Abstract
Background: Violent deaths (i.e., those due to road traffic injury, homicide, and suicide) are among the most important causes of premature and preventable mortality in young people. This study aimed at exploring inequalities in violent death across income levels between males and females aged 10 to 24 years from the Americas in 2015, the SDG baseline year. Methods: In a cross-sectional ecological study design, eleven standard summary measures of health inequality were calculated separately for males and females and for each cause of violent death, using age-adjusted mortality rates and average income per capita for 17 countries, which accounted for 87.9% of the target population. Results: Premature mortality due to road traffic injury and homicide showed a pro-poor inequality pattern, whereas premature mortality due to suicide showed a pro-rich inequality pattern. These inequalities were statistically significant (p < 0.001), particularly concentrated among young males, and dominated by homicide. The ample array of summary measures of health inequality tended to generate convergent results. Conclusions: Significant inequalities in violent death among young people seems to be in place across countries of the Americas, and they seem to be socially determined by both income and gender. These findings shed light on the epidemiology of violent death in young people and can inform priorities for regional public health action. However, further investigation is needed to confirm inequality patterns and to explore underlying mechanisms, age- and sex-specific vulnerabilities, and gender-based drivers of such inequalities.
1. Introduction
The year 2015 marked the end of the Millennium Development Goals era. For the region of the Americas, this era brought much to celebrate, including economic growth [1], increases in national educational attainment for both men and women, and the expansion of health services for millions of people. Despite these achievements, in some areas of development young people aged 10 to 24 years continued to be at a heightened risk of dying prematurely from preventable causes, as reflected by their increasing mortality rates between 2000 and 2015 [2]. Among these causes of premature, preventable mortality among young people, violent deaths due to road traffic injuries, homicide, and suicide stand out [3].
The year 2015 also marked the beginning of the Sustainable Development Goals (SDG) agenda [4]. The region of the Americas has embraced this new global health agenda that prioritizes universal health and equity, as well as the new Global Strategy for Women’s, Children’s and Adolescents’ Health [5]. The SDG Agenda explicitly defines global target indicators for road traffic injury (3.6.1), homicide (16.1.1), and suicide (3.4.2). For the countries from this region to implement this ambitious agenda and fulfill its promise to leave no one behind, they have to start looking beyond regional and national averages and examine inequalities at the local level [6]. In a region dubiously distinguished by being recognized as the most inequitable in the world, especially in terms of income inequality, [1,6] there is an urgent need to identify groups that are disproportionately affected by poor health and/or groups that are at an increased risk of dying prematurely due to avoidable causes, and thereafter act on their social determinants, including the gender-related drivers of these inequalities. To do so, disaggregated data need to be analyzed repeatedly using equity-based measurements.
To support countries in this monitoring task, this study aims at defining a baseline by exploring inequalities in mortality due to the top three causes of violent death (i.e., road traffic injuries, homicide, and suicide) across income levels among young males and females aged 10–24 years, from selected countries of the Americas in 2015, the SDG baseline year.
2. Materials and Methods
A cross-sectional ecological study was conducted by using 2015 mortality data from countries of the Americas, available through the Pan American Health Organization (PAHO) Regional Mortality Database. To assemble this data set, death entries of all 34 countries and territories with 2015 data available in the regional mortality database at the time of the study were considered and reviewed for quality, based on data completeness and consistency. An additional standard validation process [7] was applied to correct for deaths that might not have been registered (i.e., under-registration), as well as for those with undetermined underlying causes of death (International Classification of Diseases, Tenth Revision, ICD-10, codes Y10–Y34), followed by proportional redistribution into sex, age group and main burden of disease categories (i.e., communicable, non-communicable, and injuries). ICD-10 codes used were V01–V89 (road traffic injury), X85–Y09 (homicide), and X60–X84 (suicide).
Age-adjusted, cause- and sex-specific mortality rates were calculated using the standard population distribution of the WHO world population age structure for the period 2000–2025. All rates were calculated per 100,000 population, as follows:
where is the number of deaths in age group i, is the population size of the age group i, and represents the weight of the age group i (derived from the standard population distribution, where the population percentages have been rescaled to add up to 1). The actual weights used for the 3 age groups (ages 10–14, 15–19, and 20–24) were 34.0%, 33.5% and 32.5%, respectively.
