Abstract
Addressing the field of health and safety at work, the primary objective of the present systematic review was to analyze the organizational risk factors for aircrew health according to professional category (flight attendants and pilots/co-pilots) and their consequences. The secondary objective was to identify the countries in which studies were carried out, focusing on the quality of content of the publications. The Medline/Pubmed, Cochrane, Web of Science, and Scopus databases were searched for eligible studies according to PRISMA statements. The risk of bias and the methodological quality of the studies were assessed using the Newcastle-Ottawa scale and Loney tools. Of the 3230 abstracts of articles screened, 36 studies met the inclusion criteria. Most of the research conducted on risk factors for the work organization of aircrew was carried out in the United States and the European Union and had moderate or low-quality methodology and evidence. However, the findings are homogeneous and allow the most prevalent organizational risk factors for the health of aircrew to be determined, namely, high work demand, long hours, and night work. Consequently, the most pervasive health problems were sleep disturbances, mental health disorders, musculoskeletal disorders, and fatigue. Thus, the regulation of the aircrew profession must prioritize measures that minimize these risk factors to promote better health and sleep for these professionals and, consequently, to provide excellent safety for workers and passengers.
1. Introduction
In Brazil, the demand for studies on the working conditions of aircrew and risks they are exposed to during work shifts has been growing in recent years. These demands stem from associations and organizations representing aviation professionals, as well as from airlines and government seeking to determine the impact on the social security system. Hence, these three dimensions intrinsically involve the regulatory framework governing the aviation industry and, consequently, related public policies.
In recent years, the civil aviation sector has grown significantly. According to the Brazilian Civil Aviation Agency (ANAC), in 2019, a record number of passengers (119.4 million) were carried on commercial flights in the country [1]. However, this high work demand, together with changes in flight schedules, stress, and psychological pressure, can cause fatigue, directly affecting the health of aircrew (Melo and Silvany Neto, 2012). This situation has given rise to a number of issues, such as instability, intense work pace, long working hours, irregular working hours, reduced pay, and loss of control over job activities [2,3].
Previous studies by Goode [4], Powell et al. [5], Marqueze et al. [6], Goffeng et al. [7], and Pellegrino and Marqueze [8] have highlighted that organizational aspects, such as long working hours, work demands, and schedules, numbered among the main risk factors for aircrew health. However, no study was found in the literature that summarized the findings on risk factors for these professionals. A study that synthesizes the main risk factors and their consequences for the aircrew’s health will be important to be able to think about health polices for these workers, as well as to synthesize what we already know about the subject and what still needs to be researched. Therefore, the primary objective of the present systematic review was to analyze the organizational risk factors for the health of aircrew according to professional category (flight attendants and pilots/co-pilots), as well as their consequences. The secondary objective was to identify the countries in which studies were carried out, focusing on the quality of content of publications.
2. Materials and Methods
A systematic review was performed according to the guidelines of the PRISMA checklist (Preferred Reporting Items for Systematic Reviews and Meta-analyses) [9] available in the Supplementary Materials (Table S1) and registered on PROSPERO under number 240012. Given this was a review of the literature, approval by the Ethics Committee was not required.
The PICO strategy for non-clinical research was used to devise the research question (Table 1): what are the organizational risk factors for aircrew health? Pubmed, Cochrane, Web of Science, and Scopus databases were systematically searched from February to May 2021 to identify studies related to the research question.

Table 1.
PICO strategy for devising the research question.
Keywords were defined according to medical subject headings (MeSH) and are presented in Table 2. The references of each study retrieved were manually investigated to identify additional eligible studies.

Table 2.
Search terms on electronic databases.
Potentially relevant studies were selected by two independent reviewers based on the following inclusion criteria: (1) studies in Portuguese, English, and Spanish only; (2) full studies; (3) observational (cross-sectional, cohort, case-control) and intervention studies only; (4) articles published after 1990; (5) studies involving men and women from any age group; (6) studies whose objective was to assess occupational risks, analyze their impact on aircrew health, and describe ways of mitigating these factors; (7) peer-reviewed studies; (8) studies on commercial aviation only. Exclusion criteria included clinical trials, ecological studies, reviews, qualitative studies, studies of retired aircrew, studies with objectives different from those of the present review (off-topic), abstracts, technical reports, oral communications, letters to the editors, and studies of flight simulation.
Article selection was performed independently, in a double-blind fashion, by two reviewers who screened all titles and abstracts. Subsequently, both reviewers read the full papers that met the inclusion criteria. In the case of disagreement regarding the eligibility of studies, a third researcher was consulted to reach a consensus.
The researchers created an electronic synthesis form to extract data from the papers reviewed. Data extraction covered the following variables: authors, publication year, study design, sample, study aim, main results, and study limitations declared by the authors. Microsoft Office Excel 2021® was used to manage the selection of articles.
The risk of bias and methodological quality of studies involving human subjects were assessed using the Newcastle-Ottawa tools for cohort and case-control studies [10]; and Loney’s criteria [11] was used for cross-sectional studies. As described in the Newcastle-Ottawa scale, the methodological quality score of the cohort and case-control studies was calculated based on three components (range 0–9 points): (1) selection of groups (0–4); (2) quality of adjustment for confounders (0–2); and (3) ascertainment of exposure after outcome (0–3) [10]. Cross-sectional studies, in turn, were evaluated using the Loney criteria, (range 0–8 points), in which higher scores indicate superior methodological quality. This score is obtained from the eight questions making up the scale, and one or zero is assigned to each of the questions evaluated, according to the adequacy of the methods and presentation of the results [11].
3. Results
Application of the search strategy led to the retrieval of 3230 records, of which 1942 duplicates were removed. The remaining 1288 studies were screened based on title and abstract, of which 1223 were excluded for not meeting the inclusion criteria. Of the remaining 64 studies, 28 were excluded because they were not eligible, giving 36 studies for inclusion in the systematic review. Consensus was reached between the two reviewers on all articles selected (Figure 1).
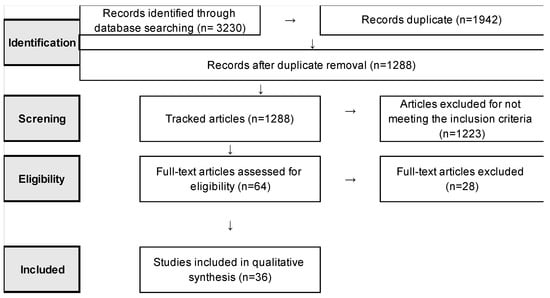
Figure 1.
Search and selection process according to PRISMA statement.
3.1. Study Characteristics
The place of origin of the publications reviewed is shown in Figure 2. Most of the studies were carried out in the United States (22.2%), followed by Germany (11.1%) and Sweden (11.1%). Brazilian studies accounted for 8.3% of the publications selected.
