survey of Impact of COVID-19 on Venezuelan Migrants in Trinidad and Tobago. J. Refug. Stud. 2021, 34, 4445–4455. [Google Scholar] [CrossRef]
- Hallgren, E.; Moore, R.; Riklon, S.; Alik, E.; McElfish, P.A. Pandemic-Amplified Material Hardship and Community-Led Support among Marshallese Diasporic Communities in the United States. J. Poverty 2022, 1–16. [Google Scholar] [CrossRef]
- Haro-Ramos, A.Y.; Bacong, A.M. Prevalence and risk factors of food insecurity among Californians during the COVID-19 pandemic: Disparities by immigration status and ethnicity. Prev. Med. 2022, 164, 107268. [Google Scholar] [CrossRef]
- Hossain, M.A.; Ullah, A.; Mohiuddin, M. Rohingya refugees in the pandemic: Crisis and policy responses. Glob. Policy 2023, 14, 183–191. [Google Scholar] [CrossRef]
- Kent, K.; Murray, S.; Penrose, B.; Auckland, S.; Horton, E.; Lester, E.; Visentin, D. The new normal for food insecurity? A repeated cross-sectional survey over 1 year during the COVID-19 pandemic in Australia. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 115. [Google Scholar] [CrossRef]
- Loganathan, T.; Chan, Z.E.X.; Hassan, F.; Kunpeuk, W.; Suphanchaimat, R.; Yi, H.S.; Majid, H.A. Education for non-citizen children in Malaysia during the COVID-19 pandemic: A qualitative study. PLoS ONE 2021, 16, e0259546. [Google Scholar] [CrossRef] [PubMed]
- Logie, C.H.; Berry, I.; Okumu, M.; Loutet, M.; McNamee, C.; Hakiza, R.; Musoke, D.K.; Mwima, S.; Kyambadde, P.; Mbuagbaw, L. The prevalence and correlates of depression before and after the COVID-19 pandemic declaration among urban refugee adolescents and youth in informal settlements in Kampala, Uganda: A longitudinal cohort study. Ann. Epidemiol. 2022, 66, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Martin, K.J.; Castano, C.; Geraghty, S.; Horner, S.R.; McCann, E.; Beck, A.F.; Xu, Y.Y.; Gomez, L.; O’Dea, C.; Jacquez, F.; et al. Barriers and Facilitators to Prevention and Care of COVID-19 Infection in Cincinnati Latinx Families: A Community-Based Convergent Mixed Methods Study. J. Racial Ethn. Health Disparities 2022, 1–19. [Google Scholar] [CrossRef] [PubMed]
- McDougal, L.; Erikat, J.; Yusufi, H.; Sahid, R.; Streuli, S.; Fielding-Miller, R. Understanding the impact of the COVID-19 pandemic on refugee communities in San Diego, California: A participatory action research cross-sectional study. SSM Popul. Health 2022, 18, 101110. [Google Scholar] [CrossRef]
- Mihrshahi, S.; Dharmayani, P.N.A.; Amin, J.; Bhatti, A.; Chau, J.Y.; Ronto, R.; Turnip, D.; Taylor, M. Higher Prevalence of Food Insecurity and Psychological Distress among International University Students during the COVID-19 Pandemic: An Australian Perspective. Int. J. Environ. Res. Public Health 2022, 19, 14101. [Google Scholar] [CrossRef]
- Nakhaie, R.; Ramos, H.; Vosoughi, D.; Baghdadi, O. Mental Health of Newcomer Refugee and Immigrant Youth during COVID-19. Can. Ethn. Stud. Etudes Ethn. Au Can. 2022, 54, 1–28. [Google Scholar] [CrossRef]
