Effectiveness and Safety of Different Treatment Modalities for Patients Older Than 60 Years with Distal Radius Fracture: A Network Meta-Analysis of Clinical Trials
Abstract
1. Introduction
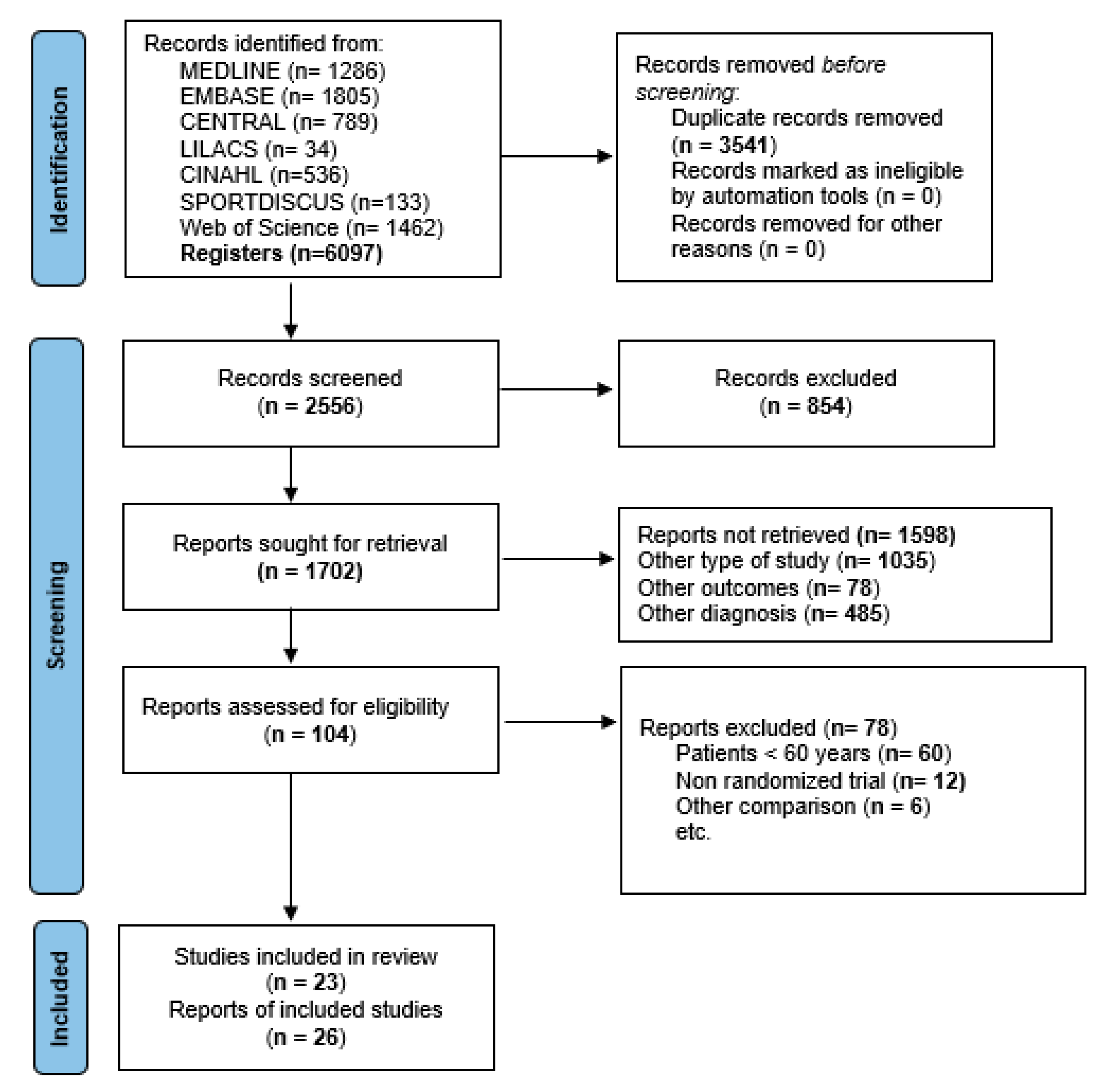
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Electronic Search
2.4. Study Selection
2.5. Data Extraction Process
2.6. Risk of Bias in Individual Studies
2.7. Statistical Methods
3. Results
3.1. Study Selection
3.2. Study Characteristics
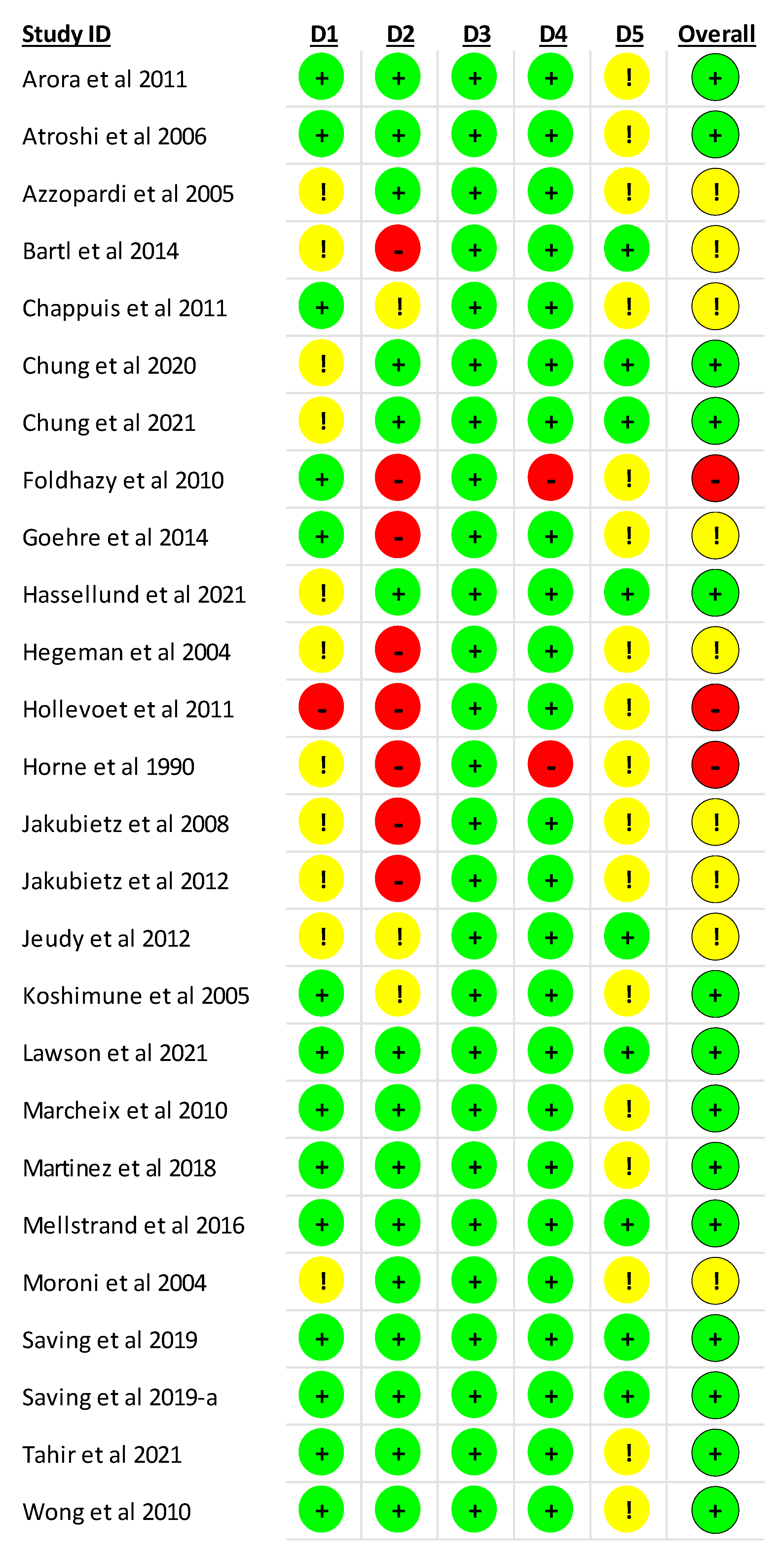
3.3. Risk of Bias Assessment in the Individual Studies
3.4. Network Analyses
3.4.1. Different Modalities of Treatment on Functional Outcomes
3.4.2. Probabilities
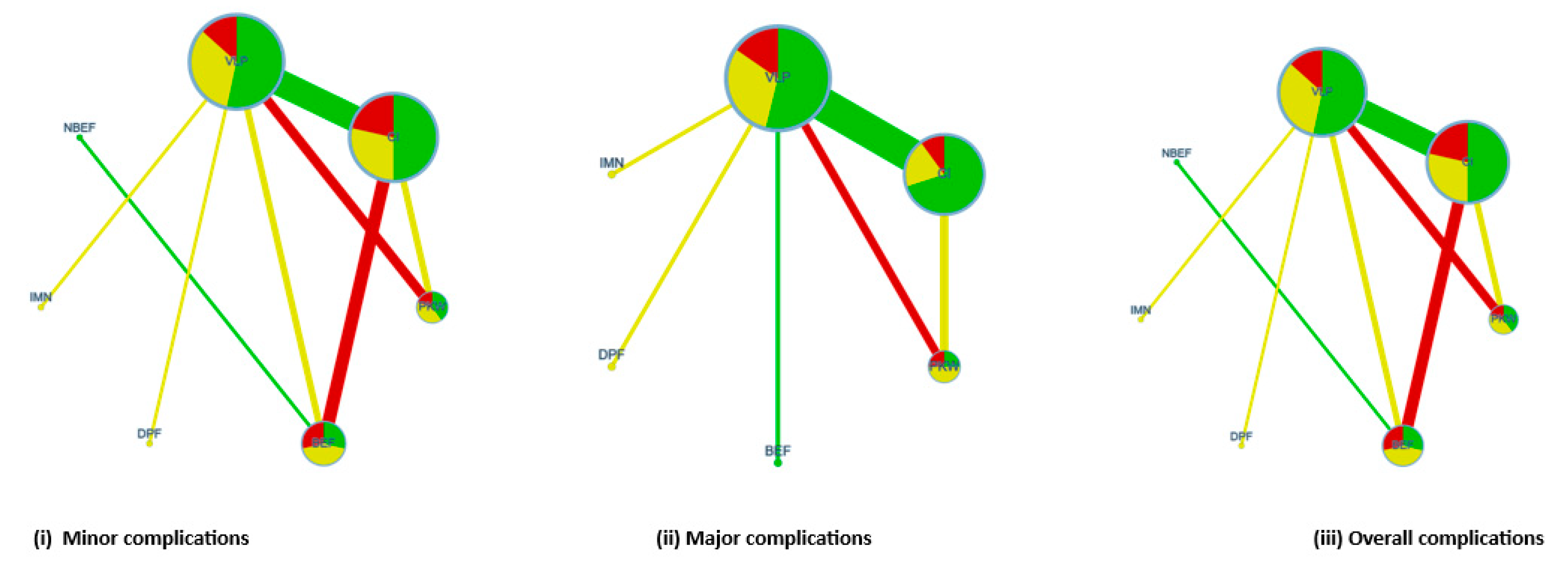
3.4.3. Different Modalities of Treatment on Clinical Complications
3.4.4. Probabilities
3.5. Subgroup and Publication Bias Analyses
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Nellans, K.W.; Kowalski, E.; Chung, K.C. The epidemiology of distal radius fractures. Hand Clin. 2012, 28, 113–125. [Google Scholar] [CrossRef] [PubMed]
- MacIntire, N.J.; Dewan, N. Epidemiology of distal radius fracture and factors predicting risk and prognosis. J. Hand Ther. 2016, 29, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Vannabouathong, C.; Hussain, N.; Guerra-Farfan, E.; Bhandari, M. Interventions for Distal Radius Fractures: A Network Meta-analysis of Randomized Trials. J. Am. Acad. Orthop. Surg. 2019, 27, e596–e605. [Google Scholar] [CrossRef]
- Chung, K.C.; Sasor, S.E.; Speth, K.A.; Wang, L.; Shauver, M.J.; WRIST Group. Patient satisfaction after treatment of distal radial fractures in older adults. J. Hand Surg. Eur. Vol. 2020, 45, 77–84. [Google Scholar] [CrossRef]
- Walenkamp, M.M.J.; Mulders, M.A.M.; Goslings, J.C.; Westert, G.P.; Schep, N.W.L. Analysis of variation in the surgical treatment of patients with distal radial fractures in the Netherlands. J. Hand Surg. Eur. Vol. 2017, 42, 39–44. [Google Scholar] [CrossRef]
- Waljee, J.F.; Zhong, L.; Shauver, M.J.; Chung, K.C. The influence of surgeon age on distal radius fracture treatment in the United States: A population-based study. J. Hand Surg. Am. 2014, 39, 844–851. [Google Scholar] [CrossRef]
- Chung, K.C.; Shauver, M.J.; Birkmeyer, J.D. Trends in the United States in the treatment of distal radial fractures in the elderly. J. Bone Joint Surg. Am. 2009, 91, 1868–1873. [Google Scholar] [CrossRef]
- Mulders, M.A.M.; Detering, R.; Rikli, D.A.; Rosenwasser, M.P.; Goslings, J.C.; Schep, N.W.L. Association between Radiological and Patient-Reported Outcome in Adults with a Displaced Distal Radius Fracture: A Systematic Review and Meta-Analysis. J. Hand Surg. Am. 2018, 43, 710–719. [Google Scholar] [CrossRef]
- Gutiérrez-Monclus, R.; Gutiérrez-Espinoza, H.; Zavala-González, J.; Olguín-Huerta, C.; Rubio-Oyarzún, D.; Araya-Quintanilla, F. Correlation between Radiological Parameters and Functional Outcomes in Patients Older than 60 Years of Age with Distal Radius Fracture. Hand 2019, 14, 770–775. [Google Scholar] [CrossRef]
