Amazon Amandaba—Sociodemographic Factors, Health Literacy, Biochemical Parameters and Self-Care as Predictors in Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting and Period of Study
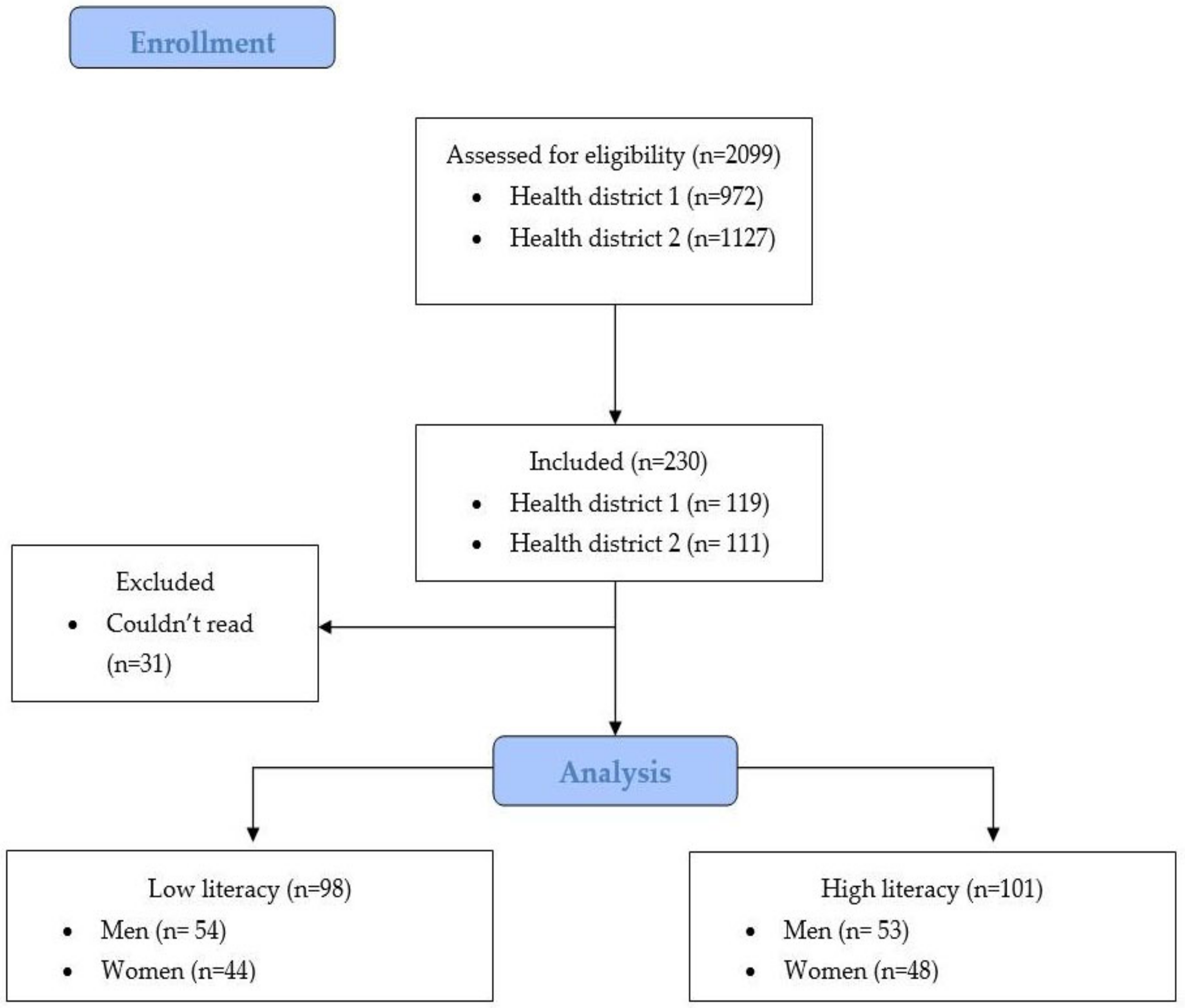
2.3. Population
2.4. Eligibility Criteria
2.5. Sampling
2.6. Sample
2.7. Data Collection and Variables
2.8. Primary Outcomes
2.9. Bias
2.10. Statistical Analysis
3. Results
3.1. Analysis of The Sociodemographic, Health-Related, and Clinical Characteristics between Groups
3.2. Sociodemographic Characteristics as Predictors of Health Literacy
3.3. Sociodemographic Characteristics and Health Literacy as Predictors of Biochemical Parameters
3.4. Health Literacy as Predictors of Self-Care
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Simonds, S.K. Health Education as Social Policy. Health Educ. Monogr. 1974, 2, 1–10. [Google Scholar] [CrossRef]
- Peerson, A.; Saunders, M. Health literacy revisited: What do we mean and why does it matter? Health Promot. Int. 2009, 24, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Adams, R.J.; Stocks, N.P.; Wilson, D.H.; Hill, C.L.; Gravier, S.; Kickbusch, I.; Beilby, J.J. Health literacy—A new concept for general practice? Aust. Fam. Physician 2009, 38, 144–147. [Google Scholar] [PubMed]
- Passamai, M.P.B.; Sampaio, H.A.C.; Dias, A.M.I.; Cabral, L.A. Functional health literacy: Reflections and concepts on its impact on the interaction among users, professionals and the health system. Interface-Comun. Saúde Educ. 2012, 16, 301–314. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. (HLS-EU) Consortium Health Literacy Project European. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef]
- Andrus, M.R.; Roth, M.T. Health Literacy: A Review. Pharmacotherapy 2002, 22, 282–302. [Google Scholar] [CrossRef]
- Burnett, N. Education for All: Literacy for Life; The United Nations Educational, Scientific and Cultural Organization Publishing: Paris, France, 2005. [Google Scholar]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. Available online: https://academic.oup.com/heapro/article/15/3/259/551108 (accessed on 20 March 2022). [CrossRef]
- DeWalt, D.A.; Berkman, N.D.; Sheridan, S.; Lohr, K.N.; Pignone, M.P. Literacy and health outcomes. J. Gen. Intern. Med. 2004, 19, 1228–1239. [Google Scholar] [CrossRef]
- Berkman, N.D.; Dewalt, D.A.; Pignone, M.P.; Sheridan, S.L.; Lohr, K.N.; Lux, L.; Sutto, S.F.; Swinson, T.; Bonito, A.J. Literacy and Health Outcomes: Summary; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2004. Available online: https://www.ncbi.nlm.nih.gov/books/NBK11942/ (accessed on 22 March 2022).
