Management of Non-Communicable Diseases in Kosovo: A Scoping Review
Abstract
1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Information Sources, Search Strategy, and Eligibility Criteria
2.3. Selection of Sources of Evidence and Data Extraction
2.4. Critical Appraisal of Evidence
2.5. Synthesis of Results
3. Results
3.1. Selection of Sources of Evidence
3.2. Characteristics of Sources of Evidence
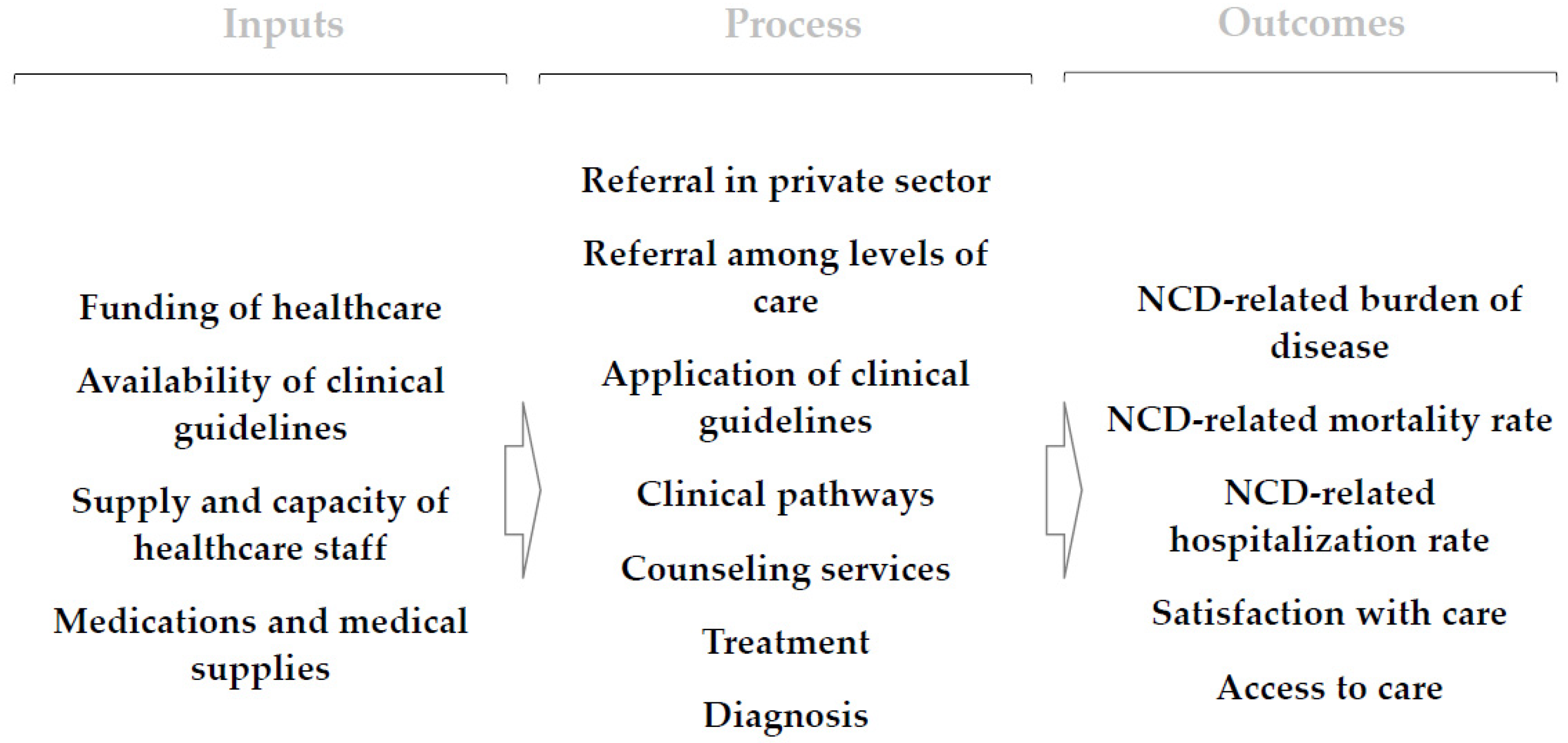
3.3. Inputs for NCDs Management
3.4. Management of NCDs
3.5. Outcomes from the Management of NCDs
4. Discussion
4.1. Summary of Findings
4.2. Strengths and Weaknesses
4.3. Context
4.4. Implications for Policy, Practice, and Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The World Bank. Policy Note on Kosovo Health Financing; World Bank: Prishtina, Kosovo, 2019. [Google Scholar]
- Country Context. Available online: https://www.worldbank.org/en/country/kosovo/overview (accessed on 6 April 2020).