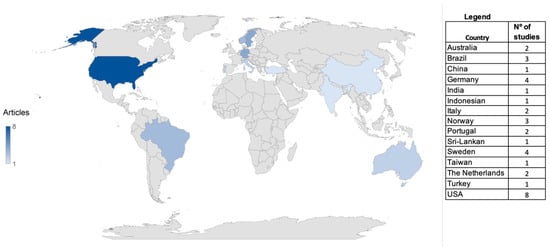
Figure 2.
Countries of publication of studies reviewed.
The studies involving flight attendants were conducted between 1998 and 2019, 25% of which were published in 2019 (Table 3). The studies involving pilots were carried out between 1997 and 2020, with 30.4% published in the last five years (Table 4). Lastly, studies involving both flight attendants and pilots were conducted over the period 2002–2021, 70% in the last five years (Table 5). Overall, 36.1% of the studies reviewed were published during the period spanning from 2017 to 2021.

Table 3.
Characteristics and main results of studies of flight attendants.

Table 4.
Characteristics and main results of studies of airline pilots.
The analysis of the results found in the studies involving flight attendants revealed that the main risk factors for work organization were high work demands (physical and psychological), harassment, and low job experience. The main consequences of these risk factors included sleep problems, cardiovascular diseases, mental health disorders, musculoskeletal disorders, injuries, and low work capacity (Table 3).
Lowden and Åkerstedt [12], in a prospective cohort study of cabin crew over a nine-day period, found that shorter rest time between work shifts (flights with quick layovers) led to decreased sleep time and efficiency. Sleep was not restorative, making it difficult to wake up and, consequently, increasing drowsiness during wakefulness. In the retrospective cohort study of Zeeb et al. [13], involving male cockpit crew members only, it was found that those who started working at age 30 or older had more than double the risk of cardiovascular mortality compared to professionals who entered the profession earlier. No risk gradient was observed for duration of employment (Table 3).
Ballard et al. [14], in a cross-sectional study of flight attendants, found that low job satisfaction and sexual harassment by passengers were risk factors for psychological distress. Lee et al. [15], also in a cross-sectional study involving flight attendants, identified both physical and mental work demands as risk factors for musculoskeletal disorders. Furthermore, in a cross-sectional study conducted by Castro et al. [16] investigating cabin crew members, the authors lack of humidity/moisture in the cabin, longer working experience, and being female were also risk factors for fatigue, poor sleep quality, and body aches. These factors, as well as their outcomes, can contribute to decreased work capacity (Table 3).
In a cross-sectional study by Hu et al. [17] of cabin crew, purser, and cabin manager, the authors confirmed that exhaustion from work, emotional distress, and insomnia were risk factors for decreased work ability. However, in a cross-sectional study of flight attendants conducted by Widyanti and Firdaus [18], a moderate mental workload was noted, regardless of flight duration. Lastly, Agampodi et al. [19], in a cross-sectional study of flight attendants, found that females (the predominant gender in this role), low weight (under 56 kg), and shorter work experience (<7 years) were risk factors for injuries on board (Table 3).
The most investigated topics among pilots were fatigue, drowsiness and alertness, which are frequent complaints among these professionals. In chronological order, the first study [20] with a prospective cohort design showed that long-haul flights, night flights, and short rest time between flights were associated with fatigue. In a cross-sectional study, Gander et al. [21] demonstrated that night flights, as well as short sleep duration, increased fatigue and decreased alertness levels led to poor eating habits, headaches, and backache among pilots. According to a cross-sectional study by Eriksen and Åkerstedt [22], night flights involve higher levels of sleepiness than morning flights for pilots (Table 4).
In a three-month prospective cohort study, Powell et al. [5] reported an association of long working hours and greater number of daily flights with a higher level of fatigue. Similarly, Roach et al. [23], in a prospective cohort, found that long working hours and sleep restriction increased fatigue and decreased level of attention among pilots. In a cross-sectional study carried out by Gander et al. [24], long working hours, with consequent sleep restriction on trans-meridional flights (crossing 7–9 time zones westwards), were also shown to affect pilots’ alertness level (Table 4).
In a cross-sectional study, Reis et al. [25] found that short-and medium-duration flights were factors associated with mental and physical fatigue among pilots. The authors explained this result as due to a large number of takeoffs and landings in shorter flights, events that demand the greatest attention and action of pilots. In a cross-sectional study by Gander et al. [26], the authors found that at top of descent (TOD—computed transition from cruise phase of flight to descent phase) and flights that lasted between 6:00 and 9:59 h led to most fatigue and impairment of pilots’ reaction time. Vejvoda et al. [27], in a cross-sectional study, also identified extended wakefulness and short-haul flights ending late at night as risk factors for fatigue (Table 4).
In a cross-sectional study, Van Drongelen et al. [28] showed that higher age, being an evening type, disturbance of work and personal-life balance, more need for recovery from work, lower perceived health, less physical activity, and moderate alcohol consumption were risk factors for fatigue. Lastly, Arsintescu et al. [29], also in a cross-sectional study, observed that higher workload, short sleep, greater number of daily flights, and short flights were factors associated with fatigue and impairment of pilots’ reaction time (Table 4).
According to Goode [4], pilots’ long working hours are risk factors for work accidents. Working days that last approximately 10–12 h increase the risk of accidents by 66%, and days of 13 h or more were associated with a 4.62 times greater risk. Another major problem among pilots is unintentional sleep during flights. In a cross-sectional study by Marqueze et al. [6], the prevalence of unintentional sleep was almost 60% among the pilots assessed. The authors found that longer monthly flying hours, frequent technical delays, greater need for recovery after work, work ability below optimal, insufficient sleep, and excessive sleepiness during waking hours were risks factors for unintentional sleep (Table 4).
Fatigue resulting from these risk factors can lead to other problems among pilots, as demonstrated by O’Hagan et al. [30]. In a cross-sectional study conducted by these authors, high work-related fatigue, frequent sleep disturbances, and unintentional naps during work were associated with depression and anxiety. Other factors were also associated with mental problems in this professional category. Feijó et al. [31], for instance, in a cross-sectional study, identified high work demand and sedentary lifestyle as risk factors for common mental disorders among pilots. The cross-sectional study by Demerouti et al. [32], also established that high demand and effort at work are risk factors for burnout in the same population. In addition to these factors, Wu et al. [33], in a cross-sectional study, found that the use of sleeping pills and harassment at work were associated with depression among pilots (Table 4).
Another frequent complaint among pilots is musculoskeletal disorder. In a cross-sectional study, Lawson et al. [34] observed that long flights are predictive factors for neck pain. Moreover, in a cross-sectional study, Runeson-Broberg et al. [35] identified having a high work demand, being female, having low social support, and suffering from psychosocial stress as risk factors for musculoskeletal symptoms. Albermann et al. [36], in a cross-sectional study, identified a high prevalence of chronic low back pain among pilots (82.7%) and a significant association with low back pain in those who had a total flight time of more than 600 h in the previous 12 months (Table 4).