- Rudd, R.E. Health literacy skills of U.S. adults. Am. J. Health Behav. 2007, 31 (Suppl. 1), S8–S18. [Google Scholar] [CrossRef]
- Inoue, M.; Takahashi, M.; Kai, I. Impact of communicative and critical health literacy on understanding of diabetes care and self-efficacy in diabetes management: A cross-sectional study of primary care in Japan. BMC Fam. Pract. 2013, 14, 40. [Google Scholar] [CrossRef]
- Tomita, S.; Aoki, T.; Ohde, S.; Takahashi, O.; Kimura, T.; Matsushima, M. Association between health literacy and multimorbidity: A nationwide, cross-sectional study of a Japanese population. BMJ Open 2022, 12, e052731. [Google Scholar] [CrossRef]
- Carthery-Goulart, M.T.; Anghinah, R.; Areza-Fegyveres, R.; Bahia, V.S.; Brucki, S.M.D.; Damin, A.; Formigoni, A.P.; Frota, N.; Guariglia, C.; Jacinto, A.F.; et al. Performance of a Brazilian population on the test of functional health literacy in adults. Rev. Saúde Pública 2009, 43, 631–638. [Google Scholar] [CrossRef]
- Murphy, P.W.; Davis, T.C.; Long, S.W.; Jackson, R.H.; Decker, B.C. Rapid Estimate of Adult Literacy in Medicine (REALM): A Quick Reading Test for Patients. J. Read. 1993, 37, 124–130. [Google Scholar]
- Rowlands, G.; Khazaezadeh, N.; Oteng-Ntim, E.; Seed, P.; Barr, S.; Weiss, B.D. Development and validation of a measure of health literacy in the UK: The newest vital sign. BMC Public Health 2013, 13, 116. [Google Scholar] [CrossRef]
- Sørensen, K.; van den Broucke, S.; Pelikan, J.M.; Fullam, J.; Doyle, G.; Slonska, Z.; Kondilis, B.; Stoffels, V.; Osborne, R.H.; Brand, H. Measuring health literacy in populations: Illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health 2013, 13, 948. [Google Scholar] [CrossRef]
- Suka, M.; Odajima, T.; Kasai, M.; Igarashi, A.; Ishikawa, H.; Kusama, M.; Nakayama, T.; Sumitani, M.; Sugimori, H. The 14-item health literacy scale for Japanese adults (HLS-14). Environ. Health Prevent. Med. 2013, 18, 407–415. [Google Scholar] [CrossRef]
- Osborne, R.H.; Batterham, R.W.; Elsworth, G.R.; Hawkins, M.; Buchbinder, R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013, 13, 658. [Google Scholar] [CrossRef]
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021; Available online: https://www.diabetesatlas.org (accessed on 22 March 2022).
- Malta, D.C.; Ribeiro, E.G.; Gomes, C.S.; Alves, F.T.A.; Stopa, S.R.; Sardinha, L.M.V.; Pereira, C.A.; Duncan, B.B.; Schimidt, M.I. Indicadores da linha de cuidado de pessoas com diabetes no Brasil: Pesquisa Nacional de Saúde 2013 e 2019. Epidemiol. Serviços Saúde 2022, 31, e2021382. [Google Scholar] [CrossRef]
- Freund, A.; Johnson, S.B.; Silverstein, J.; Thomas, J. Assessing daily management of childhood diabetes using 24-hour recall interviews: Reliability and stability. Health Psychol. 1991, 10, 200–208. [Google Scholar] [CrossRef]
- Sallis, J.F.; Haskell, W.L.; Wood, P.D.; Fortmann, S.P.; Rogers, T.; Blair, S.N.; Paffenbarger, R.S., Jr. Physical activity assessment methodology in the Five-City Project. Am. J. Epidemiol. 1985, 121, 91–106. [Google Scholar] [CrossRef]
- Weinger, K.; Butler, H.A.; Welch, G.W.; La Greca, A.M. Measuring diabetes self-care: A psychometric analysis of the Self-Care Inventory-Revised with adults. Diabetes Care 2005, 28, 1346–1352. [Google Scholar] [CrossRef] [PubMed]
- Toobert, D.J.; Glasgow, R.E. Assessing diabetes self-management: The summary of diabetes self-care activities questionnaire. In Handbook of Psychology and Diabetes; Hardwood Academic; Bradley, C., Ed.; Routledge: Chur, Switzerland, 1994; pp. 351–375. [Google Scholar]
- Lovrić, B.; Placento, H.; Farčić, N.; Lipič Baligač, M.; Mikšić, Š.; Mamić, M.; Jovanović, T.; Vidić, H.; Karabatić, S.; Cviljević, S.; et al. Association between Health Literacy and Prevalence of Obesity, Arterial Hypertension, and Diabetes Mellitus. Int. J. Environ. Res. Public Health 2022, 19, 9002. [Google Scholar] [CrossRef] [PubMed]
