Abstract
Background: Research suggests that changes in social support and loneliness have affected mental disorder symptoms during the COVID-19 pandemic. However, there are a lack of studies comparing the robustness of these associations. Aims: The aims were to estimate the strength of the associations of loneliness and social support with symptoms of depression, anxiety, and posttraumatic stress during the COVID-19 pandemic (2020–2022) in the general population. Method: The method entailed a systematic review and random-effects meta-analysis of quantitative studies. Results: Seventy-three studies were included in the meta-analysis. The pooled correlations of the effect size of the association of loneliness with symptoms of depression, anxiety, and posttraumatic stress were 0.49, 0.40, and 0.38, respectively. The corresponding figures for social support were 0.29, 0.19, and 0.18, respectively. Subgroup analyses revealed that the strength of some associations could be influenced by the sociodemographic characteristics of the study samples, such as age, gender, region, and COVID-19 stringency index, and by methodological moderators, such as sample size, collection date, methodological quality, and the measurement scales. Conclusions: Social support had a weak association with mental disorder symptoms during the COVID-19 pandemic while the association with loneliness was moderate. Strategies to address loneliness could be highly effective in reducing the impact of the pandemic on social relationships and mental health.
1. Introduction
Since the appearance of the coronavirus disease (COVID-19) in December 2019, one of the greatest concerns has been its effects on the general population’s mental health in both the short- and long-term. For example, the implementation of public health and social measures during the pandemic could have had a negative impact on social relationships [1,2], which in turn could have resulted in an adverse impact on mental health outcomes [3,4]. Indeed, the current evidence concerning the impact of the pandemic on the prevalence of mental disorders and their symptoms shows a significant increase in the general population [5]. Although the available studies consistently report an increasing trend, the use of different measures to assess mental disorders or their symptoms makes comparison between studies difficult, with a wide variation being reported. Specifically, the reported prevalence of depression ranges from 16% to 34%, anxiety from 15% to 38% [1,6,7,8], and post-traumatic stress disorder (PTSD) from 18% to 33% [9,10].
The effect of social relationships on mental health has been widely documented. Researchers have distinguished between subjective and objective aspects of social relationships, which often interact with each other as moderators [11] or mediators [12] impacting mental health. Objective factors refer to the characteristics of a social network described through quantifiable measures such as the number of close contacts or social interactions, whereas subjective factors refer to how individuals feel regarding that social network [13,14]. Social support and loneliness are, respectively, widely used measures for operationalizing these two types of factors. Social support has been defined as the instrumental, informational, and emotional support provided by a social network that includes family, friends, and neighbours [15] while loneliness has been defined as the unpleasant feeling that occurs because of the difference between the desired and the available social relationships, both quantitatively and qualitatively [16].
According to previous research, loneliness and low social support are among the social determinants most closely related to mental health compared to socioeconomic, material, and behavioural factors [13,17]. These relationships mainly occur with loneliness as the origin [18]. Pre-pandemic and during the pandemic investigations indicate that low social support boosts the development of loneliness [19,20,21,22] and that the effect of social support on mental health is mediated by loneliness [23,24,25]. Both factors increase the odds of having symptoms of depression and anxiety [11,18]. Post-traumatic stress symptoms (PTSS), as already observed during and after the SARS pandemic of 2003, are likely to appear and increase in the long-term following the COVID-19 pandemic, particularly among the most vulnerable groups (e.g., COVID-19 patients and their close contacts, health care workers and other hospital staff, persons with a psychiatric illness history or with underlying health conditions, older people, individuals who reside in high COVID-19 prevalence areas, etc.) [26,27,28]. This increase could also be aggravated by the effects of loneliness and poor social support [4].
The COVID-19 pandemic has generated unprecedented situations and posed unique challenges globally, leading to a fast and constantly growing body of scientific evidence related to the topic. Although there is now an expanding literature about objective and subjective aspects of social relationships, it is still unclear which constructs (i.e., social support or loneliness) have a higher impact on mental health and how this impact differs from the symptoms of one mental disorder to another. Clarifying these aspects would provide relevant information for the design of psychosocial interventions aimed at improving the population’s mental health, which is particularly necessary in the COVID-19 pandemic context.
Thus, the aim of this study was to systematically review quantitative studies published from 2020 to 2022 exploring the associations of loneliness and/or social support with mental disorder symptoms (i.e., depression, anxiety, and post-traumatic stress) during the COVID-19 pandemic. In order to estimate the strength of the associations among these variables, we aimed to perform a statistical meta-analysis, so as to be able to objectively combine and analyse the results of the selected studies.
