A Pilot Study on Pharmacists’ Knowledge, Attitudes and Practices towards Medication Dysphagia via Asynchronous Online Focus Group Discussion
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. AOFG Platform
2.3. AOFG Discussion Guide
2.4. Participants and Recruitment
2.5. Procedure
2.6. Data Analysis
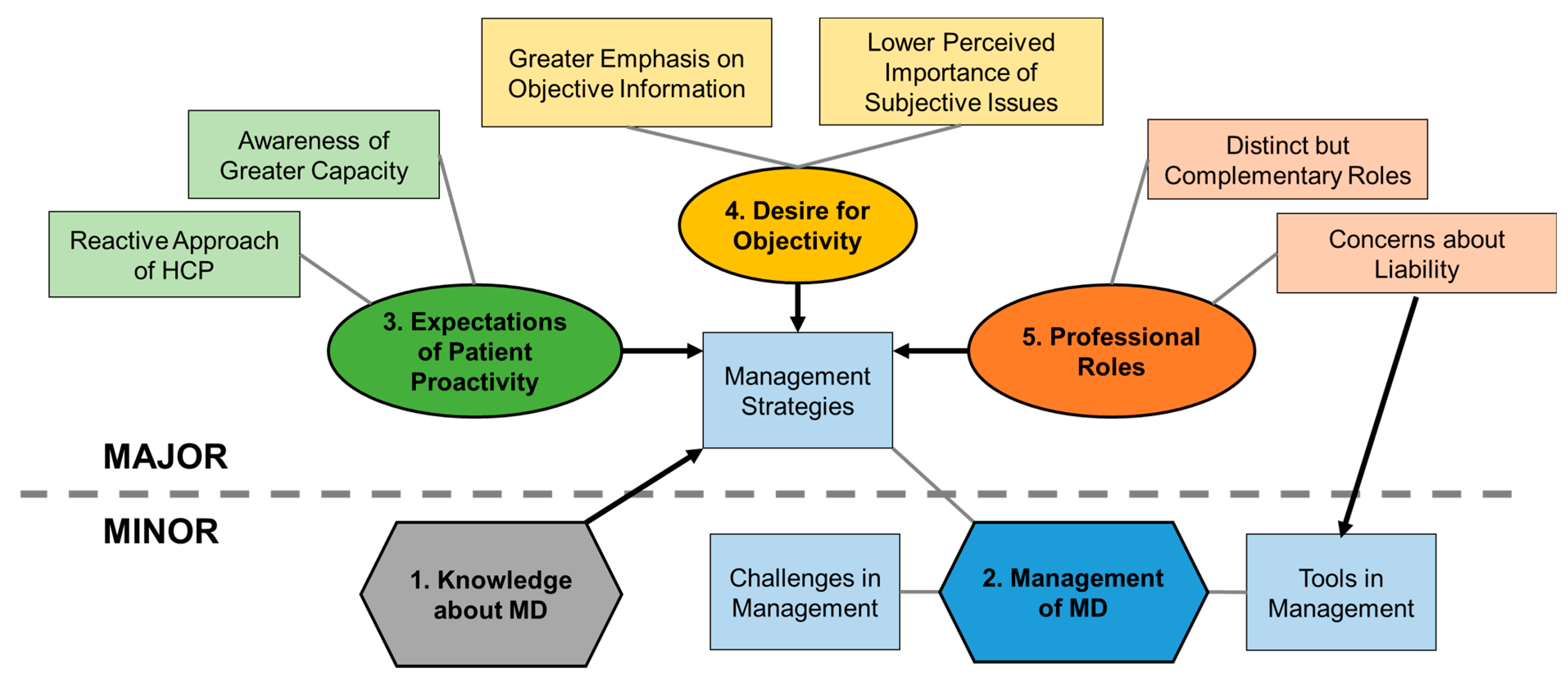
3. Results
3.1. Minor Theme: Knowledge about MD
3.2. Minor Theme: Management of MD
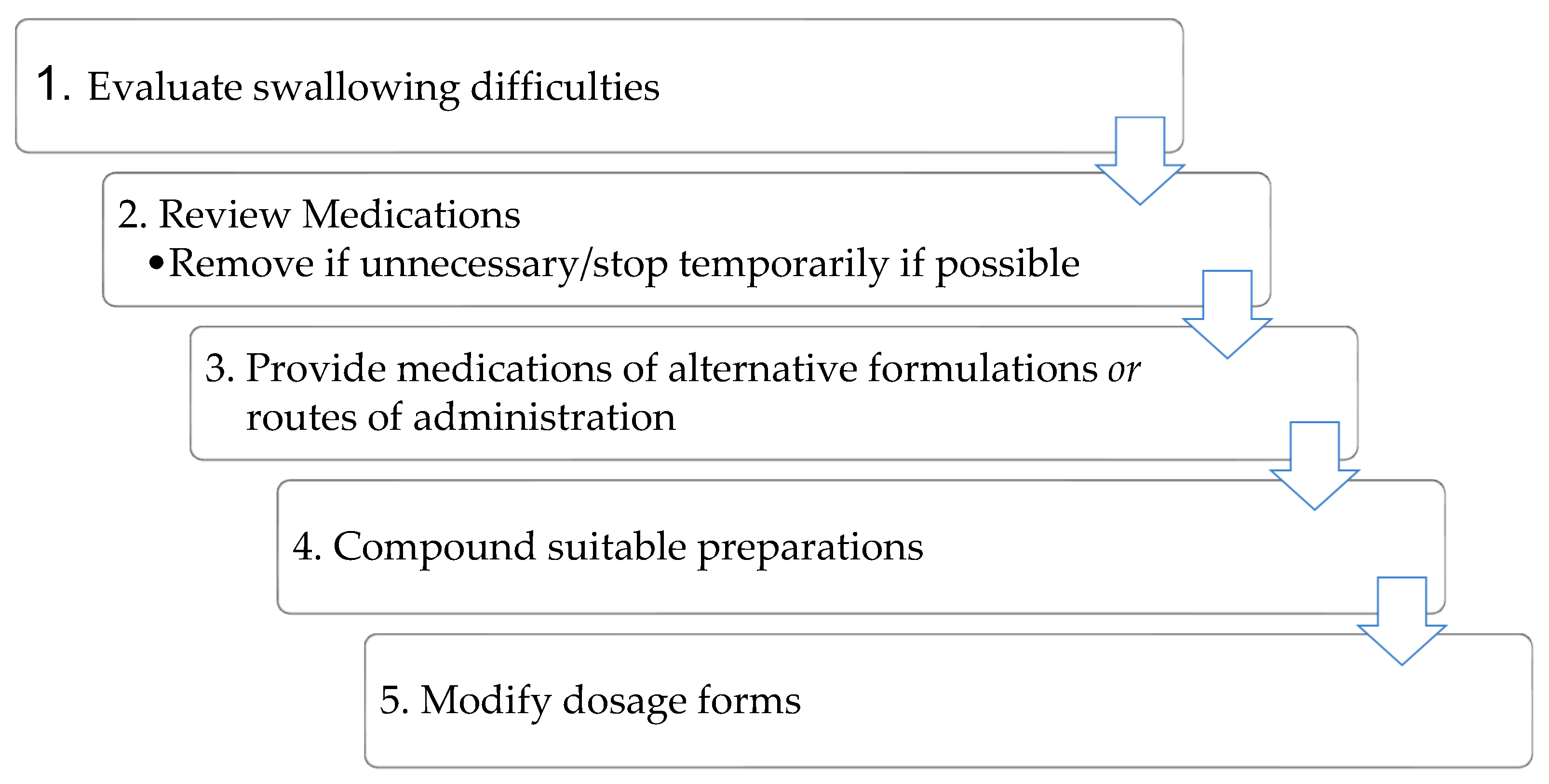
3.2.1. Sub-Theme: Management Strategies
3.2.2. Sub-Theme: Tools in Management
3.2.3. Sub-Theme: Challenges in Management
3.3. Major Theme: Expectations of Patient Proactivity
3.3.1. Sub-Theme: Awareness of Greater Capacity
3.3.2. Sub-Theme: Reactive Approach of HCPs
3.4. Major Theme: Desire for Objectivity
3.4.1. Sub-Theme: Greater Emphasis on Objective Information
3.4.2. Sub-Theme: Lower Perceived Importance of Subjective Issues
3.5. Major Theme: Professional Roles
3.5.1. Sub-Theme: Distinct but Complementary Roles
3.5.2. Sub-Theme: Concerns about Liability
4. Discussion
4.1. Knowledge
4.2. Management of MD
4.3. Expectations of Patient Proactivity
4.4. Desire for Objectivity
4.5. Professional Roles
4.6. Implications on Clinical Practice
4.7. Metholodogical Considerations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schiele, J.T.; Quinzler, R.; Klimm, H.D.; Pruszydlo, M.G.; Haefeli, W.E. Difficulties swallowing solid oral dosage forms in a general practice population: Prevalence, causes, and relationship to dosage forms. Eur. J. Clin. Pharmacol. 2013, 69, 937–948. [Google Scholar] [CrossRef]
- Proportion of Older Adults with Multiple Chronic Diseases Surges. Available online: https://www.sgh.com.sg/news/tomorrows-medicine/proportion-of-older-adults-with-multiple-chronic-diseases-surges (accessed on 26 November 2022).
