Association between Cardiovascular Disease Risk Factors and Cardiorespiratory Fitness in Firefighters: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Summary of Methods
- (i)
- Studies that included full-time, part-time, and volunteer adult male and female firefighters between the ages of 18 and 65 years;
- (ii)
- Cross-sectional, observational, and experimental (intervention) study designs;
- (iii)
- Studies that investigated the association between CVD risk factors or health metrics and cardiorespiratory fitness in firefighters;
- (iv)
- Studies that were available in full text or that could be acquired through a request from the authors.
- (i)
- Studies that failed to mention exposure and outcome measures, such as cardiorespiratory fitness and risk factors for cardiovascular disease;
- (ii)
- Various forms of reviews, such as systematic reviews, literature reviews, scoping reviews, etc.;
- (iii)
- Non-English language articles.
2.2. Study Selection, Screening, and Data Management
2.3. Critical Appraisal of Included Studies
2.4. Study Selection
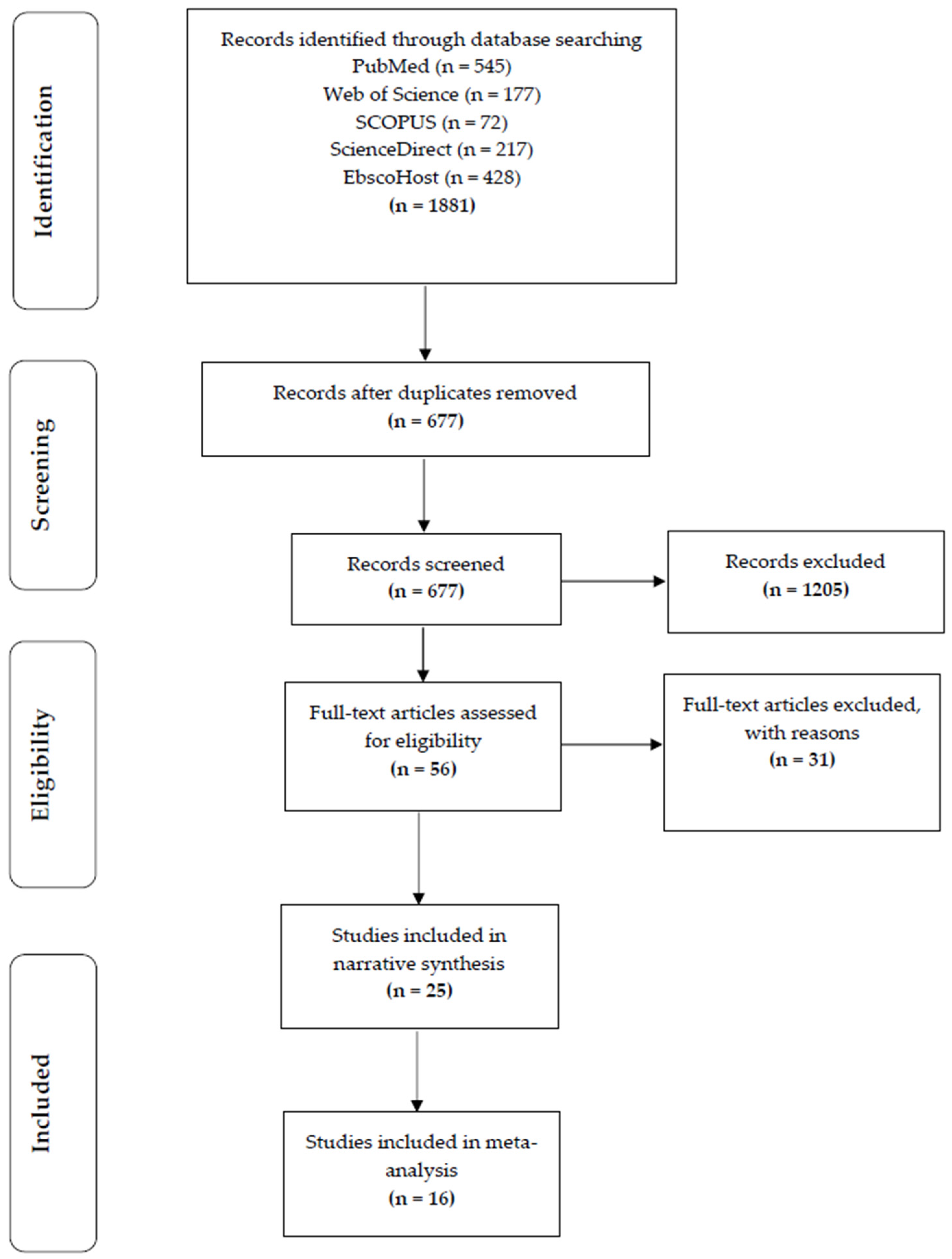
2.5. Data Analysis
2.5.1. Assessment of Overall Effect Size
- Very high correlation, from 0.90 to 1.00 (−0.90 to −1.00);
- High correlation, from 0.70 to 0.90 (−0.70 to −0.90);
- Moderate correlation, from 0.50 to 0.70 (−0.50 to −0.70);
- Low correlation, from 0.30 to 0.50 (−0.30 to −0.50);
- Negligible correlation, from 0.00 to 0.30 (−0.00 to −0.30).
2.5.2. Classification of Cardiovascular Disease Risk Factors and Cardiorespiratory Fitness
2.5.3. Assessment of Heterogeneity and Publication Bias
- (i)
- From 0% to 30%, indicated heterogeneity may not be important;
- (ii)
- From 31% to 60%, indicated that there was moderate heterogeneity;
- (iii)
- From 61% to 80%, indicated that there was substantial heterogeneity;
- (iv)
- From 81% to 100%, indicated that there was considerable heterogeneity.
2.5.4. Risk of Bias
2.5.5. Subgroup Analysis and Investigation of Heterogeneity
3. Results
3.1. Study Characteristics
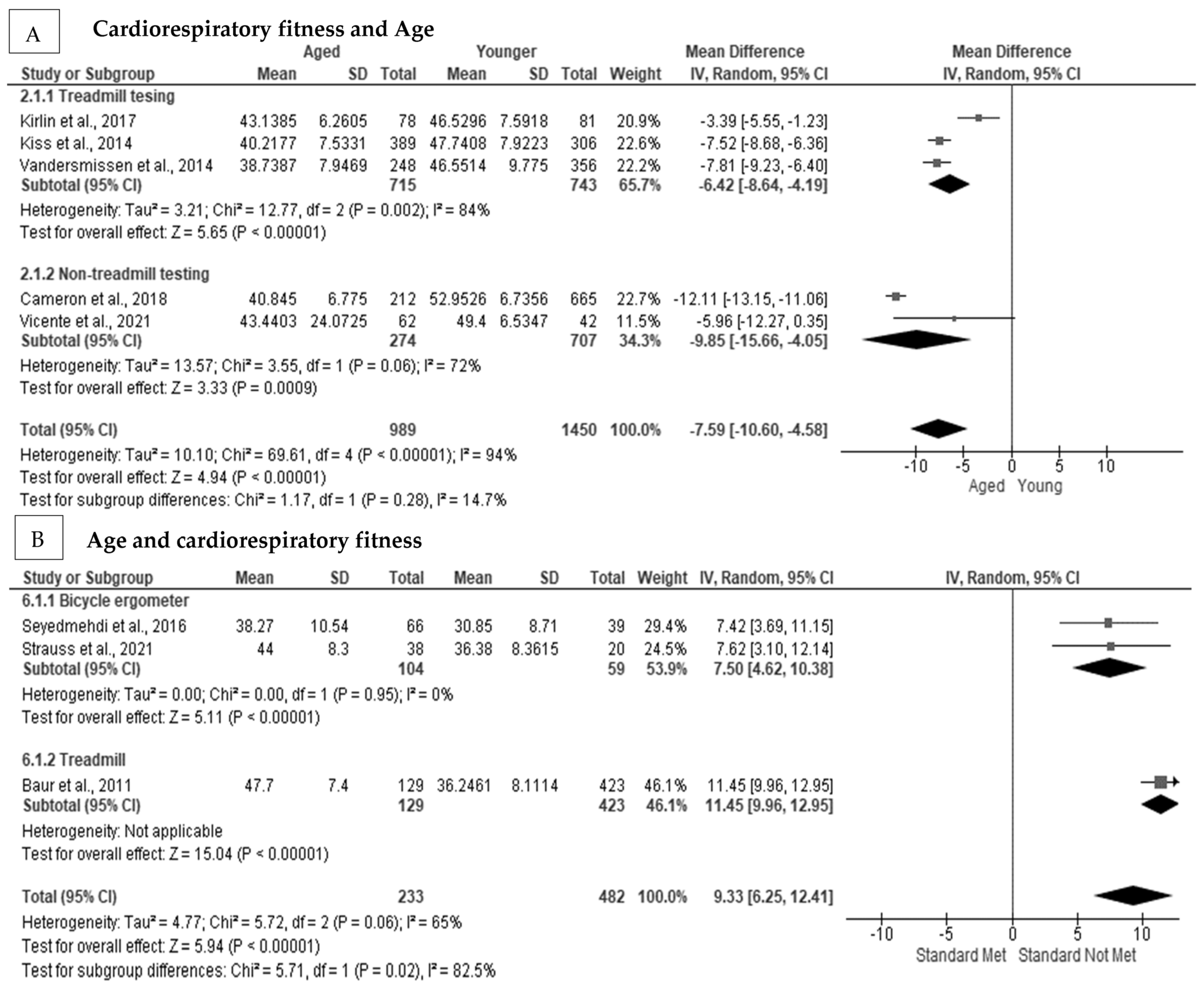
3.2. The Association between Aging and Cardiorespiratory Fitness in Firefighters
3.3. The Association between Obesity and Cardiorespiratory Fitness in Firefighters
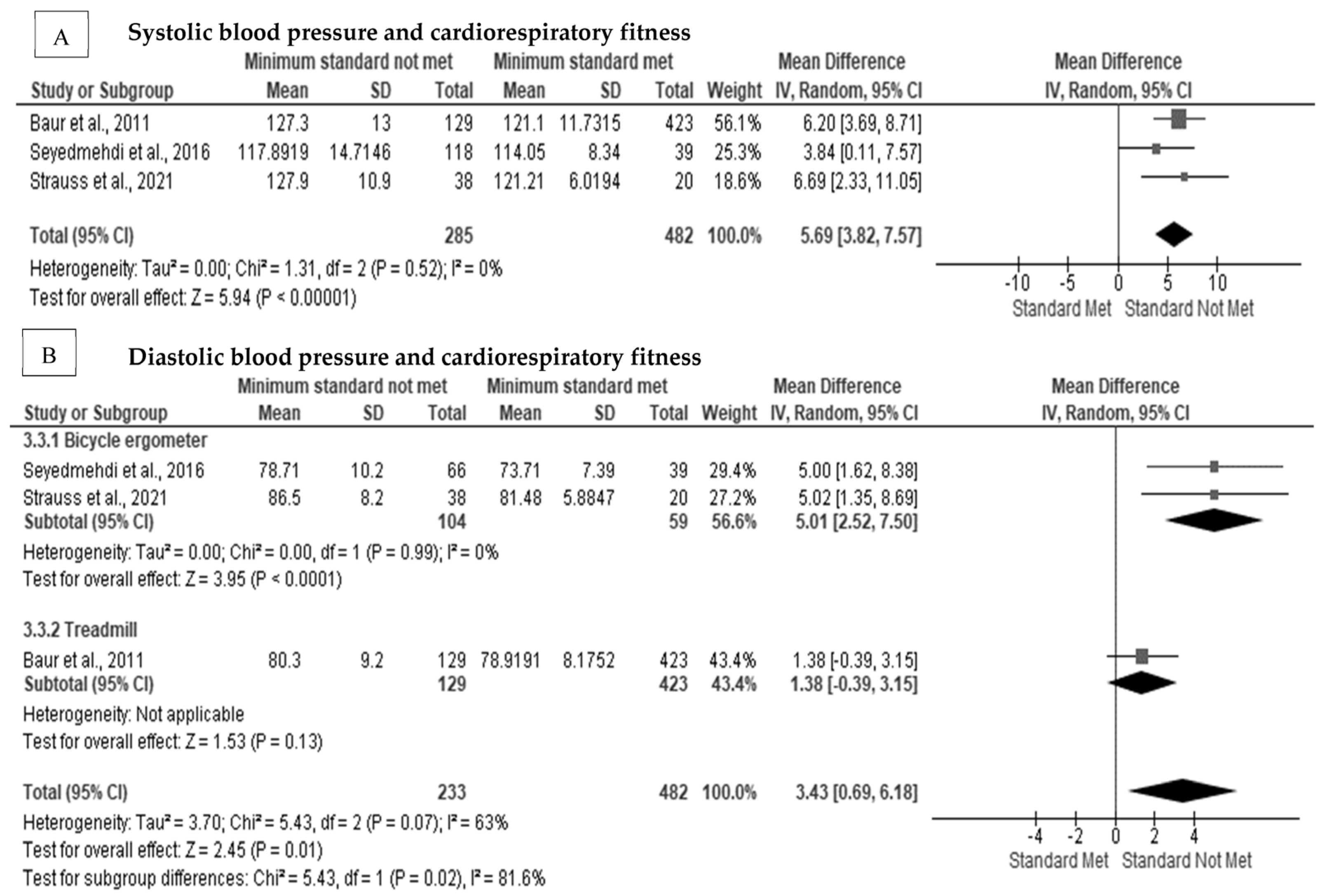
3.4. The Effect of Cardiorespiratory Fitness on Blood Pressure in Firefighters
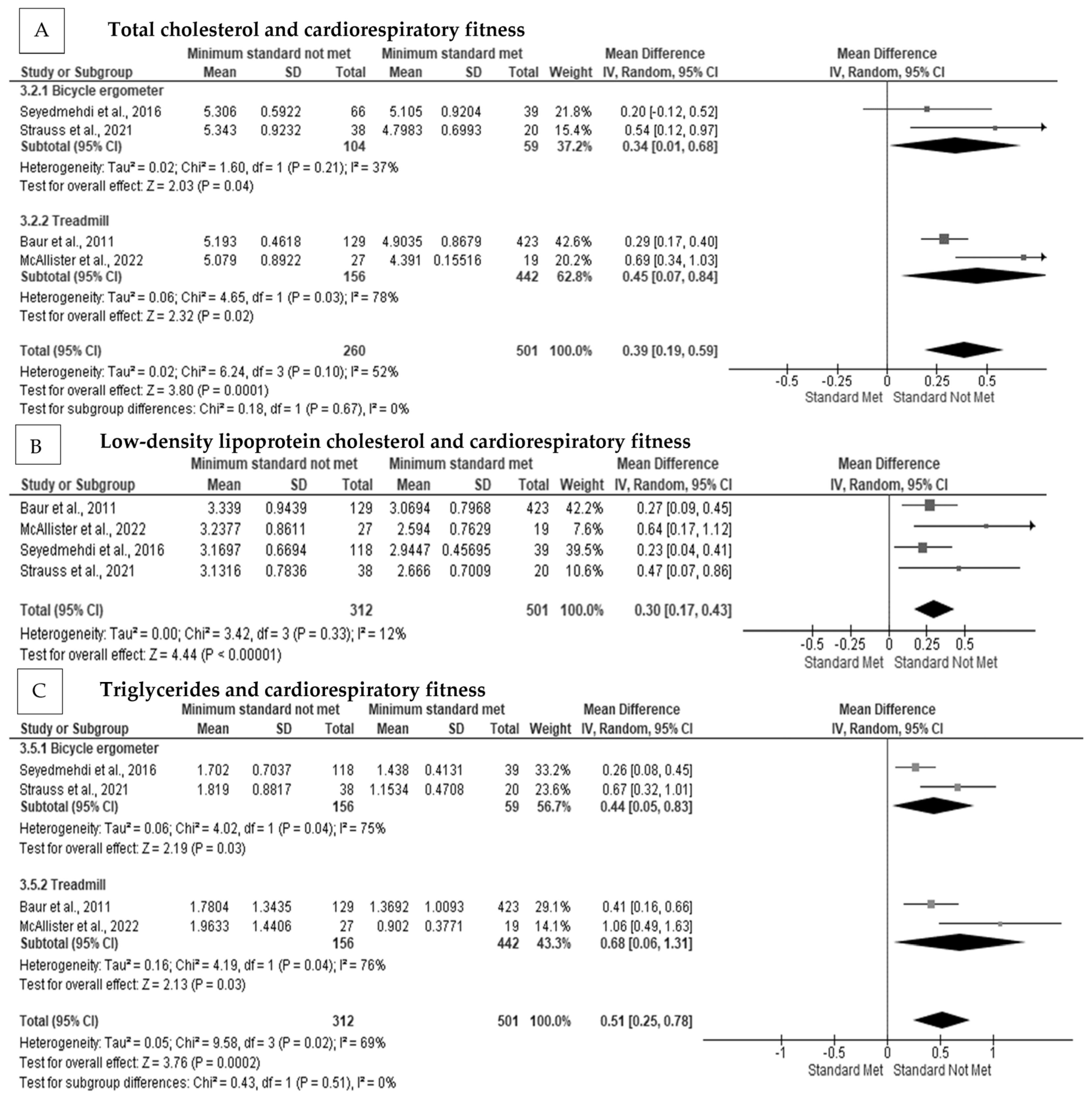
3.5. The Effect of Cardiorespiratory Fitness on Blood Cholesterol Concentration in Firefighters
3.6. The Effect of Cardiorespiratory Fitness on Blood Glucose in Firefighters
3.7. The Associations between Cigarette Smoking, Physical Inactivity, CVD Risk, and Heart Rate Variability and Cardiorespiratory Fitness in Firefighters
3.8. Correlations between Cardiovascular Disease Risk Factors and Cardiorespiratory Fitness
4. Discussion
4.1. Summary of Evidence
4.2. Cardiovascular Disease Risk Factors and Cardiorespiratory Fitness
4.3. Strengths and Limitations
5. Conclusions
6. Patents
Protocol Registration
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smith, D.L.; Haller, J.M.; Korre, M.; Sampani, K.; Porto, L.G.G.; Fehling, P.C.; Christophi, C.A.; Kales, S.N. The Relation of Emergency Duties to Cardiac Death Among US Firefighters. Am. J. Cardiol. 2019, 123, 736–741. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.L.; Barr, D.A.; Kales, S.N. Extreme Sacrifice: Sudden Cardiac Death in the US Fire Service. Extrem. Physiol. Med. 2013, 2, 6. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.L.; DeBlois, J.P.; Kales, S.N.; Horn, G.P. Cardiovascular Strain of Firefighting and the Risk of Sudden Cardiac Events. Exerc. Sport Sci. Rev. 2016, 44, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Soteriades, E.S.; Smith, D.L.; Tsismenakis, A.J.; Baur, D.M.; Kales, S.N. Cardiovascular Disease in US Firefighters: A Systematic Review. Cardiol. Rev. 2011, 19, 202–215. [Google Scholar] [CrossRef]
- Henderson, N.D.; Berry, M.W. Field Measures of Strength and Fitness Predict Firefighter Performance on Physically Demanding Tasks. Pers. Psychol. 2007, 60, 431–473. [Google Scholar] [CrossRef]
- Marcel-Millet, P.; Ravier, G.; Grospretre, S.; Gimenez, P.; Freidig, S.; Groslambert, A. Physiological Responses and Parasympathetic Reactivation in Rescue Interventions: The Effect of the Breathing Apparatus. Scand. J. Med. Sci. Sports 2018, 28, 2710–2722. [Google Scholar] [CrossRef]
- Taylor, N.A.S.; Lewis, M.C.; Notley, S.R.; Peoples, G.E. A Fractionation of the Physiological Burden of the Personal Protective Equipment Worn by Firefighters. Eur. J. Appl. Physiol. 2012, 112, 2913–2921. [Google Scholar] [CrossRef]
- Li, J.; Wang, Y.; Jiang, R.; Li, J. Quantifying Self-Contained Breathing Apparatus on Physiology and Psychological Responses during Firefighting: A Systematic Review and Meta-Analysis. Int. J. Occup. Saf. Ergon. 2022. [Google Scholar] [CrossRef]
- Ras, J.; Leach, L. Prevalence of Coronary Artery Disease Risk Factors in Firefighters in the City of Cape Town Fire and Rescue Service–A Descriptive Study. J. Public Health Res. 2021, 10. [Google Scholar] [CrossRef]
- Risavi, B.L.; Staszko, J. Prevalence of Risk Factors for Coronary Artery Disease in Pennsylvania (USA) Firefighters. Prehosp. Disaster. Med. 2015, 31, 102–107. [Google Scholar] [CrossRef]