Standard summary measures of inequality in mortality due to road traffic injury, homicide, and suicide were calculated across the country hierarchy defined by income. We used 2015 estimates of gross national income per capita adjusted by purchase power in 2017-constant international dollars, as reported in the World Bank’s World Development Indicators database. Inequality measurements were computed using the Health Disparities Calculator (HD*Calc) [8], free statistical software developed by the US National Cancer Institute that calculates a set of 11 summary measures of health inequality, including range difference (RD), between-group variation (BGV), absolute concentration index (ACI), slope index of inequality (SII), range ratio (RR), index of disparity (IDisp), mean log deviation (MLD), relative concentration index (RCI), Theil index (T), relative index of inequality (RII), and the Kunst–Mackenbach relative index (KMI) [9,10,11]. Four of these quantities (RD, BGV, ACI, and SII) measure absolute inequality, while the remaining seven measure relative inequality. It is important to calculate both absolute and relative inequality measures because they provide fundamentally different types of information [12]. The standard errors of these inequality measures were computed using the Taylor Series method, as implemented in HD*Calc. Additional details regarding these measures can be found in the HD*Calc documentation [8] and in related publications [13,14,15,16]. More information about the advantages and disadvantages of using different health inequality measures can be found elsewhere [12,17].
After computing inequality measures separately for each sex, we evaluated their differences between sexes by performing hypothesis testing using Z-tests to answer two different types of research questions: the first question was whether each inequality measure was different from its null value, which is 0 for absolute inequality and 1 for relative inequality. In this case, a one-sample Z-test was used. The null hypothesis was that there was no inequality present, denoted by , where is the true value of the inequality measure and is its null value (0 or 1). The test statistic used was
The second question was whether there were differences in the inequality measures between males and females. In this case, a two-sample Z-test was used. The null hypothesis was that there was no difference in inequality between males and females, denoted by , where is the true value of the inequality measure for males and is the true value of the inequality measure for females. The test statistic used was
For both situations, we calculated and reported the corresponding p-values.
3. Results
A total of 17 countries were included in the analysis, comprising Argentina, Belize, Brazil, Canada, Chile, Colombia, Ecuador, Guatemala, Mexico, Nicaragua, Panama, Paraguay, Peru, Puerto Rico, Saint Vincent and the Grenadines, the United States of America, and Uruguay. These countries accounted for 87.9% of the population aged 10 to 24 years in the Americas in 2015 [18].
Table 1 shows the corresponding age-adjusted mortality rates due to the three causes of violent death studied, by sex and country, along with the reference population and the income per capita estimates for the baseline year 2015. Among young males, mortality rates due to road traffic injury ranged from 42.5 per 100,000 in Paraguay to 3.5 in Peru; those due to homicide from 104.9 per 100,000 in Colombia to 1.7 in Canada; and those due to suicide from 19.4 per 100,000 in Uruguay to 1.9 in Peru. Among young females, mortality rates due to road traffic injury ranged from 16.3 per 100,000 in Paraguay to 1.1 in Peru; those due to homicide from 13.9 per 100,000 in Saint Vincent and the Grenadines to 0.5 in Chile; and those due to suicide from 9.7 per 100,000 in Paraguay to 0.5 in Puerto Rico.

Table 1.
Age-adjusted mortality rates (per 100,000 pop) due to road traffic injury, homicide, and suicide in young (10–24 years old) males and females, reference population and average income per capita. Selected countries of the Americas, 2015.
Regional cross-country income-related inequalities in mortality rates were conspicuous in all three causes of violent death and in both sexes. Among young males, all 11 summary measures of inequality in mortality due to road traffic injury, homicide, and suicide were statistically significantly different from their null value of no inequality, whereas among young females statistical significance was reached for all measures of inequality in mortality due to road traffic injury, nine measures of inequality in mortality due to homicide (except RD and RR), and four measures of inequality in mortality due to suicide (RD, BGV, MLD, and T) (details shown in Supplementary Table S1).
Regional cross-country sex-related differences in those income-related inequalities in mortality rates were also conspicuous in all three causes of violent death for most of the summary measures explored. Table 2 shows the results of these inequalities between young males and females. Twenty-six out of all thirty-three pairwise comparisons were statistically significant, mostly in mortality due to homicide and road traffic injury. Invariably, all these statistically significant differences between sexes showed excess mortality among young males.

