The Urgent Need for Cardiopulmonary Fitness Evaluation among Wildland Firefighters in Thailand
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Questionnaire Design
- (1)
- General information of the participants, including age, gender, body weight (kg), height (cm), waist circumference (cm), body mass index (BMI, kg/m2), smoking status, and alcohol drinking status. BMI was categorized into four groups using the Asian BMI classification: underweight (<18.5 kg/m2), normal weight (18.5–22.9 kg/m2), overweight (23–24.9 kg/m2), and obese (≥25 kg/m2) [18].
- (2)
- Information on work tasks, including work experience (years), working hours (h/day), shift work, and job tasks.
- (3)
- Prior cardiopulmonary problems, such as myocardial infarction, arrythmia, asthma, and stroke.
2.4. Cardiopulmonary Fitness Assessment
- (1)
- Spirometry, chest X-ray (CXR), and electrocardiogram (EKG) were performed for the participants. The spirometry test was assessed using the SpiroMaster PC-10. The procedures were performed and required at least three acceptable graphs, following the ATS/ERS standards [19]. Various parameters, including FEV1, FCV, and FEV1/FCV, were collected. The Thai Siriraj equation [20] was used as the predicted value reference.
- (2)
- Metabolic equivalents are defined as caloric consumption during an activity. One MET means caloric consumption at rest. They are used as an estimate of functional capacity, with greater METs indicating that more energy is consumed during an activity. To estimate METs for physical activities performed at work, a face-to-face interview using the global physical activity questionnaire (GPAQ) was utilized [21]. The participants were asked about their “intensity and duration” of physical activity at work and in transportation. Using the GPAQ data, the following MET values were used to determine a person’s overall energy expenditure: four METs for moderate activity and eight METs for vigorous activity. The data were analyzed as MET minutes per week based on the intensity of physical activity and duration of activity in minutes per week. We categorized the MET groups as eight METs (19,200 MET minutes per week) and twelve METs (28,800 MET minutes per week) according to the requirements in the guidance of NFPA. The calculation was based on the assumption of 8 working hours in 5 days a week.
- (3)
- The Thai CV risk score was used to estimate the 10-year incidence prediction of cardiovascular disease [22]. The parameters included age, sex, height, blood pressure, smoking status, diabetes history, and waist circumference. The researcher measured each participant’s waist circumference. The risks of over 10% were categorized as intermediate risks.
2.5. Definition of Fitness Level
2.6. Statistical Analysis
3. Results
Cardiopulmonary Fitness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Evaluation of Electrocardiogram and Chest X-ray to Classify Medical Conditions with Work Restrictions
| Category A | Category B | |
| Electrocardiogram If EKG shows any clue to the following list |
|
|
| Chest X-ray If CXR shows any clue to the following list |
|
|
References
- Koopmans, E.; Cornish, K.; Fyfe, T.M.; Bailey, K.; Pelletier, C.A. Health risks and mitigation strategies from occupational exposure to wildland fire: A scoping review. J. Occup. Med. Toxicol. 2022, 17, 2. [Google Scholar] [CrossRef] [PubMed]
- Soteriades, E.S.; Smith, D.L.; Tsismenakis, A.J.; Baur, D.M.; Kales, S.N. Cardiovascular disease in US firefighters: A systematic review. Cardiol. Rev. 2011, 19, 202–215. [Google Scholar] [CrossRef] [PubMed]
- The Department of the Interior. The Essential Functions and Work Conditions of a Wildland Firefighter. Available online: https://www.nifc.gov/medical_standards/index.html (accessed on 5 January 2023).
- The Department of the Interior. Federal Interagency Wildland Firefighter Medical Standards. Available online: https://www.nifc.gov/medical_standards (accessed on 5 January 2023).
- Adetona, O.; Reinhardt, T.E.; Domitrovich, J.; Broyles, G.; Adetona, A.M.; Kleinman, M.T.; Ottmar, R.D.; Naeher, L.P. Review of the health effects of wildland fire smoke on wildland firefighters and the public. Inhal. Toxicol. 2016, 28, 95–139. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Marroyo, J.A.; Lopez-Satue, J.; Pernia, R.; Carballo, B.; Garcia-Lopez, J.; Foster, C.; Villa, J.G. Physiological work demands of Spanish wildland firefighters during wildfire suppression. Int. Arch. Occup. Environ. Health 2012, 85, 221–228. [Google Scholar] [CrossRef] [PubMed]
- National Fire Protection Association (Ed.) NFPA 1582: Standard on Comprehensive Occupational Medical Program for Fire Departments; NFPA: Quincy, MA, USA, 2022. [Google Scholar]
- Cheshire Fire and Rescue Service. Cheshire Fire and Rescue Health Safety and Wellbeing Fitness Policy; Cheshire Fire and Rescue Service: Cheshire, UK, 2018. [Google Scholar]
- Fire and Rescue NSW. Health Standard for Firefighters. Available online: http://fbeu.net/wp-content/uploads/2016/12/FINAL-FRNSW-Health-Standard.pdf (accessed on 1 November 2022).