- Ministria e Shndetësisë. Strategjia Sektoriale e Shëndetësisë 2017–2021; Ministria e Shndetësisë, Qeveria e Kosovës: Prishtina, Kosovo, 2016. [Google Scholar]
- Sofia Stanculescu, M.; Neculau, G.; Atanasov, P.; Benkovic, V.; Bjelovic, M.; Goldstein, J.; Hoxha, I.; Ljaljevic, A.; Mitevska, L.; Mecineanu, A. The Performance of Public Health-Care Systems in South-East Europe; Friedrich Ebert Stiftung Belgrade: Prishtina, Kosovo, 2014. [Google Scholar]
- Oncology Clinic. Available online: www.shskuk.rks-gov.net (accessed on 13 May 2021).
- Islami, D.A. Breast Cancer. Our Data and Challenges. In In Proceedings of the 1st Pan-Albanian Conference on Breast Cancer, Prishtina, Kosovo, 25 October 2019. [Google Scholar]
- Hoxha, I.; Fejza, A.; Malushaj, I.; Lumi, D.; Gashi, M.; Husaj, I.; Qarkaxhiu, L.; Gola, L. Policy Brief 1—Diagnosis and The Gravity of Diabetes in Kosovo; Solidar Suisse: Prishtina, Kosovo, 2015. [Google Scholar]
- Raunio, E.; Engel, R.; Fejza, A.; Telaku, M.; Hoxha, I. Policy Brief 9—Nutrition and Life Choices in The Roma, Ashkali and Egyptian Communities; Solidar Suisse: Prishtina, Kosovo, 2015. [Google Scholar]
- Telaku, M.; Engel, R.; Raunio, E.; Perry, J.; Rashiti, A.; Fejza, A.; Hoxha, I. New National Health Insurance will Save Lives: Life Expectancy and Health in Kosovo’s Roma, Ashkali and Egyptian Communities; Solidar Suisse: Prishtina, Kosovo; Balkan Sunflowers Kosova: Prishtina, Kosovo, 2015. [Google Scholar]
- Hoxha, I.; Muhaxheri, E.; Berisha, V. A Proposal for a Health Insurance Plan: How Does It Affect Us? Solidar Suisse: Prishtina, Kosovo, 2012. [Google Scholar]
- Marusic, D.; Ademi-Osmani, A.; Hoxha, I.; Ceglar, J. Situation Analysis at Kosovo Hospital and University Clinical Services; Lux Development: Prishtina, Kosovo, 2017. [Google Scholar]
- Hoxha, I.; Shaipi, K. Analizë Krahasmitare E Skemave Të Sigurimit Shëndetësor Në EJL; Friedrich Ebert Stiftung: Prishtina, Kosovo, 2009. [Google Scholar]
- Lee-Kwan, S.H.; Gittelsohn, J.; Hoxha, I.; Berisha, V.; Basha, V. Kosovo Poverty Social Impact Analysis: Report of a Qualitative Study of Stakeholder Perceptions of Potential Health Insurance Reforms and Cost-Sharing Strategies; Johns Hopkins Bloomberg School of Public Health: Prishtina, Kosovo, 2013. [Google Scholar]
- Schneider, P.; Langenbrunner, J.; Cho, J.; Kelmendi, F.; Tep, S.; Lebedeva, V. Kosovo Health Financing Reform Study; World Bank: Prishtina, Kosovo, 2008. [Google Scholar]
- Hoxha, I.; Duraj, B.; Xharra, S.; Avdaj, A.; Beqiri, V.; Grezda, K.; Selmani, E.; Avdiu, B.; Cegllar, J.; Marušič, D.; et al. Clinical Decision-Making for Appendectomy in Kosovo: A Conjoint Analysis. Int. J. Environ. Res. Public Health 2022, 19, 4027. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid. Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Sucharew, H.; Macaluso, M. Progress Notes: Methods for Research Evidence Synthesis: The Scoping Review Approach. J. Hosp. Med. 2019, 14, 416–418. [Google Scholar] [CrossRef]
- Lucas, P.J.; Baird, J.; Arai, L.; Law, C.; Roberts, H.M. Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med. Res. Methodol. 2007, 7, 4. [Google Scholar] [CrossRef]
- Barbullushi, M.; Elezi, Y.; Idrizi, A. Kosovo 2002: The epidemiology of renal disease and the impact of 1999 Kosovo war on end-stage renal disease patients. Nephrol. Dial. Transplant. 2002, 17, 2275–2276. [Google Scholar] [CrossRef]
- Haxhikadrija, A.; Voncina, L.; Hantchel, D. Reproductive Health Services in Kosovo: An Investment with Long Term Benefits; UNFPA: Mitrovica, Kosovo, 2008. [Google Scholar]
- Knowles, S.; Parker, M. Female Genital Cancer in Kosovo: A Situational analysis of breast and cervical cancer; UNFPA: Mitrovica, Kosovo, 2008. [Google Scholar]
- The World Bank. Kosovo Health Financing Reform Study; World Bank: Prishtina, Kosovo, 2008. [Google Scholar]