- Luokkala, T.; Laitinen, M.K.; Hevonkorpi, T.P.; Raittio, L.; Mattila, V.; Launonen, A.P. Distal radius fractures in the elderly population. EFORT Open Rev. 2020, 5, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, H.; Gutiérrez, R.; Aguilera, R.; Ortiz, L. Manejo terapéutico de pacientes con fractura del extremo distal de radio mayores de 60 años: Revisión Sistemática. Rev. Chil. Ortop. Y Traum. 2010, 51, 79–90. [Google Scholar]
- Diaz-Garcia, R.J.; Oda, T.; Shauver, M.J.; Chung, K.C. A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly. J. Hand Surg. Am. 2011, 36, 824–835. [Google Scholar] [CrossRef]
- Ju, J.H.; Jin, G.Z.; Li, G.X.; Hu, H.Y.; Hou, R.X. Comparison of treatment outcomes between nonsurgical and surgical treatment of distal radius fracture in elderly: A systematic review and meta-analysis. Langenbecks Arch. Surg. 2015, 400, 767–779. [Google Scholar] [CrossRef]
- Song, J.; Yu, A.X.; Li, Z.H. Comparison of conservative and operative treatment for distal radius fracture: A meta-analysis of randomized controlled trials. Int. J. Clin. Exp. Med. 2015, 8, 17023–17035. [Google Scholar]
- Chen, Y.; Chen, X.; Li, Z.; Yan, H.; Zhou, F.; Gao, W. Safety and efficacy of operative versus nonsurgical management of distal radius fractures in elderly patients: A systematic review and meta-analysis. J. Hand Surg. Am. 2016, 41, 404–413. [Google Scholar] [CrossRef]
- Li, Q.; Ke, C.; Han, S.; Xu, X.; Cong, Y.X.; Shang, K.; Liang, J.-D.; Zhang, B.-F. Nonoperative treatment versus volar locking plate fixation for elderly patients with distal radial fracture: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2020, 15, 263. [Google Scholar] [CrossRef]
- Stephens, A.R.; Presson, A.P.; McFarland, M.M.; Zhang, C.; Sirniö, K.; Mulders, M.A.M.; Schep, N.W.L.; Tyser, A.R.; Kazmers, N.H. Volar Locked Plating Versus Closed Reduction and Casting for Acute, Displaced Distal Radial Fractures in the Elderly: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Bone Joint Surg. Am. 2020, 102, 1280–1288. [Google Scholar] [CrossRef]
- Zhang, Y.X.; Li, C.; Wang, S.W.; Zhang, M.L.; Zhang, H.W. Volar plate fixation vs. non-operative management for distal radius fractures in older adults: A meta-analysis. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 3955–3966. [Google Scholar]
- Gutiérrez-Espinoza, H.; Araya-Quintanilla, F.; Olguín-Huerta, C.; Gutiérrez-Monclus, R.; Valenzuela-Fuenzalida, J.; Román-Veas, J.; Campos-Jara, C. Effectiveness of surgical versus conservative treatment of distal radius fractures in elderly patients: A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 2022, 108, 103323. [Google Scholar] [CrossRef]