- Payan, D.D.; Perez-Lua, F.; Goldman-Mellor, S.; Young, M.E.D. Rural Household Food Insecurity among Latino Immigrants during the COVID-19 Pandemic. Nutrients 2022, 14, 2772. [Google Scholar] [CrossRef]
- Serafini, R.A.; Powell, S.K.; Frere, J.J.; Saali, A.; Krystal, H.L.; Kumar, V.; Yashaswini, C.; Hernandez, J.; Moody, K.; Aronson, A.; et al. Psychological distress in the face of a pandemic: An observational study characterizing the impact of COVID-19 on immigrant outpatient mental health. Psychiatry Res. 2021, 295, 113595. [Google Scholar] [CrossRef]
- Stein, D.; Bergemann, R.; Lanthorn, H.; Kimani, E.; Nshakira-Rukundo, E.; Li, Y. Cash, COVID-19 and aid cuts: A mixed-method impact evaluation among South Sudanese refugees registered in Kiryandongo settlement, Uganda. BMJ. Glob. Health 2022, 7, e007747. [Google Scholar] [CrossRef]
- van den Muijsenbergh, M.; Torensma, M.; Skowronek, N.; de Lange, T.; Stronks, K. Undocumented Domestic Workers and Coronavirus Disease 2019: A Qualitative Study on the Impact of Preventive Measures. Front. Commun. 2022, 7, 736148. [Google Scholar] [CrossRef]
- Villatoro, A.P.; Wagner, K.M.; de Snyder, V.N.S.; Garcia, D.; Walsdorf, A.A.; Valdez, C.R. Economic and Social Consequences of COVID-19 and Mental Health Burden Among Latinx Young Adults during the 2020 Pandemic. J. Lat. Psychol. 2022, 10, 25–38. [Google Scholar] [CrossRef]
- Weiss-Laxer, N.S.; Brandt, A.J.; Acosta, J.; Boynton-Jarrett, R.; Polk, S.; Mendelson, T.; Platt, R. Group well-child care model for Latino children in immigrant families: Adapting to and learning from the coronavirus disease 2019 (COVID-19) context. Fam. Syst. Health 2022, 40, 364–382. [Google Scholar] [CrossRef] [PubMed]
- Zuntz, A.C.; Klema, M.; Abdullateef, S.; Mazeri, S.; Alnabolsi, S.F.; Alfadel, A.; Abi-habib, J.; Azar, M.; Calia, C.; Burke, J.; et al. Syrian refugee labour and food insecurity in Middle Eastern agriculture during the early COVID-19 pandemic. Int. Labour Rev. 2022, 161, 245–266. [Google Scholar] [CrossRef]
- Pautz, H.; Dempsey, D. COVID-19 and the crisis of food insecurity in the UK. Contemp. Soc. Sci. 2022, 17, 434–449. [Google Scholar] [CrossRef]
- Manirambona, E.; Uwizeyimana, T.; Uwiringiyimana, E.; Reddy, H. Impact of the COVID-19 pandemic on the food rations of refugees in Rwanda. Int. J. Equity Health 2021, 20, 107. [Google Scholar] [CrossRef]
- Mukumbang, F.C.; Ambe, A.N.; Adebiyi, B.O. Unspoken inequality: How COVID-19 has exacerbated existing vulnerabilities of asylum-seekers, refugees, and undocumented migrants in South Africa. Int. J. Equity Health 2020, 19, 141. [Google Scholar] [CrossRef]
- Odunitan-Wayas, F.A.; Alaba, O.A.; Lambert, E.V. Food insecurity and social injustice: The plight of urban poor African immigrants in South Africa during the COVID-19 crisis. Glob. Public Health 2021, 16, 149–152. [Google Scholar] [CrossRef]
- Payan, D.D.; Diaz Rios, L.K.; Ramirez, A.S.; De Trinidad Young, M.E. Structural Barriers Influencing Food Insecurity, Malnutrition, and Health Among Latinas During and After COVID-19: Considerations and Recommendations. J. Acad. Nutr. Diet. 2021, 121, 837–843. [Google Scholar] [CrossRef]