- Ajvazi, H.; Goranci, I.; Goranci, A.; Govori, V.; Goranci, D. Results of laser treatment-PRP to the diabetic retinopathy. Oftalmologia 2009, 53, 74–78. [Google Scholar]
- Balkan Investigative Reporting Network. Report on Kosovo’s Healthcare System; Balkan Investigative Reporting Network (BIRN): Prishtina, Kosovo, 2009. [Google Scholar]
- Devolli-Disha, E.; Manxhuka-Kerliu, S.; Ymeri, H.; Kutllovci, A. Comparative accuracy of mammography and ultrasound in women with breast symptoms according to age and breast density. Bosn. J. Basic Med. Sci. 2009, 9, 131–136. [Google Scholar] [CrossRef]
- FRIDOM Project. Vertical Functional Review of the Kosovo Ministry of Health; FRIDOM Project: Prishtina, Kosovo, 2009. [Google Scholar]
- Burkle, F.M., Jr. Post-conflict health system recovery: The case of Kosovo. Prehospital Disaster Med. 2010, 25, 34–36. [Google Scholar] [CrossRef]
- Percival, V.; Sondorp, E. A case study of health sector reform in Kosovo. Confl. Health 2010, 4, 7. [Google Scholar] [CrossRef]
- Bakalli, A.; Kocinaj, D.; Bakalli, A.; Krasniqi, A. Relationship of hypertensive retinopathy to thoracic aortic atherosclerosis in patients with severe arterial hypertension. Clin. Exp. Hypertens. 2011, 33, 89–94. [Google Scholar] [CrossRef]
- Begolli, I.; Arënliu-Qosaj, F. Public Health System Reform; Forum 2015: Prishtina, Kosovo, 2011. [Google Scholar]
- Bielecka-Dabrowa, A.; Aronow, W.S.; Rysz, J.; Banach, M. The Rise and Fall of Hypertension: Lessons Learned from Eastern Europe. Curr. Cardiovasc. Risk Rep. 2011, 5, 174–179. [Google Scholar] [CrossRef]
- Daullxhiu, I.; Haliti, E.; Poniku, A.; Ahmeti, A.; Hyseni, V.; Olloni, R.; Vela, Z.; Elezi, S.; Bajraktari, G.; Daullxhiu, T. Predictors of exercise capacity in patients with chronic heart failure. J. Cardiovasc. Med. 2011, 12, 223–225. [Google Scholar] [CrossRef]
- Health for All. Improving Health of Roma, Ashkali and Egyptian Comunities in Fushë Kosovë; Health for All: Prishtina, Kosovo, 2011. [Google Scholar]
- O’Hanlon, K.P.; Budosan, B. Post-disaster recovery: A case study of human resource deployment in the health sector in post-conflict Kosovo. Prehospital Disaster Med. 2011, 26, 7–14. [Google Scholar] [CrossRef]
- BIRN. Public Health Monitoring Report 2011; Balkan Investigative Reporting Network (BIRN): Prishtina, Kosovo, 2012. [Google Scholar]
- Luta, X.; Draebel, T. Kosovo-Serbs’ experiences of seeking healthcare in a post-conflict and ethnically segregated health system. Int. J. Public Health 2013, 58, 377–383. [Google Scholar] [CrossRef]
- Lux Dev. Capacity Building Within the MoH for Implementation of Healthcare Reforms; Lux Dev: Prishtina, Kosovo, 2011. [Google Scholar]
- Arifi, H.M.; Duci, S.B.; Zatriqi, V.K.; Ahmeti, H.R.; Ismajli, V.H.; Gashi, M.M.; Zejnullahu, Y.M.; Mekaj, A.Y. A retrospective study of 22 patients with necrotising fasciitis treated at the University Clinical Center of Kosovo (2005–2010). Int. Wound J. 2013, 10, 461–465. [Google Scholar] [CrossRef]
- Lee-Kwan, S.H.; Gittelsohn, J. Kosovo Poverty Social Impact Analysis: Report of a Qualitative Study of Stakeholder Perceptions of Potential Health Insurance Reforms and Cost-Sharing Strategies; World Bank: Prishtina, Kosovo, 2013. [Google Scholar]
- Hoxha, I. The Performance of Public Health Care System in South-Eastern Europe; Friedrich Ebert Stiftung: Prishtina, Kosovo, 2013. [Google Scholar]
- Balidemaj, A.; Balidemaj, F. Globalization and Health in Kosovo. Eur. J. Soc. Sci. Educ. Res. 2014, 1, 193–198. [Google Scholar] [CrossRef]
- Harvard University. Post-war Kosovo and Its Policies Towards the Roma, Ashkali, and Egyptian Communities; François-Xavier Bagnoud Center for Health and Human Rights: Boston, MA, USA; Harvard School of Public Health: Boston, MA, USA; Harvard University: Boston, MA, USA, 2014. [Google Scholar]
