Depression and Anxiety in Old Age during the COVID-19 Pandemic: A Comparative Study of Individuals at Cardiovascular Risk and the General Population
Abstract
1. Introduction
2. Methods
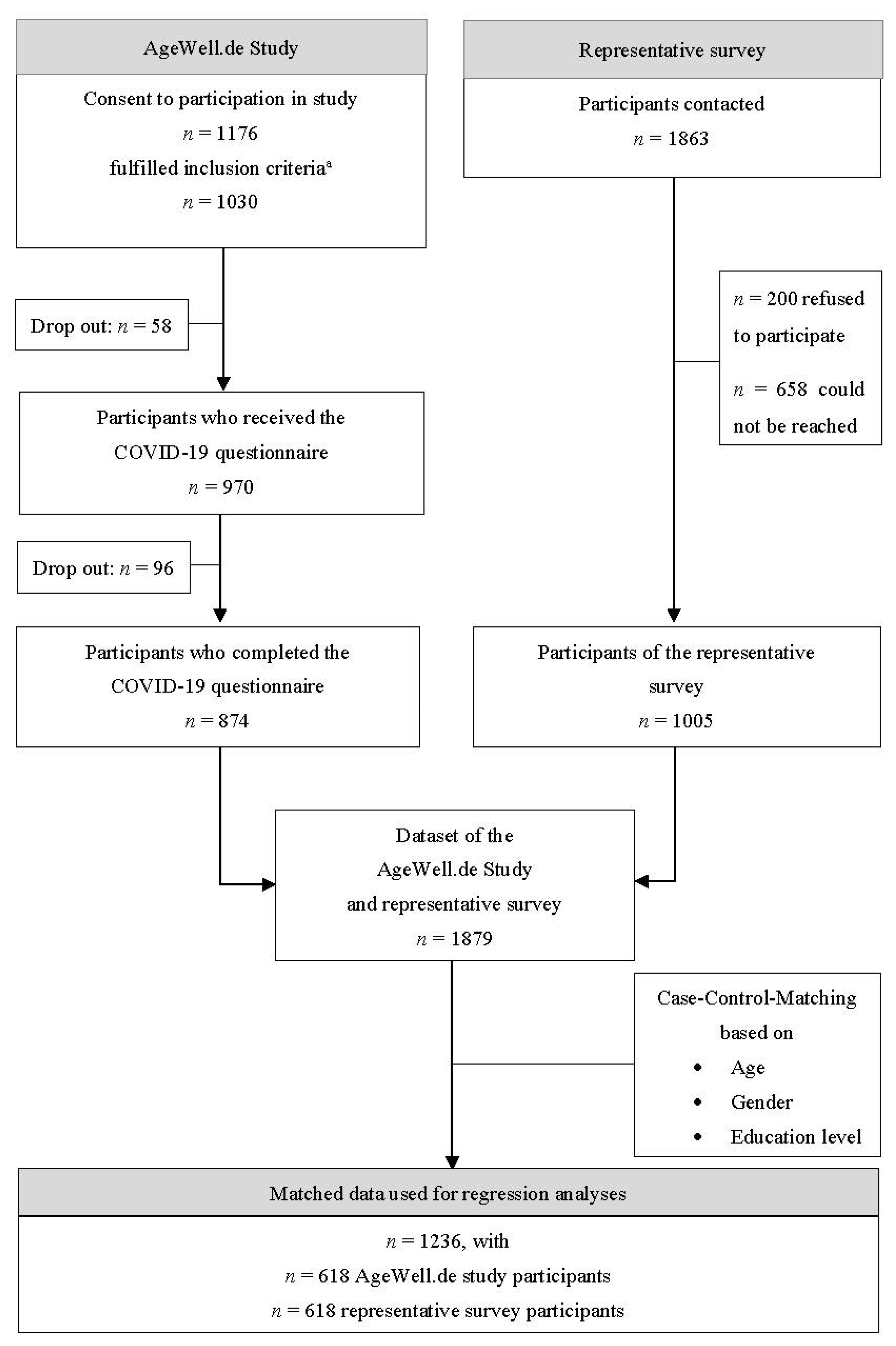
2.1. Procedure and Participants
2.2. Measures
2.2.1. Independent Variables
2.2.2. Dependent Variables
2.3. Data Analysis
3. Results
3.1. Sample Characteristics and Differences in Psychosocial Variables
3.2. Predicting Mental Health Factors in the Cardiovascular Risk Sample
3.3. Predicting Mental Health Factors in the General Population
4. Discussion
4.1. Differences in Psychosocial Characteristics between the Older Cardiovascular Risk Group and the General Population
4.2. Determinants of Anxiety and Depression Symptoms in the Cardiovascular Risk Group Compared to the General Population
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Röhr, S.; Müller, F.; Jung, F.; Apfelbacher, C.; Seidler, A.; Riedel-Heller, S.G. Psychosocial Impact of Quarantine Measures During Serious Coronavirus Outbreaks: A Rapid Review. Psychiatr. Prax. 2020, 47, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Mergel, E.; Schützwohl, M. COVID-19 und psychisches Befinden im zweiten Lockdown—Fortsetzung einer Verlaufsuntersuchung. Psychiatr. Prax. 2021, 48, 265–268. [Google Scholar] [CrossRef]
- Palmieri, L.; Vanacore, N.; Donfrancesco, C.; Lo Noce, C.; Canevelli, M.; Punzo, O.; Raparelli, V.; Pezzotti, P.; Riccardo, F.; Bella, A.; et al. Clinical Characteristics of Hospitalized Individuals Dying With COVID-19 by Age Group in Italy. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 1796–1800. [Google Scholar] [CrossRef]
- Mai, F.; Del Pinto, R.; Ferri, C. COVID-19 and cardiovascular diseases. J. Cardiol. 2020, 76, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Yang, J.; Zhao, F.; Zhi, L.; Wang, X.; Liu, L.; Bi, Z.; Zhao, Y. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin. Res. Cardiol. 2020, 109, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Tyrovolas, S.; Lionis, C.; Zeimbekis, A.; Bountziouka, V.; Micheli, M.; Katsarou, A.; Papairakleous, N.; Metallinos, G.; Makri, K.; Polychronopoulos, E.; et al. Increased body mass and depressive symptomatology are associated with hypercholesterolemia, among elderly individuals; results from the MEDIS study. Lipids Health Dis. 2009, 8, 10. [Google Scholar] [CrossRef] [PubMed]
- Turana, Y.; Tengkawan, J.; Chia, Y.C.; Shin, J.; Chen, C.H.; Park, S.; Tsoi, K.; Buranakitjaroen, P.; Soenarta, A.A.; Siddique, S.; et al. Mental health problems and hypertension in the elderly: Review from the HOPE Asia Network. J. Clin. Hypertens. 2021, 23, 504–512. [Google Scholar] [CrossRef]