Another problem studied that affects pilots was metabolic disorders. In a prospective cohort study, Zhao et al. [37] showed that pilots aged 31–50 years had a high prevalence of dyslipidemia compared to the general male population in China. De Souza Palmeira and Marqueze [38] observed a high prevalence of overweight among pilots (53.7%). Longer night work hours, difficulty relaxing after work, short sleep duration, chronic diseases, and a sedentary lifestyle were associated with excess weight. These problems, according to Bhat et al. [39], can lead to the development of other diseases. The authors found a positive correlation between overweight and hypertension among pilots, especially in individuals aged 26–35 years (Table 4).
Based on the results obtained in the studies of pilots only, the main organizational risk factors for the health of aircrew were long working hours, night work, little rest time between workdays, sleep restriction, and long waking hours due to working hours, high number of daily flights, low social support, organizational stress, frequent technical delays, lack of work and personal life balance, high work demand, and long-haul flights. The main health outcomes of these factors were physical and mental fatigue, lower alertness, poor eating habits, headaches, muscle pain, injuries, mental disorders, metabolic problems, unintentional sleep, and excessive sleepiness (Table 4).
In studies of flight attendants and pilots, other health issues were investigated besides fatigue. Ballard et al. [40], in a retrospective cohort study evaluating the association of causes of death (malignant neoplasms, non-cancerous, non-injurious, and external causes) with job position and gender, found that males with longer working hours were at higher risk of leukemia, while flight attendants (female) were at higher risk of suicide. In the cross-sectional study of Omholt et al. [41], flight attendants had a higher prevalence of musculoskeletal symptoms, as well as psychological, gastrointestinal, and allergy complaints, compared to pilots. In total, 20% reported high stress levels, which were associated with these symptoms and complaints. Regarding restless legs syndrome (RLS), Düz et al. [42], in a cross-sectional study, found that the prevalence of RLS among pilots and flight attendants was similar to that of the general population, and that flying at high altitudes was not a risk factor for the syndrome (Table 5).
The studies by Goffeng et al. [43] and Åkerstedt et al. [44] evaluated both pilots and flight attendants. The first of these investigations, a seven-day prospective cohort study confirmed higher number of consecutive workdays (≥days), short sleep, less rest time between flights, and high workload as risk factors for greater cardiovascular effort among pilots and flight attendants. More specifically, Åkerstedt et al. [44], in a 14-day prospective cohort of flight attendants, found that long working hours, night work, short sleep, and very early flights were risk factors for fatigue in this group (Table 5).
In summary, these studies found that the main work organization risk factors for these professionals were longer work experience, consecutive working days, sleep restriction due to working hours, high work demand, long working hours, and very early flights. The main outcomes of these factors were the development of cardiovascular diseases, mental disorders, and fatigue (Table 5).

Table 5.
Characteristics and main results of studies involving both flight attendants and airline pilots.
Table 5.
Characteristics and main results of studies involving both flight attendants and airline pilots.
| Authors (Year) | Study Design | Sample | Aim | Main Results | Limitations Declared by the Authors |
|---|---|---|---|---|---|
| Pilots and Flight Attendants | |||||
| Ballard TJ, Lagorio S, De Santis M, De Angelis G, Santaquilani M, Caldora M, Verdecchia A (2002) | Cohort retrospective | An amount of 3022 male (28.6 years, 20.4–61.2 yrs) and six female cockpit crew members (29.9 years, 23.6–33.5 yrs); 3418 male (25.6 years, 18.8–60.1 yrs) and 3428 female cabin attendants (22.6 years, 18.9–59.7 yrs) | To evaluate the association between causes of death (malignant neoplasms, non-cancer, non-injury causes and external causes) according to position level and sex. | This study demonstrated reduced risks among Italian male cockpit crew members for all-causes and all-sites cancer mortality with respect to the reference population. Mortality from all cancers was less than expected for all categories (SMRs of 0.58 for male cockpit crew, 0.67 for male cabin attendants, and 0.90 for female cabin attendants). Among male flight personnel, the SMR for leukemia was somewhat elevated (SMR 1.73; 95% CI: 0.75–3.41) based on eight deaths, with a positive trend by length of employment (p = 0.046). Additionally, an excess of death by suicide was seen among female cabin attendants (SMR 3.38; 95% CI: 1.24–7.35). | The cohort was relatively young, with few deaths, resulting in imprecise risk estimates. This reduced the ability to identify associations between occupational exposures, including exposure to cosmic radiation, and mortality from cancer, if such an association exists. For persons exposed to 100 mSv of cosmic radiation over a lifetime career of flying at high altitudes, the overall excess lifetime cancer mortality risk due to cosmic radiation is very low, estimated at 0.5%, compared with a lifetime cancer mortality risk of 25% from all other possible causes. For breast cancer, the presumed relative risk is 1.04 for occupational exposure to cosmic radiation, a rate that is extremely difficult to detect in an epidemiologic study of moderate dimension such as this one. A second limitation of this study is related to the use of length of employment as a surrogate of absorbed radiation dose. To address the validity of various measures of exposure to cosmic radiation, a team of European researchers conducted a correlation study of four methods for estimating absorbed cosmic radiation, using flight data of German pilots. It was found that length of employment, although the least specific of the measures, did correlate somewhat with more precise methods of estimating dose. |
| Omholt ML, Tveito TH, Ihlebæk C (2017) | Cross-sectional study | An amount of 843 aircrew members: cockpit crew 28% (4% female, 46% 41–50 years; cabin crew 17% (75% female, 34% 31–40 years) | To investigate the relationships between work-related stress, self-efficacy and subjective health complaints (SHCs) in commercial aircrew in Norway and to explore differences between cockpit and cabin crew. | Tiredness, sleep problems, bloating, low back pain, headaches, and neck pain were the most prevalent SHCs. Cabin crew reported significantly higher numbers, prevalence and mean values for all SHCs compared with cockpit crew (p < 0.05). In total, 20% reported high stress levels. High levels of work-related stress were significantly associated with all SHC factors in both groups. Self-efficacy partly moderated the relationship between stress and psychological complaints in both cockpit and cabin crew, and for musculoskeletal complaints in cockpit crew. The model explained 23 and 32% of the variance in psychological complaints for cockpit and cabin crew, respectively. High levels of work-related stress were significantly associated with the level of musculoskeletal, psychological, gastrointestinal and allergic complaints. | One weakness was the low response rate, and as no data were available on how many aircrew were actually reached and invited and no information on the non-responders, possible selection bias cannot be ruled out. The prevalence values might therefore not exactly represent the general population of Norwegian aircrew members since an over-representation of healthy subjects in health surveys has been reported. Furthermore, there was no information on the frequency or duration of flights or on work schedules and had to rely on the information aircrew members gave on whether they currently worked on domestic, Scandinavian, European and/or intercontinental flights. Lastly, the cross-sectional design of the study precluded the drawing of any conclusions about any causal relationships. |