- Woolnough, T.; Axelrod, D.; Bozzo, A.; Koziarz, A.; Koziarz, F.; Oitment, C.; Gyemi, L.; Gormley, J.; Gouveia, K.; Johal, H. What Is the Relative Effectiveness of the Various Surgical Treatment Options for Distal Radius Fractures? A Systematic Review and Network Meta-analysis of Randomized Controlled Trials. Clin. Orthop. Relat. Res. 2021, 479, 348–362. [Google Scholar] [CrossRef]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.A.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Thomas, J. Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 [Updated 2022]. The Cochrane Collaboration. 2022. Available online: http:/handbook.cochrane.org (accessed on 20 November 2022).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Salanti, G.; Ades, A.E.; Ioannidis, J.P. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: An overview and tutorial. J. Clin. Epidemiol. 2011, 64, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Nikolakopoulou, A.; Higgins, J.P.T.; Papakonstantinou, T.; Chaimani, A.; Giovane, C.D.; Egger, M.; Salanti, G. CINeMA: An approach for assessing confidence in the results of a network meta-analysis. PLoS Med. 2020, 17, e1003082. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials. 1986, 7, 177–188. [Google Scholar] [CrossRef] [PubMed]
- Chaimani, A.; Higgins, J.P.; Mavridis, D.; Spyridonos, P.; Salanti, G. Graphical tools for network meta-analysis in STATA. PLoS One 2013, 8, e76654. [Google Scholar] [CrossRef]
- Sterne, J.A.; Egger, M.; Smith, G.D. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ 2001, 323, 101–105. [Google Scholar] [CrossRef]
- Arora, R.; Lutz, M.; Deml, C.; Krappinger, D.; Haug, L.; Gabl, M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J. Bone Joint Surg. Am. 2011, 93, 2146–2153. [Google Scholar] [CrossRef]
- Atroshi, I.; Brogren, E.; Larsson, G.U.; Kloow, J.; Hofer, M.; Berggren, A.M. Wrist-bridging versus non-bridging external fixation for displaced distal radius fractures: A randomized assessor-blind clinical trial of 38 patients followed for 1 year. Acta Orthop. 2006, 77, 445–453. [Google Scholar] [CrossRef]
- Azzopardi, T.; Ehrendorfer, S.; Coulton, T.; Abela, M. Unstable extra-articular fractures of the distal radius: A prospective, randomised study of immobilisation in a cast versus supplementary percutaneous pinning. J. Bone Joint Surg. Br. 2005, 87, 837–840. [Google Scholar] [CrossRef]
- Bartl, C.; Stengel, D.; Bruckner, T.; Gebhard, F.; ORCHID Study Group. The treatment of displaced intra-articular distal radius fractures in elderly patients. Dtsch. Arztebl. Int. 2014, 111, 779–787. [Google Scholar] [CrossRef]
- Chappuis, J.; Bouté, P.; Putz, P. Dorsally displaced extra-articular distal radius fractures fixation: Dorsal IM nailing versus volar plating. A randomized controlled trial. Orthop. Traumatol. Surg. Res. 2011, 97, 471–478. [Google Scholar] [CrossRef]