- Zhang, X.C.; Woud, M.L.; Becker, E.S.; Margraf, J. Do health-related factors predict major depression? A longitudinal epidemiologic study. Clin. Psychol. Psychother. 2018, 25, 378–387. [Google Scholar] [CrossRef]
- Deimel, D.; Köhler, T.; Dyba, J.; Graf, N.; Firk, C. Mental health of Covid-19 risk groups during the first Covid-19 lockdown in Germany: A cross-sectional study. BMC Public Health 2022, 22, 1187. [Google Scholar] [CrossRef]
- Mitchell, P.B.; Harvey, S.B. Depression and the older medical patient--when and how to intervene. Maturitas 2014, 79, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.Y.S.; Zhang, D.; Sit, R.W.S.; Yip, B.H.K.; Chung, R.Y.N.; Wong, C.K.M.; Chan, D.C.C.; Sun, W.; Kwok, K.O.; Mercer, S.W. Impact of COVID-19 on loneliness, mental health, and health service utilisation: A prospective cohort study of older adults with multimorbidity in primary care. Br. J. Gen. Pract. 2020, 70, e817–e824. [Google Scholar] [CrossRef] [PubMed]
- Szkody, E.; Stearns, M.; Stanhope, L.; McKinney, C. Stress-Buffering Role of Social Support during COVID-19. Fam. Process 2021, 60, 1002–1015. [Google Scholar] [CrossRef] [PubMed]
- Levkovich, I.; Shinan-Altman, S.; Essar Schvartz, N.; Alperin, M. Depression and Health-Related Quality of Life Among Elderly Patients during the COVID-19 Pandemic in Israel: A Cross-sectional Study. J. Prim. Care Community Health 2021, 12, 2150132721995448. [Google Scholar] [CrossRef]
- Özmete, E.; Pak, M. The Relationship between Anxiety Levels and Perceived Social Support during the Pandemic of COVID-19 in Turkey. Soc. Work Public Health 2020, 35, 603–616. [Google Scholar] [CrossRef]
- Röhr, S.; Reininghaus, U.; Riedel-Heller, S.G. Mental wellbeing in the German old age population largely unaltered during COVID-19 lockdown: Results of a representative survey. BMC Geriatr. 2020, 20, 489. [Google Scholar] [CrossRef]
- Müller, F.; Röhr, S.; Reininghaus, U.; Riedel-Heller, S.G. Social Isolation and Loneliness during COVID-19 Lockdown: Associations with Depressive Symptoms in the German Old-Age Population. Int. J. Environ. Res. Public Health 2021, 18, 3615. [Google Scholar] [CrossRef]
- Weitzel, E.C.; Löbner, M.; Röhr, S.; Pabst, A.; Reininghaus, U.; Riedel-Heller, S.G. Prevalence of High Resilience in Old Age and Association with Perceived Threat of COVID-19—Results from a Representative Survey. Int. J. Environ. Res. Public Health 2021, 18, 7173. [Google Scholar] [CrossRef]