- Marciano, L.; Camerini, A.-L.; Schulz, P.J. The Role of Health Literacy in Diabetes Knowledge, Self-Care, and Glycemic Control: A Meta-analysis. J. Gen. Intern. Med. 2019, 34, 1007–1017. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.H.; Pang, S.M.C.; Chan, M.F.; Yeung, G.S.P.; Yeung, V.T.F. Health literacy, complication awareness, and diabetic control in patients with type 2 diabetes mellitus. J. Adv. Nurs. 2008, 62, 74–83. [Google Scholar] [CrossRef] [PubMed]
- De Sampaio, H.A.C.; Carioca, A.A.F.; Sabry, M.O.D.; dos Santos, P.M.; Coelho, M.A.M.; da Passamai, M.P.B. Letramento em saúde de diabéticos tipo 2: Fatores associados e controle glicêmico. Ciência Saúde Coletiva 2015, 20, 865–874. [Google Scholar] [CrossRef]
- De Santos, M.I.P.O.; Portella, M.R. Condições do letramento funcional em saúde de um grupo de idosos diabéticos. Rev. Bras. Enferm. 2016, 69, 156–164. [Google Scholar] [CrossRef]
- World Health Organization. Health Promotion Glossary of Terms 2021; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Rodrigues, V.P.; Matos, L.R.; Tenani, C.F.; Batista, M.J. Literacia em saúde em adultos e idosos diabéticos usuários de sistema público de saúde em municípios de São Paulo. Rev. Ciênc. Med. 2022, 31, e215094. [Google Scholar]
- Ishikawa, H.; Nomura, K.; Sato, M.; Yano, E. Developing a measure of communicative and critical health literacy: A pilot study of Japanese office workers. Health Promot. Int. 2008, 23, 269–274. [Google Scholar] [CrossRef]
- Batista, M.J.; de Marques, A.C.P.; Silva Junior, M.F.; Alencar, G.P.; Sousa, M.D.L.R.D. Translation, cross-cultural adaptation and psychometric evaluation of Brazilian Portuguese version of the 14-item Health Literacy Scale. Ciênc. Saúde Coletiva 2020, 25, 2847–2857. [Google Scholar] [CrossRef]
- Pavão, A.L.B.; Werneck, G.L.; Campos, M.R. Autoavaliação do estado de saúde e a associação com fatores sociodemográficos, hábitos de vida e morbidade na população: Um inquérito nacional. Cad. Saúde Pública 2013, 29, 723–734. Available online: https://www.scielo.br/j/csp/a/b4Nyg8BYjDRzDMjnZpdWshB/abstract/?lang=pt (accessed on 13 September 2022). [CrossRef]
- De Oliveira, F.B.; Botelho, K.K.P.; Bezerra, A.R.; de Azevedo, D.I.O.; dos Santos-Couto-Paz, C.C.; Fachin-Martins, E. Cross-cultural adaptation to Brazilian Portuguese of the Michigan Neuropathy Screening Instrument: MNSI-Brazil. Arq. Neuro-Psiquiatr. 2016, 74, 653–661. [Google Scholar] [CrossRef]
- Michels, M.J.; Coral, M.H.C.; Sakae, T.M.; Damas, T.B.; Furlanetto, L.M. Questionário de Atividades de Autocuidado com o Diabetes: Tradução, adaptação e avaliação das propriedades psicométricas. Arq. Bras. Endocrinol. Metabol. 2010, 54, 644–651. [Google Scholar] [CrossRef]
- Tenani, C.F.; Junior, M.F.S.; Lino, C.M.; Sousa, M.d.L.R.d.; Batista, M.J. The role of health literacy as a factor associated with tooth loss. Rev. Saúde Pública 2021, 55, 116. Available online: https://www.revistas.usp.br/rsp/article/view/194671 (accessed on 13 September 2022). [CrossRef]
- Abdullah, A.; Liew, S.M.; Salim, H.; Ng, C.J.; Chinna, K. Correction: Prevalence of limited health literacy among patients with type 2 diabetes mellitus: A systematic review. PLoS ONE 2022, 17, e0261430. [Google Scholar] [CrossRef]
- Fede, B.P.; Artuso, L.R.; Tenani, C.F.; Lino, C.M.; Batista, M.J. Health literacy and prevention practices for COVID-19: A cross-sectional study in Brazilian adults. RSD 2021, 10, e425101623839. [Google Scholar] [CrossRef]
- Polonski, T.C.; Zanin, L.; Oliveira, A.M.G.; Dutra, E.R.; da Filho, D.A.S.; Flório, F.M. Influência da inclusão digital na alfabetização em saúde de idosos. ETD-Educ. Temática Digit. 2022, 24, 584–597. [Google Scholar] [CrossRef]
- Silva-Junior, M.F.; Rosário de Sousa, M.d.L.; Batista, M.J. Health literacy on oral health practice and condition in an adult and elderly population. Health Promot. Int. 2020, 36, 933–942. [Google Scholar] [CrossRef]
- IBGE-Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional por Amostra de Domicílios Contínua: Educação 2019; IBGE: Rio de Janeiro, Brazil, 2020; ISBN 978-65-87201-09-2.