- Smith, D.L.; Graham, E.; Stewart, D.; Mathias, K.C. Cardiovascular Disease Risk Factor Changes Over 5 Years Among Male and Female US Firefighters. J. Occup. Environ. Med. 2020, 62, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Drew-Nord, D.C.; Hong, O.S.; Froelicher, E.S. Cardiovascular Risk Factors among Career Firefighters. AAOHN J. 2009, 57, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Farioli, A.; Yang, J.; Teehan, D.; Baur, D.M.; Smith, D.L.; Kales, S.N. Duty-Related Risk of Sudden Cardiac Death among Young US Firefighters. Occup. Med. (Chic Ill) 2014, 64, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.L. Firefighter Fitness: Improving Performance and Preventing Injuries and Fatalities. Curr. Sports Med. Rep. 2011, 10, 167–172. [Google Scholar] [CrossRef]
- Smith, D.L.; Haller, J.M.; Benedict, R.; Moore-merrell, L. Cardiac Strain Associated with High-Rise Firefighting. J. Occup. Environ. Hyg. 2015, 12, 213–221. [Google Scholar] [CrossRef]
- Soares, E.M.K.V.K.; Smith, D.; Grossi Porto, L.G. Worldwide Prevalence of Obesity among Firefighters: A Systematic Review Protocol. BMJ Open 2020, 10, e031282. [Google Scholar] [CrossRef]
- Choi, B.K.; Steiss, D.; Garcia-Rivas, J.; Kojaku, S.; Schnall, P.; Dobson, M.; Baker, D. Comparison of Body Mass Index with Waist Circumference and Skinfold-Based Percent Body Fat in Firefighters: Adiposity Classification and Associations with Cardiovascular Disease Risk Factors. Int. Arch. Occup Environ. Health 2016, 89, 435–448. [Google Scholar] [CrossRef]
- Damacena, F.C.; Batista, T.J.; Ayres, L.R.; Zandonade, E.; Sampaio, K.N. Obesity Prevalence in Brazilian Firefighters and the Association of Central Obesity with Personal, Occupational and Cardiovascular Risk Factors: A Cross-Sectional Study. BMJ Open 2020, 10, e032933. [Google Scholar] [CrossRef]
- Nogueira, E.C.; Porto, L.G.G.; Nogueira, R.M.; Martins, W.R.; Fonseca, R.M.C.; Lunardi, C.C.; de Oliveira, R.J. Body Composition Is Strongly Associated with Cardiorespiratory Fitness in a Large Brazilian Military Firefighter Cohort: The Brazilian Firefighters Study. J. Strength Cond. Res. 2016, 30, 33–38. [Google Scholar] [CrossRef]
- Choi, B.K.; Schnall, P.; Dobson, M. Twenty-Four-Hour Work Shifts, Increased Job Demands, and Elevated Blood Pressure in Professional Firefighters. Int. Arch. Occup. Environ. Health 2016, 89, 1111–1125. [Google Scholar] [CrossRef]
- Choi, B.; Dobson, M.; Schnall, P.; Garcia-Rivas, J. 24-Hour Work Shifts, Sedentary Work, and Obesity in Male Firefighters. Am. J. Ind. Med. 2016, 59, 486–500. [Google Scholar] [CrossRef] [PubMed]
- Soteriades, E.S.; Hauser, R.; Kawachi, I.; Christiani, D.C.; Kales, S.N. Obesity and Risk of Job Disability in Male Firefighters. Occup. Med. (Chic Ill) 2008, 58, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Nor, N.; Lee, C.J.; Park, K.S.; Chang, S.-J.; Kim, C.; Park, S. The Risk of Mortality and Cardiovascular Disease is Increased in Firefighters with Elevated Blood Pressure Compared to the General Population. J. Hypertens 2019, 37, e11. [Google Scholar] [CrossRef]
- Jitnarin, N.; Haddock, C.K.; Poston, W.S.C.; Jahnke, S. Smokeless Tobacco and Dual Use among Firefighters in the Central United States. J. Environ. Public Health 2013, 2013, 675426. [Google Scholar] [CrossRef]
- Haddock, C.K.; Jitnarin, N.; Poston, W.S.C.; Tuley, B.; Jahnke, S.A. Tobacco Use among Firefighters in the Central United States. Am. J. Ind. Med. 2011, 54, 697–706. [Google Scholar] [CrossRef] [PubMed]
- Planinc, N.; Kokalj-Kokot, M.; Pajk, A.; Zupet, P. P-100 Analysis of Voluntary Firefighters’ Health Status in Slovenia. Br. J. Sports Med. 2016, 50, A88–A89. [Google Scholar] [CrossRef]
- Martin, Z.T.; Schlaff, R.A.; Hemenway, J.K.; Coulter, J.R.; Knous, J.L.; Lowry, J.E.; Ode, J.J. Cardiovascular Disease Risk Factors and Physical Fitness in Volunteer Firefighters. Int. J. Exerc. Sci. 2019, 12, 764–776. [Google Scholar]
- Noh, J.; Lee, C.J.; Hyun, D.S.; Kim, W.; Kim, M.J.; Park, K.S.; Koh, S.; Chang, S.J.; Kim, C.; Park, S. Blood Pressure and the Risk of Major Adverse Cardiovascular Events among Firefighters. J. Hypertens 2020, 38, 850–857. [Google Scholar] [CrossRef]
- Leary, D.B.; Takazawa, M.; Kannan, K.; Khalil, N. Perfluoroalkyl Substances and Metabolic Syndrome in Firefighters: A Pilot Study. J. Occup. Environ. Med. 2020, 62, 52–57. [Google Scholar] [CrossRef]
- Seyedmehdi, S.M.; Attarchi, M.; Cherati, A.S.; Hajsadeghi, S.; Tofighi, R.; Jamaati, H. Relationship of Aerobic Fitness with Cardiovascular Risk Factors in Firefighters. Work 2016, 55, 155–161. [Google Scholar] [CrossRef]
- Byczek, L.; Walton, S.M.; Conrad, K.M.; Reichelt, P.A.; Samo, D.G. Implications for Occupational Health Nurse Practice. Aaohn 2004, 52, 66–77. [Google Scholar] [CrossRef]
- Cohen, H.W.; Zeig-Owens, R.; Joe, C.; Hall, C.B.; Webber, M.P.; Weiden, M.D.; Cleven, K.L.; Jaber, N.; Skerker, M.; Yip, J.; et al. Long-Term Cardiovascular Disease Risk Among Firefighters After the World Trade Center Disaster. JAMA Netw. Open 2019, 2, e199775. [Google Scholar] [CrossRef]
- Smith, D.L.; Fehling, P.C.; Frisch, A.; Haller, J.M.; Winke, M.; Dailey, M.W. The Prevalence of Cardiovascular Disease Risk Factors and Obesity in Firefighters. J. Obes. 2012, 2012, 908267. [Google Scholar] [CrossRef]
- Mehrdad, R.; Movasatian, F.; Momenzadeh, A.S. Fitness for Work Evaluation of Firefighters in Tehran. Acta Med. Iran. 2013, 51, 265–269. [Google Scholar]
- Durand, G.; Tsismenakis, A.J.; Jahnke, S.A.; Baur, D.M.; Christophi, C.A.; Kales, S.N. Firefighters’ Physical Activity: Relation to Fitness and Cardiovascular Disease Risk. Med. Sci. Sports Exerc. 2011, 43, 1752–1759. [Google Scholar] [CrossRef] [PubMed]