Table 2.
Magnitude of mortality inequality, its standard error, and p-value, by type of inequality measurement, sex, and cause of violent death in young (10–24 years old) people. Region of the Americas, 2015.
The presence of mortality gradients across the income hierarchy between countries was apparent and statistically significant for both sexes and the three causes of violent death explored, yet the patterns of inequality were distinctive in each case, as explained below.
Figure 1 shows the cross-country income-related inequality gradients in mortality due to road traffic injury for young people of both sexes in the Americas. Among young men, the weighted regression line shows a strong pattern of decreasing inequality with increasing income; that is, a disproportionate concentration of the outcome of interest (mortality, in our study) at the poorer end of the social hierarchy, the so-called pro-poor inequality pattern. This pattern corresponds to the non-zero negative value of the slope index of inequality (SII), which amounts to −17.89 (95%CI: −18.87; −16.91). In contrast, there is a weak pro-rich inequality pattern among young women (SII: 1.27; 95%CI: 0.74; 1.80); that is, a disproportionate concentration of deaths due to road traffic injury at the richer end of the female social hierarchy.
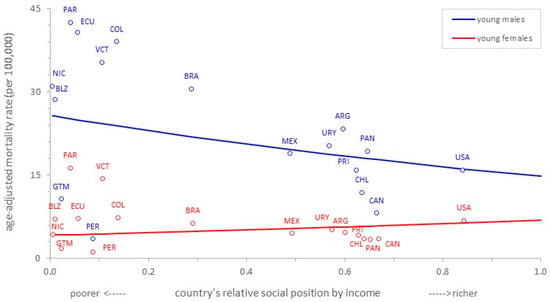
Figure 1.
Cross-country income-related inequality gradients in mortality due to road traffic injury in young (10–24 years old) males and females. Region of the Americas, 2015.
Figure 2 shows the cross-country income-related inequality gradients in mortality due to homicide for young people of both sexes in the Americas. There is a pro-poor inequality pattern for both sexes, and both are statistically significant, although the disproportionate concentration of deaths due to homicide at the poorer end of the social hierarchy is more apparent among young males. The SII in young men was −81.75 (95%CI: −83.00; −80.50), whereas in young women it was −5.55 (95%CI: −5.96; −5.14).
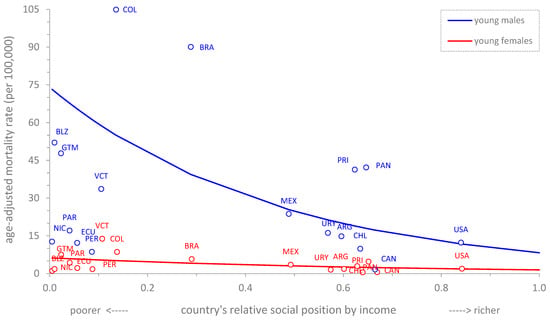
Figure 2.
Cross-country income-related inequality gradients in mortality due to homicide in young (10–24 years old) males and females. Region of the Americas, 2015.
Figure 3 shows the cross-country income-related inequality gradients in mortality due to suicide for young people of both sexes in the Americas. There is a distinctive pro-rich inequality pattern among young males (SII: 7.78; 95%CI: 7.07; 8.49); the higher the relative social position defined by income per capita of a country, the higher the disproportionality in the concentration of deaths due to suicide in young men in that country. There is no statistically discernible pattern of inequality in mortality due to suicide among young women (SII: 0.09; 95%CI: −0.36; 0.54).
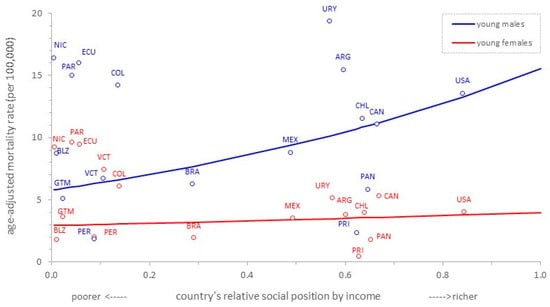
Figure 3.
Cross-country income-related inequality gradients in mortality due to suicide in young (10–24 years old) males and females. Region of the Americas, 2015.
