Aerobic and Postural Strength Exercise Benefits in People with Schizophrenia
Abstract
1. Introduction
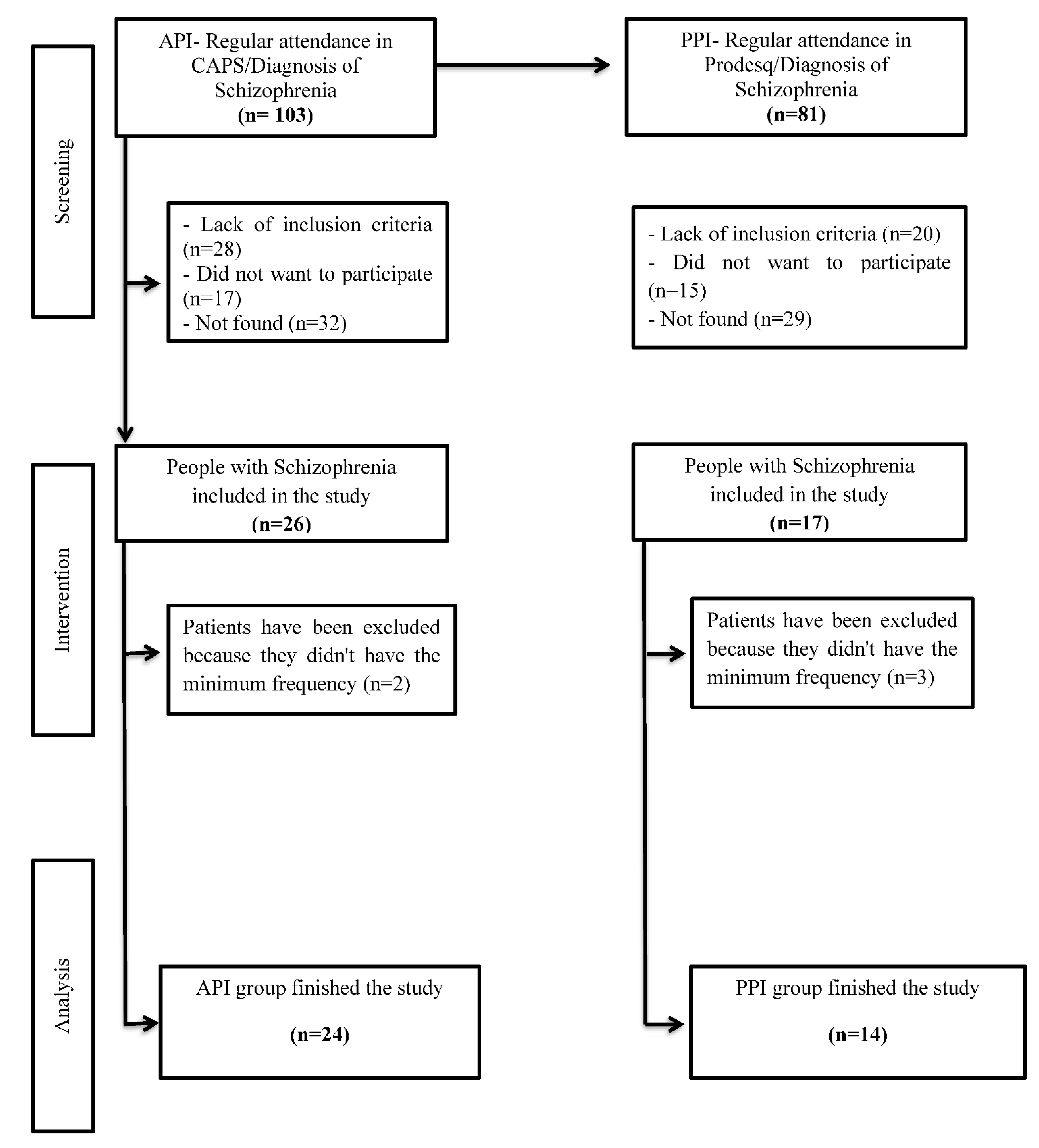
2. Methods
2.1. Trial Design
2.2. Participants
2.3. Ethics
2.4. Clinical Assessment
2.5. Sedentary Lifestyle
2.6. Disease Severity
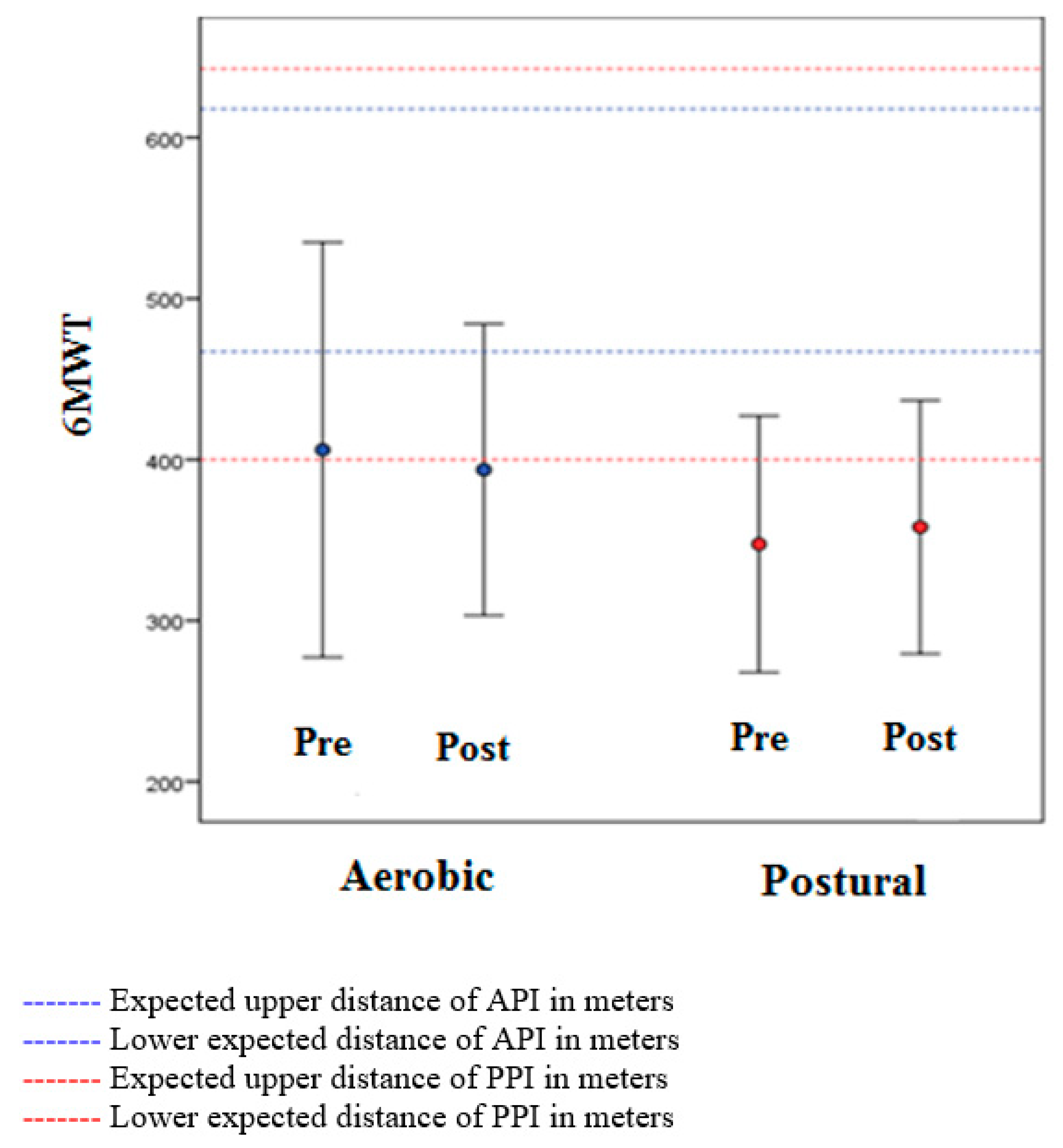
2.7. Physical Performance
2.8. Stretching
2.9. Quality of Life
2.10. Physical Intervention
2.10.1. Aerobic Physical Intervention [API]
2.10.2. Physical Intervention
2.11. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Mental Health. World Health Organization Home. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/schizophrenia (accessed on 1 June 2021).