- Health Promotion Board Singapore. Tips to Prevent and Manage Chronic Diseases in the Workplace. Available online: https://www.hpb.gov.sg/article/tips-to-prevent-and-manage-chronic-diseases-in-the-workplace (accessed on 11 March 2022).
- Lau, E.T.; Steadman, K.J.; Cichero, J.A.; Nissen, L.M. Dosage form modification and oral drug delivery in older people. Adv. Drug Deliv. Rev. 2018, 135, 75–84. [Google Scholar] [CrossRef]
- Forough, A.S.; Lau, E.T.; Steadman, K.J.; Cichero, J.A.; Kyle, G.J.; Serrano Santos, J.M.; Nissen, L.M. A spoonful of sugar helps the medicine go down? A review of strategies for making pills easier to swallow. Patient Prefer. Adherence 2018, 12, 1337–1346. [Google Scholar] [CrossRef]
- Farpour, S.; Farpour, H.R.; Smithard, D.; Kardeh, B.; Ghazaei, F.; Zafarghasempour, M. Dysphagia management in Iran: Knowledge, attitude and practice of healthcare providers. Dysphagia 2019, 34, 105–111. [Google Scholar] [CrossRef] [PubMed]
- National Center for Biotechnology Information, U.S. National Library of Medicine. Deglutition Disorders—MeSH. Available online: https://www.ncbi.nlm.nih.gov/mesh/68003680 (accessed on 11 March 2022).
- Stoschus, B.; Allescher, H.D. Drug-induced dysphagia. Dysphagia 1993, 8, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Nativ-Zeltzer, N.; Bayoumi, A.; Mandin, V.P.; Kaufman, M.; Seeni, I.; Kuhn, M.A.; Belafsky, P.C. Validation of the PILL-5: A 5-item patient reported outcome measure for pill dysphagia. Front. Surg. 2019, 6, 43. [Google Scholar] [CrossRef] [PubMed]
- Stegemann, S.; Gosch, M.; Breitkreutz, J. Swallowing dysfunction and dysphagia is an unrecognized challenge for oral drug therapy. Int. J. Pharm. 2012, 430, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.; D’Cruz, G.; Wright, D. Patients with dysphagia: Experiences of taking medication. J. Adv. Nurs. 2010, 66, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Lau, E.T.; Steadman, K.J.; Mak, M.; Cichero, J.A.; Nissen, L.M. Prevalence of swallowing difficulties and medication modification in customers of community pharmacists. J. Res. Pharm. Pract. 2015, 45, 18–23. [Google Scholar] [CrossRef]
- Tahaineh, L.; Wazaify, M. Difficulties in swallowing oral medications in Jordan. Int. J. Clin. Pharm. 2017, 39, 373–379. [Google Scholar] [CrossRef]
- Llorca, P.M. Discussion of prevalence and management of discomfort when swallowing pills: Orodispersible tablets expand treatment options in patients with depression. Ther. Deliv. 2011, 2, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Balzer, K.M. Drug-induced dysphagia. Int. J. MS Care 2000, 2, 40–50. [Google Scholar] [CrossRef]
- Logrippo, S.; Ricci, G.; Sestili, M.; Cespi, M.; Ferrara, L.; Palmieri, G.F.; Ganzetti, R.; Bonacucina, G.; Blasi, P. Oral drug therapy in elderly with dysphagia: Between a rock and a hard place! Clin. Interv. Aging 2017, 12, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.; D’Cruz, G.; Wright, D. A qualitative study of the problems surrounding medicine administration to patients with dysphagia. Dysphagia 2009, 24, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Wright, D.; Chapman, N.; Foundling-Miah, M.; Greenwall, R.; Griffith, R.; Guyon, A.; Merriman, H. Guideline on the Medication Management of Adults with Swallowing Difficulties. Available online: https://www.rosemontpharma.com/sites/default/files/20150911_adult_dysphagia_full_guideline_clean_approved_sept_15.pdf (accessed on 11 March 2022).