| Düz OA, Yilmaz NH, Olmuscelik O (2019) | Cross-sectional study | A total of 301 actively flying Turkish aircrew (192 pilots, 109 cabin crew)—37.4 yrs (24–63 yrs), 22.6% female—and 272 age- and sex-matched healthy subjects—39.0 yrs (23–63 yrs), 26.1% female | To explore the frequency of restless legs syndrome (RLS) in aircrew. | The impact of being at a high altitude on RLS is controversial. The RLS frequency in aircrew was 6.7%, which is similar to that of the normal population. It is considered that this similarity is due to modern technology which regulates and adjusts oxygen saturation and air pressure inside the aircraft throughout the flight. We can conclude flying at high altitude was not a risk factor for RLS. | One limitation of this study is daily sleep duration was measured subjectively by self-reporting of the participants; objectively measured sleep gives more information about the relationship between RLS and being an aircrew member. |
| Goffeng EM, Nordby KC, Tarvainen M, Järvelin-Pasanen S, Wagstaff A, Skare Ø, Lie JÁ (2019) | Cohort prospective (7 days) | An amount of 17 pilots (15 men; mean age 52 yrs, SD 12.3 yrs) and 41 cabin crewmembers (six men; mean age 40 yrs, SD 7.4 yrs) | To evaluate changes in heart rate variability (HRV) during an actual flight duty period and sleep, and with respect to work characteristics and breaks. | The results indicate higher levels of cardiovascular strain on the 4th compared to the 1st workday, most prominent among cabin crewmembers. In this group, there were indications of decreased cardiovascular strain by increasing duration of sleep, demonstrated by increased root mean square of successive differences (RMSSD) (B = 2.7, 95% CI 1.6, 3.8) and standard deviation of the normal beat-to-beat differences (SDNN) (B = 4.4, 95% CI 3.0, 5.7), and decreased low and high frequency ratio (LF/HF) (B = 20.2, 95% CI, 20.4, 20.01). Similarly, longer duration of breaks was associated with lower cardiovascular strain, indicated by increased RMSSD (B = 0.1, 95% CI 0.03, 0.1) and SDNN (B = 0.1, 95% CI 0.1, 0.1). Among pilots, increased LF/HF indicated higher cardiovascular strain in those who often or always reported of high workload (B = 4.3, 95% CI 2.3, 6.3; and B = 7.3, 95% CI 3.2, 11.4, respectively). | One limitation of the study was the small sample size, particularly the small pilot group, which reduced statistical power and thus the capacity to detect differences and trends observed at a borderline statistical significance. This was partly modified by the repeated-measurement design. Furthermore, the study population was not a random sample, which may have resulted in selection bias, and decreased the generalizability of the results. The skewed gender distribution within the group of cabin crewmembers and pilots in most airlines. Finally, although though the number of work hours was similar among all subjects, the exact times for check-in and check-out for duty varied, which may also have influenced the results. |
| Åkerstedt T, Klemets T, Karlsson D, Häbel H, Widman L, Sallinen M (2021) | Cohort prospective (7–14 days) | An amount of 106 aircrew, age (38.3 yrs, SD 8.6 yrs), 76% male, 84.2% flight deck and 7.2% cabin crew | To investigate the associations of schedule characteristics with fatigue and amount of sleep in the acute 24-h window, and as cumulative effects across the seven-day work period. | For the 24-h window (acute), all variables entered singly were significantly associated with fatigue. Duty time, block time, sectors, time from start and non-day duty types were all associated with increased fatigue, whereas amount of sleep was associated with decreased fatigue. When all variables were entered at the same time, sleep, non- daytime duties and duty time retained their significant regression. Block time, hours since start and number of sectors lost their explanatory power due to the influence of duty type and sleep. For the seven-day work period, the results indicate that the accumulation of early and very early duties was associated with increased fatigue, whereas accumulation of sleep was associated with decreasing fatigue. When accumulated sleep was entered into the regression, accumulated duty time, number of sectors, and block time became associated with increasing fatigue, and early duties lost their significant association. The results suggest that sleep, duty time, and early starts are important predictors of fatigue in the 24-h window and that the number of very early starts and short sleep have cumulative effects on fatigue across a seven-day work period. | Among the limitations of the present study is that the dependent variable was based on self-report. Yet, there are no well established objective measures of fatigue usable in real-life work situations. The psychomotor vigilance test is a well established fatigue measure under controlled conditions (Lim and Dinges, 2008) [45], but it has never been validated against real work performance during a work shift and would take too long to carry out in a study with many (short) sectors. Another limitation is that some participants did not provide information on age and gender, probably due to concerns of anonymity. Another limitation is that no data were collected on bedtimes and times of rising, which would have made it possible to evaluate effects of time awake. A weakness is also that the study did not attract sufficient numbers of cabin crew to make a proper evaluation of that group. Finally, the results are only generalizable to daytime operations, albeit with a wide span of early and late flights. |
Notably, none of the studies included in this review researched ways of mitigating the risk factors investigated. The study authors only suggested measures to minimize health risks, including a reduction of consecutive workdays, especially night work, longer rest time between shifts, particularly after long-haul flights crossing time zones, provision of a suitable rest area on planes, optimizing the work by support team to shorten flight turnaround times, avoiding work schedules with very early starts, having greater social support at work, and prioritizing rest days on weekends.
3.2. Quality Assessment
The results of the quality assessment of the study designs according to the Newcastle-Ottawa or Loney criteria are given in Table 6. Out of the 36 articles reviewed, eight (22.2%) involved flight attendants only, 23 (63.9%) pilots only, and five evaluated both flight attendants and pilots (13.9%). Regarding the eight studies of flight attendants only, two (25%) were cohort studies, and six were cross-sectional (75%). Only one of the cross-sectional studies was rated with 7 points, i.e., of ‘high methodological quality’. Two studies were rated with five points, one with four points, and two studies were attributed a rating of 3 points, indicating that studies were predominantly of low methodological quality.

Table 6.
Risk of bias of studies assessed by Newcastle-Ottawa tool or Loney criteria, according to study design.
Regarding the studies of pilots only (n = 23), most were cross-sectional (n = 19, 82.6%). Of this total, four were rated with 6 points, indicating better quality. Eleven studies had a rating of 5, and two were attributed four points, indicating moderate quality. The remaining two studies scored only 3 points, i.e., were of low methodological quality. Only four publications were prospective cohort studies (17.4%), while none had a high level of evidence. Three of the studies had a moderate level of evidence, comprising two with 5 points and one with 4 points, while one had a low level of evidence (3 points) (Table 6).