- Tahiri, Z.; Toci, E.; Rrumbullaku, L.; Hoti, K.; Roshi, E.; Burazeri, G. Patients’ evaluation of primary health care services in Gjilan region, Kosovo. J. Public Health 2014, 36, 161–169. [Google Scholar] [CrossRef]
- Uka, A. Understanding Informal Patient Payments in Kosovo’s Health Care System; Health Policy Institute: Bratislava, Slovakia, 2014. [Google Scholar]
- Vian, T. Corruption Risk Assessment in the Health Sector in Kosovo; UNDP: Prishtina, Kosovo; Swiss Agency for Development and Cooperation: Berne, Switzerland, 2014. [Google Scholar]
- Davies, P.; Ahmedi, E.; Berisha, M. Assessment to Characterise the Current Situation & Capacities for the Prevention & Control of Breast, Cervical & Prostate Cancers in Kosovo; Technical Report; UNFPA: Prishtina, Kosovo, 2015. [Google Scholar]
- Hoxha, I.; Fejza, A.; Malushaj, I.; Lumi, D.; Gashi, M.; Husaj, I.; Qarkaxhiu, L.; Gola, L. Policy Brief 3—Health Costs and Affordability among Diabetic Patients; Solidar Suisse: Prishtina, Kosovo, 2015. [Google Scholar]
- Hoxha, I.; Fejza, A.; Malushaj, I.; Lumi, D.; Gashi, M.; Husaj, I.; Qarkaxhiu, L.; Gola, L. Policy Brief 2—Access to a Specialized Health Care Workforce for Diabetic Patients; Solidar Suisse: Prishtina, Kosovo, 2015. [Google Scholar]
- Hoxha, I.; Zhubi, M.; Telaku, M. Barriers in Access to Primary Health Care among Vulnerable Citizens in Kosovo; Save The Children Kosovo: Prishtina, Kosovo, 2015. [Google Scholar]
- Raunio, E.; Engel, R.; Fejza, A.; Telaku, M.; Hoxha, I. Policy Brief 10—Kosovo Roma, Ashkali and Egyptian Access to and Use of Health Care Services; Solidar Suisse: Prishtina, Kosovo, 2015. [Google Scholar]
- Raunio, E.; Engel, R.; Fejza, A.; Telaku, M.; Hoxha, I. Policy Brief 11—Cost of The Future Health Insurance Plan and Financial Implications for Roma, Ashkali, and Egyptians in Kosovo; Solidar Suisse: Prishtina, Kosovo, 2015. [Google Scholar]
- Dixit, A.; Mishra, M.; Sandhu, M.; Delwiche, K.; Ajeti, R.; Goebbels, K.; Farnsworth, N. Barriers to Accessing Healthcare for Women and Men in Kosovo; The Kosova Women’s Network: Prishtina, Kosovo, 2016. [Google Scholar]
- Farnsworth, N.; Goebbels, K.; Ajeti, R. Access to Healthcare in Kosovo; The Kosova Women’s Network: Prishtina, Kosovo, 2016. [Google Scholar]
- Giordano, L.; Bisanti, L.; Salamina, G.; Ancelle Park, R.; Sancho-Garnier, H.; Espinas, J.; Berling, C.; Rennert, G.; Castagno, R.; Dotti, M.; et al. The EUROMED CANCER network: State-of-art of cancer screening programmes in non-EU Mediterranean countries. Eur. J. Public Health 2016, 26, 83–89. [Google Scholar] [CrossRef]
- Kantar TNS. Knowledge, Attitudes, Practices and Behavior: Non-Communicable Diseases, Child Health and Citizens’ Right to Health in Kosovo; Kantar TNS: Prishtina, Kosovo; Swiss Tropical and Public Health Institute: Allschwil, Switzerland, 2016. [Google Scholar]
- Moore, J.E.; Uka, S.; Vogel, J.P.; Timmings, C.; Rashid, S.; Gulmezoglu, A.M.; Straus, S.E. Navigating barriers: Two-year follow up on recommendations to improve the use of maternal health guidelines in Kosovo. BMC Public Health 2016, 16, 987. [Google Scholar] [CrossRef]
- Thompson, E.; Harding, A.L.; Pond, F.; Hammond, C.; Taylor, M. A Partnership to Improve Health Care in Kosovo: Dartmouth Medical School and Kosovar nurses worked together on a two-year project to rebuild primary health care in the postconflict city of Gjilan. Am. J. Nurs. 2006, 106, 72CC–72DD. [Google Scholar] [CrossRef]
- Ramadani, N.; Dedushi, K.; Mucaj, S.; Kabashi, S.; Jerliu, N.; Hoxhaj, A. The Frequency of Risk Factors on Trends of Pancreatic Cancer in Kosovo. Mater. Socio Med. 2016, 28, 108–111. [Google Scholar] [CrossRef] [PubMed]
- Primary Health Care in Kosovo. Quality of Care Study 2016; Accessible Quality Healthcare: Prishtina, Kosovo; Swiss Tropical and Public Health Institute: Allschwil, Switzerland; Save the Children Schweiz: Prishtina, Kosovo, 2016. [Google Scholar]