4. Discussion
Violent unintentional and intentional deaths—including those due to road traffic injury, homicide, and suicide—are among the most important causes of premature and preventable mortality, especially in young people [19,20]. Our study highlights the underlying inequality in the distribution of these preventable risks across country income levels and sexes in people aged 10 to 24 years in the Americas by 2015, the SDG timeframe baseline year, by quantifying the magnitude of such disparities through 11 standard summary measures of health (mortality) inequality.
As expected, the quantification of social inequalities in mortality with different summary measures yielded different numerical results, yet they mostly converged toward the prevailing cause-sex inequality pattern. This is the case because each metric has unique mathematical properties inherent to its definition. For instance, some of them (such as RD and RR) quantify the inequality by a single pairwise comparison, usually between unweighted extreme social groups (such as the poorest and richest income quintiles), whereas others (such as BGV and MLD) quantify the inequality across all weighted social groups; other metrics (such as ACI, RCI, SII and RII) are sensitive to the polarity of the social hierarchy; and yet others (such as BGV and T) impose greater aversion to inequality [8,9,12,17,21,22]. On the other hand, far from being a value-neutral process, the measurement of health inequalities is inevitably affected by implicit value judgments [23]. These constraints notwithstanding, as our study has shown, most of the summary measures of health inequality converge in reproducing either a pro-poor or a pro-rich inequality pattern when this is statistically present in the data. This is so either for the absolute (i.e., the first four measures listed in Table 2) and the relative (i.e., the remaining seven) inequality summary measures for all three causes of violent death studied. Absolute inequality is assessed in the additive scale, and therefore it expresses the magnitude of inequality in absolute terms; that is, in the same units of the health variable (namely, deaths per 100,000 people aged 10–24 years). Relative inequality is assessed in the multiplicative scale, and therefore it expresses the magnitude of inequality in relative terms; that is, as a mortality rate ratio. Heuristically, both absolute and relative measures of inequality summarize the difference and the ratio, respectively, of the mortality rate at the extremes of the social hierarchy as defined by the stratifier (i.e., the country average income per capita), from the most disadvantaged (poorest end) to the least disadvantaged. It is worth noting that, of the thirty-three gender gap inequalities assessed as shown in Table 2, only five lacked statistical significance; not surprisingly, four of these referred to suicide which, among the three causes of violent death analyzed, is the least frequent (i.e., lowest rates). Moreover, the five statistically non-significant results correspond to less sophisticated summary measures of inequality: range ratio (RR) only uses the information of extreme quartiles; index of disparity (IDisp) does not take into account the size of the classes (i.e., countries); and the mean log deviation (MLD), as its name implies, works in the contracted logarithmic scale.
Consistent with our findings, Kristensen et al. [24] found an inverse relationship between the municipal proportion of high-income earners and road traffic injury mortality among adolescents (16 to 20 years old) in Norway; Pirdavani et al. [25], studying the general population of Flanders, Belgium, found a similar pro-poor inequality pattern only among males; and Harper et al. [26] found an analogous inequality pattern among US adults, but across the education gradient after controlling for age, sex, and race. In Iran, an analysis of the Multiple Indicator Demographic and Health Survey among women and children under 5 years of age by Roshanfekr et al. [27] yielded a negative SII value for road traffic injury mortality, revealing the same pro-poor pattern. To the best of our knowledge, our finding of a (weak) cross-country pro-rich inequality pattern in premature mortality due to road traffic injury among young females in the Americas has not been reported previously in the literature, and demands in-depth inquiry into its true causal nature, if any, and possible underlying mechanisms.
The finding of a clear cross-country pro-poor inequality pattern in mortality due to homicide among young males and females—along with its significant gender gap—is also supported by external evidence [28,29,30,31,32], albeit in studies on either general or adult populations. Interestingly, this inequality pattern is found to be mediated by an array of psychosocial factors, such as income inequality [28,29,30], interpersonal trust and social capital [28], social disorganization [31], institutionalization of social norms [32], and even climate temperature [30]. It remains to be explored what particular psychosocial factors and vulnerabilities might be at play among adolescents and young adults in the Americas that could explain the ubiquitous inequality pattern observed elsewhere.