2. Methods
The review’s protocol was registered in PROSPERO, which is an international prospective register of systematic reviews with protocols related to COVID-19 (registration number: CRD42021260142). The methodology followed the recommendations published in the PRISMA statement [29].
2.1. Eligibility Criteria
Literature included in this review was limited to journal articles using general population-based cohort studies measuring the associations of social support or loneliness (i.e., independent variables [IV]) with symptoms of depression, anxiety, or posttraumatic stress (PTS) (i.e., dependent variables [DV]). All the main variables had to be measured quantitatively using validated scales.
The publication period was restricted to the first three years from the appearance of COVID-19 (i.e., from January 2020 (1 January 2020) to October 2022 (3 October 2022)). Observational studies, both cross-sectional and longitudinal with cross-sectional associations between the variables of interest, were included. Only publications in English and Spanish were included.
Studies on the general adult population were included in this review, excluding cohorts of specific populations that the pandemic may have affected differently (e.g., medical staff, caregivers, patients of specific diseases or those in a hospital setting, pregnant women, etc.). We also excluded studies focused on older adults (>60 years) or on children (<16 years) due to the differences regarding mental health outcomes in these specific age groups [30,31,32]. Moreover, eligibility was restricted to studies with a sample size of 450 participants or more to guarantee that the included articles had enough statistical power to provide substantial estimates of the general population [33,34].
Finally, regarding the measures of interest, studies in which the variables (at least one IV and one DV) were measured quantitatively were included. We ruled out those studies that did not (i) use a valid mode of ascertainment of the measures of interest (e.g., studies that assessed the main variables with a single-item measure or with a non-validated scale, including self-developed scales and adaptations of valid scales), (ii) report disjoint data for each variable (e.g., studies reporting overall mental health as the DV), or (iii) contain relevant and/or complete data for the associations between the variables of interest.
2.2. Article Search, Identification, and Selection
The PubMed, ScienceDirect, and Web of Science databases were searched for relevant studies due to their relevance to the review’s objectives and scope. Separate search strategies were developed for each database (Table S1). Key search terms for mental health outcomes were ‘depression’, ‘anxiety’, ‘post-traumatic stress’, and ‘mental health’. For the social determinants, the terms included were ‘loneliness’, ‘social connectedness’, ‘social isolation’, ‘social network’, ‘social relationships’, and ‘social support’. For the COVID-19 pandemic, we searched for ‘COVID-19’, ‘lockdown’, ‘pandemic’, and ‘quarantine’.
Figure 1 is a flow diagram of the search and inclusion process. The literature search resulted in 6211 publications (Figure 1). For the study selection, Rayyan reference manager app was used. After removing duplicates, 5239 publications were screened based on their titles and abstracts and categorized as ‘include’, ‘maybe’, or ‘exclude’ by two independent reviewers (AG-P & JD-A) based on the eligibility criteria (researchers were blinded to each other’s decisions). Subsequently, decisions of the two reviewers were merged, yielding a percentage of agreement higher than 95%. Discrepancies between the reviewers were resolved by consensus. Finally, the two reviewers independently reviewed the full text articles in the ‘include’ and ‘maybe’ categories (n = 259). The 186 studies excluded at the full-text screening stage were tabulated alongside the reason for exclusion in accordance with best practice guidelines [29,35].
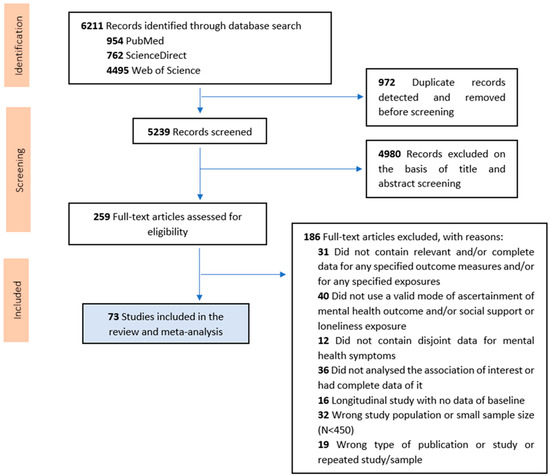
Figure 1.
PRISMA flow diagram outlining results of the study selection process.
2.3. Data Extraction
A total of 73 studies were included in the present review and meta-analysis. One systematic reviewer (AG-P) extracted the data from the selected studies into a structured template and assessed their methodological quality. A second reviewer validated all the extracted data (JD-A). The following data were extracted (where available): study details (first author, publication date, article title, study design, country, collection date, main inclusion/exclusion criteria, sample size (N), type of population, aims of the study, and data collection methods), sample characteristics (age, sex), statistical methods, social relationships and mental health measurements, adjustment for covariates, estimates of associations, and key findings. In the case of longitudinal studies, as just few studies used this design and they used distinct follow-up periods, we just included their cross-sectional baseline data.