- Mc Gillicuddy, A.; Crean, A.M.; Sahm, L.J. Older adults with difficulty swallowing oral medicines: A systematic review of the literature. Eur. J. Clin. Pharmacol. 2016, 72, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Stubbs, J.; Haw, C.; Dickens, G. Dose form modification—A common but potentially hazardous practice. A literature review and study of medication administration to older psychiatric inpatients. Int. Psychogeriatr. 2008, 20, 616–627. [Google Scholar] [CrossRef] [PubMed]
- Griffith, R.; Tengnah, C. A guideline for managing medication related dysphagia. Br. J. Community Nurs. 2007, 12, 426–429. [Google Scholar] [CrossRef] [PubMed]
- Mercovich, N.; Kyle, G.J.; Naunton, M. Safe to crush? A pilot study into solid dosage form modification in aged care. Australas J. Ageing 2014, 33, 180–184. [Google Scholar] [CrossRef]
- Marquis, J.; Schneider, M.P.; Payot, V.; Cordonier, A.C.; Bugnon, O.; Hersberger, K.E.; Arnet, I. Swallowing difficulties with oral drugs among polypharmacy patients attending community pharmacies. Int. J. Clin. Pharm. 2013, 35, 1130–1136. [Google Scholar] [CrossRef]
- Strachan, I.; Greener, M. Medication-related swallowing difficulties may be more common than we realise. Pharm. Pract. 2005, 15, 411–414. [Google Scholar]
- Andrade, C.; Menon, V.; Ameen, S.; Kumar Praharaj, S. Designing and conducting knowledge, attitude, and practice surveys in psychiatry: Practical guidance. Indian J. Psychol. Med. 2020, 42, 478–481. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.; Clausen, M.G.; Robertson, A. Methodological reflections on the use of asynchronous online focus groups in health. Int. J. Qual. Methods 2012, 11, 368–383. [Google Scholar] [CrossRef]
- Zwaanswijk, M.; van Dulmen, S. Advantages of asynchronous online focus groups and face-to-face focus groups as perceived by child, adolescent and adult participants: A survey study. BMC Res. Notes 2014, 7, 756. [Google Scholar] [CrossRef] [PubMed]
- Reisner, S.L.; Randazzo, R.K.; White Hughto, J.M.; Peitzmeier, S.; DuBois, L.Z.; Pardee, D.J.; Marrow, E.; McLean, S.; Potter, J. Sensitive health topics with underserved patient populations: Methodological considerations for online focus group discussions. Qual. Health Res. 2018, 28, 1658–1673. [Google Scholar] [CrossRef]
- Ripat, J.; Colatruglio, A. Exploring winter community participation among wheelchair users: An online focus group. Occup. Ther. Health Care 2016, 30, 95–106. [Google Scholar] [CrossRef]
- Boateng, B.; Nelson, M.K.; Huett, A.; Meaux, J.B.; Pye, S.; Schmid, B.; Berg, A.; LaPorte, K.; Riley, L.; Green, A. Online focus groups with parents and adolescents with heart transplants: Challenges and opportunities. Pediatr. Nurs. 2016, 42, 120–123. [Google Scholar]
- Rolls, K.; Hansen, M.; Jackson, D.; Elliott, D. Why We Belong—Exploring membership of healthcare professionals in an intensive care virtual community Via Online Focus Groups: Rationale and Protocol. JMIR Res. Protoc. 2016, 5, e99. [Google Scholar] [CrossRef]
- Henderson, E.M.; Eccleston, C. An online adolescent message board discussion about the internet: Use for pain. J. Child Health Care 2015, 19, 412–418. [Google Scholar] [CrossRef]
- Lagan, B.M.; Sinclair, M.; Kernohan, W.G. What is the impact of the Internet on decision-making in pregnancy? A global study. Birth 2011, 38, 336–345. [Google Scholar] [CrossRef]
- Yu, J.; Taverner, N.; Madden, K. Young people’s views on sharing health-related stories on the Internet. Health Soc. Care Community 2011, 19, 326–334. [Google Scholar] [CrossRef]
- Stefansdottir, V.; Johannsson, O.T.; Skirton, H.; Jonsson, J.J. Counsellee’s experience of cancer genetic counselling with pedigrees that automatically incorporate genealogical and cancer database information. J. Community Genet. 2016, 7, 229–235. [Google Scholar] [CrossRef] [PubMed]
- FocusGroupIt. Focus Groups Made Easy. Available online: https://www.focusgroupit.com/ (accessed on 11 March 2022).