- Welzel, F.D.; Schladitz, K.; Förster, F.; Löbner, M.; Riedel-Heller, S.G. Gesundheitliche Folgen sozialer Isolation: Qualitative Studie zu psychosozialen Belastungen und Ressourcen älterer Menschen im Zusammenhang mit der COVID-19-Pandemie. Bundesgesundheitsblatt—Gesundh.—Gesundh. 2021, 64, 334–341. [Google Scholar] [CrossRef]
- McCleskey, J.; Gruda, D. Risk-taking, resilience, and state anxiety during the COVID-19 pandemic: A coming of (old) age story. Personal. Individ. Differ. 2021, 170, 110485. [Google Scholar] [CrossRef]
- Grolli, R.E.; Mingoti, M.E.D.; Bertollo, A.G.; Luzardo, A.R.; Quevedo, J.; Réus, G.Z.; Ignacio, Z.M. Impact of COVID-19 in the Mental Health in Elderly: Psychological and Biological Updates. Mol. Neurobiol. 2021, 58, 1905–1916. [Google Scholar] [CrossRef] [PubMed]
- Zülke, A.; Luck, T.; Pabst, A.; Hoffmann, W.; Thyrian, J.R.; Gensichen, J.; Kaduszkiewicz, H.; König, H.H.; Haefeli, W.E.; Czock, D.; et al. AgeWell.de—Study protocol of a pragmatic multi-center cluster-randomized controlled prevention trial against cognitive decline in older primary care patients. BMC Geriatr. 2019, 19, 203. [Google Scholar] [CrossRef]
- Röhr, S.; Zülke, A.; Luppa, M.; Brettschneider, C.; Weißenborn, M.; Kühne, F.; Zöllinger, I.; Samos, F.A.Z.; Bauer, A.; Döhring, J.; et al. Recruitment and Baseline Characteristics of Participants in the AgeWell.de Study-A Pragmatic Cluster-Randomized Controlled Lifestyle Trial against Cognitive Decline. Int. J. Environ. Res. Public Health 2021, 18, 408. [Google Scholar] [CrossRef] [PubMed]
- Kivipelto, M.; Ngandu, T.; Laatikainen, T.; Winblad, B.; Soininen, H.; Tuomilehto, J. Risk score for the prediction of dementia risk in 20 years among middle aged people: A longitudinal, population-based study. Lancet Neurol. 2006, 5, 735–741. [Google Scholar] [CrossRef] [PubMed]
- Kendel, F.; Spaderna, H.; Sieverding, M.; Dunkel, A.; Lehmkuhl, E.; Hetzer, R.; Regitz-Zagrosek, V. Eine deutsche Adaptation des ENRICHD Social Support Inventory (ESSI). Diagnostica 2011, 57, 99–106. [Google Scholar] [CrossRef]
- Mitchell, P.H.; Powell, L.; Blumenthal, J.; Norten, J.; Ironson, G.; Pitula, C.R.; Froelicher, E.S.; Czajkowski, S.; Youngblood, M.; Huber, M.; et al. A Short Social Support Measure for Patients Recovering from Myocardial Infarction. J. Cardiopulm. Rehabil. 2003, 23, 398–403. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef]
- Chmitorz, A.; Wenzel, M.; Stieglitz, R.D.; Kunzler, A.; Bagusat, C.; Helmreich, I.; Gerlicher, A.; Kampa, M.; Kubiak, T.; Kalisch, R.; et al. Population-based validation of a German version of the Brief Resilience Scale. PLoS ONE 2018, 13, e0192761. [Google Scholar] [CrossRef]