- Lee, H.Y.; Lee, J.; Kim, N.K. Gender Differences in Health Literacy Among Korean Adults: Do Women Have a Higher Level of Health Literacy Than Men? Am. J. Men’s Health 2015, 9, 370–379. [Google Scholar] [CrossRef]
- Kautzky-Willer, A.; Harreiter, J. Sex and gender differences in therapy of type 2 diabetes. Diabetes Res. Clin. Pract. 2017, 131, 230–241. [Google Scholar] [CrossRef]
- Chiu, C.-J.; Wray, L.A. Gender Differences in Functional Limitations in Adults Living with Type 2 Diabetes: Biobehavioral and Psychosocial Mediators. Ann. Behav. Med. 2010, 41, 71–82. Available online: https://academic.oup.com/abm/article/41/1/71/4569509 (accessed on 30 April 2021). [CrossRef]
- Duarte, F.G.; da Silva Moreira, S.; da Almeida, M.C.C.; de Souza Teles, C.A.; Andrade, C.S.; Reingold, A.L.; Moreira, E.D., Jr. Sex differences and correlates of poor glycaemic control in type 2 diabetes: A cross-sectional study in Brazil and Venezuela. BMJ Open 2019, 9, e023401. [Google Scholar] [CrossRef] [PubMed]
- Alexandre, K.; Campbell, J.; Bugnon, M.; Henry, C.; Schaub, C.; Serex, M.; Elmers, J.; Desrichard, O.; Peytremann-Bridevaux, I. Factors influencing diabetes self-management in adults: An umbrella review of systematic reviews. JBI Evid. Synth. 2021, 19, 1003–1118. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Wang, D.; Liu, C.; Jiang, J.; Wang, X.; Chen, H.; Ju, X.; Zhang, X. What is the meaning of health literacy? A systematic review and qualitative synthesis. Fam. Med. Community Health 2020, 8, e000351. [Google Scholar] [CrossRef] [PubMed]
- Rothman, R.L. Influence of Patient Literacy on the Effectiveness of a Primary Care–Based Diabetes Disease Management Program. JAMA 2004, 292, 1711. [Google Scholar] [CrossRef]
- Zhang, N.J.; Terry, A.; McHorney, C.A. Impact of Health Literacy on Medication Adherence. Ann. Pharmacother. 2014, 48, 741–751. [Google Scholar] [CrossRef]
- Guo, X.; Zhai, X.; Hou, B. Adequacy of health literacy and its effect on diabetes self-management: A meta-analysis. Aust. J. Prim. Health 2020, 26, 458. [Google Scholar] [CrossRef]
- Lai, A.Y.; Ishikawa, H.; Kiuchi, T.; Mooppil, N.; Griva, K. Communicative and critical health literacy, and self-management behaviors in end-stage renal disease patients with diabetes on hemodialysis. Patient Educ. Couns. 2013, 91, 221–227. [Google Scholar] [CrossRef]
- Lee, Y.-J.; Shin, S.-J.; Wang, R.-H.; Lin, K.-D.; Lee, Y.-L.; Wang, Y.-H. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ. Couns. 2016, 99, 287–294. [Google Scholar] [CrossRef]
| Total | G1 n = 98 (49.3%) | G2 n = 101 (50.7%) | χ2 (or Fisher’s Exact Test)/Mann–Whitney | p-Value | |
|---|---|---|---|---|---|
| Sociodemographic variables | |||||
| Sex | |||||
| Female | 92 (46.6%) | 44 (44.9%) | 48 (47.5%) | ||
| Male | 107 (53.8%) | 54 (55.1%) | 53 (52.5%) | 0.138 a | 0.777 |
| Age (years) | 62 (IQR: 15) | 62 (IQR: 15) | 61 (IQR: 15) | 4924 c | 0.951 |
| 30–40 | 6 (3.0%) | 3 (3.1%) | 3 (3.1%) | ||
| 41–50 | 24 (12.1%) | 12 (12.2%) | 12 (11.9%) | ||
| 51–60 | 61 (30.7%) | 26 (26.5%) | 35 (34.7%) | ||
| ≥61 | 108 (54.3%) | 57 (58.2%) | 51 (50.5%) | 1.711 b | 0.643 |
| Race/color | |||||
| Blacks and Browns | 176 (88.4%) | 88 (89.8%) | 88 (87.1%) | ||
| Whites | 23 (11.6%) | 10 (10.2%) | 13 (12.9%) | 0.346 a | 0.659 |
| Education (years of study) | 8 (IQR: 7.0, 8.2) | 7 (IQR: 6.2, 7.8) | 9 (IQR: 7.3, 8.9) | 4191.5 c | 0.060 |
| Functional HL | |||||