- Primary Health Care in Kosovo. Report on the Healthcare Management Survey in Kosovo; Accessible Quality Healthcare: Prishtina, Kosovo; Swiss Tropical and Public Health Institute: Allschwil, Switzerland; Save the Children: Prishtina, Kosovo, 2016. [Google Scholar]
- Hoxha, I.; Braha, M. Policy Brief 2: Problemi Me Shërbimin Spitalor Dhe Klinik Universitar Të Kosovës; Friedrich Ebert Stiftung: Prishtina, Kosovo; Center for Health Policy and Economics: Prishtina, Kosovo, 2017. [Google Scholar]
- Hoxha, I. Thematic Report—Health for “Luxembourg Initiative in Support of Civil Society in Kosovo”; Kosovo Civil Society Foundation: Prishtina, Kosovo, 2017. [Google Scholar]
- Hoxha, I.; Braha, M. Policy Brief 1: Propozimet Për Skemën E Sigurimeve Shëndetësore; Friedrich Ebert Stiftung: Prishtina, Kosovo; Center for Health Policy and Economics: Prishtina, Kosovo, 2017. [Google Scholar]
- Hoxha, I.; Fejza, A.; Murataj, N.; Syla, B.; Delija, B. Policy Brief 13—Family Physicians’ Perceptions and Preferences in Relation to Health Financing in Kosovo; Solidar Suisse: Prishtina, Kosovo, 2017. [Google Scholar]
- Hughes, J.D.; Wibowo, Y.; Sunderland, B.; Hoti, K. The role of the pharmacist in the management of type 2 diabetes: Current insights and future directions. Integr. Pharm. Res. Pract. 2017, 6, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Bajraktari, G.; Henein, M.Y. The uncertain/questionable prognostic value of exercise hypertension. J. Hypertens. Res. 2018, 75–78. [Google Scholar]
- Jakupi, A.; Godman, B.; Martin, A.; Haycox, A.; Baholli, I. Utilization and Expenditure of Anti-cancer Medicines in Kosovo: Findings and Implications. Pharm. Open 2018, 2, 423–432. [Google Scholar] [CrossRef] [PubMed]
- Zejnullahu Raci, P.; Hosnjak, L.; Poljak, M.; Lepej, S.Z.; Vince, A. Pre-vaccination prevalence of high-risk human papillomaviruses (HPV) in women from Kosovo and their related sociodemographic characteristics. Ginekol. Pol. 2018, 89, 485–494. [Google Scholar] [CrossRef]
- Bytyci, A.; Ymerhalili, G.; Dorner, T.E.; Stein, K.V.; Maxhera, O. Pilot study of an integrated care model using the geriatric assessment tool. Wien. Klin. Wochenschr. 2019, 131, 273–277. [Google Scholar] [CrossRef]
- Bytyqi-Damoni, A.; Kestane, A.; Taslimi, P.; Tuzun, B.; Zengin, M.; Bilgicli, H.G.; Gulcin, İ. Novel carvacrol based new oxypropanolamine derivatives: Design, synthesis, characterization, biological evaluation, and molecular docking studies. J. Mol. Struct. 2020, 1202. [Google Scholar] [CrossRef]
- Cuperjani, F.; Gashi, L.; Kurshumliu, F.; Dreshaj, S.; Selimi, F. Relationship between Ribosomal Protein S6-pS240 Expression and other Prognostic Factors in Non-Special Type Invasive Breast Cancer. Breast Care 2019, 14, 171–175. [Google Scholar] [CrossRef]
- World Health Organization. Primary health care in Kosovo: Rapid assessment; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2019. [Google Scholar]
- Ymerhalili, G.; Bytyci, A.; Maxhera, O.; Stein, V.; Dorner, T. Integrated care for older people in Kosovo. Int. J. Integr. Care 2019, 19, 226P. [Google Scholar] [CrossRef]
- Dimitrova, M.; Lakic, D.; Petrova, G.; Beslija, S.; Culig, J. Comparative analysis of the access to health-care services and breast cancer therapy in 10 Eastern European countries. SAGE Open Med. 2020, 8, 922029. [Google Scholar] [CrossRef]
- Eyvazzadeh, A.; Kumar, P.; Ramakrishna, N. Breast Cancer Prevention in Kosovo: Understanding Capacity Constraints and Identifying Policy Options for Prevention; Nelson A. Rockefeller Center For Public Policy and the Social Sciences, Dartmouth College: Hanover, NH, USA, 2021. [Google Scholar]
- Milosevic, J.; Milic, M.; Mirkovic, M.; Milosevic, N.; Novakovic, T.; Vitosevic, Z.; Djuric, S.; Stojanovic-Tasic, M.; Kulic, L. Association between non-communicable diseases and satisfaction with healthcare and self-rated health: Experiences from post-conflict communities. Srp. Arh. Za Celok. Lek. 2021, 149, 16–23. [Google Scholar] [CrossRef]