- Spitzer, C.; Hammer, S.; Löwe, B.; Grabe, H.J.; Barnow, S.; Rose, M.; Wingenfeld, K.; Freyberger, H.J.; Franke, G.H. Die kurzform des Brief Symptom Inventory (BSI-18): Erste Befunde zu den psychometrischen Kennwerten der deutschen Version. [The short version of the Brief Symptom Inventory (BSI-18): Preliminary psychometric properties of the German translation]. Fortschr. Neurol. Psychiatr. 2011, 79, 517–523. [Google Scholar] [CrossRef]
- SPSS Statistics for Windows; IBM Corp.: Armonk, NY, USA, 2020.
- Stata Statistical Software: Release 16; StataCorp LLC: College Station, TX, USA, 2019.
- Hayes, A.F.; Cai, L. Using heteroskedasticity-consistent standard error estimators in OLS regression: An introduction and software implementation. Behav. Res. Methods 2007, 39, 709–722. [Google Scholar] [CrossRef]
- Mattioli, A.V.; Ballerini Puviani, M.; Nasi, M.; Farinetti, A. COVID-19 pandemic: The effects of quarantine on cardiovascular risk. Eur. J. Clin. Nutr. 2020, 74, 852–855. [Google Scholar] [CrossRef] [PubMed]
- Grey, I.; Arora, T.; Thomas, J.; Saneh, A.; Tohme, P.; Abi-Habib, R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. 2020, 293, 113452. [Google Scholar] [CrossRef] [PubMed]
- Thyrian, J.R.; Kracht, F.; Nikelski, A.; Boekholt, M.; Schumacher-Schönert, F.; Rädke, A.; Michalowsky, B.; Vollmar, H.C.; Hoffmann, W.; Rodriguez, F.S.; et al. The situation of elderly with cognitive impairment living at home during lockdown in the Corona-pandemic in Germany. BMC Geriatr. 2020, 20, 540. [Google Scholar] [CrossRef]
- Diefenbach, G.J.; McCarthy-Larzelere, M.E.; Williamson, D.A.; Mathews, A.; Manguno-Mire, G.M.; Bentz, B.G. Anxiety, depression, and the content of worries. Depress. Anxiety 2001, 14, 247–250. [Google Scholar] [CrossRef]
| Representative Survey Sample (n = 618) | Cardiovascular Risk Sample (n = 618) | Group Differences (p-Value) | |
|---|---|---|---|
| Sociodemographic characteristics of the matched sample | |||
| Age; M (SD) | 71.99 (4.36) | 71.94 (4.38) | 0.811 |
| Gender; n (%) | 1.000 | ||
| Female | 358 (57.9) | 358 (57.9) | |
| Male | 260 (42.1) | 260 (42.1) | |
| Education level; n (%) | 1.000 | ||
| Low | 159 (25.7) | 159 (25.7) | |
| Middle | 275 (44.5) | 275 (44.5) | |
| High | 184 (29.8) | 184 (29.8) | |
| Marital Status; n (%) | 0.006 | ||
| Single/divorced | 144 (23.3) | 102 (16.5) | |
| Married/with partner | 355 (57.4) | 403 (65.2) | |
| Widowed | 117 (18.9) | 113 (18.3) | |
| Living situation; n (%) | 0.050 | ||
| Living alone | 229 (37.1) | 196 (31.7) | |
| Living with someone | 389 (62.9) | 421 (68.1) | |
| Cardiovascular risk score | 10.13 (1.24, 9–14) | ||
| M (SD, range) | |||