- Cavalcante Neto, J.L.; Calheiros, D.d.S.; Calheiros, D. dos S.; Neto, T. dos S.; Pinto, M.P.; da Rocha, D.F. Levels of Physical Activity and Associated Factors between Military Policemen and Firemen. Work 2019, 62, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Eastlake, A.C.; Knipper, B.S.; He, X.; Alexander, B.M.; Davis, K.G. Lifestyle and Safety Practices of Firefighters and Their Relation to Cardiovascular Risk Factors. Work 2015, 50, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Amodeo, K.L.; Nickelson, J. Predicting Intention to Be Physically Active among Volunteer Firefighters. Am. J. Health Educ. 2020, 51, 1–13. [Google Scholar] [CrossRef]
- Soteriades, E.S.; Psalta, L.; Leka, S.; Spanoudis, G. Occupational Stress and Musculoskeletal Symptoms in Firefighters. Int. J. Occup. Med. Environ Health 2019, 32, 341–352. [Google Scholar] [CrossRef]
- Strauss, M.; Foshag, P.; Jehn, U.; Brzęk, A.; Littwitz, H.; Leischik, R. Higher Cardiorespiratory Fitness Is Strongly Associated with Lower Cardiovascular Risk Factors in Firefighters: A Cross-Sectional Study in a German Fire Brigade. Sci. Rep. 2021, 11, 2445. [Google Scholar] [CrossRef]
- Donovan, R.; Nelson, T.; Peel, J.; Lipsey, T.; Voyles, W.; Israel, R.G. Cardiorespiratory Fitness and the Metabolic Syndrome in Firefighters. Occup. Med. (Chic Ill) 2009, 59, 487–492. [Google Scholar] [CrossRef] [PubMed]
- Perroni, F.; Cignitti, L.; Cortis, C.; Capranica, L. Physical Fitness Profile of Professional Italian Firefighters: Differences among Age Groups. Appl. Ergon. 2014, 45, 456–461. [Google Scholar] [CrossRef] [PubMed]
- McArdle, W.D.; Katch, F.I.; Katch, V.L. Exercise Physiology: Nutrition, Energy, and Human Performance; Lippincott Williams & Wilkins: Phillidelphia, PH, USA, 2010; ISBN 0781797810. [Google Scholar]
- Carbone, S.; del Buono, M.G.; Ozemek, C.; Lavie, C.J. Obesity, Risk of Diabetes and Role of Physical Activity, Exercise Training and Cardiorespiratory Fitness. Prog. Cardiovasc. Dis. 2019, 62, 327–333. [Google Scholar] [CrossRef]
- Karelis, A.D.; Pasternyk, S.M.; Messier, L.; St-Pierre, D.H.; Lavoie, J.-M.; Garrel, D.; Rabasa-Lhoret, R. Relationship between Insulin Sensitivity and the Triglyceride–HDL-C Ratio in Overweight and Obese Postmenopausal Women: A MONET Study. Appl. Physiol. Nutr. Metab. 2007, 32, 1089–1096. [Google Scholar] [CrossRef]
- Kajuluri, L.P.; Singh, K.; Morgan, K.G. Vascular Aging, the Vascular Cytoskeleton and Aortic Stiffness. Explor. Med. 2021, 2, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Alpert, M.A.; Lavie, C.J.; Agrawal, H.; Kumar, A.; Kumar, S.A. Cardiac Effects of Obesity: Cardiac Effects of Obesity: Pathophysiologic, clinical, and prognostic consequences—A review. J. Cardiopulm Rehabil. Prev. 2016, 36, 1–11. [Google Scholar] [CrossRef]
- Yu, C.C.W.; Au, C.T.; Lee, F.Y.F.; So, R.C.H.; Wong, J.P.S.; Mak, G.Y.K.; Chien, E.P.; McManus, A.M. Association between Leisure Time Physical Activity, Cardiopulmonary Fitness, Cardiovascular Risk Factors, and Cardiovascular Workload at Work in Firefighters. Saf. Health Work 2015, 6, 192–199. [Google Scholar] [CrossRef]
- Barry, A.M.; Lyman, K.J.; Dicks, N.D.; Landin, K.D.; McGeorge, C.R.; Hackney, K.J.; Walch, T.J. Firefighters’ Physical Activity and Waist Circumference as Predictors of VO2max. J. Occup. Environ. Med. 2019, 61, 849–853. [Google Scholar] [CrossRef]
- Yang, J.; Farioli, A.; Korre, M.; Kales, S.N. Dietary Preferences and Nutritional Information Needs among Career Firefighters in the United States. Glob. Adv. Health Med. 2015, 4, 16–23. [Google Scholar] [CrossRef]
- Christodoulou, A.; Sotos-Prieto, M.; Kales, S.N.; Christophi, C.A. Dietary Patterns and Their Association with Cardio-Metabolic Outcomes in US Firefighters. Eur. J. Public Health 2020, 30, ckaa165-717. [Google Scholar] [CrossRef]
- Bucala, M.; Sweet, E. Obesity in the Fire Service: An inside Look at the Perceptions of Firefighters towards Obesity and Other Health Issues. Res. Sq. 2019. [Google Scholar] [CrossRef]
- Dobson, M.; Choi, B.; Schnall, P.L.; Wigger, E.; Garcia-Rivas, J.; Israel, L.; Baker, D.B. Exploring Occupational and Health Behavioral Causes of Firefighter Obesity: A Qualitative Study. Am. J. Ind. Med. 2013, 56, 776–790. [Google Scholar] [CrossRef] [PubMed]
- Nazari, G.; Lu, S.; MacDermid, J.C. Quantifying Physiological Responses during Simulated Tasks among Canadian Firefighters: A Systematic Review and Meta-Analysis. J. Mil. Veteran. Fam. Health 2021, 7, 55–75. [Google Scholar] [CrossRef]
- Yang, J.; Teehan, D.; Farioli, A.; Baur, D.M.; Smith, D.; Kales, S.N. Sudden Cardiac Death among Firefighters ≤45 Years of Age in the United States. Am. J. Cardiol. 2013, 112, 1962–1967. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B.; et al. Meta-Analysis of Observational Studies in EpidemiologyA Proposal for Reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Brand, R.A. Editorial: Standards of Reporting: The CONSORT, QUORUM, and STROBE Guidelines. Clin. Orthop Relat. Res. 2009, 467, 1393–1394. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Collaboration, C. Review Manager (RevMan); Version 5.3; The Nordic Cochrane Centre: Copenhagen, Denmark, 2014. [Google Scholar]
- Downes, M.J.; Brennan, M.L.; Williams, H.C.; Dean, R.S. Development of a Critical Appraisal Tool to Assess the Quality of Cross-Sectional Studies (AXIS). BMJ Open 2016, 6, e011458. [Google Scholar] [CrossRef]
- Sanderson, S.; Tatt, I.D.; Higgins, J.P.T. Tools for Assessing Quality and Susceptibility to Bias in Observational Studies in Epidemiology: A Systematic Review and Annotated Bibliography. Int. J. Epidemiol. 2007, 36, 666–676. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, T.P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Haidich, A.B. Meta-Analysis in Medical Research. Hippokratia 2010, 14, 29–37. [Google Scholar]