- Podvorica, E.; Bekteshi, T.; Oruqi, M.; Kalo, I. Education of the Patients Living with Heart Disease. Mater. Socio Med. 2021, 33, 10–15. [Google Scholar] [CrossRef]
- Katanolli, A.B.; Probst-Hensch, N.; Obas, K.A.; Gerold, J.; Zahorka, M.; Jerliu, N.; Ramadani, Q.; Fota, N.; Merten, S. Perceived barriers to physical activity behaviour among patients with diabetes and hypertension in Kosovo: A qualitative study. Bmc Prim. Care 2022, 23, 257. [Google Scholar] [CrossRef]
- Bytyci-Katanolli, A.; Merten, S.; Kwiatkowski, M.; Obas, K.; Gerold, J.; Zahorka, M.; Jerliu, N.; Ramadani, Q.; Fota, N.; Probst-Hensch, N. Non-communicable disease prevention in Kosovo: Quantitative and qualitative assessment of uptake and barriers of an intervention for healthier lifestyles in primary healthcare. BMC Health Serv. Res. 2022, 22, 647. [Google Scholar] [CrossRef]
- Ejupi, V.; Demiri, L.; Qazimi, B.; Dragusha, S. Study on current therapeutic management of breast cancer in hospital and university clinical service of Kosovo. Maced. Pharm. Bull. 2022, 68, 455–456. [Google Scholar] [CrossRef]
- Hoxha, I.; Islami, D.A.; Uwizeye, G.; Forbes, V.; Chamberlin, M.D. Forty-Five Years of Research and Progress in Breast Cancer: Progress for Some, Disparities for Most. JCO Glob. Oncol. 2022, 8, e2100424. [Google Scholar] [CrossRef]
- Hoxha, I.; Guda, B.; Hoti, A.; Zhubi, E.; Selmani, E.; Avdiu, B.; Cegllar, J.; Marušič, D.; Osmani, A. Clinical Decision-Making for Heart Failure in Kosovo: A Conjoint Analysis. Int. J. Environ. Res. Public Health 2022, 19, 4638. [Google Scholar] [CrossRef]
- Obas, K.A.; Bytyci-Katanolli, A.; Kwiatkowski, M.; Ramadani, Q.; Fota, N.; Jerliu, N.; Statovci, S.; Gerold, J.; Zahorka, M.; Probst-Hensch, N. Strengthening Primary Healthcare in Kosovo Requires Tailoring Primary, Secondary and Tertiary Prevention Interventions and Consideration of Mental Health. Front. Public Health 2022, 10, 794309. [Google Scholar] [CrossRef]
- Ministry of Health. Action Plan 2011–2014 for The Health Sector Strategy 2010–2014; Ministry of Health: Prishtina, Kosovo, 2010. [Google Scholar]
- Hoxha, I.; Fejza, A.; Aliu, M.; Juni, P.; Goodman, D.C. Health system factors and caesarean sections in Kosovo: A cross-sectional study. BMJ Open 2019, 9, e026702. [Google Scholar] [CrossRef] [PubMed]
- Collier, J.; Kienzler, H. Barriers to cardiovascular disease secondary prevention care in the West Bank, Palestine—A health professional perspective. Confl. Health 2018, 12, 27. [Google Scholar] [CrossRef] [PubMed]
- Murataj, N.; Syla, B.; Krasniqi, Y.; Bahtiri, S.; Bekaj, D.; Beqiri, P.; Hoxha, I.S. Migration Intent of Health Care Workers during the COVID-19 Pandemic in Kosovo. Int. J. Environ. Res. Public Health 2022, 19, 1122. [Google Scholar] [CrossRef] [PubMed]
- Gheorghe, A.; Griffiths, U.; Murphy, A.; Legido-Quigley, H.; Lamptey, P.; Perel, P. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: A systematic review. BMC Public Health 2018, 18, 975. [Google Scholar] [CrossRef] [PubMed]

| Author | Year | Type of Publication | Factors Influencing the Management of NCDs (Subthemes Reported) | Information on the Management of NCDs (Subthemes Reported) | Outcomes of Management of NCDs (Subthemes Reported) | NCDs Reported |
|---|---|---|---|---|---|---|
| Barbullushi et al. [21] | 2002 | Journal article | Treatment, clinical pathways, application of clinical guidelines | Overall | ||
| Haxhikadrija et al. [22] | 2008 | Journal article | NCD-related mortality rate | Breast cancer | ||
| Knowles et al. [23] | 2008 | Report | Supply and capacity of healthcare staff | Diagnosis, treatment, clinical pathways, application of clinical guidelines | NCD-related burden of disease | Breast cancer, cervical cancer |