- Blanchard, J.J.; Cohen, A.S. The structure of negative symptoms within schizophrenia: Implications for assessment. Schizophr. Bull. 2006, 32, 238. [Google Scholar] [CrossRef] [PubMed]
- Batinic, B. Cognitive Models of Positive and Negative Symptoms of Schizophrenia and Implications for Treatment. Psychiatr. Danub. 2019, 31 (Suppl. 2), 181–184. [Google Scholar] [PubMed]
- Vancampfort, D.; Knapen, J.; Probst, M.; Scheewe, T.; Remans, S.; De Hert, M. A systematic review of correlates of physical activity in patients with schizophrenia. Acta Psychiatr. Scand. 2012, 125, 352–362. [Google Scholar] [CrossRef] [PubMed]
- Fagiolini, A.; Goracci, A. The effects of undertreated chronic medical illnesses in patients with severe mental disorders. J. Clin. Psychiatry 2009, 70 (Suppl. 3), 22–29. [Google Scholar] [CrossRef]
- Vancampfort, D.; Probst, M.; Scheewe, T.; Knapen, J.; De Herdt, A.; De Hert, M. The functional exercise capacity is correlated with global functioning in patients with schizophrenia. Acta Psychiatr. Scand. 2012, 125, 382–387. [Google Scholar] [CrossRef]
- Mittal, V.A.; Vargas, T.; Osborne, K.J.; Dean, D.; Gupta, T.; Ristanovic, I.; Hooker, C.; Shankman, S.A. Exercise Treatments for Psychosis: A Review. Curr. Treat. Options Psychiatry 2017, 4, 152–166. [Google Scholar] [CrossRef]
- Abdul Rashid, N.A.; Nurjono, M.; Lee, J. Clinical determinants of physical activity and sedentary behaviour in individuals with schizophrenia. Asian J. Psychiatr. 2019, 46, 62–67. [Google Scholar] [CrossRef]
- Firth, J.; Cotter, J.; Elliott, R.; French, P.; Yung, A.R. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol. Med. 2015, 45, 1343–1361. [Google Scholar] [CrossRef]
- Stubbs, B.; Williams, J.; Gaughran, F.; Craig, T. How sedentary are people with psychosis? A systematic review and meta-analysis. Schizophr. Res. 2016, 171, 103–109. [Google Scholar] [CrossRef]
- Girdler, S.; Confino, J.; Woesner, M. Exercise as a Treatment for Schizophrenia: A Review. Psychopharmacol. Bull. 2019, 49, 56–69. [Google Scholar]
- Dauwan, M.; Begemann, M.J.; Heringa, S.M.; Sommer, I. Exercise Improves Clinical Symptoms, Quality of Life, Global Functioning, and Depression in Schizophrenia: A Systematic Review and Meta-analysis. Schizophr. Bull. 2016, 42, 588–599. [Google Scholar] [CrossRef] [PubMed]
- Vancampfort, D.; Probst, M.; De Hert, M.; Soundy, A.; Stubbs, B.; Stroobants, M.; De Herdt, A. Neurobiological effects of physical exercise in schizophrenia: A systematic review. Disabil. Rehabil. 2014, 36, 1749–1754. [Google Scholar] [CrossRef] [PubMed]
- Vakhrusheva, J.; Marino, B.T.; Stroup, S.; Kimhy, D. Aerobic Exercise in People with Schizophrenia: Neural and Neurocognitive Benefits. Curr. Behav. Neurosci. Rep. 2016, 3, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Firth, J.; Stubbs, B.; Vancampfort, D.; Schuch, F.; Lagopoulos, J.; Rosenbaum, S.; Ward, P. Effect of aerobic exercise on hippocampal volume in humans: A systematic review and meta-analysis. Neuroimage 2018, 166, 230–238. [Google Scholar] [CrossRef]