- NowComment. Turning Texts, Images & Videos into Conversations. Available online: https://nowcomment.com/ (accessed on 11 March 2022).
- Discourse. Civilized Discussion for your _____. Available online: https://www.discourse.org/ (accessed on 11 March 2022).
- NING. All You Need for a Perfect Website. Available online: https://www.ning.com/features/ (accessed on 11 March 2022).
- Microsoft Teams. Make Amazing Things Happen Together at Home, Work, and School. Available online: https://www.microsoft.com/en/microsoft-teams/group-chat-software (accessed on 11 March 2022).
- Collabito. Bulletin Board Focus Groups. Available online: https://www.collabito.com/online-bulletin-board-focus-group/ (accessed on 11 March 2022).
- Kialo. Kialo Edu—The tool to Teach Critical Thinking and Rational Debate. Available online: https://www.kialo-edu.com/ (accessed on 11 March 2022).
- YoTeach by PALMS. The New Alternative to Todaysmeet. Available online: https://yoteachapp.com/ (accessed on 11 March 2022).
- Backchannel Chat. Backchannel Chat Will Change the Way You Think about Safe Online Chat. Available online: http://backchannelchat.com/Benefits (accessed on 11 March 2022).
- L-Soft International, I. LISTSERV Email List Management Software. Available online: http://www.lsoft.com/products/listserv.asp (accessed on 11 March 2022).
- MH Sub I Ldv. Feature Comparison: VB5 vs. VBCloud. Available online: https://www.vbulletin.com/en/vbcloud-features (accessed on 11 March 2022).
- itracks. Board–itracks. Available online: https://www.itracks.com/products-services/board/ (accessed on 11 March 2022).
- Community I. Invision Community Features—Powerful Community Apps to Delight Users–Invision Community. Available online: https://invisioncommunity.com/features/content/ (accessed on 11 March 2022).
- FluxBB. Feature List—FluxBB. Available online: https://fluxbb.org/about/features.html (accessed on 11 March 2022).
- phpBB Forum Software. The #1 Free, Open Source Bulletine Board Software. Available online: https://www.phpbb.com/ (accessed on 11 March 2022).
- Johansson, E. How Can Remote Communication Be Made More Accessible to People with Communication Disabilities? An Online Focus Group Study with Support Persons to People with Communication Disabilities in Need of Augmentative and Alternative Communication (AAC). Master’s Thesis, Chalmers University of Technology, Gothenburg, Sweden, 2019. [Google Scholar]
- McLafferty, I. Focus group interviews as a data collecting strategy. J. Adv. Nurs. 2004, 48, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Maguire, M.; Delahunt, B. Doing a thematic analysis: A practical, step-by-step guide for learning and teaching scholars. All Irel. J. High. Educ. 2017, 9, 3351–33514. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Gibbs, G.R. Thematic coding and categorizing. In Analyzing Qualitative Data; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 2007; pp. 38–55. [Google Scholar]
- Nguyen, T.M.U.; Lau, E.; Steadman, K.; Cichero, J.; Dingle, K.; Nissen, L. Pharmacist, general practitioner, and nurse perceptions, experiences, and knowledge of medication dosage form modification. Integr. Pharm. Res. Pract. 2014, 2014, 3. [Google Scholar]
- Meltzer, E.O.; Welch, M.J.; Ostrom, N.K. Pill swallowing ability and training in children 6 to 11 years of age. Clin. Pediatr. 2006, 45, 725–733. [Google Scholar] [CrossRef]
- Dorman, R.M.; Sutton, S.H.; Yee, L.M. Understanding HIV-related pill aversion as a distinct barrier to medication adherence. Behav. Med. 2019, 45, 294–303. [Google Scholar] [CrossRef]
- Shapiro, J.; Franko, D.L.; Gagne, A. Phagophobia: A form of psychogenic dysphagia. A new entity. Ann. Otol. Rhinol. Laryngol. 1997, 106, 286–290. [Google Scholar]
- Macleod, A.D.; Vella-Brincat, J.; Frampton, C. Swallowing capsules. Palliat. Med. 2003, 17, 559. [Google Scholar] [CrossRef]
- Budget Debate: More Healthcare Workers Needed in Coming Years. Available online: https://www.straitstimes.com/singapore/politics/budget-debate-more-healthcare-workers-needed-in-coming-years (accessed on 26 November 2022).