- Xu, D.; Song, Y.; Meng, Y.; Istvan, B.; Gu, Y. Relationship between Firefighter Physical Fitness and Special Ability Performance: Predictive ReseArch. Based on Machine Learning Algorithms. Int. J. Environ. Res. Public Health 2020, 17, 7689. [Google Scholar] [CrossRef] [PubMed]
- Chizewski, A.; Box, A.; Kesler, R.; Petruzzello, S.J. Fitness Fights Fires: Exploring the Relationship between Physical Fitness and Firefighter Ability. Int. J. Environ. Res. Public Health 2021, 18, 11733. [Google Scholar] [CrossRef]
- Martin, Z.T.; Schlaff, R.A.; Hemenway, J.K.; Coulter, J.R.; Knous, J.L.; Lowry, J.E.; Ode, J.J. Cardiovascular Disease Risk Factors and Physical Fitness in Volunteer Firefighters. Int. J. Exerc. Sci. 2019, 12, 764–776. [Google Scholar]
- Groot, E.; Caturay, A.; Khan, Y.; Copes, R. A systematic review of the health impacts of occupational exposure to wildland fires. Int. J. Occup. Med. Environ. Health 2019, 32, 121–140. [Google Scholar] [CrossRef]
- Amster, E.D.; Fertig, S.S.; Baharal, U.; Linn, S.; Green, M.S.; Lencovsky, Z.; Carel, R.S. Occupational exposuRes. and symptoms among firefighters and police during the carmel forest fire: The Carmel cohort study. Isr. Med. Assoc. J. 2013, 15, 288–292. [Google Scholar]
- Gaughan, D.M.; Siegel, P.D.; Hughes, M.D.; Chang, C.Y.; Law, B.F.; Campbell, C.R.; Richards, J.C.; Kales, S.F.; Chertok, M.; Kobzik, L.; et al. Arterial stiffness, oxidative stress, and smoke exposure in wildland firefighters. Am. J. Ind. Med. 2014, 57, 748–756. [Google Scholar] [CrossRef]
- Jacquin, L.; Michelet, P.; Brocq, F.X.; Houel, J.G.; Truchet, X.; Auffray, J.P.; Carpentier, J.P.; Jammes, Y. Short-term spirometric changes in wildland firefighters. Am. J. Ind. Med. 2011, 54, 819–825. [Google Scholar] [CrossRef] [PubMed]
- Adetona, O.; Hall, D.B.; Naeher, L.P. Lung function changes in wildland firefighters working at prescribed burns. Inhal. Toxicol. 2011, 23, 835–841. [Google Scholar] [CrossRef]
- Kanazawa, M.; Yoshiike, N.; Osaka, T.; Numba, Y.; Zimmet, P.; Inoue, S. Criteria and classification of obesity in Japan and Asia-Oceania. World Rev. Nutr. Diet 2005, 94, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Graham, B.L.; Steenbruggen, I.; Miller, M.R.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, e70–e88. [Google Scholar] [CrossRef] [PubMed]
- Dejsomritrutai, W.; Nana, A.; Maranetra, K.N.; Chuaychoo, B.; Maneechotesuwan, K.; Wongsurakiat, P.; Chierakul, N.; Charoenratanakul, S.; Tscheikuna, J.; Juengprasert, W.; et al. Reference spirometric values for healthy lifetime nonsmokers in Thailand. J. Med. Assoc. Thai. 2000, 83, 457–466. [Google Scholar]
- WHO. Global Physical Activity Questionnaire (GPAQ). Noncommunicable Disease Surveillance, Monitoring and Reporting. Available online: https://www.who.int/publications/m/item/global-physical-activity-questionnaire (accessed on 10 December 2022).