- Chung, K.C.; Kim, H.M.; Malay, S.; Shauver, M.J.; Wrist and Radius Injury Surgical Trial Group. The Wrist and Radius Injury Surgical Trial: 12-Month Outcomes from a Multicenter International Randomized Clinical Trial. Plast. Reconstr. Surg. 2020, 145, 1054e–1066e. [Google Scholar] [CrossRef]
- Chung, K.C.; Kim, H.M.; Malay, S.; Shauver, M.J.; WRIST Group. Comparison of 24-Month Outcomes after Treatment for Distal Radius Fracture: The WRIST Randomized Clinical Trial. JAMA Netw. Open. 2021, 4, e2112710. [Google Scholar] [CrossRef]
- Földhazy, Z.; Ahrengart, L. External fixation versus closed treatment of displaced distal radial fractures in elderly patients: A randomized controlled trial. Curr. Orthop. Pract. 2010, 21, 288–295. [Google Scholar] [CrossRef]
- Goehre, F.; Otto, W.; Schwan, S.; Mendel, T.; Vergroesen, P.P.; Lindermann-Sperfeld, L. Comparison of palmar fixed-angle plate fixation with K-wire fixation of distal radius fractures (AO A2, A3, C1) in elderly patients. J. Hand Surg. Eur. Vol. 2014, 39, 249–257. [Google Scholar] [CrossRef]
- Hassellund, S.S.; Williksen, J.H.; Laane, M.M.; Pripp, A.; Rosales, C.P.; Karlsen, O.; Madsen, J.E.; Frihagen, F. Cast immobilization is non-inferior to volar locking plates in relation to QuickDASH after one year in patients aged 65 years and older: A randomized controlled trial of displaced distal radius fractures. Bone Joint J. 2021, 103-B(2), 247–255. [Google Scholar] [CrossRef]
- Hegeman, J.H.; Oskam, J.; van der Palen, J.; ten Duis, H.J.; Vierhout, P.A.M. Primary external fixation versus plaster immobilization of the intra-articular unstable distal radial fracture in the elderly. Aktuelle Traumatol. 2004, 34, 64–70. [Google Scholar] [CrossRef]
- Hollevoet, N.; Vanhoutie, T.; Vanhove, W.; Verdonk, R. Percutaneous K-wire fixation versus palmar plating with locking screws for Colles’ fractures. Acta Orthop. Belg. 2011, 77, 180–187. [Google Scholar]
- Horne, J.G.; Devane, P.; Purdie, G. A prospective randomized trial of external fixation and plaster cast immobilization in the treatment of distal radial fractures. J. Orthop. Trauma. 1990, 4, 30–34. [Google Scholar]
- Jakubietz, R.G.; Gruenert, J.G.; Kloss, D.F.; Schindele, S.; Jakubietz, M.G. A randomised clinical study comparing palmar and dorsal fixed-angle plates for the internal fixation of AO C-type fractures of the distal radius in the elderly. J. Hand Surg. Eur. Vol. 2008, 33, 600–604. [Google Scholar] [CrossRef] [PubMed]
- Jakubietz, M.G.; Gruenert, J.G.; Jakubietz, R.G. Palmar and dorsal fixed-angle plates in AO C-type fractures of the distal radius: Is there an advantage of palmar plates in the long term? J. Orthop. Surg. Res. 2012, 7, 8. [Google Scholar] [CrossRef] [PubMed]
- Jeudy, J.; Steiger, V.; Boyer, P.; Cronier, P.; Bizot, P.; Massin, P. Treatment of complex fractures of the distal radius: A prospective randomised comparison of external fixation ‘versus’ locked volar plating. Injury 2012, 43, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Koshimune, M.; Kamano, M.; Takamatsu, K.; Ohashi, H. A randomized comparison of locking and non-locking palmar plating for unstable Colles’ fractures in the elderly. J. Hand Surg. Br. 2005, 30, 499–503. [Google Scholar] [CrossRef]