| Low | 87 (43.7%) | 64 (73.6%) | 23 (26.4%) | ||
| High | 112 (56.3%) | 34 (30.4%) | 78 (69.6%) | 36.571 a | 0.000 * |
| Communicative HL | |||||
| Low | 99 (49.7%) | 68 (68.7%) | 31 (31.3%) | ||
| High | 100 (50.3%) | 30 (30.0%) | 70 (70.0%) | 29.790 a | 0.000 * |
| Critical HL | |||||
| Low | 86 (43.2%) | 62 (72.1%) | 24 (27.9%) | ||
| High | 113 (56.8%) | 36 (31.9%) | 77 (68.1%) | 31.629 a | 0.000 * |
| Per capita income (Reais) | 400 (IQR: 435.0, 529.8) | 367 (IQR: 383.4, 498.2) | 413 (IQR: 447.6, 597.9) | 4891.5 c | 0.171 |
| <300 | 72 (36.2%) | 36 (36.7%) | 36 (35.6%) | ||
| 300–600 | 77 (38.7%) | 43 (43.9%) | 34 (33.7%) | ||
| 601–1000 | 35 (17.6%) | 13 (13.3%) | 22 (21.8%) | ||
| >1000 | 15 (7.5%) | 6 (6.1%) | 9 (8.9%) | 3.922 a | 0.274 |
| Health-related and clinical characteristics | |||||
| Perception of general health status | |||||
| Very good | 16 (8.0%) | 6 (6.1%) | 10 (9.9%) | ||
| Good | 59 (29.6%) | 28 (28.6%) | 31 (30.7%) | ||
| Regular | 100 (50.3%) | 49 (50%) | 51 (50.5%) | ||
| Bad | 15 (7.5%) | 7 (7.1%) | 8 (7.9%) | ||
| Very bad | 9 (4.5%) | 8 (8.2%) | 1 (1.0%) | 6.666 b | 0.152 |
| Diagnosis time (years) | 8 (IQR: 11) | 6 (IQR: 10.25) | 10 (IQR: 10) | 4303 c | 0.111 |
| <5 | 53 (26.6%) | 30 (30.6%) | 23 (22.8%) | ||
| 5–10 | 77 (38.7%) | 39 (39.8%) | 38 (37.6%) | ||
| 11–20 | 46 (23.1%) | 14 (14.3%) # | 32 (31.7%) # | ||
| 21–30 | 17 (8.5%) | 9 (9.2%) | 8 (7.9%) | ||
| >30 | 6 (3.0%) | 6 (6.1%) | 0 (0%) | 14.134 b | 0.005 * |
| Consultations in past year | |||||
| 0 | 21 (10.6%) | 11 (11.2%) | 10 (9.95%) | ||
| 1–5 | 108 (54.3%) | 50 (51.0%) | 58 (57.4%) | ||
| >5 | 70 (35.2%) | 37 (37.8%) | 33 (32.7%) | 0.824 a | 0.655 |
| Private health insurance | |||||
| Yes | 23 (11.6%) | 6 (6.1%) # | 17 (16.8%) # | ||
| No | 176 (88.4%) | 91 (93.9%) | 84 (83.2%) | 5.158 a | 0.025 * |
| Smoking consumption | |||||
| Non-smokers | 100 (50.3%) | 42 (42.9%) | 58 (57.4%) | ||
| Ex-smoker | 87 (43.7%) | 48 (49%) | 39 (38.6%) | ||
| Smoker | 12 (6.0%) | 8 (8.2%) | 4 (4%) | 4.78 a | 0.093 |
| Alcohol consumption | |||||
| Yes | 134 (67.3%) | 68 (69.4%) | 66 (65.3%) | ||
| No | 65 (32.7%) | 30 (30.6%) | 35 (34.7%) | 0.369 a | 0.550 |
| Physical activity | |||||
| Sedentary | 69 (34.7%) | 32 (32.7%) | 37 (36.6%) | ||
| Irregular | 92 (46.2%) | 48 (49%) | 44 (43.6%) | ||
| Regular | 38 (19.1%) | 18 (18.4%) | 20 (19.8%) | 0.596 a | 0.748 |
| SAH | |||||
| Yes | 136 (68.3%) | 70 (71.4%) | 66 (65.3%) | ||
| No | 63 (31.7%) | 28 (28.6%) | 35 (34.7%) | 0.850 a | 0.366 |
| Peripheral neuropathy | |||||
| Present | 132 (66.3%) | 70 (71.4%) | 62 (61.4%) | ||
| Absent | 67 (33.7%) | 28 (28.6%) | 39 (38.6%) | 2.246 a | 0.177 |
| Biochemical parameters | |||||
| Total cholesterol (mg/dL) | |||||
| 87–189 | 98 (49.2%) | 50 (51%) | 48 (47.5%) | ||
| ≥190 | 101 (50.8%) | 48 (49%) | 51.3 (52.5%) | 0.243 a | 0.671 |
| HDL (mg/dL) | |||||
| 20–39 | 94 (47.2%) | 44 (44.9%) | 50 (49.5%) | ||
| ≥40 | 105 (52.8%) | 54 (55.1%) | 51 (50.5%) | 0.424 a | 0.571 |
| LDL (mg/dL) | |||||
| 15–99 | 76 (38.2%) | 36 (36.7%) | 40 (39.6%) | ||
| ≥100 | 123 (61.8%) | 62 (63.3%) | 60.1 (60.4%) | 0.173 a | 0.771 |
| Non-HDL (mg/dL) | |||||
| 59–129 | 73 (36.7%) | 40 (40.8%) | 33 (32.7%) | ||
| ≥130 | 126 (63.3%) | 58 (59.2%) | 68 (67.3%) | 1.420 a | 0.243 |
| Triglycerides (mg/dL) | |||||
| 36–149 | 72 (36.2%) | 42 (42.9%) | 30 (29.7%) | ||
| ≥150 | 127 (63.8%) | 56 (57.1%) | 71 (70.3%) | 3.727 a | 0.057 |