- Vathesatogkit, P.; Woodward, M.; Tanomsup, S.; Ratanachaiwong, W.; Vanavanan, S.; Yamwong, S.; Sritara, P. Cohort profile: The electricity generating authority of Thailand study. Int. J. Epidemiol. 2012, 41, 359–365. [Google Scholar] [CrossRef]
- Li, K.; Lipsey, T.; Leach, H.J.; Nelson, T.L. Cardiac health and fitness of Colorado male/female firefighters. Occup. Med. 2017, 67, 268–273. [Google Scholar] [CrossRef]
- Houck, J.M.; Mermier, C.M.; Beltz, N.M.; Johnson, K.E.; VanDusseldorp, T.A.; Escobar, K.A.; Gibson, A.L. Physical Fitness Evaluation of Career Urban and Wildland Firefighters. J. Occup. Environ. Med. 2020, 62, e302–e307. [Google Scholar] [CrossRef]
- Kenny, G.P.; Groeller, H.; McGinn, R.; Flouris, A.D. Age, human performance, and physical employment standards. Appl. Physiol. Nutr. Metab. 2016, 41, S92–S107. [Google Scholar] [CrossRef]
- Kiss, P.; De Meester, M.; Maes, C.; De Vriese, S.; Kruse, A.; Braeckman, L. Cardiorespiratory fitness in a representative sample of Belgian firefighters. Occup. Med. 2014, 64, 589–594. [Google Scholar] [CrossRef]
- Jae, S.Y.; Kurl, S.; Franklin, B.A.; Laukkanen, J.A. Changes in cardiorespiratory fitness predict incident hypertension: A population-based long-term study. Am. J. Hum. Biol. 2017, 29, e22932. [Google Scholar] [CrossRef] [PubMed]
- Poplin, G.S.; Roe, D.J.; Peate, W.; Harris, R.B.; Burgess, J.L. The association of aerobic fitness with injuries in the fire service. Am. J. Epidemiol. 2014, 179, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Hunter, A.L.; Shah, A.S.; Langrish, J.P.; Raftis, J.B.; Lucking, A.J.; Brittan, M.; Venkatasubramanian, S.; Stables, C.L.; Stelzle, D.; Marshall, J.; et al. Fire Simulation and Cardiovascular Health in Firefighters. Circulation 2017, 135, 1284–1295. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.L.; Horn, G.P.; Fernhall, B.; Kesler, R.M.; Fent, K.W.; Kerber, S.; Rowland, T.W. Electrocardiographic Responses Following Live-Fire Firefighting Drills. J. Occup. Environ. Med. 2019, 61, 1030–1035. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, J.E.; Ugelvig Petersen, K.; Ebbehoj, N.E.; Bonde, J.P.; Hansen, J. Incidence of cardiovascular disease in a historical cohort of Danish firefighters. Occup. Environ. Med. 2018, 75, 337–343. [Google Scholar] [CrossRef]
- Belafsky, S.; Vlach, J.; McCurdy, S.A. Cardiopulmonary fitness and respirator clearance: An update. J. Occup. Environ. Hyg. 2013, 10, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Szeinuk, J.; Beckett, W.S.; Clark, N.; Hailoo, W.L. Medical evaluation for respirator use. Am. J. Ind. Med. 2000, 37, 142–157. [Google Scholar] [CrossRef]
- Niyatiwatchanchai, N.; Pothirat, C.; Chaiwong, W.; Liwsrisakun, C.; Phetsuk, N.; Duangjit, P.; Choomuang, W. Short-term effects of air pollutant exposure on small airway dysfunction, spirometry, health-related quality of life, and inflammatory biomarkers in wildland firefighters: A pilot study. Int. J. Environ. Health Res. 2022, 1–14. [Google Scholar] [CrossRef]