For the three studies involving both flight attendants and pilots, most were cohort studies (two prospective and one retrospective—60%). Of these studies, two had moderate evidence (one with four points and another with five points), and only one study had low evidence. Of the two cross-sectional studies (40%), one scored five points, indicating moderate quality, and the other scored three points, indicating low quality (Table 6).
4. Discussion
The most prevalent organizational health risk factors faced by flight attendants and pilots were long hours, high work demand, and night work. These same risk factors are often found in other work activities also involving irregular hours and night shifts. An estimated 30% of the adult population are engaged in shiftwork, including night work [46]. According to the Working Time Society consensus statements, shift and night work are risk factors for workers’ health, as circadian desynchronization, sleep restriction, and social misalignment can cause health problems (directly or indirectly) as a result of exposure tonight work [47]. Shift and night work lead to acute and chronic disturbances in sleep and alertness, increased risk of fatigue-related accidents and incidents, cardiovascular problems, metabolic disorders, musculoskeletal disorders, increased risk of developing cancer (prostate, colorectal and breast), unhealthy behavioral changes, such as those related to timing of meals and low physical activity, and gastrointestinal and digestive disorders [46,47,48,49]. Moreover, mental health problems are common in shift workers. According to Boivin et al. [46], these conditions develop due to long-term exposure to work schedules, leading to the disruption of the sleep/wake cycle and circadian desynchronization, significant risk factors for mental health.
In a systematic analysis carried out jointly by the World Health Organization (WHO) and the International Labor Organization (ILO), individuals who work long hours have a higher risk of developing ischemic heart disease and stroke [50]. Other systematic reviews have also revealed that long working hours are associated with burnout syndrome [51], decline cognitive capacity [52], depression [53,54], increased alcohol consumption [55], mental health disorders [56], and adverse pregnancy outcomes (preterm birth, chance of miscarriage, low birth weight) [57]. High work demands related to working hours and shift and night-work are also associated with problems such as burnout and anxiety [58], musculoskeletal disorders [59], sleep disorders [60], emotional exhaustion [61], and sedentary lifestyle [62].
In the case of aircrew, in addition to hours spent in flight, commuting time, especially for professionals living far from their designated place of work or staying in hotels, should be taken into account. Hotels located far from airports will mean longer commutes to work. Furthermore, the authors note that, even when at work base, most airports are far from cities and require a long commuting time. Moreover, it is necessary to account for the time needed to carry out briefings and administrative activities, as well as the time engaged at the end of the workday, which ends not when the engines are shut off but when aircrew are at home to rest. Technical delays are also a factor that can extend work hours of aircrew and should thus be taken in account [6].
As a result of these risk factors, the most prevalent health problems reported in the studies analyzed were related to sleep, mental health disorders, musculoskeletal disorders, impaired cognition and performance, and fatigue. Sleepiness and impaired cognition and performance are common among airline pilots [63,64,65]. In a study by Bostock and Steptoe [66] of airline pilots, based on an analysis of salivary cortisol, the authors found a decrease in wake-up response time on shifts that started either very early or very late, directly impacting sleepiness and impaired cognition and performance. According to Kecklund and Axelsson [67] and Fischer et al. [68], shift work and its deleterious effects on workers’ sleep and concentration impair alertness levels and increase the risk of fatigue-related accidents.
As reported by Wingelaar-Jagt et al. [69], fatigue is related to several factors, including sleep debt, long wakefulness, circadian desynchronization and high workload, has several deleterious effects on health, and decreases aircrew performance during flight. Problems associated with fatigue in aircrew include decreased alertness, mental health problems, excessive sleepiness, sleep disturbances, and increased cardiovascular effort [8,43,70,71]. Although regulations limit flight time, it is noteworthy that fatigue cannot be mitigated entirely and the best way to avoid it is to obtain adequate sleep at night for recovery [69].
Wingelaar-Jagt et al. [69] identified some factors in aviation that contribute to fatigue, namely, long-haul flights, mainly as a result of jet lag, night flights, and circadian rhythm disturbances; short-haul flights, because of the high work demand and sleep loss for having to wake up very early to work or sleep late due to late flights; international flights; problems with work schedules, such as many consecutive nights of work, lack of a suitable rest area on the aircraft, and flight schedules, especially those starting very early or ending late at night; high number of flights; and long working hours, while taking into account, in addition to flight time, the time dedicated to briefings, administrative activities, etc.
Regarding the quality of the studies analyzed in the present review, most were cross-sectional (75%). In cross-sectional designs, a cause-and-effect relationship between risk factors and outcomes cannot be established, only indicating the existence of any associations between the variables studied [72]. However, these studies contribute significantly to the understanding of which organizational factors are associated with the health problems of aircrew, as well as helping identify the most frequent issues.
These data are important for designing and planning new studies, specifically longitudinal studies to elucidate the impact of work organization on the health of these workers and contribute to the management and care of these professionals. It is also essential to carry out dose-response studies to assess biological and behavioral factors that may impact individual susceptibility to the work schedules to which flight attendants and pilots are exposed, in addition to identifying mediating factors between risk factors and health outcomes. Social, economic, and legal aspects should be simultaneously considered and evaluated [45]. On the other hand, it is important to emphasize that most of the analyzed studies (86.1%) were classified as having moderate or low methodological and evidence quality, pointing to the need for more robust studies with fewer biases.
Finally, when considering the places where the studies were carried out, according to the Science and Engineering Indicators report [73], the United States and the European Union are the places that publish the most scientific studies in the worldwide, especially in the area of health. This same trend was also found in the present review, which analyzed studies conducted mainly in the United States, followed by Germany and Sweden.
This review contributes to the growing body of evidence suggesting that the work of aircrew has relevant risk factors which need to be better understood. Further studies, especially those with longitudinal designs, should be carried out to provide more robust evidence on organizational risk factors to the health of this group of professionals and to assess the actions and measures which could be taken to mitigate these risks.
5. Conclusions
In short, most of the research conducted on risk factors for the work organization of aircrew was carried out in the United States and the European Union and had moderate or low-quality methodology and evidence. The findings are homogeneous and allow the most prevalent organizational risk factors for the health of aircrew to be determined, namely, high work demand, long hours, and night work. As a result of these factors, the most prevalent health problems in both professional categories were those related to sleep, mental disorders, musculoskeletal disorders, and fatigue.
Our findings have interesting implications for gaining a better understanding of the main risk factors of aircrew health since this job is significant for society and guides future discussion about the regulation of the aircrew profession. The present review makes it clear that further studies with this professional category need to be carried out, especially longitudinal studies, to understand the causal relationships between occupational risk factors to health.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20043401/s1, Table S1: PRISMA checklist.