- Lawson, A.; Naylor, J.M.; Buchbinder, R.; Ivers, R.; Balogh, Z.J.; Smith, P.; Xuan, W.; Howard, K.; Vafa, A.; Perriman, D.; et al. Surgical Plating vs. Closed Reduction for Fractures in the Distal Radius in Older Patients: A Randomized Clinical Trial. JAMA Surg. 2021, 156, 229–237. [Google Scholar]
- Marcheix, P.S.; Dotzis, A.; Benkö, P.E.; Siegler, J.; Arnaud, J.P.; Charissoux, J.L. Extension fractures of the distal radius in patients older than 50: A prospective randomized study comparing fixation using mixed pins or a palmar fixed-angle plate. J. Hand Surg. Eur. Vol. 2010, 35, 646–651. [Google Scholar] [CrossRef]
- Martinez-Mendez, D.; Lizaur-Utrilla, A.; de-Juan-Herrero, J. Intra-articular distal radius fractures in elderly patients: A randomized prospective study of casting versus volar plating. J. Hand Surg. Eur. Vol. 2018, 43, 142–147. [Google Scholar] [CrossRef]
- Mellstrand Navarro, C.; Ahrengart, L.; Törnqvist, H.; Ponzer, S. Volar Locking Plate or External Fixation with Optional Addition of K-Wires for Dorsally Displaced Distal Radius Fractures: A Randomized Controlled Study. J. Orthop. Trauma. 2016, 30, 217–224. [Google Scholar] [CrossRef]
- Moroni, A.; Vannini, F.; Faldini, C.; Pegreffi, F.; Giannini, S. Cast vs external fixation: A comparative study in elderly osteoporotic distal radial fracture patients. Scand. J. Surg. 2004, 93, 64–67. [Google Scholar] [CrossRef]
- Saving, J.; Severin Wahlgren, S.; Olsson, K.; Enocson, A.; Ponzer, S.; Sköldenberg, O.; Wilcke, M.; Mellstrand Navarro, C. Nonoperative Treatment Compared with Volar Locking Plate Fixation for Dorsally Displaced Distal Radial Fractures in the Elderly: A Randomized Controlled Trial. J. Bone Joint Surg. Am. 2019, 101, 961–969. [Google Scholar] [CrossRef]
- Saving, J.; Enocson, A.; Ponzer, S.; Mellstrand-Navarro, C. External Fixation Versus Volar Locking Plate for Unstable Dorsally Displaced Distal Radius Fractures-A 3-Year Follow-Up of a Randomized Controlled Study. J. Hand Surg. Am. 2019, 44, 18–26. [Google Scholar] [CrossRef]
- Tahir, M.; Khan Zimri, F.; Ahmed, N.; Jamali, A.R.; Mehboob, G.; Watson, K.R.; Faraz, A. Plaster immobilization versus anterior plating for dorsally displaced distal radial fractures in elderly patients in Pakistan. J. Hand Surg. Eur. Vol. 2021, 46, 647–653. [Google Scholar] [CrossRef]
- Wong, T.C.; Chiu, Y.; Tsang, W.L.; Leung, W.Y.; Yam, S.K.; Yeung, S.H. Casting versus percutaneous pinning for extra-articular fractures of the distal radius in an elderly Chinese population: A prospective randomised controlled trial. J. Hand Surg. Eur. Vol. 2010, 35, 202–208. [Google Scholar] [CrossRef]