- World Health Organization. Global Health Workforce Shortage to Reach 12.9 Million in Coming Decades. 2013. Available online: https://www.who.int/mediacentre/news/releases/2013/health-workforce-shortage/en/ (accessed on 28 March 2021).
- Picton, C.; Wright, H. Medicines Optimisation: Helping Patients to Make the Most of Medicines. Available online: https://www.nhs.uk/about-the-nhs-website/professionals/healthandcareprofessionals/your-pages/documents/rps-medicines-optimisation.pdf (accessed on 28 March 2021).
- Barnes, L.; Cheek, J.; Nation, R.L.; Gilbert, A.; Paradiso, L.; Ballantyne, A. Making sure the residents get their tablets: Medication administration in care homes for older people. J. Adv. Nurs. 2006, 56, 190–199. [Google Scholar] [CrossRef]
- Tan, P.L.; Chung, W.L.; Sklar, G.E.; Yap, K.Z.; Chan, S.Y. Development and validation of the INappropriate solid oral dosaGE form modification aSsessmenT (INGEST) Algorithm using data of patients with medication dysphagia from a neurology ward and nursing home in Singapore. BMJ Open 2022, 12, e061774. [Google Scholar] [CrossRef] [PubMed]
- Breen, R.L. A practical guide to focus-group research. J. Geogr. High Educ. 2006, 30, 463–475. [Google Scholar] [CrossRef]
- Onwuegbuzie, A.J.; Dickinson, W.B.; Leech, N.L.; Zoran, A.G. A qualitative framework for collecting and analyzing data in focus group research. Int. J. Qual. Methods 2009, 8, 1–21. [Google Scholar] [CrossRef]
| Features of the AOFG Format | Postulated Benefits |
|---|---|
| Participation from any location with internet access | Minimization of health and safety risks amidst a pandemic |
| Participants can respond at a time of their choice/convenience during the study | Flexibility of time for potentially better response rates [26,28,29] |
| Elicitation of more thoughtful responses by removing the need for an immediate answer [26,29] | |
| Participant anonymity | Minimization of social desirability bias and power imbalances to disinhibit participants and facilitate honest discussion [26,28] |
| Direct input of data by participants | Improved accuracy and time-savings in data collection [26,28,29] |
| Direct download of participants’ responses |
| Theme | Topic | Exemplar Quotes (Participant) |
|---|---|---|
| Knowledge about medication dysphagia | Low prevalence | “Maybe about 5% … I don’t think this is representative of Singapore’s population as I rarely see children in my practice” (#7) |
| MD assumed in children and elderly | “Most common group: children…medication dysphagia is relevant in virtually all pediatric patients I see…2nd most common group: elderly patients…” (#3) | |
| MD assumed absent in adults | “In adults…we generally assume patients has no difficulty swallowing medications until they voice out the problem.” (#4) | |
| Temporary nature of MD in children | “Definitely most common in children. Sometimes this carry through to teens and adulthood” (#5) | |
| Persistent nature of MD | “If … there’s no durable alternative for patient, we can…” (#4) | |
| Coping strategies of DFM and non-adherence Patients unaware of implications of DFM | “I agree that patients may just crush the medication, cut it, attempt to dissolve the tablet or open up the capsules. I have also encountered some anecdotal evidence from caregivers that some patients just do not take the medication. Patients are likely not cognizant that the actions of modifying the medication may alter the intended PK properties of the medication, increase adverse effects or even render the medication less or ineffective.” (#5) | |
| Patients’ perceived benefits and non-adherence | “Depends on how the patient view the medication. (1) Patient does not view the medication as something ‘real’ or ‘important’…more likely that patient will just default their medication” (#1) |
| Theme | Subtheme | Topic | Exemplar Quotes (Participant) |
|---|---|---|---|
| Management of Medication Dysphagia | Management Strategies | Confidence in managing MD | “I am confident of caring for patients with medication dysphagia…” (#5) |
| DFM and switching formulations | “… figure out if there’s anything that can be done before considering alternative agents e.g., tablet too large -> cut or crush the tablets if possible, or find a liquid product if possible.” (#3) | ||
| Other MD management strategies | “The last resort might be to switch to another drug within the same class…” (#7) “…team would assess and decide if patients needs referral to speech therapist…” (#4) “…I would take a reassuring and encouraging stance” (#6) “…tilting the head slightly back helps with tablets and tilting slightly forward helps with capsules. Not sure how useful this is since I never really had the chance to try advising this in actual practice or to search for corroborating references.” (#3) “Is there a way to “train” individuals to swallow pills?” (#4) | ||