- Gurevitch, J.; Koricheva, J.; Nakagawa, S.; Stewart, G. Meta-Analysis and the Science of Research Synthesis. Nature 2018, 555, 175–182. [Google Scholar] [CrossRef]
- Lin, L. Comparison of Four Heterogeneity Measures for Meta-Analysis. J. Eval. Clin. Pract. 2020, 26, 376–384. [Google Scholar] [CrossRef]
- Akkaya-Hocagil, T. Meta-Analysis: Methods for Health and Experimental Studies; Springer Nature Pte. Ltd.: Berlin/Heidelberg, Germany, 2020; p. 293. [Google Scholar]
- Atikah, C.W.; Nihayah, M.; Leonard, J.H.; Omar, B.; Noor Ibrahim, M.S.; Zurkarnain, M.K.; Jamri, M.; Wan Mohd Noor, I. A Cross-Sectional Evaluation on Physical Fitness of Malaysian Firefighters. Sains Malays. 2015, 44, 1461–1466. [Google Scholar] [CrossRef]
- Baur, D.M.; Leiba, A.; Christophi, C.A.; Kales, S.N. Low Fitness Is Associated with Exercise Abnormalities among Asymptomatic Firefighters. Occup. Med. 2012, 62, 566–569. [Google Scholar] [CrossRef] [PubMed]
- Baur, D.M.; Christophi, C.A.; Tsismenakis, A.J.; Cook, E.F.; Kales, S.N. Cardiorespiratory Fitness Predicts Cardiovascular Risk Profiles in Career Firefighters. J. Occup. Environ. Med. 2011, 53, 1155–1160. [Google Scholar] [CrossRef] [PubMed]
- Baur, D.M.; Christophi, C.A.; Kales, S.N. Metabolic syndrome is inversely related to cardiorespiratory fitness in male career firefighters. J. Strength Cond. Res. 2012, 26, 2331–2337. [Google Scholar] [CrossRef]
- Cameron, N.A.; Shen, J.; Rusk, K.; Parker, R.; Godino, J.G.; Nichols, J.F. Longitudinal Decline in Cardiorespiratory Fitness with Age among Male Firefighters in San Diego, California, 2005-2015. Am. J. Public Health 2018, 108, 1388–1393. [Google Scholar] [CrossRef]
- Delisle, A.T.; Piazza-Gardner, A.K.; Cowen, T.L.; Sayedul Huq, M.B.; Delisle, A.D.; Stopka, C.B.; Tillman, M.D. Validation of a cardiorespiratory fitness assessment for firefighters. J. Strength Cond. Res. 2014, 28, 2717–2723. [Google Scholar] [CrossRef]
- Espinoza, F.; Delgado-Floody, P.; Martínez-Salazar, C.; Jerez-Mayorga, D.; Guzmán-Guzmán, I.P.; Caamaño-Navarrete, F.; Ramirez-Campillo, R.; Chamorro, C.; Campos-Jara, C. The Influence of Cardiometabolic Risk Factors on Cardiorespiratory Fitness in Volunteer Chilean Firefighters. Am. J. Hum. Biol. 2019, 31, e23280. [Google Scholar] [CrossRef]
- Kirlin, L.K.; Nichols, J.F.; Rusk, K.; Parker, R.A.; Rauh, M.J. The Effect of Age on Fitness among Female Firefighters. Occup. Med. 2017, 67, 528–533. [Google Scholar] [CrossRef]
- Kiss, P.; de Meester, M.; Maes, C.; de Vriese, S.; Kruse, A.; Braeckman, L. Cardiorespiratory Fitness in a Representative Sample of Belgian Firefighters. Occup. Med. 2014, 64, 589–594. [Google Scholar] [CrossRef]
- Houck, J.M.; Mermier, C.M.; Beltz, N.M.; Johnson, K.E.; VanDusseldorp, T.A.; Escobar, K.A.; Gibson, A.L. Physical Fitness Evaluation of Career Urban and Wildland Firefighters. J. Occup. Environ. Med. 2020, 62, e302–e307. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Ochoa, E.; Lipsey, T.; Nelson, T. Correlates of Atherosclerotic Cardiovascular Disease Risk in Older Colorado Firefighters. Occup. Med. 2018, 68, 51–55. [Google Scholar] [CrossRef]
- Li, K.; Lipsey, T.; Leach, H.J.; Nelson, T.L. Cardiac Health and Fitness of Colorado Male/Female Firefighters. Occup. Med. 2017, 67, 268–273. [Google Scholar] [CrossRef]
- McAllister, M.J.; Gonzalez, D.E.; Leonard, M.; Martaindale, M.H.; Bloomer, R.J.; Pence, J.; Martin, S.E. Firefighters with Higher Cardiorespiratory Fitness Demonstrate Lower Markers of Cardiovascular Disease Risk. J. Occup. Environ. Med. 2022, 64, 1036–1040. [Google Scholar] [CrossRef] [PubMed]
- Porto, L.G.G.; Schmidt, A.C.B.; de Souza, J.M.; Nogueira, R.M.; Fontana, K.E.; Molina, G.E.; Korre, M.; Smith, D.L.; Junqueira, L.F.; Kales, S.N. Firefighters’ Basal Cardiac Autonomic Function and Its Associations with Cardiorespiratory Fitness. Work 2019, 62, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Poston, W.S.C.; Haddock, C.K.; Jahnke, S.A.; Jitnarin, N.; Tuley, B.C.; Kales, S.N. The Prevalence of Overweight, Obesity, and Substandard Fitness in a Population-Based Firefighter Cohort. J. Occup. Environ. Med. 2011, 53, 266–273. [Google Scholar] [CrossRef]
- Punakallio, A.; Lindholm, H.; Luukkonen, R.; Lusa, S. Lifestyle Factors Predicting Changes in Aerobic Capacity of Aging Firefighters at 3-and 13-Year Follow-Ups. J. Occup. Environ. Med. 2012, 54, 1133–1141. [Google Scholar] [CrossRef]
- Vandersmissen, G.J.M.; Verhoogen, R.A.J.R.; van Cauwenbergh, A.F.M.; Godderis, L. Determinants of Maximal Oxygen Uptake (VO2max) in Fire Fighter Testing. Appl. Ergon. 2014, 45, 1063–1066. [Google Scholar] [CrossRef]
- Vicente, M.M.; Herrero, D.C.; Prieto, J.P. Cardiorespiratory Fitness in Spanish Firefighters. J. Occup. Environ. Med. 2021, 63, e318–e322. [Google Scholar] [CrossRef] [PubMed]
- Poston, W.S.C.; Jitnarin, N.; Haddock, C.K.; Jahnke, S.A.; Tuley, B.C. Obesity and Injury-Related Absenteeism in a Population-Based Firefighter Cohort. Obesity 2011, 19, 2076–2081. [Google Scholar] [CrossRef] [PubMed]
- Chizewski, A.; Box, A.; Kesler, R.; Petruzzello, S.J. Fitness Fights Fires: Exploring the Relationship between Physical Fitness and Firefighter Ability. Int. J. Environ. Res. Public Health 2021, 18, 11733. [Google Scholar] [CrossRef] [PubMed]