- Vogel, J.S.; van der Gaag, M.; Slofstra, C.; Knegtering, H.; Bruins, J.; Castelein, S. The effect of mind-body and aerobic exercise on negative symptoms in schizophrenia: A meta-analysis. Psychiatry Res. 2019, 279, 295–305. [Google Scholar] [CrossRef]
- Cristiano, V.; Szortyka, M.; Lobato, M.; Ceres, K.; Belmonte-de-Abreu, P. Postural changes in different stages of schizophrenia is associated with inflammation and pain: A cross-sectional observational study. Int. J. Psychiatry Clin. Pract. 2016, 21, 104–111. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Reed, G.M. Toward ICD-11: Improving the clinical utility of WHO’s International Classification of mental disorders. Prof. Psychol. Res. Pract. 2010, 41, 457–464. [Google Scholar] [CrossRef]
- Rosenbaum, S.; Morell, R.; Abdel-Baki, A.; Ahmadpanah, M.; Anilkumar, T.; Baie, L.; Bauman, A.; Bender, S.; Han, J.; Brand, S.; et al. Assessing physical activity in people with mental illness: 23-country reliability and validity of the simple physical activity questionnaire (SIMPAQ). BMC Psychiatry 2020, 20, 108. [Google Scholar] [CrossRef]
- Available online: http://conitec.gov.br/images/Relatorios/2016/Diretrizes_Metodologicas_WEB.pdf (accessed on 1 June 2021).
- American Thoracic Society. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Enright, P.L. The six-minute walk test. Respir. Care 2003, 48, 783–785. [Google Scholar]
- Wells, K.F.; Dillon, E.K. The Sit and Reach—A Test of Back and Leg Flexibility, Research Quarterly. Am. Assoc. Health Phys. Educ. Recreat. 1952, 23, 115–118. [Google Scholar] [CrossRef]
- Martín-Sierra, A.; Vancampfort, D.; Probst, M.; Bobes, J.; Maurissen, K.; Sweers, K.; De Schepper, E.; De Hert, M. Walking capacity is associated with health related quality of life and physical activity level in patients with schizophrenia: A preliminary report. Actas Esp. Psiquiatr. 2011, 39, 211–216. [Google Scholar] [PubMed]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age—Predicted Maximal Heart Revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Suetani, S.; Waterreus, A.; Morgan, V.; Foley, D.L.; Galletly, C.; Badcock, J.C.; Watts, G.; Scott, J.G.; Mcgrath, J.J. The importance of the physical health needs of people with psychotic disorders. Aust. N. Z. J. Psychiatry 2017, 51, 94–95. [Google Scholar] [CrossRef] [PubMed]
- Stubbs, B.; Firth, J.; Berry, A.; Schuch, F.; Rosenbaumg, S.; Gaughran, F.; Veronesse, N.; Williams, J.; Craig, T.; Yung, A.; et al. How much physical activity do people with schizophrenia engage in? A systematic review, comparative meta-analysis and meta-regression. Schizophr. Res. 2016, 176, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Dodd, K.J.; Duffy, S.; Stewart, J.A.; Impey, J.; Taylor, N. A small group aerobic exercise programme that reduces body weight is feasible in adults with severe chronic schizophrenia: A pilot study. Disabil. Rehabil. 2011, 33, 1222–1229. [Google Scholar] [CrossRef]