| Partial agreement with MD management plan | “While I agree with the algorithm in principle, I find it hard for me as a pharmacist to properly evaluate a patient’s swallowing difficulties…but don’t consider compounding to be a realistic option” (#3) | ||
| Tools in Management | Consulting references for DFM suitability | “(i) Product inserts is a good source of information that pharmaceutical companies can guide how the medication can be handled (ii) institutional/in house guidelines would have a collated list of medications and alternatives to recommend i.e., how to modify to accommodate patients with med dysphagia” (#6) | |
| Consulting colleagues | “I would turn to seniors when in doubt… to pharmacists who are handling HIV clinics, or oncology patients or even contact pharmacists at our cancer center pharmacy” (#4) | ||
| Expertise of other professions required | “I would feel that as pharmacists, we would be suited to advise on the medication administration and formulation concerns. But speech therapists would be in a better position to evaluate and manage the patient.” (#6) | ||
| Challenges in Management | Lack expertise in evaluation | “I agree with the other participants that as pharmacists, we are not trained to evaluate swallowing difficulties” (#5) | |
| Lack of time | “I don’t usually screen for medication dysphagia …also because it takes up too much time, especially when I have to check for other medical/medication history. It takes more time to manage their medication dysphagia problems as well” (#3) | ||
| Missing information from references | “…in-house NGT guide for common medications whether they can be crushed and possible alternatives. However, the list is non-exhaustive and not updated frequently.” (#4) | ||
| Availability issues | “…liquid alternatives are usually available in varying rarities…” (#3) | ||
| Different pharmaco-kinetic profile of alternative formulations | “provide medications of alternative formulations (if available) and/or routes of administration (even though the bioavailability and onset of action of medication may be altered).” (#6) | ||
| Prescriber resistance | “I once had trouble convincing a prescriber to consider alternatives for a patient…” (#3) |
| Theme | Subtheme | Topic | Exemplar Quotes (Participant) |
|---|---|---|---|
| Expectations of Patient Proactivity | Awareness of Greater Capacity | Earlier identification of MD | “I think it is most likely to be discovered in the administering stage.” (#2) “Yes, if HCP could identify during the prescribing or dispensing phase by asking the patient or caregiver if there’s any difficulty or issues with medication…” (#4) |
| Acknowledging more could be done | “Currently, we are still more ‘reactive’ in identifying them.” (#1) “I have never thought of how to guide patient in identifying medication dysphagia. Hopefully there are validated questions out there that is easy to administer. (I have yet to do my lit-search).” (#1) | ||
| Reactive Approach of HCPs | Reliance on patient/caregiver reporting | “Unfortunately, I don’t actively screen for medication dysphagia in these patients. It may not be something that actively comes to my mind in a busy day. I will address it if patients or family members bring up the issue.” (#2) | |
| Conditional screening for MD | “The only time where we will actively ask is when I am dispensing the medication for a child below 12 years old.” (#1) “I find out when I ask them regarding any medication dysphagia, if I am dispensing medications that must be swallowed whole. For med recon inpatient, the presence of medication dysphagia is routinely asked as well.” (#7) | ||
| Extended expectations of patient proactivity | “Patients probably aren’t aware of such implications as they weren’t informed, though some may discuss with a HCP or google about their medications then they could be aware” (#4) “They would … or simply check with a family member.” (#6) |
| Theme | Subtheme | Topic | Exemplar Quotes (Participant) |
|---|---|---|---|
| Desire for Objectivity | Greater Emphasis on Objective Information | Seeking objective information | “Find out more details regarding his/her past experience with medication dysphagia e.g., -what medication/supplement caused the problem -what was the problem exactly e.g., burning sensation in the throat after swallowing doxycycline, problems swallowing calcium supplements” (#3) |
| Subjective factors of MD | “Well, it can happen earlier if the tablet is large…” (#6) “…if I can see medical records and see medical conditions that may predispose a patient to medication dysphagia, this will help me identify patients…” (#3) | ||
| “Came across patients with psychological issues that exhibit this.” (#5) “Subsequently, there may be some effort in determining if there is a concern about ‘taking medication’ (negative association with medicine, such as medication damaging the kidney, being addicted, being reliant, etc).” (#1) | |||