Author Contributions
Conceptualization, E.C.M., E.A.d.S.e.B., P.C.V.G. and C.A.S.; validation, E.C.M., E.A.d.S.e.B., A.C.R., M.S.G.F., R.C.R., P.C.V.G. and C.A.S.; investigation, E.C.M. and A.C.R.; resources, E.C.M. and A.C.R.; data curation, E.C.M. and A.C.R.; writing—original draft preparation, E.C.M.; writing—review and editing, E.C.M., E.A.d.S.e.B., A.C.R., M.S.G.F., R.C.R., P.C.V.G. and C.A.S.; visualization, E.C.M., E.A.d.S.e.B., A.C.R., M.S.G.F., R.C.R., P.C.V.G. and C.A.S.; supervision, C.A.S.; project administration, E.C.M., E.A.d.S.e.B., A.C.R., M.S.G.F., R.C.R., P.C.V.G. and C.A.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Transporte Aéreo—Sumário Executivo 2019. Brasília, 2020. Disponível em: Dados do Anuário do Transporte Aéreo—Português (Brasil). Available online: https://www.gov.br/anac/pt-br/assuntos/dados-e-estatisticas/mercado-de-transporte-aereo/anuario-do-transporte-aereo/dados-do-anuario-do-transporte-aereo (accessed on 10 March 2021).
- Caldwell, J.A. Fatigue in aviation. Travel Med. Infect. Dis. 2005, 3, 85–96. [Google Scholar] [CrossRef]
- Sack, R.L. Jet Lag. N. Engl. J. Med. 2010, 362, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Goode, J.H. Are pilots at risk of accidents due to fatigue? J. Saf. Res. 2003, 34, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Powell, D.M.C.; Spencer, M.B.; Holland, D.; Broadbent, E.; Petrie, K.J. Pilot fatigue in short-haul operations: Effects of number of sectors, duty length, and time of day. Aviat. Space Environ. Med. 2007, 78, 698–701. [Google Scholar]
- Marqueze, E.C.; Nicola, A.C.B.; Diniz, D.H.M.D.; Fischer, F.M. Working hours associated with unintentional sleep at work among airline pilots. Rev. Saude Publica 2017, 51, 61. [Google Scholar] [CrossRef]
- Goffeng, E.M.; Wagstaff, A.; Nordby, K.-C.; Meland, A.; Goffeng, L.O.; Skare, Ø.; Lilja, D.; Lie, J.-A.S. Risk of Fatigue Among Airline Crew During 4 Consecutive Days of Flight Duty. Erratum in Aerosp. Med. Hum. Perform. 2019, 90, 663. [Google Scholar] [CrossRef]
- Pellegrino, P.; Marqueze, E.C. Aspects of work and sleep associated with work ability in regular aviation pilots. Rev. Saude Publica 2019, 53, 16. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Rev. Esp. Cardiol. Engl. Ed. 2022, 75, 192. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses; The Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2013. [Google Scholar]
- Loney, P.L.; Chambers, L.W.; Bennett, K.J.; Roberts, J.G.; Stratford, P.W. Critical appraisal of the health research literature: Prevalence or incidence of a health problem. Chronic Dis. Can. 1998, 19, 170–176. [Google Scholar] [PubMed]
- Lowden, A.; Akerstedt, T. Sleep and wake patterns in aircrew on a 2-day layover on westward long distance flights. Aviat. Space Environ. Med. 1998, 69, 596–602. [Google Scholar]
- Zeeb, H.; Langner, I.; Blettner, M. Cardiovascular mortality of cockpit crew in Germany: Cohort study. Z Kardiol. 2003, 92, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Ballard, T.J.; Romito, P.; Lauria, L.; Vigiliano, V.; Caldora, M.; Mazzanti, C.; Verdecchia, A. Self perceived health and mental health among women flight attendants. Occup. Environ. Med. 2006, 63, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Wilbur, J.; Kim, M.J.; Miller, A.M. Psychosocial risk factors for work-related musculoskeletal disorders of the lower-back among long-haul international female flight attendants. J. Adv. Nurs. 2008, 61, 492–502. [Google Scholar] [CrossRef]
- Castro, M.; Carvalhais, J.; Teles, J. Irregular working hours and fatigue of cabin crew. Work 2015, 51, 505–511. [Google Scholar] [CrossRef]
- Hu, C.-J.; Hong, R.-M.; Yeh, G.-L.; Hsieh, I.-C. Insomnia, Work-Related Burnout, and Eating Habits Affecting the Work Ability of Flight Attendants. Aerosp. Med. Hum. Perform. 2019, 90, 601–605. [Google Scholar] [CrossRef]
- Widyanti, A.; Firdaus, M. Assessment of mental workload of flight attendants based on flight duration: An effort to provide safe working condition. Aviation 2020, 23, 97–103. [Google Scholar] [CrossRef]
- Agampodi, S.B.; Dharmaratne, S.D.; Agampodi, T.C. Incidence and predictors of onboard injuries among Sri Lankan flight attendants. BMC Public Health 2009, 9, 22. [Google Scholar] [CrossRef]
- Samel, A.; Wegmann, H.-M.; Vejvoda, M. Aircrew fatigue in long-Haul operations. Accid. Anal. Prev. 1997, 29, 439–452. [Google Scholar] [CrossRef]
- Gander, P.H.; Gregory, K.B.; Miller, D.L.; Graeber, R.C.; Connell, L.J.; Rosekind, M.R. Flight crew fatigue V: Long-haul air transport operations. Aviat. Space Environ. Med. 1998, 69, B37–B48. [Google Scholar]
- Eriksen, C.A.; Akerstedt, T. Aircrew fatigue in trans-Atlantic morning and evening flights. Chronobiol. Int. 2006, 23, 843–858. [Google Scholar] [CrossRef]
- Roach, G.D.; Petrilli, R.M.A.; Dawson, D.; Lamond, N. Impact of Layover Length on Sleep, Subjective Fatigue Levels, and Sustained Attention of Long-Haul Airline Pilots. Chronobiol. Int. 2012, 29, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Gander, P.; Berg, M.V.D.; Mulrine, H.; Signal, L.; Mangie, J. Circadian adaptation of airline pilots during extended duration operations between the USA and Asia. Chronobiol. Int. 2013, 30, 963–972. [Google Scholar] [CrossRef] [PubMed]
- Reis, C.; Mestre, C.; Canhão, H. Prevalence of Fatigue in a Group of Airline Pilots. Aviat. Space Environ. Med. 2013, 84, 828–833. [Google Scholar] [CrossRef] [PubMed]
- Gander, P.H.; Mulrine, H.M.; Berg, M.V.D.; Smith, A.A.T.; Signal, T.L.; Wu, L.J.; Belenky, G. Pilot Fatigue: Relationships with Departure and Arrival Times, Flight Duration, and Direction. Aviat. Space Environ. Med. 2014, 85, 833–840. [Google Scholar] [CrossRef]