- Rogers, M.A.; Hagberg, J.M.; Martin, W.H.; Ehsani, A.A.; Holloszy, J.O. Decline in VO2max with Aging in Master Athletes and Sedentary Men. J. Appl. Physiol. 1990, 68, 2195–2199. [Google Scholar] [CrossRef]
- Harridge, S.D.R.; Lazarus, N.R. Physical Activity, Aging, and Physiological Function. Physiology 2017, 32, 152–161. [Google Scholar] [CrossRef]
- Craighead, D.H.; Freeberg, K.A.; Seals, D.R. The Protective Role of Regular Aerobic Exercise on Vascular Function with Aging. Curr. Opin. Physiol. 2019, 10, 55–63. [Google Scholar] [CrossRef]
- Suarez-Arrones, L.; Lara-Lopez, P.; Maldonado, R.; Torreno, N.; de Hoyo, M.; Nakamura, F.Y.; di Salvo, V.; Mendez-Villanueva, A. The Effects of Detraining and Retraining Periods on Fat-Mass and Fat-Free Mass in Elite Male Soccer Players. PeerJ 2019, 7, e7466. [Google Scholar] [CrossRef]
- Robertson, N.; Vohora, R. Fitness vs. Fatness: Implicit Bias towards Obesity among Fitness Professionals and Regular Exercisers. Psychol. Sport Exerc. 2008, 9, 547–557. [Google Scholar] [CrossRef]
- Myhre, L.G.; Tucker, D.M.; Bauer, D.H.; Fisher, J.R., Jr.; Grimm, W.H. Relationship Between Selected Measures of Physical Fitness and Performance of a Simulated Fire Fighting Emergency Task. Armstrong Lab Brooks Afb Tx 1997. [Google Scholar]
- Hauschild, V.D.; de Groot, D.W.; Hall, S.M.; Grier, T.L.; Deaver, K.D.; Hauret, K.G.; Jones, B.H. Fitness Tests and Occupational Tasks of Military Interest: A Systematic Review of Correlations. Occup. Environ. Med. 2017, 74, 144–153. [Google Scholar] [CrossRef]
- Khan, A.; van Iterson, E.H.; Laffin, L.J. The Obesity Paradox in Heart Failure: What Is the Role of Cardiorespiratory Fitness? Cleve. Clin. J. Med. 2021, 88, 449–458. [Google Scholar] [CrossRef] [PubMed]
- Arena, R.; Cahalin, L.P. Evaluation of Cardiorespiratory Fitness and Respiratory Muscle Function in the Obese Population. Prog. Cardiovasc. Dis. 2014, 56, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Fyock-Martin, M.B.; Erickson, E.K.; Hautz, A.H.; Sell, K.M.; Turnbaugh, B.L.; Caswell, S.V.; Martin, J.R. What Do Firefighting Ability Tests Tell Us About Firefighter Physical Fitness? A Systematic Review of the Current Evidence. J. Strength Cond. Res. 2020, 34, 2093–2103. [Google Scholar] [CrossRef] [PubMed]
- Mazic, S.; Suzic Lazic, J.; Dekleva, M.; Antic, M.; Soldatovic, I.; Djelic, M.; Nesic, D.; Acimovic, T.; Lazic, M.; Lazovic, B.; et al. The Impact of Elevated Blood Pressure on Exercise Capacity in Elite Athletes. Int. J. Cardiol. 2015, 180, 171–177. [Google Scholar] [CrossRef]
- Parto, P.; Lavie, C.J.; Swift, D.; Sui, X. The Role of Cardiorespiratory Fitness on Plasma Lipid Levels. Expert. Rev. Cardiovasc. Ther. 2015, 13, 1177–1183. [Google Scholar] [CrossRef]
- Vega, G.L.; Grundy, S.M.; Barlow, C.E.; Leonard, D.; Willis, B.L.; DeFina, L.F.; Farrell, S.W. Association of Triglyceride-to-High Density Lipoprotein Cholesterol Ratio to Cardiorespiratory Fitness in Men. J. Clin. Lipidol. 2016, 10, 1414–1422.e1. [Google Scholar] [CrossRef] [PubMed]
- Rumora, A.E.; Lentz, S.I.; Hinder, L.M.; Jackson, S.W.; Valesano, A.; Levinson, G.E.; Feldman, E.L. Dyslipidemia Impairs Mitochondrial Trafficking and Function in Sensory Neurons. FASEB J. 2018, 32, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Tarp, J.; Støle, A.P.; Blond, K.; Grøntved, A. Cardiorespiratory Fitness, Muscular Strength and Risk of Type 2 Diabetes: A Systematic Review and Meta-Analysis. Diabetologia 2019, 62, 1129–1142. [Google Scholar] [CrossRef]
- Savall, A.; Charles, R.; Bertholon, A.; Gramont, B.; Trombert, B.; Barthélémy, J.C.; Roche, F. Volunteer and Career French Firefighters: Cardiovascular Risk Factors and Cardiovascular Risk Assessment. Eur. J. Prev. Cardiol. 2020, 27, 107–109. [Google Scholar] [CrossRef]
- de Borba, A.T.; Jost, R.T.; Gass, R.; Nedel, F.B.; Cardoso, D.M.; Pohl, H.H.; Reckziegel, M.B.; Corbellini, V.A.; Paiva, D.N. The Influence of Active and Passive Smoking on the Cardiorespiratory Fitness of Adults. Multidiscip Respir Med. 2014, 9, 34. [Google Scholar] [CrossRef]
- Baquet, G.; van Praagh, E.; Berthoin, S. Endurance Training and Aerobic Fitness in Young People. Sports Med. 2003, 33, 1127–1143. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Rohatgi, A.; Ayers, C.R.; Willis, B.L.; Haskell, W.L.; Khera, A.; Drazner, M.H.; de Lemos, J.A.; Berry, J.D. Cardiorespiratory Fitness and Classification of Risk of Cardiovascular Disease Mortality. Circulation 2011, 123, 1377–1383. [Google Scholar] [CrossRef] [PubMed]
- Chu, D.J.; al Rifai, M.; Virani, S.S.; Brawner, C.A.; Nasir, K.; Al-Mallah, M.H. The Relationship between Cardiorespiratory Fitness, Cardiovascular Risk Factors and Atherosclerosis. Atherosclerosis 2020, 304, 44–52. [Google Scholar] [CrossRef] [PubMed]


| References | Study Design and Setting | Sample | Cardiovascular Disease Risk Factors | Cardiorespiratory Fitness | Performance Measures | Outcome |
|---|---|---|---|---|---|---|
| Atikah et al. [67] | Cross-sectional study Malaysia, Kebangsaan | 385 Male firefighters | Age: N/A BMI: N/A | VO2max: 26.49 ± 5.14 mL·kg·min | 20 m shuttle run test | The cardiorespiratory fitness of firefighters aged between 20 and 28 years old was significantly higher as compared with firefighters aged between 29 and 37 years old and between 38 and 46 years old. |
| Baur et al. [68] | Cross-sectional study USA, Massachusetts | 957 Male firefighters | Age: 39.6 ± 8.5 years BMI: 29.4 ± 4.3 BF%: 21.6 ± 6.0 | MaxMETs: 12.0 ± 1.9 METs | Maximal treadmill exercise stress test | The number of metabolic syndrome risk factors was significantly different between maximum MET groups (<0.00001). Metabolic syndrome was a significant predictor of cardiorespiratory fitness (CRF). |