2.4. Quality Assessment
To evaluate the methodological quality of the studies, we used an adapted version of the Newcastle Ottawa Scale (NOS) [36] for cross-sectional studies, used in previous systematic reviews [37,38] (Supplementary Material File S2). The NOS checklist has three sections that examine different characteristics of the studies (i.e., selection, comparability, and outcome). Some items are rated with one star and others with two. The total score for each section is what determines the quality of the studies (i.e., 1 = ‘poor’, 2 = ‘fair’, or 3 = ‘good’). Any discrepancies in terms of rating were resolved between the reviewers.
2.5. Meta-Analytical Method
2.5.1. Calculating Effect Sizes
All the analyses were done using the meta package [39] for R software [40].
For the meta-analysis, we required the correlation values of the cross-sectional relationships of interest between continuous variables. When correlations were not available, we converted equivalent statistical measures (e.g, odds ratio (OR)) to correlations. Regarding OR, it was necessary to use a single cut-off point that allowed comparison of people feeling loneliness or having poor social support with the rest of the population. Priority was given to non-adjusted OR and, when not available, to OR adjusted for basic sociodemographic variables (e.g., age and sex), but not for other variables with a potentially mediating role. When the independent variable had more than one category (e.g., low/moderate/high social support), it was dichotomized, and the OR was calculated comparing those with low social support to the remaining sample. Finally, ORs were transformed to Pearson’s r according to the following conversions [41,42,43]:
Odds ratio to Cohen’s d:
Cohen’s d to Pearson’s r:
In cases where the independent variable was divided into different dimensions from the construct ‘loneliness’ or ‘social support’, the average overall correlation between the different dimensions was obtained [44]. If the study met the inclusion criteria and none of the aforementioned options were possible, the corresponding authors of the original articles were contacted to obtain the required unreported data. Correlations were reported as positive when the relationship was what was expected (i.e., lower social support or higher loneliness directly related to greater mental disorder symptoms).
2.5.2. Statistical Analysis
We conducted a series of random-effects meta-analyses, according to the relationships reported for each study [45]. We used the random effects model due to the high heterogeneity across studies. We assessed statistical heterogeneity using restricted maximum likelihood as a heterogeneity variance estimator with the I2 statistic, which describes the percentage of total variation across studies that is due to heterogeneity rather than to chance, and the among-study variance τ2, which is the random effects variance of the true effect sizes [46].
2.5.3. Sources of Heterogeneity
In order to assess the sources of heterogeneity identified in the meta-analysis, we performed subgroup analyses. We evaluated (i) sociodemographic moderator variables and (ii) methodological moderator variables.
Sociodemographic moderator variables were proportion of females in the sample, mean age of the sample, economic region where the study was conducted, and COVID-19 stringency index. The COVID-19 stringency index [47] is a composite score between 0 and 100 designed to compare countries’ policy responses to the pandemic, where higher values represent greater strictness of ‘lockdown policies’ (i.e., closure and containment measures). For each study, the COVID-19 stringency index was determined according to the study setting and the first day of data collection.
Methodological moderator variables were sample size, collection date, study methodological quality, and type of measure to assess the dependent and independent variables. To classify the scales to measure the main variables, we distinguished between the most commonly used measures (i.e., UCLA for loneliness [48], PHQ for depressive symptoms [49], GAD for anxiety symptoms [50], and MSPSS for social support [51]) and “Others”. In the case of the measures used to assess PTSS, due to the concern about flawed published work caused by measuring PTSD related to the pandemic without adequately considering PTSD criteria [52], we performed sub-group analyses distinguishing between those studies that assessed traumatic stress symptoms relative to the COVID-19 pandemic compliant with the DSM-5 criteria [53], using updated measures, and specifying the symptomatic timeframe and those that did not. All the studies that met these criteria also used the PTSD Checklist for DSM-5 (PCL-5) scale [54], so the subgroup was called “PCL5”; while the studies that did not meet any of the criteria were classified in the “Other” group.
The studies that did not have available data regarding a covariate were excluded when carrying out the subgroup analysis for that covariate.