Our study found a statistically significant positive mortality gradient due to suicide among young males in the cross-country social hierarchy defined by income level. The association between income and suicide has been well known since the time of Émile Durkheim [33], the formal father of modern sociology, although the direction of that association is a matter of contention [20,34]. In his seminal 1897 work, Durkheim found a direct relationship between income and suicide, a finding replicated by our study, recognizing the relevance of anomie or social fragmentation in influencing suicide. The same positive gradient has been reported by Bando et al. [34] across São Paulo city’s districts and across Brazil’s microregions. In a study of young people aged 10 to 24 years from 21 Latin American and Caribbean countries using the WHO-CDC Global School Health Survey (GSHS), Elia et al. [35] found a direct relationship between income and obesity, and then a direct relationship between obesity and suicide ideation with planning, suggesting that overweight/obesity might be on the causal pathway from economic disadvantage to suicide. In another study with worldwide GSHS data, Assarson et al. [36] found a positive association of suicide ideation with gender inequality when controlling for income. Other studies have found a negative gradient or inverse relationship between income and suicide, in the Americas [20,37,38] and elsewhere [20,39,40,41], and yet other studies have described the positive gradient between suicide and income inequality rather than income level [37,42,43,44].
The copious supply of summary measures of health inequality available not only makes the decision of which metric to use difficult in principle, but also tells something about the lack of agreement on which is the best for the task at hand. A priori, the selection of a health inequality measure should be based on the study’s primary objective as much as the primary audience of interest. Depending on that, one may choose between quantitatively simpler, more intuitive gap inequality measures or more complex, precise, and sophisticated gradient inequality measures [6,9]. From a practical standpoint, it is a good strategy to explore inequalities with several measures at the same time to verify whether the results converge and the conclusions are qualitatively consistent [12,45]. When drawing conclusions, one should not only focus on the statistical significance of the results, but also pay attention to their practical, public health significance. The latter interpretation is the most important information an analyst can provide to policymakers.
Our study has several limitations. A major one is its ecological design, which prevents making any causal claim; however, its exploratory data analysis approach allows for data pattern extraction [46], which can have very useful informative purposes. In this regard, for instance, the income level considered in this work is the per capita average per country and, as such, it does not reflect the actual income level of the study subjects (i.e., females and males aged 10 to 24 years). Another major limitation is its poor granularity. Using countries as units of analysis not only hides potentially significant vulnerabilities associated with territory and spatially patterned ecosocial inequalities, but also misses a fundamental point: for promoting health equity in the Americas, addressing within-country health inequalities is a higher imperative than exposing between-countries health inequalities. Still, the cross-country approach of our study succeeded in uncovering statistically significant patterns of health inequality that can better inform the epidemiology of violent deaths among young people in the Americas. Additionally, as suggested by Wilkinson [47], it is not uncommon for patterns uncovered at lower levels of granularity to be reproduced at higher levels of granularity. A third limitation of our study is its handling of the income gradient vis à vis the gender gap; we kept invariant the distribution of income per capita across countries regardless of sex (this was so because country data series on income per capita by sex is usually unavailable). If we assume that income is more unequally distributed among women than men, then our results may have underestimated the true mortality inequality. The intersectionality of income and gender in shaping violent death inequalities, therefore, should be taken with caution.
5. Conclusions
Significant inequalities in violent death among young people seem to be in place across countries of the Americas, and they seem to be socially determined by both income and sex/gender. In 2015, the start point of the 2030 Agenda, premature mortality due to road traffic injury and homicide showed a pro-poor inequality pattern, whereas premature mortality due to suicide showed a pro-rich inequality pattern in the studied population. These inequalities were particularly concentrated among young males, and were dominated by homicide as the cause of violent death. In general, the ample array of available summary measures of health inequality seem to generate convergent results. These findings shed light on the epidemiology of violent death in young people of the Americas, and can inform priorities for public health action. However, further investigation is needed at the individual level to confirm inequality patterns and to explore underlying mechanisms, sex- and age-specific vulnerabilities, and gender-based drivers of such avoidable, unnecessary, and socially costly inequalities.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20075256/s1, Table S1: Summary measures of income-related inequality in mortality due to violent death in young (10–24 years old) males and females by cause of death and sex. Region of the Americas (n = 17 countries), 2015.