- Vejvoda, M.; Elmenhorst, E.-M.; Pennig, S.; Plath, G.; Maass, H.; Tritschler, K.; Basner, M.; Aeschbach, D. Significance of time awake for predicting pilots’ fatigue on short-haul flights: Implications for flight duty time regulations. J. Sleep Res. 2014, 23, 564–567. [Google Scholar] [CrossRef]
- van Drongelen, A.; Boot, C.R.L.; Hlobil, H.; Smid, T.; van der Beek, A.J. Risk factors for fatigue among airline pilots. Int. Arch. Occup. Environ. Health 2016, 90, 39–47. [Google Scholar] [CrossRef]
- Arsintescu, L.; Chachad, R.; Gregory, K.B.; Mulligan, J.B.; Flynn-Evans, E.E. The relationship between workload, performance and fatigue in a short-haul airline. Chronobiol. Int. 2020, 37, 1492–1494. [Google Scholar] [CrossRef]
- O’Hagan, A.D.; Issartel, J.; Nevill, A.; Warrington, G. Flying into Depression. Work. Health Saf. 2016, 65, 109–117. [Google Scholar] [CrossRef]
- Feijó, D.; Câmara, V.M.; Luiz, R. Psychosocial aspects of work and common mental disorders among civil aviation pilots. Cad Saude Publica 2014, 30, 2433–2442. [Google Scholar] [CrossRef]
- Demerouti, E.; Veldhuis, W.; Coombes, C.; Hunter, R. Burnout among pilots: Psychosocial factors related to happiness and performance at simulator training. Ergonomics 2019, 62, 233–245. [Google Scholar] [CrossRef]
- Wu, A.C.; Donnelly-McLay, D.; Weisskopf, M.G.; McNeely, E.; Betancourt, T.S.; Allen, J.G. Correction to: Airplane pilot mental health and suicidal thoughts: A cross-sectional descriptive study via anonymous web-based survey. Environ. Health 2017, 16, 129. [Google Scholar] [CrossRef] [PubMed]
- Lawson, B.K.; Scott, O.; Egbulefu, F.J.; Ramos, R.; Jenne, J.W.; Anderson, E.R. Demographic and occupational predictors of neck pain in pilots: Analysis and multinational comparison. Aviat. Space Environ. Med. 2014, 85, 1185–1189. [Google Scholar] [CrossRef]
- Runeson-Broberg, R.; Lindgren, T.; Norbäck, D. Musculoskeletal symptoms and psychosocial work environment, among Swedish commercial pilots. Int. Arch. Occup. Environ. Health 2014, 87, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Albermann, M.; Lehmann, M.; Eiche, C.; Schmidt, J.; Prottengeier, J. Low Back Pain in Commercial Airline Pilots. Aerosp. Med. Hum. Perform. 2020, 91, 940–947. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Xiao, D.; Fan, X.; Ge, Z.; Wang, L.; Yan, T.; Wang, J.; Wei, Q.; Zhao, Y. Epidemiological Survey of Dyslipidemia in Civil Aviators in China from 2006 to 2011. Int. J. Endocrinol. 2014, 2014, 215076. [Google Scholar] [CrossRef]
- Palmeira, M.L.D.S.; Marqueze, E.C. Excess weight in regular aviation pilots associated with work and sleep characteristics. Sleep Sci. 2016, 9, 266–271. [Google Scholar] [CrossRef]
- Bhat, K.G.; Verma, N.; Pant, P.; Marwaha, M.P.S. Hypertension and Obesity Among Civil Aviation Pilots. Aerosp. Med. Hum. Perform. 2019, 90, 703–708. [Google Scholar] [CrossRef]
- Ballard, T.J.; Lagorio, S.; De Santis, M.; De Angelis, G.; Santaquilani, M.; Caldora, M.; Verdecchia, A. A Retrospective Cohort Mortality Study of Italian Commercial Airline Cockpit Crew and Cabin Attendants, 1965–96. Int. J. Occup. Environ. Health 2002, 8, 87–96. [Google Scholar] [CrossRef]
- Omholt, M.L.; Tveito, T.H.; Ihlebæk, C. Subjective health complaints, work-related stress and self-efficacy in Norwegian aircrew. Occup. Med. 2016, 67, 135–142. [Google Scholar] [CrossRef]
- Düz, O.A.; Yilmaz, N.H.; Olmuscelik, O. Restless Legs Syndrome in Aircrew. Aerosp. Med. Hum. Perform. 2019, 90, 934–937. [Google Scholar] [CrossRef]
- Goffeng, E.M.; Nordby, K.-C.; Tarvainen, M.; Järvelin-Pasanen, S.; Wagstaff, A.; Skare, A.; Lie, J.-A. Cardiac Autonomic Activity in Commercial Aircrew During an Actual Flight Duty Period. Aerosp. Med. Hum. Perform. 2019, 90, 945–952. [Google Scholar] [CrossRef]
- Åkerstedt, T.; Klemets, T.; Karlsson, D.; Häbel, H.; Widman, L.; Sallinen, M. Acute and cumulative effects of scheduling on aircrew fatigue in ultra-short-haul operations. J. Sleep Res. 2021, 30, e13305. [Google Scholar] [CrossRef]
- Lim, J.; Dinges, D.F. Sleep deprivation and vigilant attention. Ann. N. Y. Acad. Sci. 2008, 1129, 305–322. [Google Scholar] [CrossRef]
- Boivin, D.B.; Boudreau, P.; Kosmadopoulos, A. Disturbance of the Circadian System in Shift Work and Its Health Impact. J. Biol. Rhythm. 2022, 37, 3–28. [Google Scholar] [CrossRef] [PubMed]
- Moreno, C.R.C.; Marqueze, E.C.; Sargent, C.; Wright, K.P., Jr.; Ferguson, S.A.; Tucker, P. Working Time Society consensus statements: Evidence-based effects of shift work on physical and mental health. Ind. Health 2019, 57, 139–157. [Google Scholar] [CrossRef] [PubMed]
- Gupta, C.C.; Centofanti, S.; Dorrian, J.; Coates, A.M.; Stepien, J.M.; Kennaway, D.; Wittert, G.; Heilbronn, L.; Catcheside, P.; Noakes, M.; et al. Subjective Hunger, Gastric Upset, and Sleepiness in Response to Altered Meal Timing during Simulated Shiftwork. Nutrients 2019, 11, 1352. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer Night Shift Work. IARC Monographs on the Identification of Carcinogenic Hazards to Humans; World Health Organization: Geneva, Switzerland, 2020; Volume 124, 371p. [Google Scholar]
- Pega, F.; Náfrádi, B.; Momen, N.C.; Ujita, Y.; Streicher, K.N.; Prüss-Üstün, A.M.; Descatha, A.; Driscoll, T.; Fischer, F.M.; Godderis, L.; et al. Global, regional, and national burdens of ischemic heart disease and stroke attributable to exposure to long working hours for 194 countries, 2000–2016: A systematic analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021, 154, 106595. [Google Scholar] [CrossRef]