- Andrews, K.L.; Gallagher, S.; Herring, M.P. The effects of exercise interventions on health and fitness of firefighters: A meta-analysis. Scand. J. Med. Sci. Sports 2019, 29, 780–790. [Google Scholar] [CrossRef]
- Yu, C.C.; Au, C.T.; Lee, F.Y.; So, R.C.; Wong, J.P.; Mak, G.Y.; Chien, E.P.; McManus, A.M. Association Between Leisure Time Physical Activity, Cardiopulmonary Fitness, Cardiovascular Risk Factors, and Cardiovascular Workload at Work in Firefighters. Saf. Health Work 2015, 6, 192–199. [Google Scholar] [CrossRef]
- Chizewski, A.; Box, A.; Kesler, R.M.; Petruzzello, S.J. High Intensity Functional Training (HIFT) Improves Fitness in Recruit Firefighters. Int. J. Environ. Res. Public Health 2021, 18, 13400. [Google Scholar] [CrossRef] [PubMed]
- Aadahl, M.; Kjaer, M.; Kristensen, J.H.; Mollerup, B.; Jorgensen, T. Self-reported physical activity compared with maximal oxygen uptake in adults. Eur. J. Cardiovasc. Prev. Rehabil. 2007, 14, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Peate, W.F.; Lundergan, L.; Johnson, J.J. Fitness self-perception and Vo2max in firefighters. J. Occup. Environ. Med. 2002, 44, 546–550. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | Total (N = 62) | Fit (n = 8) | Job Restriction (n = 54) | p-Value |
|---|---|---|---|---|
| N (%) | n (%) | n (%) | ||
| Sex | 0.656 a | |||
| Male | 59 (95.16) | 8 (100) | 51 (94.44) | |
| Female | 3 (4.84) | 0 | 3 (5.56) | |
| Age (year), mean (SD) | 41.66 (10.42) | 42.63 (6.76) | 41.52 (10.90) | 0.700 b |
| Weight (kg), mean (SD) | 67.39 (9.86) | 67.63 (5.45) | 67.35 (10.39) | 0.911 b |
| Height (cm), mean (SD) | 166.24 (6.91) | 166.88 (5.22) | 166.15 (7.16) | 0.731 b |
| Waist circumference (cm), mean (SD) | 34.75 (3.42) | 36.10 (2.32) | 34.55 (3.53) | 0.129 b |
| Work experience (year), mean (SD) | 13.23 (9.97) | 16 (8.09) | 12.82 (10.22) | 0.348 b |
| BMI (kg/m2), mean (SD) | 24.30 (3.06) | 24.30 (1.73) | 24.30 (3.22) | 0.996 b |
| BMI categories | 1.000 a | |||
| Underweight | 1 (1.61) | 0 | 1 (1.85) | |
| Normal | 18 (29.03) | 2 (25.00) | 16 (29.63) | |
| Overweight | 22 (35.48) | 3 (37.50) | 19 (35.19) | |
| Obese | 21 (33.87) | 3 (37.50) | 18 (33.33) | |
| Shift work | 0.620 a | |||
| Yes | 45 (72.58) | 6 (75.00) | 39 (72.22) | |
| No | 17 (27.42) | 2 (25.00) | 15 (27.78) | |
| Smoke | 0.712 a | |||
| Active smoker | 26 (41.94) | 4 (50.00) | 22 (40.74) | |
| Ex-smoker | 20 (32.26) | 3 (37.50) | 17 (31.48) | |
| Non-smoker | 16 (25.81) | 1 (12.50) | 15 (27.78) | |
| Alcohol | 0.403 a | |||
| Regular drinking | 32 (51.61) | 3 (37.50) | 29 (53.70) | |
| Social drinking | 16 (25.81) | 4 (50.00) | 12 (22.22) | |
| Ex-drinking | 5 (8.06) | 0 | 5 (9.26) | |
| Non-drinking | 9 (14.52) | 1 (12.50) | 8 (14.81) |
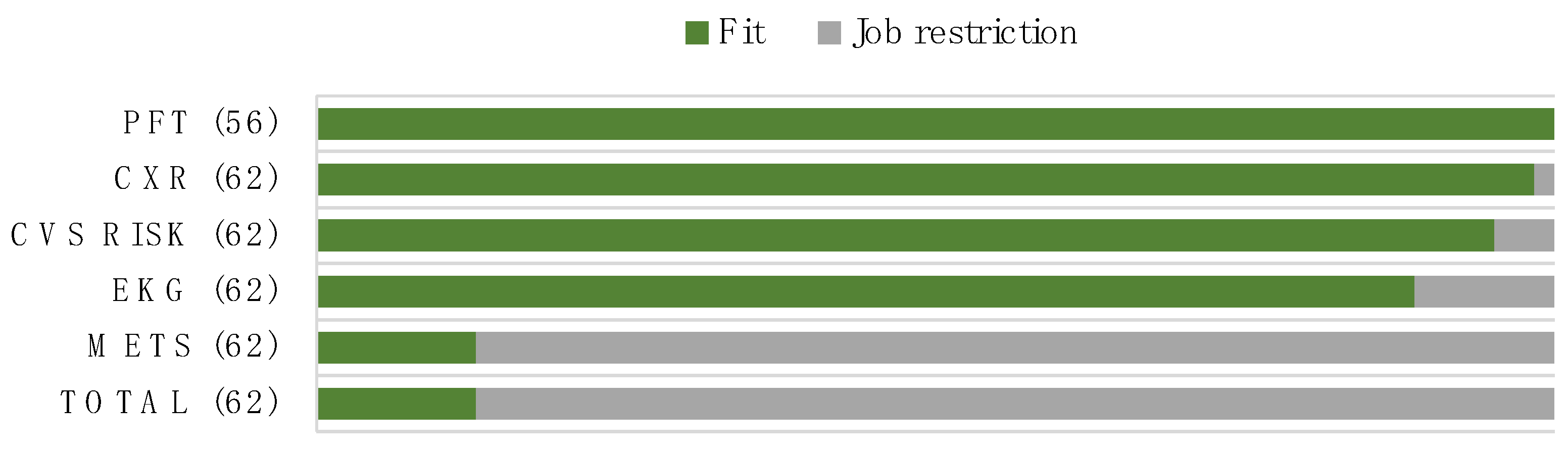