| Glycated hemoglobin (mg/dL) | |||||
| 4.8–6.9% | 33 (16.6%) | 17 (17.3%) | 16 (15.8%) | ||
| ≥7% | 166 (83.4%) | 81 (82.7%) | 85 (84.2%) | 0.081 a | 0.850 |
| Microalbumi-nuria (Creatinina mg/g) | |||||
| <30 | 142 (71.4%) | 71 (72.4%) | 71 (70.3%) | ||
| 30–300 | 41 (20.6%) | 18 (18.4%) | 23 (22.8%) | ||
| >300 | 16 (8.0%) | 9 (9.2%) | 7 (6.9%) | 0.815 a | 0.705 |
| QAD | |||||
| Geral diet (days) | 3 (IQR: 5) | 3 (IQR: 3.25) | 3 (IQR: 5) | 4896 c | 0.894 |
| Specific diet (days) | 1 (IQR: 1) | 1 (IQR: 1) | 1 (IQR: 1) | 4875 c | 0.848 |
| Physical activity (days) | 0 (IQR: 4) | 0 (IQR: 4) | 0 (IQR: 4) | 4893 c | 0.879 |
| Foot care (days) | 4 (IQR: 3) | 3 (IQR: 3) | 5 (IQR: 5) | 3908.5 c | 0.009 * |
| Medication | 5 (IQR: 1) | 5 (IQR: 2) | 5 (IQR: 0) | 4037.5 c | 0.013 * |
| Glycemic monitoring (days) | 0 (IQR: 1) | 0 (IQR: 1) | 0 (IQR: 1) | 4891.5 c | 0.867 |
| N | OR 1 | CI 95% 1 | p-Value 1 | OR 2 | CI 95% 2 | p-Value 2 | |
|---|---|---|---|---|---|---|---|
| TOTAL HL | |||||||
| Sex | 199 | 0.90 | 0.51, 1.57 | 0.710 | |||
| Age | 199 | 1.00 | 0.97, 1.02 | 0.884 | |||
| Race/color | 199 | 1.30 | 0.54, 3.12 | 0.557 | |||
| Education | 199 | 1.07 | 0.98, 1.14 | 0.058 # | 0.93 | 0.87, 1.00 | 0.070 |
| Per capita income | 199 | 1.00 | 1.00, 1.00 | 0.092 # | 0.99 | 0.99, 1.00 | 0.110 |
| FUNCTIONAL HL | |||||||
| Sex | 199 | 1.82 | 1.03, 3.22 | 0.039 # | 1.96 | 1.09, 3.52 | 0.024 * |
| Age | 199 | 1.00 | 0.97, 1.03 | 0.728 | |||
| Race/color | 199 | 0.80 | 0.33, 1.96 | 0.638 | |||
| Education | 199 | 1.10 | 1.02, 1.18 | 0.008 # | 1.11 | 1.03, 1.19 | 0.005 * |
| Per capita income | 199 | 1.00 | 0.99, 1.00 | 0.555 | |||
| COMMUNICATIVE HL | |||||||
| Sex | 199 | 0.83 | 0.47, 1.45 | 0.526 | |||
| Age | 199 | 0.98 | 0.95, 1.01 | 0.214 | |||
| Race/color | 199 | 0.73 | 0.30, 1.76 | 0.491 | |||
| Education | 199 | 1.00 | 0.94, 1.07 | 0.856 | |||
| Per capita income | 199 | 1.00 | 0.99, 1.00 | 0.664 | |||
| CRITICAL HL | |||||||
| Sex | 199 | 0.86 | 0.49, 1.51 | 0.614 | |||
| Age | 199 | 0.98 | 0.95, 1.01 | 0.225 | |||
| Race/color | 199 | 1.23 | 0.51, 2.94 | 0.636 | |||
| Education | 199 | 0.99 | 0.92, 1.06 | 0.885 | |||
| Per capita income | 199 | 1.00 | 1.00, 1.00 | 0.069 # |
| N | OR 1 | 95% CI 1 | p-Value 1 | OR 2 | 95% CI 2 | p-Value 2 | |
|---|---|---|---|---|---|---|---|
| GLYCATED HEMOGLOBIN | |||||||
| Sex | 199 | 1.20 | 0.56, 2.55 | 0.631 | |||
| Age | 199 | 0.95 | 0.91, 0.99 | 0.017 # | 0.96 | 0.92, 1.00 | 0.071 |
| Race/color | 199 | 0.73 | 0.20, 2.61 | 0.629 | |||
| Education | 199 | 0.95 | 0.86, 1.04 | 0.283 | |||
| Total literacy | 199 | 0.89 | 0.42, 1.89 | 0.775 | |||
| Functional literacy | 199 | 0.91 | 0.43, 1.94 | 0.826 | |||
| Communicative literacy | 199 | 0.79 | 0.37, 1.68 | 0.547 | |||
| Critical literacy | 199 | 0.36 | 0.16, 0.79 | 0.011 # | 0.32 | 0.14, 0.74 | 0.008 * |
| Per capita income | 199 | 0.99 | 0.99, 1.00 | 0.066 # | 0.99 | 0.99, 1.00 | 0.071 |
| TOTAL CHOLESTEROL | |||||||
| Sex | 199 | 2.40 | 1.36, 4.26 | 0.003 # | 0.41 | 0.23, 0.75 | 0.004 * |
| Age | 199 | 0.97 | 0.95, 1.00 | 0.092 # | 0.98 | 0.95, 1.01 | 0.323 |
| Race/color | 199 | 0.93 | 0.39, 2.23 | 0.885 | |||
| Education | 199 | 0.98 | 0.91, 1.05 | 0.614 | |||
| Total HL | 199 | 0.86 | 0.49, 1.51 | 0.622 | |||
| Functional HL | 199 | 0.79 | 0.45, 1.38 | 0.416 | |||
| Communicative HL | 199 | 1.19 | 0.68, 2.09 | 0.524 | |||
| Critical HL | 199 | 1.88 | 1.06, 3.31 | 0.029 # | 0.50 | 0.28, 0.91 | 0.024 * |