- Walenkamp, M.M.; de Muinck Keizer, R.J.; Goslings, J.C.; Vos, L.M.; Rosenwasser, M.P.; Schep, N.W. The Minimum Clinically Important Difference of the Patient-rated Wrist Evaluation Score for Patients with Distal Radius Fractures. Clin. Orthop. Relat. Res. 2015, 473, 3235–3241. [Google Scholar] [CrossRef]
- Sorensen, A.A.; Howard, D.; Tan, W.H.; Ketchersid, J.; Calfee, R.P. Minimal clinically important differences of 3 patient-rated outcomes instruments. J. Hand Surg. Am. 2013, 38, 641–649. [Google Scholar] [CrossRef]
- Hardman, J.; Al-Hadithy, N.; Hester, T.; Anakwe, R. Systematic review of outcomes following fixed angle intramedullary fixation of distal radius fractures. Int. Orthop. 2015, 39, 2381–2387. [Google Scholar] [CrossRef]
- Chen, Z.; Zhu, Y.; Zhang, W.; Eltagy, H.; Elerian, S. Comparison of Intramedullary Nail and Volar Locking Plate for Distal Radius Fractures: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Cureus 2021, 13, e17972. [Google Scholar] [CrossRef]
- Wei, J.; Yang, T.B.; Luo, W.; Qin, J.B.; Kong, F.J. Complications following dorsal versus volar plate fixation of distal radius fracture: A meta-analysis. J. Int. Med. Res. 2013, 41, 265–275. [Google Scholar] [CrossRef]
- Del Piñal, F.; Jupiter, J.B.; Rozental, T.D.; Arora, R.; Nakamura, T.; Bain, G.I. Distal radius fractures. J. Hand Surg. Eur. Vol. 2022, 47, 12–23. [Google Scholar] [CrossRef]
- Alter, T.H.; Sandrowski, K.; Gallant, G.; Kwok, M.; IIas, A.M. Complications of Volar Plating of Distal Radius Fractures: A Systematic Review. J. Wrist Surg. 2019, 8, 255–262. [Google Scholar] [CrossRef]


| Cast Immobilization | NA | NA | NA | NA | −1.84 (−3.78, 0.10) |
| −0.7 (−17.12, 15.72) | Intramedullary Nail | NA | NA | NA | −2.3 (−16.82, 12.22) |
| −1 (−7.1, 5.1) | −0.3 (−17.23, 16.63) | Bridging External Fixation | NA | 4 (−2.48, 10.48) | −2 (−3.58, −0.42) |
| 0.64 (−5.78, 7.07) | 1.34 (−15.73, 18.42) | 1.64 (−6.04, 9.33) | Percutaneous Kirshner Wire | NA | −3.8 (−12.19, 4.59) |
| 3 (−8.33, 14.33) | 3.7 (−15.74, 23.14) | 4 (−5.55, 13.55) | 2.36 (−9.9, 14.61) | Nonbridging External Fixation | NA |
| −3 (−6.17, 0.17) | −2.3 (−18.41, 13.81) | −2 (−7.21, 3.21) | −3.64 (−9.29, 2.01) | −6 (−16.88, 4.88) | Volar Locking Plate |
| Cast Immobilization | NA | −4.48 (−8.61, −0.34) |
| −3.45 (−12.46, 5.57) | Bridging External Fixation | −1 (−3.68, 1.68) |
| −4.45 (−8.62, −0.28) | −1 (−9, 6.99) | Volar Locking Plate |
| Cast Immobilization | −2.04 (−8.88, 4.8) | 2 (1.82, 2.19) | NA | 7.25 (1.75, 12.76) |
| −0.06 (−5.43, 5.32) | Bridging External Fixation | 9 (0.36, 17.64) | NA | 4.36 (−4.36, 13.09) |
| 3.69 (−2.45, 9.84) | 3.75 (−3.14, 10.64) | Percutaneous Kirshner Wire | NA | 4 (−4.97, 12.97) |
| −23.89 (−38.33, −9.45) | −23.83 (−9.1, −38.56) | −27.58 (−12.51, −42.65) | Dorsal Plate Fixation | 30 (20.59, 39.41) |
| 6.11 (2, 10.21) | 6.16 (1.12, 11.21) | 2.42 (−3.54, 8.37) | 30 (16.16, 43.84) | Volar Locking Plate |