- Battaglia, G.; Alesi, M.; Inguglia, M.; Roccella, M.; Caramazza, G.; Bellafiore, M.; Palma, A. Soccer practice as an add-on treatment in the management of individuals with a diagnosis of schizophrenia. Neuropsychiatr. Dis. Treat. 2013, 9, 595–603. [Google Scholar] [CrossRef]
- Vancampfort, D.; Rosenbaum, S.; Schuch, F.; Ward, P.; Richards, J.; Mugisha, J.; Probst, M.; Stubbs, B. Cardiorespiratory Fitness in Severe Mental Illness: A Systematic Review and Meta-analysis. Sports Med. 2016, 47, 343–352. [Google Scholar] [CrossRef]
- Cramer, H.; Lauche, R.; Klose, P.; Langhorst, J.; Dobos, G. Yoga for schizophrenia: A systematic review and meta-analysis. BMC Psychiatry 2013, 13, 32. [Google Scholar] [CrossRef]
- Kaltsatou, A.; Kouidi, E.; Fountoulakis, K.; Sipka, C.; Theochari, V.; Kandylis, D.; Deligiannis, A. Effects of exercise training with traditional dancing on functional capacity and quality of life in patients with schizophrenia: A randomized controlled study. Clin. Rehabil. 2015, 29, 882–891. [Google Scholar] [CrossRef] [PubMed]
- Shrier, I. Does Stretching Help Prevent Injuries. In Evidence-Based Sports Medicine; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2007; pp. 36–58. [Google Scholar] [CrossRef]
- Assumpção, A.; Matsutani, L.; Yuan, S.; Santo, A.; Sauer, J.; Mango, P.; Marques, A. Muscle stretching exercises and resistance training in fibromyalgia: Which is better? A three-arm randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2018, 54, 663–670. [Google Scholar] [CrossRef] [PubMed]
- da Silva, L.A.; Tortelli, L.; Motta, J.; Menguer, L.; Mariano, S.; Tasca, G.; Silveira, G.D.B.; Pinho, R.A.; Silveira, P.C.L. Effects of aquatic exercise on mental health, functional autonomy and oxidative stress in depressed elderly individuals: A randomized clinical trial. Clinics 2019, 74, e322. [Google Scholar] [CrossRef] [PubMed]
- Vancampfort, D.; Probst, M.; Sweers, K.; Knapen, J.; Hert, M. Relationships between obesity, functional exercise capacity, physical activity participation and physical self-perception in people with schizophrenia. Acta Psychiatr. Scand. 2011, 123, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Vancampfort, D.; Kim, S.; Michel, P.; Mitchell, A.; Knapen, J.; Hert, M. Quality Assessment of Physical Activity Recommendations Within Clinical Practice Guidelines for the Prevention and Treatment of Cardio-metabolic Risk Factors in People with Schizophrenia. Community Ment. Health J. 2011, 47, 703–710. [Google Scholar] [CrossRef] [PubMed]
| Variables | Aerobic N = 24 (63.2%) | Postural N = 14 (36.8%) | p * |
|---|---|---|---|
| Age, mean ± SE | 39.3 ± 2.55 | 43.78 ± 2.33 | 0.245 |
| Gender Male, n (%) | 20 (83.3) | 12 (85.7) | 0.999 |
| Basic education, n (%) | 24 (100) | 14(100) | 1.000 |
| Single marital status, n (%) | 23 (95.8) | 14(100) | 0.999 |
| Smoker, n (%) | 7 (29.2) | 7(50) | 0.298 |