Author Contributions
Conceptualization, O.J.M., D.Z., Y.H., I.C.E., G.L. and A.S.; methodology, O.J.M., I.C.E., N.A., A.D., G.L. and A.S.; software, D.Z. and Y.H.; validation, O.J.M., I.C.E., N.A., A.D., G.L. and A.S.; formal analysis, O.J.M., D.Z., Y.H. and A.S.; investigation, O.J.M., I.C.E., N.A., A.D., G.L. and A.S.; resources, O.J.M. and A.S.; data curation, O.J.M., D.Z., Y.H. and A.S.; writing—original draft preparation, I.C.E., N.A. and A.S.; writing—review and editing O.J.M., D.Z., Y.H., I.C.E., N.A., A.D., G.L. and A.S.; visualization, O.J.M., D.Z. and Y.H.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data and associated materials can be made available for review upon reasonable request to the corresponding author (sanhueza@paho.org).
Acknowledgments
The authors acknowledge the support of colleagues from the Department of Evidence and Intelligence for Action in Health (EIH) of the Pan American Health Organization.
Conflicts of Interest
The authors declare no conflict of interest. This report contains the collective views of an international group of experts and does not necessarily represent the decisions or the stated policy of the Pan American Health Organization (PAHO).
References
- Shifting Gears to Accelerate Shared Prosperity in Latin America and the Caribbean. 2013. Available online: http://www.worldbank.org/content/dam/Worldbank/document/LAC/PLB%20Shared%20Prosperity%20FINAL.pdf (accessed on 12 January 2018).
- Pan American Health Organization/World Health Organization (PAHO/WHO). Regional Mortality Database; PAHO: Washington, DC, USA, 2019. [Google Scholar]
- Pan American Health Organization. The Health of Adolescent and Youth in the Americas. Implementation of the Regional Strategy and Plan of Action on Adolescent and Youth Health 2010–2018; PAHO: Washington, DC, USA, 2018. [Google Scholar]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development (A/RES/70/1); United Nations: New York, NY, USA, 2015; Available online: https://sdgs.un.org/publications/transforming-our-world-2030-agenda-sustainable-development-17981 (accessed on 16 March 2023).
- The Global Strategy for Women’s, Children’s and Adolescents’ Health (2016–2030). 2016. Available online: http://www.who.int/life-course/partners/global-strategy/global-strategy-2016-2030/en/ (accessed on 12 January 2018).
- Mujica, O.J.; Moreno, C.M. From words to action: Measuring health inequalities to “leave no one behind”. Pan Am. J. Public Health 2019, 43, e12. [Google Scholar] [CrossRef]
- Silvi, J. On the estimation of mortality rates for countries of the Americas. Epidemiol. Bull. Pan Am. Health Organ. 2003, 24, 1–5. [Google Scholar]
- National Cancer Institute. Health Disparities Calculator, Version 2.0.0—September 12, 2019; Division of Cancer Control and Population Sciences, Surveillance Research Program and Healthcare Delivery Research Program, National Cancer Institute: Bethesda, MD, USA, 2019. [Google Scholar]
- Schlotheuber, A.; Hosseinpoor, A.R. Summary measures of health inequality: A review of existing measures and their application. Int. J. Environ. Res. Public Health 2022, 19, 3697. [Google Scholar] [CrossRef] [PubMed]
- Harper, S.; Lynch, J. Methods for Measuring Cancer Disparities: Using Data Relevant to Healthy People 2010 Cancer-Related Objectives; NCI Cancer Surveillance Monograph Series, Number 6: NIH Publication No. 05-5777; National Cancer Institute: Bethesda, MD, USA, 2005. [Google Scholar]
- Harper, S.; Lynch, J. Selected Comparisons of Measures of Health Disparities: A Review Using Databases Relevant to Healthy People 2010 Cancer-Related Objectives; NCI Cancer Surveillance Monograph Series, Number 7: NIH Publication No. 07-6281; National Cancer Institute: Bethesda, MD, USA, 2007. [Google Scholar]
- World Health Organization. Handbook on Health Inequality Monitoring, with a Special Focus on Low- and Middle-Income Countries; World Health Organization: Geneva, Switzerland, 2013; Available online: https://apps.who.int/iris/handle/10665/85345 (accessed on 16 March 2023).