| Volar Locking Plate | Nonbridging External Fixation | Dorsal Plate Fixation | Percutaneous Kirshner Wire | Bridging External Fixation | Intramedullary Nail | Cast Immobilization | ||
|---|---|---|---|---|---|---|---|---|
| DASH | Rank (PrBest) | 1st (33.1) | 6th (1.3) | - | 5th (5.9) | 2nd (32.7) | 3rd (17.1) | 4th (9.9) |
| SUCRA | 78.8 | 30.5 | - | 39.6 | 57.0 | 52.1 | 42.0 | |
| Mean rank | 2.1 | 4.5 | - | 4.0 | 3.1 | 3.4 | 3.9 | |
| PRWE | Rank (PrBest) | 1st (58.7) | - | - | - | 2nd (40.2) | - | 3rd (1.1) |
| SUCRA | 79.0 | - | - | - | 59.0 | - | 12.0 | |
| Mean rank | 1.4 | - | - | - | 1.8 | - | 2.8 | |
| Grip strength | Rank (PrBest) | 1st (90.2) | - | 5th (0) | 2nd (9.8) | 4th (0) | - | 3rd (0) |
| SUCRA | 97.6 | - | 0.0 | 73.9 | 30.4 | - | 48.1 | |
| Mean rank | 1.1 | - | 5.0 | 2.0 | 3.8 | - | 3.1 | |
| Minor complications | Rank (PrBest) | 1st (57.3) | 5th (1.5) | 7th (0.5) | 4th (3) | 6th (0.5) | 2nd (28.4) | 3rd (8.9) |
| SUCRA | 84.6 | 38.5 | 7.5 | 44.4 | 36.8 | 80.7 | 57.5 | |
| Mean rank | 1.9 | 4.7 | 6.5 | 4.3 | 4.8 | 2.2 | 3.6 | |
| Major complications | Rank (PrBest) | 5th (3.3) | 4th (7.3) | 6th (3.2) | 2nd (23) | 1st (42.5) | 7th (0.1) | 3rd (20.6) |
| SUCRA | 41.1 | 63.5 | 17.9 | 68.3 | 75.9 | 17.8 | 65.6 | |
| Mean rank | 4.5 | 3.2 | 5.9 | 2.9 | 2.4 | 5.9 | 3.1 | |
| Overall complications | Rank (PrBest) | 1st (35.3) | 5th (5.8) | 7th (0.3) | 4th (9.3) | 6th (1.2) | 3rd (13.4) | 2nd (34.7) |
| SUCRA | 84.3 | 42.4 | 2.5 | 48.0 | 41.2 | 64.0 | 67.5 | |
| Mean rank | 1.9 | 4.5 | 6.9 | 4.1 | 4.5 | 3.2 | 2.9 |
| Cast Immobilization | NA | 2.49 (0.77, 8.1) | 0.52 (0.04, 6.02) | NA | NA | 0.48 (0.2, 1.13) |
| 0.28 (0.01, 7.49) | Intramedullary Nail | NA | NA | NA | NA | 1.5 (0.29, 7.73) |
| 1.87 (0.51, 6.77) | 6.7 (0.22, 100) | Bridging External Fixation | NA | NA | 1.08 (0.68, 1.72) | 0.73 (0.37, 1.45) |
| 1.5 (0.28, 8.08) | 5.26 (0.16, 100) | 0.8 (0.11, 5.88) | Percutaneous Kirshner Wire | NA | NA | 0.3 (0.13, 0.71) |
| 19.48 (0.67, 563.7) | 100 (0.75, 1000) | 10 (0.31, 1000) | 12.5 (0.36, 1000) | Dorsal Plate Fixation | NA | 0.15 (0.04, 0.57) |
| 2.36 (0.11, 51.77) | 8.3 (0.09, 1000) | 1.27 (0.08, 20) | 1.56 (0.05, 50) | 0.12 (0.001, 11.1) | Nonbridging External Fixation | NA |
| 0.46 (0.19, 1.14) | 1.61 (0.07, 33.3) | 0.25 (0.07, 0.93) | 0.3 (0.65, 1.45) | 0.02 (0.0009, 0.6) | 0.2 (0.009, 4.35) | Volar Locking Plate |
| Cast Immobilization | NA | NA | 1.6 (0.2, 12.54) | NA | NA | 1.35 (0.78, 2.32) |
| 8.59 (0.36, 204.7) | Intramedullary Nail | NA | NA | NA | NA | 0.2 (0.01, 3.92) |
| 0.78 (0.31, 2) | 0.09 (0.004, 2.33) | Bridging External Fixation | NA | NA | NA | 1.88 (0.87, 4.1) |
| 0.87 (0.22, 3.46) | 0.1 (0.003, 3.03) | 1.1 (0.23, 5.26) | Percutaneous Kirshner Wire | NA | NA | 2.91 (0.49, 17.41) |
| 8.59 (0.36, 204.7) | 1 (0.01, 100) | 11.1 (0.43, 1000) | 10 (0.33, 1000) | Dorsal Plate Fixation | NA | 0.2 (0.01, 3.92) |