- Clark, E.; Fredricksid, K.; Woc-Colburn, L.; Bottazzi, M.E.; Weatherheadid, J. Disproportionate impact of the COVID-19 pandemic on immigrant communities in the United States. PLoS Negl. Trop. Dis. 2020, 14, e0008484. [Google Scholar] [CrossRef]
- Woertz, E. Wither the self-sufficiency illusion? Food security in Arab Gulf States and the impact of COVID-19. Food Secur. 2020, 12, 757–760. [Google Scholar] [CrossRef]
- Rodriguez, C.; Crowder, S.L.; Rodriguez, M.; Redwine, L.; Stern, M. Food Insecurity and the Hispanic Population during the COVID-19 Pandemic. Ecol. Food Nutr. 2021, 60, 548–563. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Persoz, L.; Hakiza, S.; Biru, L.; Girmatsion, L. Impact of COVID-19 on Food Security in Ethiopia. Epidemiologia 2022, 3, 161–178. [Google Scholar] [CrossRef]
- Vargas-Vasquez, A.; Aparco, J.P.; Hernandez-Vasquez, A.; Pisfil-Benites, N.; Fuentes-Rivera, H.T. Food Insecurity among the migrant Venezuelan population in Peru during the COVID-19 pandemic. Rev. Chil. De Nutr. 2022, 49, 524–525. [Google Scholar] [CrossRef]
- Gosselin, A.; Melchior, M.; Carillon, S.; Gubert, F.; Ridde, V.; Kohou, V.; Zoumenou, I.; Senne, J.N.; Desgrées du Loû, A. Deterioration of mental health and insufficient COVID-19 information among disadvantaged immigrants in the greater Paris area. J. Psychosom. Res. 2021, 146, 110504. [Google Scholar] [CrossRef]
- Rasul, G.; Nepal, A.K.; Hussain, A.; Maharjan, A.; Joshi, S.; Lama, A.; Gurung, P.; Ahmad, F.; Mishra, A.; Sharma, E. Socio-Economic Implications of COVID-19 Pandemic in South Asia: Emerging Risks and Growing Challenges. Front. Sociol. 2021, 6, 629693. [Google Scholar] [CrossRef] [PubMed]
- Santiago, C.D.; Bustos, Y.; Jolie, S.A.; Flores Toussaint, R.; Sosa, S.S.; Raviv, T.; Cicchetti, C. The impact of COVID-19 on immigrant and refugee families: Qualitative perspectives from newcomer students and parents. Sch. Psychol. 2021, 36, 348–357. [Google Scholar] [CrossRef]
- Gama, A.; Rocha, J.V.; Marques, M.J.; Azeredo-Lopes, S.; Pedro, A.R.; Dias, S. How Did the COVID-19 Pandemic Affect Migrant Populations in Lisbon, Portugal? A Study on Perceived Effects on Health and Economic Condition. Int. J. Environ. Res. Public Health 2022, 19, 1786. [Google Scholar] [CrossRef]
- Bovell-Ammon, A.; Cuba, S.E.d.; Coleman, S.; Ahmad, N.; Black, M.M.; Frank, D.A.; Ochoa, E.; Cutts, D.B. Trends in Food Insecurity and SNAP Participation among Immigrant Families U.S.-Born Young Children. Children 2019, 6, E55. [Google Scholar] [CrossRef]
- Capps, R.; Fix, M.; Batalova, J. Anticipated “Chilling Effects” of the Public-Charge Rule Are Real: Census Data Reflect Steep Decline in Benefits Use by Immigrant Families; Migration Policy Institute: Washingotn, DC, USA, 2020; Available online: https://www.migrationpolicy.org/news/anticipated-chilling-effects-public-charge-rule-are-real (accessed on 4 November 2022).