- Preston, S.H.; Haines, M.R.; Pamuk, E. Effects of Industrialization and Urbanization on Mortality in Developed Countries. In Proceedings of the International Population Conference, Manila, Philippines, 1981; Ordina Editions. Solicited Papers: Liege, Belgium, 1981; pp. 233–254. [Google Scholar]
- Pearcy, J.N.; Keppel, K.G. A summary measure of health disparity. Public Health Rep. 2002, 117, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Kakwani, N.; Wagstaff, A.; van Doorslaer, E. Socioeconomic inequalities in health: Measurement, computation, and statistical inference. J. Econom. 1997, 77, 87–103. [Google Scholar] [CrossRef]
- Theil, H. Economics and Information Theory; North-Holland: Amsterdam, The Netherlands, 1967. [Google Scholar]
- Kunst, A.E.; Mackenbach, J.P. Measuring Socioeconomic Inequalities in Health; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 1995. [Google Scholar]
- United Nations Department of Economic and Social Affairs Population Division. World Population Prospects—The 2022 Revision; United Nations: New York, NY, USA, 2022; Available online: https://population.un.org/wpp/ (accessed on 25 February 2023).
- Organisation for Economic Co-Operation and Development. Avoidable Mortality: OECD/EuroStat Lists of Preventable and Treatable Causes of Death (January 2022 Version); OECD: Luxemburg, 2022; Available online: https://www.oecd.org/health/health-systems/Avoidable-mortality-2019-Joint-OECD-Eurostat-List-preventable-treatable-causes-of-death.pdf (accessed on 16 March 2023).
- Cubbin, C.; Smith, G.S. Socioeconomic inequality in injury: Critical issues in design and analysis. Annu. Rev. Public Health 2002, 23, 349–375. [Google Scholar] [CrossRef]
- Wagstaff, A.; Paci, P.; van Doorslaer, E. On the measurement of inequalities in health. Soc. Sci. Med. 1991, 33, 545–557. [Google Scholar] [CrossRef]
- Mackenbach, J.P.; Kunst, A.E. Measuring the magnitude of socioeconomic inequalities in health: An overview of available measures illustrated with two examples from Europe. Soc. Sci. Med. 1997, 44, 757–771. [Google Scholar] [CrossRef]
- Harper, S.; King, N.B.; Meersman, S.C.; Reichman, M.E.; Breen, N.; Lynch, J. Implicit Value judgments in the Measurement of Health Inequalities. Milbank Q. 2010, 88, 4–29. [Google Scholar] [CrossRef]
- Kristensen, P.; Kristiansen, T.; Rehn, M.; Gravseth, H.M.; Bjerkedal, T. Social inequalities in road traffic deaths at age 16–20 years among all 611,654 Norwegians born between 1967 and 1976: A multilevel analysis. INJ Prev. 2012, 18, 3–9. [Google Scholar] [CrossRef]
- Pirdavani, A.; Daniels, S.; van Vlierden, K.; Brijs, K.; Kochan, B. Socioeconomic and sociodemographic inequalities and their association with road traffic injuries. J. Transp. Health 2017, 4, 152–161. [Google Scholar] [CrossRef]
- Harper, S.; Charters, T.J.; Strumpf, E.C. Trends in socioeconomic inequalities in motor vehicle accident deaths in the United States, 1995–2010. Am. J. Epidemiol. 2015, 182, 606–614. [Google Scholar] [CrossRef]
- Roshanfekr, P.; Khodaie-Ardakani, M.R.; Sajjadi, H.; Ardakani, H.M.A. Income-related inequality in traffic accident health outcomes (injury, disability and mortality): Evidence from the nationwide survey in Iran. Iran. J. Public Health 2020, 49, 718–726. [Google Scholar] [CrossRef]
- Elgar, F.J.; Aitken, N. Income inequality, trust and homicide in 33 countries. Eur. J. Public Health 2010, 21, 241–246. [Google Scholar] [CrossRef]
- Gobaud, A.N.; Mehranbod, C.A.; Dong, B.; Dodington JMorrison, C.N. Absolute versus relative socioeconomic disadvantage and homicide: A spatial ecological case-control stydu of US zip codes. INJ Epidemiol. 2022, 9, 7. [Google Scholar] [CrossRef]