| 0.78 (0.01, 46.23) | 0.09 (0.0005, 14.3) | 1 (0.02, 50) | 0.89 (0.01, 50) | 0.09 (0.0005, 14.3) | Nonbridging External Fixation | NA |
| 1.5 (0.86, 2.59) | 0.17 (0.008, 4) | 1.92 (0.84, 4.35) | 1.72 (0.44, 6.7) | 0.17 (0.008, 4) | 1.92 (0.03, 100) | Volar Locking Plate |
| Cast Immobilization | NA | 2.49 (0.77, 8.1) | 1 (0.15, 6.85) | NA | NA | 0.69 (0.34, 1.39) |
| 1.02 (0.05, 19.27) | Intramedullary Nail | NA | NA | NA | NA | 0.75 (0.2, 2.8) |
| 2.01 (0.6, 6.71) | 1.96 (0.09, 50) | Bridging External Fixation | NA | NA | 1.08 (0.68, 1.71) | 0.8 (0.34, 1.92) |
| 1.69 (0.38, 7.47) | 1.67 (0.07, 33.3) | 0.84 (0.14, 5) | Percutaneous Kirshner Wire | NA | NA | 0.49 (0.21, 1.14) |
| 117.36 (2.3, 5997.8) | 100 (0.96, 1000) | 50 (1.02, 1000) | 100 (1.15, 1000) | Dorsal Plate Fixation | NA | 0.27 (0.07, 1.02) |
| 2.54 (0.14, 45.68) | 2.5 (0.04, 100) | 1.27 (0.09, 16.7) | 1.49 (0.06, 33.3) | 0.02 (0.0002, 2.7) | Nonbridging External Fixation | NA |
| 0.7 (0.32, 1.55) | 0.69 (0.04, 11.1) | 0.35 (0.1, 1.19) | 0.41 (0.1, 1.67) | 0.006 (0.0001, 0.28) | 0.28 (0.02, 5) | Volar Locking Plate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gutiérrez-Espinoza, H.; Araya-Quintanilla, F.; Cuyul-Vásquez, I.; Gutiérrez-Monclus, R.; Reina-Gutiérrez, S.; Cavero-Redondo, I.; Arenas-Arroyo, S.N.d. Effectiveness and Safety of Different Treatment Modalities for Patients Older Than 60 Years with Distal Radius Fracture: A Network Meta-Analysis of Clinical Trials. Int. J. Environ. Res. Public Health 2023, 20, 3697. https://doi.org/10.3390/ijerph20043697
Gutiérrez-Espinoza H, Araya-Quintanilla F, Cuyul-Vásquez I, Gutiérrez-Monclus R, Reina-Gutiérrez S, Cavero-Redondo I, Arenas-Arroyo SNd. Effectiveness and Safety of Different Treatment Modalities for Patients Older Than 60 Years with Distal Radius Fracture: A Network Meta-Analysis of Clinical Trials. International Journal of Environmental Research and Public Health. 2023; 20(4):3697. https://doi.org/10.3390/ijerph20043697
Chicago/Turabian StyleGutiérrez-Espinoza, Héctor, Felipe Araya-Quintanilla, Iván Cuyul-Vásquez, Rodrigo Gutiérrez-Monclus, Sara Reina-Gutiérrez, Iván Cavero-Redondo, and Sergio Núñez de Arenas-Arroyo. 2023. "Effectiveness and Safety of Different Treatment Modalities for Patients Older Than 60 Years with Distal Radius Fracture: A Network Meta-Analysis of Clinical Trials" International Journal of Environmental Research and Public Health 20, no. 4: 3697. https://doi.org/10.3390/ijerph20043697
APA StyleGutiérrez-Espinoza, H., Araya-Quintanilla, F., Cuyul-Vásquez, I., Gutiérrez-Monclus, R., Reina-Gutiérrez, S., Cavero-Redondo, I., & Arenas-Arroyo, S. N. d. (2023). Effectiveness and Safety of Different Treatment Modalities for Patients Older Than 60 Years with Distal Radius Fracture: A Network Meta-Analysis of Clinical Trials. International Journal of Environmental Research and Public Health, 20(4), 3697. https://doi.org/10.3390/ijerph20043697