| Baur et al. [69] | Cross-sectional study USA, Massachusetts | 968 Male firefighters | Age: 39.5 ± 8.6 years BMI: 29.3 ± 4.3 kg·m−2 BF%: 21.0 ± 5.6% Cigarette smokers: 23.9% SBP: 122.6 ± 12.0 mmHg DBP: 78.6 ± 8.6 mmHg TC: 5.02 ± 0.96 mmol·L LDL-C: 3.22 ± 0.83 mmol·L HDL-C: 1.13 ± 0.30 mmol·L TG: 1.5 ± 1.3 mmol·L | METs: 12.0 ± 1.9 METs | Maximal treadmill exercise stress test | There were significant associations between max METs and age, BMI, systolic blood pressure (SBP), diastolic blood pressure (DBP), triglycerides, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and blood glucose. |
| Baur et al. [70] | Cross-sectional study USA | 804 Male firefighters | Age: 37.4 ± 8.4 years BMI: 29.3 ± 4.4 kg·m−2 | MaxMETs: 10.7 ± 2.0 | Maximal treadmill stress test | Cardiorespiratory was significantly related to age, physical activity, and BMI in firefighters. |
| Barry et al. [49] | Cross-sectional study USA | 30 Male firefighters | Age: 34.45 ± 7.15 years Height: 180.74 ± 6.80 cm Body mass: 94.70 ± 10.65 kgs BMI: 28.97 ± 2.52 kg·m−2 WC: 96.48 ± 7.95 cm | VO2max: 40.82 ± 6.95 mL·kg·min | Treadmill graded exercise stress test | There were significant correlations between sedentary time (r = −0.62, p < 0.001), vigorous physical activity time (r = −0.48, p < 0.001), waist circumference (WC) (r = −0.55, p < 0.01), and BMI (r = −0.53, p < 0.01) and VO2max. |
| Cameron et al. [71] | Cross-sectional study USA, San Diego | 1169 Male firefighters | Age: 38.1 ± 0.3 years Height: 178.79 ± 6.65 cm Weight: 88.42 ± 13.36 kgs BMI: 27.65 ± 3.79 kg·m−2 | METs: 13.96 ± 2.43 METs | Maximal treadmill graded exercise stress test | Cardiorespiratory fitness was significantly different between age groups in firefighters (p < 0.001). |
| Delisle et al. [72] | Cross-sectional study USA, Florida | 30 Male and female firefighters | Age: 31.9 ± 6.4 years BF%: 26.0 ± 6.4% BMI: 27.2 ± 3.8 kg·m−2 | VO2max: 44.6 ± 3.9 mL·kg·min | Bruce treadmill protocol | Cardiorespiratory fitness was significantly and moderately associated with percentage body fat (r = −0.7353, p = 0.0001), DBP (r = −0.541, p = 0.0035), BMI (r = −0.5445, p = 0.003), 1-min recovery HR (r = 0.537, p = 0.0038), and body composition (r = −0.5178; p = 0.008). |
| Donovan et al. [41] | Cross-sectional study USA, Colorado | 214 Male firefighters | Age: 39 ± 9 Height: 179 ± 6 cm Weight: 88 ± 15 kg BMI: 28 ± 4 kg·m−2 BF%: 21 ± 7% WC: 94 ± 11 cm SBP: 129 ± 12 mmHg DBP: 83 ± 8 mmHg TG: 1.4 ± 0.9 mmol·L HDL-C: 1.2 ± 0.3 mmol·L FGL: 4.8 ± 0.5 mmol·L CS: 3.7% | VO2max: 46.3 ± 6.1 mL·kg·min | Bruce treadmill protocol | After controlling for age, cardiorespiratory fitness was inversely associated with increasing metabolic abnormalities (p < 0.001). Estimated VO2max values for firefighters with 0, 1, 2, and 3 metabolic abnormalities were 47.8 mL·kg·min, 47.7 mL·kg·min, 45.2 mL·kg·min, and 43.6 mL·kg·min, respectively. The estimated VO2max for subjects with two, three, or more metabolic abnormalities were found to be significantly lower than that of subjects with zero or one metabolic abnormality. |
| Durand et al. [35] | Cross-sectional cohort study USA, Kansas and Missouri | 527 Full-time male firefighters | Age: 37.2 ± 8.6 years BMI: 29.3 ± 4.5 kg·m−2 | METs: 12.7 ± 1.6 METs | Bruce or modified Bruce protocols | Among the four CRF outcome variables, max-METs was significantly different among the three PA categories after adjusting for age, BMI, and smoking status (p < 0.001). The association with CRF was strong across all three measures of PA dimensions, as well as with total weekly aerobic exercise. |
| Espinoza et al. [73] | Cross-sectional study Chile., South America | 76 Volunteer male firefighters | Age: 27.5 years Height: 172 cm BMI: 27.7 kg·m−2 SBP: 120 mmHg DBP: 73 mmHg FGL: 5.4 mmol·L | VO2max: 44 mL·kg·min | Leger test | CRF was negatively correlated with age, BMI, WC, BF%, SBP, DBP, and blood glucose. CRF was significantly different among normal-weight and obese firefighters. |
| Kirlin et al. [74] | Cross-sectional study USA, San Diego | 96 Full-time female firefighters | Age group: 25–34 vs. 35–44 vs. 45–54 vs. 55+ years Height: 170.7 ± 4.9 vs. 169.4 ± 5.4 168.4 ± 5.7 vs. 167.9 ± 4.3 cm Weight: 72.2 ± 10.2 vs. 74.2 ± 13.4 vs. 73.6 ± 13.4 vs. 68.7 ± 9.3 kgs BMI: 24.7 ± 3.3 vs. 25.8 ± 4.4 vs. 25.9 ± 4.4 vs. 24.4 ± 3.8 kg·m−2 BF%: 22.9 ± 7.0 vs. 25.1 ± 8.2 vs. 26.7 ± 7.7 vs. 24.0 ± 6.4% | VO2max: 50.9 ± 7.4 vs. 45.0 ± 7.1 vs. 42.8 ± 6.4 vs. 45.2 ± 5.1 METs: 14.6 ± 2.1 vs. 12.9 ± 2.0 vs. 12.2 ± 1.8 vs. 12.9 ± 1.5 METs | Graded exercise test | CRF decreased significantly across the age groups. Post hoc analysis showed a significantly lower relative VO2max in the 35–44 age group as compared with the 25–34 age group and in the 45–54 age group as compared with the 25–34 age group. Post hoc analysis of absolute VO2max revealed a significantly higher CRF in the 25–34 age group as compared with the 35–44 group, the 45–54 age group, and the 55+ group. |
| Kiss et al. [75] | Cross-sectional study Belgium, Ghent | 1249 Firefighters | Age: 38 ± 10 years BF%: 24.6 ± 7.0% BMI: 26.0 ± 3.8 kg·m−2 | VO2max: 46.5 ± 8.8 mL·kg·min | Maximal treadmill exercise stress test | Cardiorespiratory fitness was significantly different between age groups, BF% categories, and BMI categories in firefighters. In addition, age, BF%, and BMI were significant predictors of cardiorespiratory fitness. |