| Schneider et al. [24] | 2008 | Report | Funding of healthcare | Referral in private sector | Overall | |
| Ajvazi et al. [25] | 2009 | Journal article | Availability of clinical guidelines | Diabetes | ||
| Balkan Investigative Reporting Network [26] | 2009 | Report | Medications and medical supplies | Referral in private sector | Overall | |
| Devolli-Disha et al. [27] | 2009 | Journal article | Diagnosis | Breast cancer | ||
| FRIDOM [28] | 2009 | Report | Medications and medical supplies, availability of clinical guidelines | Referral in private sector | Overall | |
| Burkle [29] | 2010 | Journal article | NCD-related mortality rate | Overall | ||
| Percival et al. [30] | 2010 | Journal article | NCD-related mortality rate | Overall | ||
| Bakalli et al. [31] | 2011 | Journal article | NCD-related mortality rate | Hypertension | ||
| Begolli et al. [32] | 2011 | Report | Diagnosis, referral among levels of care, referral in private sector | Overall | ||
| Bielecka-Dabrowa et al. [33] | 2011 | Journal article | Diagnosis, treatment, application of clinical guidelines | Hypertension | ||
| Daullxhiu et al. [34] | 2011 | Journal article | NCD-related mortality rate | Hypertension | ||
| Health for All [35] | 2011 | Report | Access to care | Overall | ||
| O’Hanlon et al. [36] | 2011 | Journal article | Supply and capacity of healthcare staff | Overall | ||
| Balkan Investigative Reporting Network [37] | 2012 | Report | Medications and medical supplies | Referral among levels of care | Overall, diabetes | |
| Luta et al. [38] | 2012 | Journal article | Access to care | Overall | ||
| Ministry of Health [39] | 2012 | Report | Diagnosis, treatment | Overall | ||
| Arifi et al. [40] | 2013 | Journal article | NCD-related mortality rate | Diabetes | ||
| Hee Lee-Kwan et al. [41] | 2013 | Report | Funding of healthcare | Referral in private sector | Overall | |
| Hoxha [42] | 2013 | Report | Medications and medical supplies, supply and capacity of healthcare staff, funding of healthcare | Treatment, counseling services | Satisfaction with care | Overall, diabetes, breast cancer, cervical cancer |
| Balidemaj et al. [43] | 2014 | Journal article | Supply and capacity of healthcare staff | Treatment | Overall | |
| Bhabha et al. [44] | 2014 | Report | Access to care | Overall | ||
| Tahiri et al. [45] | 2014 | Journal article | Satisfaction with care | Overall | ||
| Uka [46] | 2014 | Report | Funding of healthcare | Overall | ||
| Vian [47] | 2014 | Report | Medications and medical supplies, funding of healthcare | Overall, breast cancer, cervical cancer | ||
| Davies et al. [48] | 2015 | Report | Supply and capacity of healthcare staff, availability of clinical guidelines | Diagnosis, treatment, clinical pathways, application of clinical guidelines | Breast cancer, cervical cancer | |
| Hoxha et al. [49] | 2015 | Policy brief | Medications and medical supplies, funding of healthcare | Treatment, counseling services, referral in private sector | Diabetes | |
| Hoxha et al. [50] | 2015 | Policy brief | Treatment | Access to care, satisfaction with care | Diabetes | |
| Hoxha et al. [51] | 2015 | Report | Medications and medical supplies, funding of healthcare | Referral in private sector | Overall | |
| Raunio et al. [52] | 2015 | Policy brief | Funding of healthcare | Access to care | Overall | |
| Raunio et al. [53] | 2015 | Policy brief | Access to care | Overall | ||
| Dixit et al. [54] | 2016 | Report | Counseling services | Access to care | Breast cancer | |
| Farnsworth et al. [55] | 2016 | Report | Diagnosis | Access to care | Hypertension, breast cancer | |
| Giordano et al. [56] | 2016 | Journal article | Diagnosis | Breast cancer | ||
| Kantar TNS [57] | 2016 | Report | Availability of clinical guidelines | Treatment, referral in private sector | Diabetes, hypertension | |