- Gostin, L.O.; Monahan, J.T.; Kaldor, J.; DeBartolo, M.; Friedman, E.A.; Gottschalk, K.; Kim, S.C.; Alwan, A.; Binagwaho, A.; Burci, G.L.; et al. The legal determinants of health: Harnessing the power of law for global health and sustainable development. Lancet 2019, 393, 1857–1910. [Google Scholar] [CrossRef]
- Alvi, M.; Gupta, M. Learning in times of lockdown: How COVID-19 is affecting education and food security in India. Food Secur. 2020, 12, 793–796. [Google Scholar] [CrossRef]
- Kinsey, E.W.; Hecht, A.A.; Dunn, C.G.; Levi, R.; Read, M.A.; Smith, C.; Niesen, P.; Seligman, H.K.; Hager, E.R. School Closures During COVID-19: Opportunities for Innovation in Meal Service. Am. J. Public Health 2020, 110, 1635–1643. [Google Scholar] [CrossRef] [PubMed]
- Lusk, J.L.; Chandra, R. Farmer and farm worker illnesses and deaths from COVID-19 and impacts on agricultural output. PLoS ONE 2021, 16, e0250621. [Google Scholar] [CrossRef] [PubMed]
- Arumugam, S.; Ozkan, B.; Jayaraman, A.; Mockaisamy, P. Impacts of COVID-19 Pandemic on Global Agriculture, Livelihoods and Food Systems. J. Agric. Sci. Tarim Bilim. Derg. 2021, 27, 239–246. [Google Scholar] [CrossRef]
- Carter, K.N.; Kruse, K.; Blakely, T.; Collings, S. The association of food security with psychological distress in New Zealand and any gender differences. Soc. Sci. Med. 2011, 72, 1463–1471. [Google Scholar] [CrossRef]
- Myers, C.A. Food Insecurity and Psychological Distress: A Review of the Recent Literature. Curr. Nutr. Rep. 2020, 9, 107–118. [Google Scholar] [CrossRef]
- Nagata, J.M.; Ganson, K.T.; Whittle, H.J.; Chu, J.; Harris, O.O.; Tsai, A.C.; Weiser, S.D. Food Insufficiency and Mental Health in the U.S. During the COVID-19 Pandemic. Am. J. Prev. Med. 2021, 60, 453–461. [Google Scholar] [CrossRef]
- Every-Palmer, S.; Jenkins, M.; Gendall, P.; Hoek, J.; Beaglehole, B.; Bell, C.; Williman, J.; Rapsey, C.; Stanley, J. Psychological distress, anxiety, family violence, suicidality, and wellbeing in New Zealand during the COVID-19 lockdown: A cross-sectional study. PLoS ONE 2020, 15, e0241658. [Google Scholar] [CrossRef] [PubMed]
- Ramiz, L.; Contrand, B.; Rojas Castro, M.Y.; Dupuy, M.; Lu, L.; Sztal-Kutas, C.; Lagarde, E. A longitudinal study of mental health before and during COVID-19 lockdown in the French population. Global Health 2021, 17, 29. [Google Scholar] [CrossRef]
- Anantharam, P.; Emerson, L.E.; Bilcha, K.D.; Fairley, J.K.; Tesfaye, A.B. Undernutrition, food insecurity, and leprosy in North Gondar Zone, Ethiopia: A case-control study to identify infection risk factors associated with poverty. PLoS Negl. Trop. Dis. 2021, 15, e0009456. [Google Scholar] [CrossRef]
- Gowda, C.; Hadley, C.; Aiello, A.E. The association between food insecurity and inflammation in the US adult population. Am. J. Public Health 2012, 102, 1579–1586. [Google Scholar] [CrossRef]
- Eicher-Miller, H.A.; Mason, A.C.; Weaver, C.M.; McCabe, G.P.; Boushey, C.J. Food insecurity is associated with iron deficiency anemia in US adolescents. Am. J. Clin. Nutr. 2009, 90, 1358–1371. [Google Scholar] [CrossRef] [PubMed]
- Schmeer, K.K.; Piperata, B.A. Household food insecurity and child health. Matern. Child. Nutr. 2017, 13, e12301. [Google Scholar] [CrossRef] [PubMed]
- Diaz, E.; Benavente, P.; Oliva-Arocas, A. Matusikkerhet under den første fasen av koronapandemien blant innvandrere og for hele befolkningen i Norge. Tidsskr. Velferdsforskning 2021, 24, 1–9. [Google Scholar] [CrossRef]
- Abubakar, I.; Aldridge, R.W.; Delan, D.; Orcutt, M.; Burns, R.; Barreto, M.L.; Dhavan, P.; Fouad, F.M.; Groce, N.; Guo, Y.; et al. The UCL—Lancet Commission on Migration and Health: The health of a world on the move. Lancet 2018, 392, 2606–2654. [Google Scholar] [CrossRef]
- OECD. The Unequal Impact of COVID-19: A Spotlight on Frontline Workers, Migrants and Racial/Ethnic Minorities. Available online: https://www.oecd.org/coronavirus/policy-responses/the-unequal-impact-of-covid-19-a-spotlight-on-frontline-workers-migrants-and-racial-ethnic-minorities-f36e931e/ (accessed on 5 December 2022).