- Chong, M.Y.; Lin, S.H.; Lim, W.Y.; Ong, J.; Kam, P.C.; Ong, S.G. Burnout in anaesthesiology residentsresidents: A systematic review of its prevalence and stressors. Eur. J. Anaesthesiol. 2022, 39, 368–377. [Google Scholar] [CrossRef]
- Leso, V.; Fontana, L.; Caturano, A.; Vetrani, I.; Fedele, M.; Iavicoli, I. Impact of Shift Work and Long Working Hours on Worker Cognitive Functions: Current Evidence and Future Research Needs. Int. J. Environ. Res. Public Health 2021, 18, 6540. [Google Scholar] [CrossRef]
- Rugulies, R.; Sørensen, K.; Di Tecco, C.; Bonafede, M.; Rondinone, B.M.; Ahn, S.; Ando, E.; Ayuso-Mateos, J.L.; Cabello, M.; Descatha, A.; et al. The effect of exposure to long working hours on depression: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021, 155, 106629. [Google Scholar] [CrossRef]
- Niedhammer, I.; Bertrais, S.; Witt, K. Psychosocial work exposures and health outcomes: A meta-review of 72 literature reviews with meta-analysis. Scand. J. Work. Environ. Health 2021, 47, 489–508. [Google Scholar] [CrossRef]
- Pachito, D.V.; Pega, F.; Bakusic, J.; Boonen, E.; Clays, E.; Descatha, A.; Delvaux, E.; De Bacquer, D.; Koskenvuo, K.; Kröger, H.; et al. The effect of exposure to long working hours on alcohol consumption, risky drinking and alcohol use disorder: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021, 146, 106205. [Google Scholar] [CrossRef]
- Purba, A.K.; Demou, E. The relationship between organisational stressors and mental wellbeing within police officers: A systematic review. BMC Public Health 2019, 19, 563–576. [Google Scholar] [CrossRef]
- Cai, C.; Vandermeer, B.; Khurana, R.; Nerenberg, K.; Featherstone, R.; Sebastianski, M.; Davenport, M.H. The impact of occupational shift work and working hours during pregnancy on health outcomes: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2019, 221, 563–576. [Google Scholar] [CrossRef]
- Zhou, A.Y.; Panagioti, M.; Esmail, A.; Agius, R.; Van Tongeren, M.; Bower, P. Factors Associated with Burnout and Stress in Trainee Physicians: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e2013761. [Google Scholar] [CrossRef]
- Jacukowicz, A. Psychosocial work aspects, stress and musculoskeletal pain among musicians. A systematic review in search of correlates and predictors of playing-related pain. Work 2016, 54, 657–668. [Google Scholar] [CrossRef]
- Linton, S.J.; Kecklund, G.; Franklin, K.; Leissner, L.C.; Sivertsen, B.; Lindberg, E.; Svensson, A.C.; Hansson, S.O.; Sundin, Ö.; Hetta, J.; et al. The effect of the work environment on future sleep disturbances: A systematic review. Sleep Med. Rev. 2015, 23, 10–19. [Google Scholar] [CrossRef]
- Seidler, A.; Thinschmidt, M.; Deckert, S.; Then, F.; Hegewald, J.; Nieuwenhuijsen, K.; Riedel-Heller, S.G. The role of psychosocial working conditions on burnout and its core component emotional exhaustion—A systematic review. J. Occup. Med. Toxicol. 2014, 9, 10. [Google Scholar] [CrossRef]
- Kirk, M.A.; Rhodes, R.E. Occupation Correlates of Adults’ Participation in Leisure-Time Physical Activity: A Systematic Review. Am. J. Prev. Med. 2011, 40, 476–485. [Google Scholar] [CrossRef]
- Sallinen, M.; Sihvola, M.; Puttonen, S.; Ketola, K.; Tuori, A.; Härmä, M.; Kecklund, G.; Åkerstedt, T. Sleep, alertness and alertness management among commercial airline pilots on short-haul and long-haul flights. Accid. Anal. Prev. 2017, 98, 320–329. [Google Scholar] [CrossRef]
- Aljurf, T.M.; Olaish, A.H.; BaHammam, A.S. Assessment of sleepiness, fatigue, and depression among Gulf Cooperation Council commercial airline pilots. Sleep Breath. 2018, 22, 411–419. [Google Scholar] [CrossRef]
- Sallinen, M.; Pylkkönen, M.; Puttonen, S.; Sihvola, M.; Åkerstedt, T. Are long-haul truck drivers unusually alert? A comparison with long-haul airline pilots. Accid. Anal. Prev. 2020, 137, 105442. [Google Scholar] [CrossRef]
- Bostock, S.; Steptoe, A. Influences of early shift work on the diurnal cortisol rhythm, mood and sleep: Within-subject variation in male airline pilots. Psychoneuroendocrinology 2013, 38, 533–541. [Google Scholar] [CrossRef]
- Kecklund, G.; Axelsson, J. Health consequences of shift work and insufficient sleep. BMJ 2016, 355, i5210. [Google Scholar] [CrossRef]
- Fischer, D.; Lombardi, D.A.; Folkard, S.; Willetts, J.; Christiani, D.C. Updating the “Risk Index”: A systematic review and meta-analysis of occupational injuries and work schedule characteristics. Chronobiol. Int. 2017, 34, 1423–1438. [Google Scholar] [CrossRef]
- Wingelaar-Jagt, Y.Q.; Wingelaar, T.T.; Riedel, W.J.; Ramaekers, J.G. Fatigue in Aviation: Safety Risks, Preventive Strategies and Pharmacological Interventions. Front. Physiol. 2021, 12, 712628. [Google Scholar] [CrossRef]
- Pasha, T.; Stokes, P.R.A. Reflecting on the Germanwings Disaster: A Systematic Review of Depression and Suicide in Commercial Airline Pilots. Front. Psychiatry 2018, 9, 86. [Google Scholar] [CrossRef]
- O’Hagan, A.D.; Issartel, J.; McGinley, E.; Warrington, G. A Pilot Study Exploring the Effects of Sleep Deprivation on Analogue Measures of Pilot Competencies. Aerosp. Med. Hum. Perform. 2018, 89, 609–615. [Google Scholar] [CrossRef]
- Gordis, L. Epidemiology, 5th ed.; Elsevier Saunders: Philadelphia, PA, USA, 2014. [Google Scholar]
- White, K. Publications Output: U.S. Trends and International Comparisons. National Science Board, Science and Engineering Indicators. Available online: https://ncses.nsf.gov/pubs/nsb20206/executive-summary (accessed on 15 January 2022).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).