| Systolic blood pressure > 140 mmHg; n (%) | 539 (87.2) | ||
| Body mass index > 30 kg/m2; n (%) | 360 (58.3) | ||
| Total cholesterol > 6.5 mmol/L; n (%) | 353 (57.1) | ||
| Physical activity less than 2 time/week for at least 30 min; n (%) | 450 (72.8) | ||
| Perception and attitude towards the COVID-19 pandemic | |||
| Being worried; M (SD) | 2.54 (1.35) | 2.58 (1.10) | 0.849 |
| Perceived threat due to pre-existing conditions; M (SD) | 1.88 (1.59) | 2.37 (1.34) | <0.001 |
| Being supportive of the governmental measures; M (SD) | 3.60 (0.82) | 3.49 (0.84) | 0.001 |
| Psychosocial variables | |||
| Perceived social support; M (SD) | 21.50 (3.76) | 21.60 (3.88) | 0.442 |
| Resilience; M(SD) | 2.62 (0.68) | 2.57 (0.78) | 0.298 |
| Depressive symptoms; M (SD) | 1.28 (1.86) | 1.65 (2.52) | 0.004 |
| Anxiety symptoms; M (SD) | 1.55 (1.98) | 1.56 (2.36) | 0.934 |
| Depressive Symptoms | Anxiety Symptoms | |||
|---|---|---|---|---|
| β | p-Value | β | p-Value | |
| Sociodemographic variables | ||||
| Age | −0.023 | 0.531 | 0.017 | 0.683 |
| Gender | ||||
| Female | Reference | Reference | ||
| Male | −0.005 | 0.907 | −0.056 | 0.173 |
| Education | F(2) = 2.93 | 0.055 | F(2) = 4.64 | 0.010 |
| Low | Reference | Reference | ||
| Middle | −0.009 | 0.854 | 0.000 | 0.993 |
| High | 0.085 | 0.073 | 0.130 | 0.011 |
| Marital Status | F(2) = 1.08 | 0.341 | F(2) = 0.090 | 0.490 |
| Single/divorced | Reference | Reference | ||
| Married/partner | 0.126 | 0.191 | 0.012 | 0.878 |
| Widowed | 0.060 | 0.287 | 0.068 | 0.215 |
| Living Situation | ||||
| Alone | Reference | |||
| With others | −0.119 | 0.191 | 0.073 | 0.306 |
| Psychosocial variables | ||||
| Perceived worries about the virus | 0.081 | 0.068 | −0.008 | 0.867 |
| Perceived threat due to preexisting conditions | 0.043 | 0.330 | 0.090 | 0.038 |
| Being supportive of governmental measures | −0.047 | 0.169 | −0.054 | 0.230 |
| Perceived social support | −0.269 | <0.001 | −0.107 | 0.015 |
| Resilience | −0.267 | <0.001 | −0.368 | <0.001 |
| Method factor | −0.105 | 0.102 | −0.059 | 0.331 |
| R2 | 0.257 | 0.225 | ||
| n | 553 | 552 | ||
| Depressive Symptoms | Anxiety Symptoms | |||
|---|---|---|---|---|
| β | p-Value | β | p-Value | |
| Sociodemographic variables | ||||
| Age | −0.057 | 0.163 | 0.008 | 0.868 |
| Gender | ||||
| Female | Reference | Reference | ||
| Male | 0.079 | 0.045 | 0.010 | 0.808 |
| Education | F(2) = 0.22 | 0.800 | F(2) = 3.50 | 0.031 |
| Low | Reference | Reference | ||
| Middle | 0.003 | 0.950 | −0.038 | 0.451 |
| High | 0.024 | 0.590 | 0.073 | 0.147 |
| Marital Status | F(2) = 4.80 | 0.009 | F(2) = 0.06 | 0.943 |