| PICO/PECO Strategy | Search Terms | |
|---|---|---|
| P | Participants | International migrants |
| I or E | Intervention/exposure | COVID-19 |
| C | Control | Not applied for this study |
| O | Outcome | Food (in)security |
| Variable | Total-N |
|---|---|
| Total-N | 46 |
| Country in which study was conducted | |
| America | 23 |
| USA | 19 |
| Canada | 2 |
| Trinidad and Tobago | 1 |
| Peru | 1 |
| Asia | 11 |
| Bangladesh | 4 |
| China | 1 |
| Gulf Cooperation Council countries | 1 |
| Israel | 2 |
| Singapore | 1 |
| Malaysia | 1 |
| Iraq, Lebanon, Turkey, Jordan, and Syria | 1 |
| Africa | 6 |
| Rwanda | 1 |
| South Africa | 2 |
| Uganda | 2 |
| Ethiopia | 1 |
| Europe | 4 |
| Switzerland | 1 |
| United Kingdom | 2 |
| Netherlands | 1 |
| Oceania | 2 |
| Australia | 2 |
| Year published | |
| 2020 | 9 |
| 2021 | 14 |
| 2022 | 23 |
| Publication type | |
| Original research | 37 |
| Qualitative design | 9 |
| Quantitative design | 16 |
| Mixed design | 12 |
| Commentary | 4 |
| Viewpoint | 1 |
| Opinion piece | 1 |
| Literature search | 2 |
| Letter to the editor | 1 |
| Link between COVID-19 Pandemic and Migrants’ Food (in) Security | Number of Studies |
|---|---|
| Increased financial hardship (job loss, decreased working hours, decreased income, and elevated food prices) | 28 |
| Migrants avoided utilising humanitarian food assistance due to legal residency policies and/or fear of deportation | 13 |
| Suspended/reduced humanitarian assistance | 7 |
| Lack of safe, high-quality, and/or culturally appropriate food during the pandemic affected migrants’ food consumption | 6 |
| Closure of schools that offered meals for children | 6 |
| Unavailability of certain food items either due to disturbed supply chain or panic buying | 5 |
| Lack of physical access due to lockdown measures | 3 |
| Language as a barrier to access governmental programmes and food aid | 2 |
| Workers staying at home not able to access food at workplace | 1 |
| Worries of gaining weight during home quarantine (reducing physical activity) that led to skipping meals | 1 |
| Physical Health (8 of 46 Studies) | Mental Health (18 of 46 Studies) |
|---|---|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmed, D.; Benavente, P.; Diaz, E. Food Insecurity among International Migrants during the COVID-19 Pandemic: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 5273. https://doi.org/10.3390/ijerph20075273
Ahmed D, Benavente P, Diaz E. Food Insecurity among International Migrants during the COVID-19 Pandemic: A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(7):5273. https://doi.org/10.3390/ijerph20075273
Chicago/Turabian StyleAhmed, Doua, Pierina Benavente, and Esperanza Diaz. 2023. "Food Insecurity among International Migrants during the COVID-19 Pandemic: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 7: 5273. https://doi.org/10.3390/ijerph20075273
APA StyleAhmed, D., Benavente, P., & Diaz, E. (2023). Food Insecurity among International Migrants during the COVID-19 Pandemic: A Scoping Review. International Journal of Environmental Research and Public Health, 20(7), 5273. https://doi.org/10.3390/ijerph20075273