| Per capita income | 199 | 1.00 | 0.99, 1.00 | 0.732 | |||
| LDL | |||||||
| Sex | 199 | 0.50 | 0.28, 0.90 | 0.022 # | 0.50 | 0.27, 0.92 | 0.027 * |
| Age | 199 | 0.97 | 0.95, 1.00 | 0.112 # | 0.98 | 0.95, 1.01 | 0.328 |
| Race/color | 199 | 1.04 | 0.42, 2.54 | 0.921 | |||
| Education | 199 | 0.99 | 0.92, 1.06 | 0.843 | |||
| Total HL | 199 | 1.12 | 0.63, 2.00 | 0.677 | |||
| Functional HL | 199 | 1.44 | 0.80, 2.59 | 0.215 | |||
| Communicative HL | 199 | 0.83 | 0.46, 1.47 | 0.523 | |||
| Critical HL | 199 | 0.45 | 0.25, 0.80 | 0.007 # | 0.43 | 0.24, 0.79 | 0.007 * |
| Per capita income | 199 | 1.00 | 0.99, 1.00 | 0.545 | |||
| HDL | |||||||
| Sex | 199 | 0.35 | 0.19, 0.63 | 0.000 # | 0.34 | 0.18, 0.62 | 0.001 * |
| Age | 199 | 0.32 | 0.17, 0.58 | 0.000 # | 1.02 | 0.99, 1.05 | 0.071 |
| Race/color | 199 | 1.25 | 0.52, 2.98 | 0.615 | |||
| Education | 199 | 1.04 | 0.97, 1.12 | 0.197 # | 1.06 | 0.98, 1.14 | 0.096 |
| Total HL | 199 | 1.20 | 0.68, 2.10 | 0.515 | |||
| Functional HL | 199 | 1.65 | 0.93, 2.91 | 0.082 # | 1.64 | 0.89, 3.02 | 0.112 |
| Communicative HL | 199 | 0.83 | 0.47, 1.45 | 0.526 | |||
| Critical HL | 199 | 1.05 | 0.60, 1.84 | 0.858 | |||
| Per capita income | 199 | 1.00 | 0.99, 1.00 | 0.403 | |||
| Non-HDL | |||||||
| Sex | 199 | 0.58 | 0.32, 1.03 | 0.066 # | 0.60 | 0.33, 1.09 | 0.093 |
| Age | 199 | 0.97 | 0.95, 1.00 | 0.120 # | 0.98 | 0.95, 1.01 | 0.265 |
| Race/color | 199 | 1.09 | 0.44, 2.73 | 0.841 | |||
| Education | 199 | 0.99 | 0.92, 1.06 | 0.844 | |||
| Total HL | 199 | 0.70 | 0.39, 1.25 | 0.23 | |||
| Functional HL | 199 | 1.08 | 0.60, 1.94 | 0.786 | |||
| Communicative HL | 199 | 0.86 | 0.48, 1.53 | 0.621 | |||
| Critical HL | 199 | 0.61 | 0.34, 1.10 | 0.106 # | 0.61 | 0.34, 1.11 | 0.112 |
| Per capita income | 199 | 1.00 | 1.00, 1.00 | 0.250 | |||
| TRIGLYCERIDES | |||||||
| Sex | 199 | 0.93 | 0.52, 1.67 | 0.833 | |||
| Age | 199 | 0.98 | 0.95, 1.01 | 0.318 | |||
| Race/color | 199 | 0.28 | 0.22, 1.56 | 0.288 | |||
| Education | 199 | 1.04 | 0.97, 1.12 | 0.193 # | 1.03 | 0.95, 1.11 | 0.405 |
| Total HL | 199 | 0.56 | 0.31, 101 | 0.055 # | 0.71 | 0.36, 1.38 | 0.322 |
| Functional HL | 199 | 0.42 | 0.23, 0.77 | 0.005 # | 0.49 | 0.25, 0.96 | 0.039 * |
| Communicative HL | 199 | 1.27 | 0.71, 2.28 | 0.406 | |||
| Critical HL | 199 | 1.20 | 0.67, 2.17 | 0.529 | |||
| Per capita income | 199 | 0.99 | 0.99, 1.00 | 0.142 # | 0.99 | 0.99, 1.00 | 0.077 |
| MICROALBUMINURIA | |||||||
| Sex | |||||||
| 30–300 | 199 | 2.16 | 1.07, 4.29 | 0.032 # | 1.77 | 0.82, 3.81 | 0.140 |
| >300 | 199 | 4.60 | 1.41, 15.00 | 0.011# | 4.74 | 1.37, 16.41 | 0.014 * |
| Age | |||||||
| 30–300 | 199 | 1.04 | 1.00, 1.08 | 0.028 # | 1.03 | 0.99, 1.08 | 0.070 |
| >300 | 1.02 | 0.97, 1.08 | 0.281 | 1.00 | 0.94, 1.06 | 0.819 | |
| Race/color | |||||||
| 30–300 | 199 | 0.57 | 0.21, 1.51 | 0.263 | 0.59 | 0.20, 1.72 | 0.337 |
| >300 | 199 | 1.77 | 0.21, 14.37 | 0.592 | 1.99 | 0.23, 17.39 | 0.530 |
| Education | |||||||
| 30–300 | 199 | 0.96 | 0.88, 1.04 | 0.370 | 0.94 | 0.85, 1.03 | 0.237 |
| >300 | 199 | 0.91 | 0.80, 1.04 | 0.179 # | 0.944 | 0.81, 1.09 | 0.440 |
| Total HL | |||||||
| 30–300 | 199 | 0.78 | 0.38, 1.57 | 0.492 | |||
| >300 | 199 | 1.28 | 0.45, 3.64 | 0.636 | |||
| Functional HL | |||||||
| 30–300 | 199 | 0.56 | 0.27, 1.18 | 0.130 # | 0.48 | 0.21, 1.09 | 0.080 |
| >300 | 199 | 2.03 | 0.70, 5.89 | 0.192 # | 2.30 | 0.72, 7.32 | 0.158 |