| Moore et al. [58] | 2016 | Journal article | Availability of clinical guidelines | Overall | ||
| Thompson et al. [59] | 2016 | Journal article | Availability of clinical guidelines | Counseling services | Hypertension | |
| Ramadani et al. [60] | 2016 | Journal article | NCD-related mortality rate | Other | ||
| Zahorka et al. [61] | 2016 | Report | Diagnosis, treatment | Hypertension | ||
| Zahorka et al. [62] | 2016 | Report | Referral among levels of care | Overall | ||
| Hoxha et al. [63] | 2017 | Policy brief | Referral among levels of care | Overall | ||
| Hoxha [64] | 2017 | Report | Referral in private sector | Overall | ||
| Hoxha et al. [65] | 2017 | Policy brief | Funding of healthcare | Overall, diabetes | ||
| Hoxha et al. [66] | 2017 | Policy brief | Satisfaction with care | Overall | ||
| Hughes et al. [67] | 2017 | Journal article | Treatment, clinical pathways | Diabetes | ||
| Bajraktari et al. [68] | 2018 | Journal article | Treatment | NCD-related mortality rate | Hypertension | |
| Jakupi et al. [69] | 2018 | Journal article | Medications and medical supplies, funding of healthcare | Other | ||
| Zejnullahu-Raci et al. [70] | 2018 | Journal article | Diagnosis, treatment | NCD-related mortality rate | Cervical cancer | |
| Bytyci et al. [71] | 2019 | Journal article | Counseling services, clinical pathways | Diabetes | ||
| Bytyqi-Damoni et al. [72] | 2019 | Journal article | Treatment | Diabetes | ||
| Cuperjani et al. [73] | 2019 | Journal article | Treatment | Breast cancer | ||
| World Health Organization [74] | 2019 | Report | Availability of clinical guidelines | Application of clinical guidelines | NCD-related hospitalization rate | Diabetes, hypertension |
| Ymerhalili et al. [75] | 2019 | Journal article | Clinical pathways | Diabetes, hypertension | ||
| Dimitrova et al. [76] | 2020 | Journal article | Availability of clinical guidelines | Overall | ||
| Eyvazzadeh et al. [77] | 2021 | Report | Referral among levels of care | Overall, breast cancer | ||
| Milosevic et al. [78] | 2021 | Journal article | Satisfaction with care | Overall | ||
| Podvorica et al. [79] | 2021 | Journal article | Counseling services | Other | ||
| Bytyci Katanolli et al. [80] | 2022 | Journal article | Counseling services | Overall | ||
| Bytyci Katanolli et al. [81] | 2022 | Journal article | Counseling services | Overall | ||
| Ejupi et al. [82] | 2022 | Journal article | Counseling services, treatment | Breast cancer | ||
| Hoxha et al. [83] | 2022 | Journal article | Treatment | Breast cancer | ||
| Hoxha et al. [84] | 2022 | Journal article | Application of clinical guidelines | Other | ||
| Obas et al. [85] | 2022 | Journal article | Diagnosis, treatment | Diabetes, hypertension, other |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoxha, I.; Apuk, V.; Kryeziu, B.; Rashiti, P.; Aliu, M.; Aquines, A.G.; Khan, O.; Nguyen, H.T.H. Management of Non-Communicable Diseases in Kosovo: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 3299. https://doi.org/10.3390/ijerph20043299
Hoxha I, Apuk V, Kryeziu B, Rashiti P, Aliu M, Aquines AG, Khan O, Nguyen HTH. Management of Non-Communicable Diseases in Kosovo: A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(4):3299. https://doi.org/10.3390/ijerph20043299
Chicago/Turabian StyleHoxha, Ilir, Valid Apuk, Besfort Kryeziu, Premtim Rashiti, Mrika Aliu, Alejandro Gonzalez Aquines, Olga Khan, and Ha Thi Hong Nguyen. 2023. "Management of Non-Communicable Diseases in Kosovo: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 4: 3299. https://doi.org/10.3390/ijerph20043299
APA StyleHoxha, I., Apuk, V., Kryeziu, B., Rashiti, P., Aliu, M., Aquines, A. G., Khan, O., & Nguyen, H. T. H. (2023). Management of Non-Communicable Diseases in Kosovo: A Scoping Review. International Journal of Environmental Research and Public Health, 20(4), 3299. https://doi.org/10.3390/ijerph20043299