| Houck et al. [76] | Cross-sectional study USA, New Mexico | 80 Male and female firefighters | Age: 34.9 ± 7.9 years Height: 178.2 ± 6.2 cm Weight: 85.0 ± 12.0 kgs BMI: 26.7 ± 3.0 kg·m−2 BF%: 18.7 ± 6.3% SBP: 122.0 ± 8.4 mmHg DBP: 78.3 ± 7.2 mmHg | VO2max: 38.4 ± 6.8 mL·kg·min | Graded exercise test Bicycle ergometer test | Cardiorespiratory fitness was significantly and negatively associated with BF% (r = −0.597), BMI (r = −0.497), maximal SBP (r = −0.305), maximal DBP (r = 0.262), and resting HR (r = 0.320). Lean body mass was significantly positively correlated with cardiorespiratory fitness (r = 0.576). |
| Li et al. [77] | Cross-sectional study USA, Colorado | 294 Full-time male and female firefighters | Age: 46.88 ± 5.67 years Height: 1.78 ± 0.10 m Weight: 89.2 ± 17.3 kgs BMI: 28.6 ± 10.1 kg·m−2 BF%: 23.8 ± 7.01% | VO2 max: 44.5 ± 5.94 mL·kg·min | Maximal exercise test | Results of bivariate logistic regression show that %BF (odds ratio [OR] = 1.24, p < 0.01), estimated VO2 max (OR = 0.90, p < 0.05), and metabolic syndrome (OR = 2.66, p < 0.05). The age group (p < 0.001) was significantly related to 10-year ASCVD risk. BMI and sex were not significantly associated with 10-year ASCVD risk. No significant association was found between VO2 max and 10-year ASCVD risk. |
| Li et al. [78] | Cross-sectional study USA, Colorado | 1099 Male and female firefighters | Age: 37.2 ± 9.8 years Male: 37.1 ± 9.8; female 38.0 ± 10.1 BF%: female: 21.1 ± 7.9%; male: 18.4 ± 6.7% | VO2max: 46.9 ± 6.8 mL·kg·min | Bruce protocol | In total, 49% of firefighters did not meet the minimum cardiorespiratory fitness level of 42.0 mL·kg·min. VO2 max, body fat values, and age group were significantly associated with the number of metabolic syndrome components among males and body fat values, but VO2max and age group, were not significantly associated with the number of metabolic syndrome components among females. VO2 max (p < 0.001) was negatively associated with the number of metabolic syndrome components. |
| Seyedmedi et al. [30] | Cross-sectional study Iran, Tehran | 157 Male firefighters | Age: 34.18 years BMI: 25.61 kg·m−2 Aerobic fitness: 33.76 mL·kg−1·min−1 SBP: 116.93 mmHg DBP: 76.03 mmHg TC: 5.22 ± 0.72 mmol·L LDL-C: 3.11 ± 0.63 mmol·L HDL-C: 1.02 ± 0.17 mmol·L TG: 1.6 ± 0.7 mmol·L FGL: 5.0 ± 0.6 mmol·L | METs: 9.64 METs | YMCA bicycle ergometer test | Significant differences between individuals with >11 MET versus individuals with <9 MET for all factors with the exception of total cholesterol, fasting blood sugar, and SBP. The high CRF group was significantly younger with lower BMI, triglycerides, LDL, resting heart rate, DBP, and higher HDL. The frequency of subjects with CVD risk factors in the group with AF < 9 MET was significantly higher than that in the group with AF ≥ 9 MET (p < 0.05) for all factors except triglycerides. Individuals with low AF were more than 5 times as likely to smoke, not participate in physical activity, and have higher LDL-C levels than firefighters with high AF. |
| McAllister et al. [79] | Cross-sectional study USA, Texas | 46 Full-time firefighters | Age: 37.2 ± 8.9 BF%: 24.1 ± 5.4 BMI: 29.5 ± 5.5 FGL: 5.1 ± 0.6 mmol·L TC: 4.79 ± 0.77 mmol·L LDL-C: 2.97 ± 0.87 mmol·L HDL-C: 1.20 ± 0.34 mmol·L TG: 1.5 ± 1.2 mmol·L | VO2max: 35.0 ± 9.6 | Bruce protocol | There were significant differences among BMI (p < 0.01), BF% (p < 0.001), cholesterol (p < 0.05), triglycerides (p < 0.001), HDL-C (p < 0.05), and LDL-C (p < 0.01) between the low fit and high fit groups. |
| Nogueira et al. [19] | Cross-sectional studyBrazil | 4237 Full-time male firefighters | Age: 39 (22–49) years BMI: 26.6 (16.9–43.8) kg·m−2 WC: 90.0 cm (55.0–136.0) BAI = 24.9 (10.5–38.3) BF% = 21.7% (14.0–34.3%) | VO2max: 42.4 mL·kg·min | 12 min Cooper test | VO2max was negatively correlated with age (r = 20.21, p < 0.001), WC (r = 20.50, p < 0.001), BMI (r = −0.45, p < 0.001), and BAI (r = −0.35, p < 0.001). The proportion of obese FF among the less fit firefighters was 5.5-fold higher than among the fittest group. Poor cardiorespiratory fitness (<12 METs) was associated with all indices of obesity, i.e., BMI (p < 0.001), BAI (p < 0.001), BF% (p <0.001), and WC (p < 0.001). |
| Perroni et al. [42] | Cross-sectional study Italy, Rome | 161 Male firefighters | Age: 33 ± 7 years Height: 176 ± 6 cm Weight: 75.8 ± 8.4 kgs BMI: 24.4 ± 2.3 kg·m−2 | VO2max: 51.8 ± 6.8 mL·kg·min | Queensland College step test | Age was significantly related to cardiorespiratory fitness in firefighters. |
| Porto et al. [80] | Cross-sectional study Brazil | 38 Firefighters | Age: 41 years BMI: 26.1 kg·m−2 | VO2max: 42.4 mL·kg·min | SRPA questionnaire estimated VO2max | PNN50, rMSSD, and LHR were significantly different between cardiorespiratory fitness categories. Fitter firefighters had better heart rate variability. |
| Poston et al. [81] | Cross-sectional study USA, Missouri | 478 Full-time and 199 volunteer firefighters | Age: 38.64 ± 10.57 years Height: 178.45 ± 6.45 cm Weight: 92.33 ± 16.47 kgs BMI: 28.86 ± 4.83 kg·m−2 BF%: 25.56 ± 6.95% SBP: 125.9 ± 13.2 mmHg DBP: 79.2 ± 10.6 mmHg TC: 4.06 ± 1.03 mmol·L LDL-C: 2.6 ± 0.9 mmol·L HDL-C: 0.98 ± 0.32 mmol·L TG: 1.4 ± 0.9 mmol·L | METs: 10.9 ± 2.5 VO2max: 37.8 ± 8.1 mL·kg·min | Self-report of physical activity questionnaire | Obese firefighters had significantly lower cardiorespiratory fitness than non-obese firefighters. |