| Communicative HL | |||||||
| 30–300 | 199 | 0.43 | 0.21, 0.90 | 0.026 # | 0.31 | 0.14, 0.69 | 0.311 |
| >300 | 199 | 0.84 | 0.30, 2.37 | 0.844 | 0.90 | 0.30, 2.75 | 0.866 |
| Critical HL | |||||||
| 30–300 | 199 | 0.78 | 0.38, 1.58 | 0.492 | |||
| >300 | 199 | 0.73 | 0.25, 2.12 | 0.565 | |||
| Per capita income | |||||||
| 30–300 | 199 | 1.00 | 1.00, 1.00 | 0.163 # | 1.00 | 0.99, 1.00 | 0.518 |
| >300 | 199 | 1.00 | 1.00, 1.00 | 0.089 # | 1.00 | 0.99, 1.00 | 0.283 |
| β | t | p-Value | |
|---|---|---|---|
| GENERAL DIET | |||
| Constant | 3.327 | 8.655 | 0.000 |
| Total HL | 0.548 | 1.108 | 0.269 |
| Functional HL | -0.779 | −1.775 | 0.078 |
| Communicative HL | −0.206 | −0.497 | 0.620 |
| Critical HL | −0.094 | −0.225 | 0.822 |
| SPECIFIC DIET | |||
| Constant | 1.353 | 9.286 | 0.000 |
| Total HL | −0.154 | −0.823 | 0.412 |
| Functional HL | −0.033 | −0.200 | 0.841 |
| Communicative HL | 0.003 | 0.019 | 0.985 |
| Critical HL | 0.485 | 3.073 | 0.002 * |
| PHYSICAL ACTIVITY | |||
| Constant | 1.669 | 4.896 | 0.000 |
| Total HL | 0.009 | 0.022 | 0.983 |
| Functional HL | −0.012 | −0.032 | 0.975 |
| Communicative HL | −0.041 | −0.111 | 0.912 |
| Critical HL | 0.029 | 0.080 | 0.937 |
| FOOT CARE | |||
| Constant | 3.193 | 9.637 | 0.000 |
| Total HL | 0.723 | 1.694 | 0.092 |
| Functional HL | 0.105 | 0.276 | 0.783 |
| Communicative HL | 0.093 | 0.261 | 0.795 |
| Critical HL | 0.076 | 0.211 | 0.833 |
| MEDICATION | |||
| Constant | 4.276 | 15.278 | 0.000 |
| Total HL | 0.804 | 2.229 | 0.027 * |
| Functional HL | −0.093 | −0.291 | 0.771 |
| Communicative HL | −0.008 | −0.025 | 0.980 |
| Critical HL | −0.380 | −1.255 | 0.211 |
| BLOOD GLUCOSE MONITORING | |||
| Constant | 0.740 | 2.478 | 0.014 |
| Total HL | 0.079 | 0.205 | 0.838 |
| Functional HL | 0.315 | 0.924 | 0.356 |
| Communicative HL | 0.073 | 0.226 | 0.821 |
| Critical HL | 0.079 | 0.304 | 0.762 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tavares, V.B.; Farias, A.L.d.; Silva, A.S.A.d.; Souza, J.d.S.e.; Silva, H.P.d.; Bastos, M.d.S.C.B.d.O.; Melo-Neto, J.S.d. Amazon Amandaba—Sociodemographic Factors, Health Literacy, Biochemical Parameters and Self-Care as Predictors in Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 3082. https://doi.org/10.3390/ijerph20043082
Tavares VB, Farias ALd, Silva ASAd, Souza JdSe, Silva HPd, Bastos MdSCBdO, Melo-Neto JSd. Amazon Amandaba—Sociodemographic Factors, Health Literacy, Biochemical Parameters and Self-Care as Predictors in Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(4):3082. https://doi.org/10.3390/ijerph20043082
Chicago/Turabian StyleTavares, Victória Brioso, Aline Lobato de Farias, Amanda Suzane Alves da Silva, Josiel de Souza e Souza, Hilton Pereira da Silva, Maria do Socorro Castelo Branco de Oliveira Bastos, and João Simão de Melo-Neto. 2023. "Amazon Amandaba—Sociodemographic Factors, Health Literacy, Biochemical Parameters and Self-Care as Predictors in Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 4: 3082. https://doi.org/10.3390/ijerph20043082
APA StyleTavares, V. B., Farias, A. L. d., Silva, A. S. A. d., Souza, J. d. S. e., Silva, H. P. d., Bastos, M. d. S. C. B. d. O., & Melo-Neto, J. S. d. (2023). Amazon Amandaba—Sociodemographic Factors, Health Literacy, Biochemical Parameters and Self-Care as Predictors in Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 20(4), 3082. https://doi.org/10.3390/ijerph20043082