- Kuznar, L.A.; Day, J. Homicide, inequality, and climate: Untangling the relationships. Front. Psychol. 2021, 12, 697126. [Google Scholar] [CrossRef]
- Peres, M.F.T.; Nivette, A. Social disorganization and homicide mortality rate trajectories in Brazil between 1991 and 2010. Soc. Sci. Med. 2017, 190, 92–100. [Google Scholar] [CrossRef]
- Briceño-León, R. Understanding homicides in Latin America: Poverty or institutionalization? Ciênc. Saúde Coletiva 2012, 17, 3159–3170. (In Spanish) [Google Scholar] [CrossRef]
- Durkheim, E. Suicide: A Study in Sociology; Spaulding, J.A.; Simpson, G., Translators; The Free Press: New York, NY, USA, 1951. [Google Scholar]
- Bando, D.H.; Brunoni, A.R.; Benseñor, I.M.; Lotufo, P.A. Suicide rates and income in São Paulo and Brazil: A temporal and spatial epidemiologic analysis from 1996 to 2008. BMC Psychiatry 2012, 12, 127. [Google Scholar] [CrossRef]
- Elia, C.; Karamanos, A.; Dregan, A.; O’Keeffe, M.; Wolfe, I.; Sandall, J.; Morgan, C.; Cruickshank, J.K.; Gobin, R.; Wilks, R.; et al. Association of macro-level determinants with adolescent overweight and suicidal ideation with planning: A cross-sectional study of 21 Latin American and Caribbean countries. PLoS Med. 2020, 17, e1003443. [Google Scholar] [CrossRef]
- Assarsson, R.; Petersen, S.; Högberg, B.; Strandh, M.; Johansson, K. Gender inequality and adolescent suicide ideation across Africa, Asia, the South Pacific and Latin America—A cross-sectional study based on the Global School Health Survey (GSHS). Glob. Health Action 2019, 11, e1663619. [Google Scholar] [CrossRef] [PubMed]
- Machado, D.B.; Rasella, D.; dos Santos, D.N. Impact of income inequality and other social determinants on suicide rate in Brazil. PLoS ONE 2015, 10, e124934. [Google Scholar] [CrossRef] [PubMed]
- Swan, B.Q. Economic disparities and suicides: The dynamic panel data analyses of 50 states in the United States. J. Forensic Sci. Res. 2021, 5, 20–29. [Google Scholar] [CrossRef]
- Näher, A.F.; Rummel-Kluge, C.; Hegerl, C. Associations of suicide rates with socioeconomic status and social isolation: Findings from longitudinal register and census data. Front. Psychiatry 2020, 10, 898. [Google Scholar] [CrossRef]
- Hiyoshi, A.; Kondo, N.; Rostila, K. Increasing income-based inequality in suicide mortality among working-age women and men, Sweden, 1990–2007: Is there a point of trend change? J. Epidemiol. Community Health 2018, 72, 1009–1015. [Google Scholar] [CrossRef]
- Hong, J.; Knapp, M.; McGuire, A. Income-related inequalities in the prevalence of depression and suicidal behaviour: A 10-year trend following economic crisis. World Psychiatry 2011, 10, 40–44. [Google Scholar] [CrossRef]
- Carcach, C. A spatio-temporal analysis of suicide in El Salvador. BMC Public Health 2017, 17, 339. [Google Scholar] [CrossRef]
- Kazemi-Galougahi, M.H.; Mansouri, A.; Akbarpour, S.; Baktiyari, M.; Sartipi, M.; Moradzadeh, R. Income-related inequality in completed suicide across the provinces of Iran. Epidemiol. Health 2018, 40, e2018012. [Google Scholar] [CrossRef]
- Inagaki, K. Income inequality and the suicide rate in Japan: Evidence from cointegration and LA-VAR. J. Appl. Econ. 2010, 13, 113–133. [Google Scholar] [CrossRef]
- Harper, S.; Lynch, J.; Meersman, S.C.; Breen, N.; Davis, W.W.; Reichman, M.E. An overview of methods for monitoring social disparities in cancer with an example using trends in lung cancer incidence by area-socioeconomic posittion and race-ethnicity, 1992–2004. Am. J. Epidemiol. 2008, 167, 889–899. [Google Scholar] [CrossRef]
- Tukey, J.W. Exploratory Data Analysis; Addison-Wesley: Reading, PA, USA, 1977. [Google Scholar]
- Wilkinson, R.G. Unhealthy Societies: The Afflictions of Inequality; Routledge: London, UK, 1996. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).