| Punakallio et al. [82] | Longitudinal study Finland, Helsinki | 78 Full-time male firefighters | Age group: 30–34 vs. 40–44 years Age: 32.5 ± 1.5 vs. 41.8 ± 1.4 years Height: 179.8 ± 6.0 vs. 176.6 ± 5.5 cm Weight: 83.6 ± 8.0 vs. 83.6 ± 8.4 kgs BMI: 25.9 ± 2.2 vs. 26.9 ± 2.7 kg·m−2 Experience: 10.4 ± 2.5 vs. 19.3 ± 2.3 years | VO2max: 41.7 ± 6.42 vs. 36.0 ± 5.97 mL·kg·min | Incremental exercise bicycle ergometer test | Age-standardized regular smoking (p = 0.048) and the sum of variables related to lifestyle factors (p = 0.034) significantly predicted absolute VO2max after 13 years. |
| Strauss et al. [40] | Cross-sectional study Germany, Westphalia | 97 Full-time male firefighters | Age: 40.5 ± 9.0 years BMI: 25.9 ± 3.2 kg·m−2 BF%: 17.7 ± 6.2% WC: 89.8 ± 10.0 cm Experience: 16.3 ± 9.1 years SBP: 126.4 ± 9.8 mmHg DBP: 84.1 ± 7.4 mmHg TC: 5.1 ± 0.9 mmol·L LDL-C: 2.9 ± 0.8 mmol·L HDL-C: 1.4 ± 0.3 mmol·L TG: 1.6 ± 0.8 mmol·L | METs: 10.7 ± 1.8 METs | Bicycle spiroergometric exercise stress test | Higher lipid concentrations, DBP, SBP, heart rates, WC, BF%, and years of work experience were inversely related to lower cardiorespiratory fitness levels. Significant associations were present between higher cardiorespiratory fitness and lower BMI (p < 0.0001), WC (p < 0.0001), BF% (p < 0.0001), SBP (p = 0.0061), triglycerides (p = 0.0018), and total cholesterol levels (p = 0.0443). |
| Vandersmissen et al. [83] | Cross-sectional study Belgium | 605 Full-time male firefighters | Age: 40.4 ± 11.5 years BMI: 25.9 ± 3.4 kg·m−2 WC: 92.3 ± 10.3 cm HRmax: 99.7 ± 7.6 bpm | VO2max: 43.3 ± 9.8 mL·kg·min | Maximal treadmill and bicycle ergometer exercise stress test | Cardiorespiratory capacity was significantly related to age (p < 0.001), BMI (p < 0.001), and WC (p < 0.001). Firefighters older than 45 years and those that were obese or had central obesity had a mean VO2max under 42 mL·kg·min. |
| Vicente et al. [84] | Cross-sectional study Italy | 104 Full-time male firefighters | Age: 47.1 ± 6.8 years BMI: 26.6 ± 2.5 kg·m−2 BF%: 22.9 ± 5.0 SBP: 125.4 ± 21 mmHg DBP: 88.9 ± 21.6 mmHg | VO2max: 45.7.3 ± 7.0 mL·kg·min | Shuttle test | CRF was significantly different between the age group categories (p < 0.001). There was a significant negative correlation between CRF and age (r = −0.50, p < 0.01). |
| Outcome | No. of Studies | No. of Participants | R (95% CI) | Z Score | p (Overall Effect) | Heterogeneity I2; Cohen’s Q; p-Value | Egger’s Test Intercept (95%CI); p | Begg’s Test (τ; p) |
|---|---|---|---|---|---|---|---|---|
| Age | 4 | 1434 | −0.471 (−0.562 to −0.369) | −8.073 | <0.001 ** | 47%; 5.66; 0.129 | 1.72 (−0.65 to 4.10); 0.089 | 0.67; 0.174 |
| Treadmill testing | 2 | 105 | −0.334 (−0.497 to −0.150) | −3.460 | 0.001 ** | 0%; 0.24; 0.628 | 1.40 (--); <0.001 | 1.00; 0.317 |
| Gas analysis | 2 | 1254 | −0.451 (−0.654 to −0.188) | −3.215 | 0.001 ** | 63%; 2.67; 0.102 | 1.93 (--); <0.001 | 1.00; 0.317 |
| Obesity | 7 | 1632 | −0.595 (−0.681 to −0.493) | −9.263 | <0.001 ** | 73%; 22.08; <0.001 | −1.28 (−4.12 to 1.57); 0.301 | −0.19; 0.538 |
| Treadmill testing | 3 | 1330 | −0.645 (−0.819 to −0.362) | −3.879 | <0.001 ** | 90%; 20.89; <0.001 | −2.71 (−42.69 to 37.28); 0.548 | −0.33; 0.602 |
| Non-Treadmill testing | 4 | 302 | −0.560 (−0.634 to −0.476) | −10.769 | <0.001 ** | 0%; 1.03; 0.793 | 0.59 (−6.08 to 7.27); 0.739 | 0.33, 0.602 |
| Gas analysis | 3 | 245 | −0.658 (−0.808 to −0.428) | −4.652 | <0.001 ** | 85%; 13.57; 0.001 | −34.02 (−691.86 to 623.82); 0.629 | −0.33; 0.602 |
| Central obesity | 2 | 105 | −0.715 (−0.884 to −0.3810 | −3.543 | <0.001 ** | 80%; 4.96; 0.026 | 6.43 (--); <0.001 | 1.00; 0.317 |
| Body-fat percentage | 4 | 290 | −0.663 (−0.753 to −0.550) | −8.640 | <0.001 ** | 55%; 6.62; 0.085 | −3.26 (−18.49 to 11.98); 0.455 | −0.67; 0.174 |
| Cycle ergometer testing | 2 | 110 | −0.639 (−0.739 to −0.511) | −7.715 | <0.001 ** | 27%; 1.37; 0.241 | −3.34 (--); <0.001 | −1.00; 0.317 |
| Systolic blood pressure | 3 | 209 | −0.190 (−0.319 to −0.053) | −2.716 | 0.007 ** | 0%; 0.37; 0.829 | −0.49 (−17.06 to 16.08); 0.772 | −0.33; 0.602 |
| Treadmill testing | 2 | 105 | −0.230 (−0.406 to −0.0367) | −2.326 | 0.020 * | 0%; 0.03; 0.854 | 0.53 (--); <0.001 | 1.00; 0.317 |
| Diastolic blood pressure | 3 | 209 | −0.267 (−0.475 to −0.030) | −2.202 | 0.028 * | 47; 1.72; 0.129 | 1.72 (−0.65 to 4.10); 0.089 | 0.67; 0.174 |
| Treadmill testing | 2 | 105 | −0.375 (−0.622 to −0.059) | −2.310 | 0.021 * | 57%; 2.33; 0.127 | −4.41 (--); <0.001 | −1.00; 0.317 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ras, J.; Kengne, A.P.; Smith, D.L.; Soteriades, E.S.; Leach, L. Association between Cardiovascular Disease Risk Factors and Cardiorespiratory Fitness in Firefighters: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 2816. https://doi.org/10.3390/ijerph20042816
Ras J, Kengne AP, Smith DL, Soteriades ES, Leach L. Association between Cardiovascular Disease Risk Factors and Cardiorespiratory Fitness in Firefighters: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2023; 20(4):2816. https://doi.org/10.3390/ijerph20042816
Chicago/Turabian StyleRas, Jaron, Andre P. Kengne, Denise L. Smith, Elpidoforos S. Soteriades, and Lloyd Leach. 2023. "Association between Cardiovascular Disease Risk Factors and Cardiorespiratory Fitness in Firefighters: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 20, no. 4: 2816. https://doi.org/10.3390/ijerph20042816
APA StyleRas, J., Kengne, A. P., Smith, D. L., Soteriades, E. S., & Leach, L. (2023). Association between Cardiovascular Disease Risk Factors and Cardiorespiratory Fitness in Firefighters: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 20(4), 2816. https://doi.org/10.3390/ijerph20042816