| Change in approach after obtaining additional objective information | “One thing I would additionally advise the patient is to ask the doctor managing his/her post-stroke care regarding possibility of seeking the expertise of a speech therapist for managing the dysphagia” (#3) | ||
| Lower Perceived Importance of Subjective issues | Prioritization of other tasks and issues above MD | “I don’t usually screen for medication dysphagia…because it takes up too much time, especially when I have to check for other medical/medication history.” (#3) | |
| “Most of the emphasis is placed on clinical dysphagia. Come to think of it, there are not much communication about medication dysphagia.” (#1) | |||
| Expression of scepticism to subjective factors and MD | “…there is a ‘psychological’ barrier…” (#5) “Given the recent stroke, the possibility of having a ‘real’ medication dysphagia/clinical dysphagia is higher” (#1) |
| Theme | Subtheme | Topic | Exemplar Quotes (Participant) |
|---|---|---|---|
| Professional Roles | Distinct but Complementary Roles | Kept within scope of practice | “caring for patients with medication dysphagia—through seeking alternatives in liquid preparations and crushing of solid preparations” (#5) |
| Team-centric approach | “…I would recommend that each step should be performed by different HCP, such as step 1 can be performed by Dr or speech therapist as they would be more appropriate to evaluate the patient’s swallowing difficulty…Modify dosage forms: Performed by nurses where they are the ones administering the medications…” (#4) | ||
| “I will be comfortable providing information to colleagues about the medication-related needs… I think doctors are best placed to assess this problem, though as mentioned, a multi-disciplinary involvement can be the final model.” (#5) | |||
| Direct patients to ask other HCPs | “…I would just recommend discussing this with the dr” (#3) | ||
| Inter-professional communication difficulties | “more limited access to communicate with prescribers” (#3) | ||
| Limited inter-professional communication | “I usually find out…through the SOAP notes/counselling notes of doctors/pharmacy colleagues” (#5) “Similarly I will include the issue and management under counselling remarks to keep my pharmacy colleagues in the loop” (#5) “Usually I’m among the last to find out, so there’s no need to communicate this information.” (#3) | ||
| Concerns about Liability | Administration instructions as minimum standards | “Due diligence probably ends at the point where the information of ‘swallow whole, do not crush’ is being presented to patient.” (#1) | |
| Checking DFM suitability | “Crushing tablets will only be suggested if it is stated in the PIL. Most people are concern of recommending any action that is not stated in the PIL.” (#1) | ||
| Obtaining prescriber approval | “…we should do our due diligence to run a check with the physicians to ensure a concurrence that modification of medications are made to accommodate the patient…” (#6) | ||
| Raising minimum standards | “However, if sufficient consideration is given to the capacity of the pharmacist to provide more detailed counselling (allow more time per consultation session), then I may be receptive to higher standards of due diligence…” (#3) | ||
| Screening for MD beyond minimum standards | “Going the extra mile perhaps meant asking the patient actively: do you think you will have problem swallowing the tablet.” (#1) | ||
| DFM of patient’s volition | “However, if the patient decide to modify the medication without discussing with the healthcare professional, or modifying the medication even it is advised against, then it is at their own risk.” (#1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tan, P.L.; Loh, T.J.; Chan, S.Y. A Pilot Study on Pharmacists’ Knowledge, Attitudes and Practices towards Medication Dysphagia via Asynchronous Online Focus Group Discussion. Int. J. Environ. Res. Public Health 2023, 20, 2858. https://doi.org/10.3390/ijerph20042858
Tan PL, Loh TJ, Chan SY. A Pilot Study on Pharmacists’ Knowledge, Attitudes and Practices towards Medication Dysphagia via Asynchronous Online Focus Group Discussion. International Journal of Environmental Research and Public Health. 2023; 20(4):2858. https://doi.org/10.3390/ijerph20042858
Chicago/Turabian StyleTan, Poh Leng, Terence JunHeng Loh, and Sui Yung Chan. 2023. "A Pilot Study on Pharmacists’ Knowledge, Attitudes and Practices towards Medication Dysphagia via Asynchronous Online Focus Group Discussion" International Journal of Environmental Research and Public Health 20, no. 4: 2858. https://doi.org/10.3390/ijerph20042858
APA StyleTan, P. L., Loh, T. J., & Chan, S. Y. (2023). A Pilot Study on Pharmacists’ Knowledge, Attitudes and Practices towards Medication Dysphagia via Asynchronous Online Focus Group Discussion. International Journal of Environmental Research and Public Health, 20(4), 2858. https://doi.org/10.3390/ijerph20042858