| Height pre, mean ± SE | 1.68 ± 0.01 | 1.70 ± 0.27 | 0.378 |
| Weight pre, mean ± SE | 89.4 ± 4.99 | 74.13 ± 5.07 | 0.053 |
| BMI pre, mean ± SE | 31.6 ± 1.72 | 25.15 ± 1.36 | 0.014 |
| Chronicity > 7 years, n (%) | 20 (83.3) | 14 (100) | 0.276 |
| Hospitalization (median, minimum and maximum) | 2 (0 and 20) | 1 (0 and 5) | 0.120 |
| Flexibility pre, mean ± SE | 16.4 ± 1.71 | 18 ± 3.38 | 0.644 |
| Aerobic N = 24 | Postural N = 14 | p * API | p * PPI | p * Interaction | |||
|---|---|---|---|---|---|---|---|
| SF-36 | Pre | Post | Pre | Post | |||
| Functional capacity | 72.50 (0–100) | 85 (40–100) | 77.50 (0–95) | 75 (30–100) | 0.004 | 0.630 | 0.187 |
| Physical limitation | 37.50 (0–100) | 50 (0–100) | 12.50 (0–100) | 75 (0–100) | 0.455 | 0.016 | 0.211 |
| Pain | 72.00 (20–100) | 71 (0–100) | 55.50 (11–100) | 82 (50–100) | 0.520 | 0.006 | 0.013 |
| General health | 46.00 (10–87) | 54.50 (15–100) | 54.50 (30–87) | 65 (15–92) | 0.209 | 0.502 | 0.819 |
| Vitality | 60.00 (0–95) | 65 (15–100) | 60.00 (20–85) | 62.50 (10–100) | 0.354 | 0.485 | 0.825 |
| Social aspects | 50.00 (0–100) | 68.50 (37–100) | 63.75 (0–100) | 75 (0–100) | 0.132 | 0.315 | 0.952 |
| Emotional limitations | 16.50 (0–100) | 83 (0–100) | 0.00 (0–100) | 100 (0–100) | 0.063 | 0.033 | 0.638 |
| Mental health | 76.00 (0–100) | 68 (8–100) | 62.00 (0–100) | 74 (28–96) | 0.778 | 0.566 | 0.728 |
| SIMPAQ | |||||||
| Time in bed | 600 (420–840) | 570 (420–750) | 660 (330–945) | 600 (520–840) | 0.467 | 0.040 | 0.246 |
| Sedentary time | 375 (60–660) | 2 (120–780) | 155 (0–780) | 210 (0–540) | 0.905 | 0.151 | 0.486 |
| Time walking | 75 (0–840) | 115 (0–1260) | 55 (0–780) | 120 (0–800) | 0.383 | < 0.001 | 0.051 |
| Exercising | 0 (0–180) | 80 (80–680) | 0 (0–0) | 120 (0–210) | < 0.001 | < 0.001 | 0.032 |
| Other Activities | 0 (0–360) | 0 (0–300) | 0 (0–60) | 0 (0–90) | 0.809 | 0.237 | 0.781 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szortyka, M.F.; Cristiano, V.B.; Belmonte-de-Abreu, P. Aerobic and Postural Strength Exercise Benefits in People with Schizophrenia. Int. J. Environ. Res. Public Health 2023, 20, 3421. https://doi.org/10.3390/ijerph20043421
Szortyka MF, Cristiano VB, Belmonte-de-Abreu P. Aerobic and Postural Strength Exercise Benefits in People with Schizophrenia. International Journal of Environmental Research and Public Health. 2023; 20(4):3421. https://doi.org/10.3390/ijerph20043421
Chicago/Turabian StyleSzortyka, Michele Fonseca, Viviane Batista Cristiano, and Paulo Belmonte-de-Abreu. 2023. "Aerobic and Postural Strength Exercise Benefits in People with Schizophrenia" International Journal of Environmental Research and Public Health 20, no. 4: 3421. https://doi.org/10.3390/ijerph20043421
APA StyleSzortyka, M. F., Cristiano, V. B., & Belmonte-de-Abreu, P. (2023). Aerobic and Postural Strength Exercise Benefits in People with Schizophrenia. International Journal of Environmental Research and Public Health, 20(4), 3421. https://doi.org/10.3390/ijerph20043421