| Cardiopulmonary Parameters | Total (N = 62) | Fit (n = 8) | Job Restriction (n = 54) | p-Value |
|---|---|---|---|---|
| mean (SD) | mean (SD) | mean (SD) | ||
| METs (minutes per week) | 7333.55 (8755.27) | 24,240 (5940) (median, (IQR)) | 4640 (5241.20) | <0.001 a |
| METs | <0.001 b | |||
| MET > 12 | 2 (3.22) | 2 (25.00) | 0 | |
| MET 8–12 | 6 (9.68) | 6 (75.00) | 0 | |
| MET < 8 | 54 (87.10) | 0 | 54 (100) | |
| CV risk in 10 years (%) | 4.53 (3.54) | 2.51 (2.33) (median, (IQR)) | 4.68 (3.66) | 0.629 a |
| CV risk classification (n, %) | 1.00 b | |||
| Low risk | 57 (91.93) | 8 (100) | 49 (90.74) | |
| Intermediate risk | 5 (8.07) | 0 | 5 (9.26) | |
| Resting heart rate (bpm) | 88.48 (13.51) | 88 (11.03) | 88.56 (13.92) | 0.901 c |
| BMI (kg/m2) | 24.30 (3.06) | 24.30 (1.73) | 24.30 (3.22) | 0.996 c |
| SBP (mmHg) | 134.35 (15.87) | 128.63 (10.35) | 135.20 (16.43) | 0.231 c |
| DBP (mmHg) | 76.58 (10.80) | 76.75 (8.36) | 76.56 (11.18) | 0.875 c |
| Pulmonary function * | ||||
| FEV1 (mL) | 3425.54 (811.37) | 3316.25 (495.58) | 3443.75 (855.24) | 0.805 c |
| FVC (mL) | 4171.79 (939.73) | 4116.25 (604.69) | 4181.04 (989.11) | 0.561 c |
| Pulmonary function result * (n, %) | 1.000 b | |||
| Normal | 51 (91.07) | 8 (100) | 43 (89.58) | |
| Obstruction | 4 (7.14) | 0 | 4 (8.34) | |
| Restriction | 1 (1.79) | 0 | 1 (2.08) | |
| Underlying disease (n, %) | ||||
| None | 53 (85.48) | 7 (87.50) | 46 (85.19) | |
| Myocardial infarction | 1 (1.61) | 0 | 1 (1.85) | 1.000 b |
| Arrhythmia | 2 (3.23) | 0 | 2 (3.70) | 1.000 b |
| Asthma | 4 (6.45) | 1 (12.50) | 3 (5.56) | 0.433 b |
| Stroke | 2 (3.23) | 0 | 2 (3.70) | 1.000 b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panumasvivat, J.; Sirikul, W.; Surawattanasakul, V.; Wangsan, K.; Assavanopakun, P. The Urgent Need for Cardiopulmonary Fitness Evaluation among Wildland Firefighters in Thailand. Int. J. Environ. Res. Public Health 2023, 20, 3527. https://doi.org/10.3390/ijerph20043527
Panumasvivat J, Sirikul W, Surawattanasakul V, Wangsan K, Assavanopakun P. The Urgent Need for Cardiopulmonary Fitness Evaluation among Wildland Firefighters in Thailand. International Journal of Environmental Research and Public Health. 2023; 20(4):3527. https://doi.org/10.3390/ijerph20043527
Chicago/Turabian StylePanumasvivat, Jinjuta, Wachiranun Sirikul, Vithawat Surawattanasakul, Kampanat Wangsan, and Pheerasak Assavanopakun. 2023. "The Urgent Need for Cardiopulmonary Fitness Evaluation among Wildland Firefighters in Thailand" International Journal of Environmental Research and Public Health 20, no. 4: 3527. https://doi.org/10.3390/ijerph20043527
APA StylePanumasvivat, J., Sirikul, W., Surawattanasakul, V., Wangsan, K., & Assavanopakun, P. (2023). The Urgent Need for Cardiopulmonary Fitness Evaluation among Wildland Firefighters in Thailand. International Journal of Environmental Research and Public Health, 20(4), 3527. https://doi.org/10.3390/ijerph20043527