| Single/divorced | Reference | Reference | ||
| Married/partner | −0.062 | 0.404 | −0.011 | 0.885 |
| Widowed | 0.141 | 0.017 | 0.011 | 0.831 |
| Living Situation | ||||
| Alone | Reference | Reference | ||
| With others | −0.006 | 0.931 | 0.024 | 0.720 |
| Psychosocial variables | ||||
| Perceived worries about the virus | 0.078 | 0.090 | 0.121 | 0.005 |
| Perceived threat due to preexisting conditions | −0.019 | 0.624 | −0.007 | 0.852 |
| Being supportive of governmental measures | −0.098 | 0.064 | −0.060 | 0.182 |
| Perceived social support | −0.220 | <0.001 | −0.084 | 0.067 |
| Resilience | −0.185 | <0.001 | −0.197 | <0.001 |
| Method factor | −0.181 | 0.002 | −0.188 | <0.001 |
| R2 | 0.235 | 0.179 | ||
| n | 575 | 576 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gerhards, S.K.; Luppa, M.; Röhr, S.; Pabst, A.; Bauer, A.; Frankhänel, T.; Döhring, J.; Escales, C.; Zöllinger, I.R.; Oey, A.; et al. Depression and Anxiety in Old Age during the COVID-19 Pandemic: A Comparative Study of Individuals at Cardiovascular Risk and the General Population. Int. J. Environ. Res. Public Health 2023, 20, 2975. https://doi.org/10.3390/ijerph20042975
Gerhards SK, Luppa M, Röhr S, Pabst A, Bauer A, Frankhänel T, Döhring J, Escales C, Zöllinger IR, Oey A, et al. Depression and Anxiety in Old Age during the COVID-19 Pandemic: A Comparative Study of Individuals at Cardiovascular Risk and the General Population. International Journal of Environmental Research and Public Health. 2023; 20(4):2975. https://doi.org/10.3390/ijerph20042975
Chicago/Turabian StyleGerhards, Sina K., Melanie Luppa, Susanne Röhr, Alexander Pabst, Alexander Bauer, Thomas Frankhänel, Juliane Döhring, Catharina Escales, Isabel Renate Zöllinger, Anke Oey, and et al. 2023. "Depression and Anxiety in Old Age during the COVID-19 Pandemic: A Comparative Study of Individuals at Cardiovascular Risk and the General Population" International Journal of Environmental Research and Public Health 20, no. 4: 2975. https://doi.org/10.3390/ijerph20042975
APA StyleGerhards, S. K., Luppa, M., Röhr, S., Pabst, A., Bauer, A., Frankhänel, T., Döhring, J., Escales, C., Zöllinger, I. R., Oey, A., Brettschneider, C., Wiese, B., Hoffmann, W., Gensichen, J., König, H.-H., Frese, T., Thyrian, J. R., Kaduszkiewicz, H., & Riedel-Heller, S. G. (2023). Depression and Anxiety in Old Age during the COVID-19 Pandemic: A Comparative Study of Individuals at Cardiovascular Risk and the General Population. International Journal of Environmental Research and Public Health, 20(4), 2975. https://doi.org/10.3390/ijerph20042975