3. Results
3.1. Study Characteristics
The meta-analysis included 73 studies reporting 137 effect sizes from a correlation of either total social support or loneliness with symptoms of depression, anxiety, or PTS (Table 1). The total number of participants involved in the analysis was 1,020,461 (466–746,217 participants), with a mean age of 33.23 (SD = 10.39, not reported in 5 studies), and with around 61.5% (SD = 12.0%, [39.9–87.8%]) of the sample being female (not reported in 2 studies). Most of the study participants were from the general population (62%, N = 45), one third were college students (33%, N = 24), and 4 studies (5%) used samples of the general population with an overrepresentation or inclusion of only young adults (18–35 years). Studies were conducted mainly in China (29%, N = 21), in European countries (29%, N = 21), and in the United States (14%, N = 10). Due to the isolation and social-distancing measures that characterized the initial stages of the COVID-19 pandemic, study data collection was mainly with non-probabilistic sampling techniques via online platforms, social media channels, and email.

Table 1.
Overview of included studies.
3.2. Meta-Analysis
Through random-effects meta-analyses, the six relationships of interest were studied: loneliness-depressive symptoms, loneliness-anxiety symptoms, loneliness-PTSS, social support-depressive symptoms, social support-anxiety symptoms, and social support-PTSS. The effect sizes of the association between loneliness and the mental health outcomes are presented in Figure 2. The pooled effect size for the association of loneliness with symptoms of depression, anxiety, and PTS were r = 0.49, r = 0.40, and r = 0.38, respectively. The three pooled effects represent a medium effect [127] characterised by a large degree of heterogeneity (I2 = 99%, I2 = 99%, and I2 = 98%, respectively). The correlations of the association between social support and mental health outcomes are presented in Figure 3. The pooled effect size for the association between social support and symptoms of depression, anxiety, and PTS were r = 0.29, r = 0.19, and r = 0.18, respectively. The effect of social support on the studied mental health outcomes was smaller when compared to loneliness. The pooled effects were characterised by a large degree of heterogeneity (I2 = 98%, I2 = 99%, and I2 = 97%, respectively).
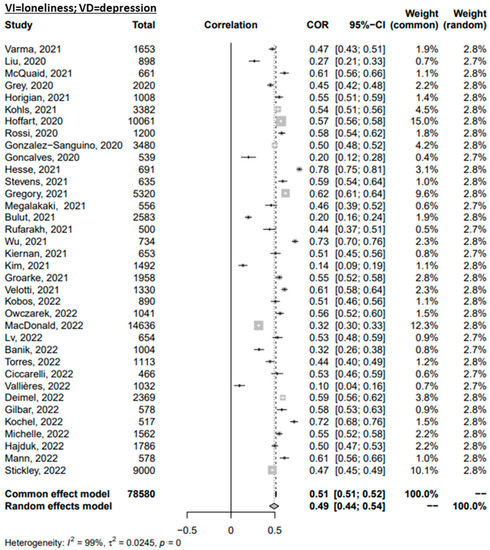
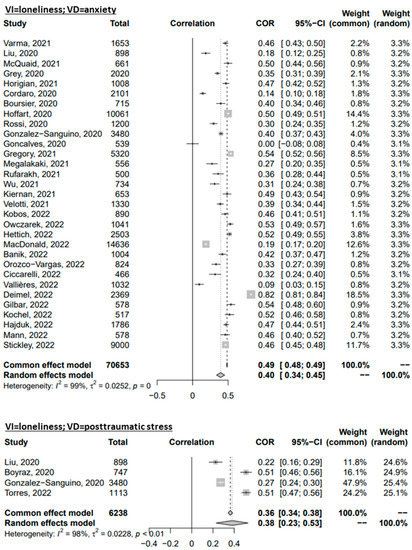
Figure 2.
Forest plot of the Omnibus Test for the correlations of loneliness with mental disorder symptoms. References: Banik, 2022 [56]; Boursier, 2020 [59]; Boyraz, 2020 [60]; Bulut, 2021 [61]; Ciccarelli, 2022 [63]; Cordaro, 2021 [64]; Deimel, 2022 [65]; Gilbar, 2022 [70]; Gonçalves, 2020 [71]; González-Sanguino, 2020 [72]; Gregory, 2021 [73]; Grey, 2020 [74]; Groarke, 2021 [75]; Hajduk, 2022 [77]; Hesse, 2021 [78]; Hettich, 2022 [79]; Hoffart, 2020 [80]; Horigian, 2021 [81]; Kiernan, 2021 [87]; Kim, 2021 [88]; Kobos, 2022 [89]; Kochel, 2022 [90]; Kohls, 2021 [91]; Lim, 2022 [94]; Liu, 2020 [4]; Lv, 2022 [95]; MacDonald, 2022 [98]; Mann, 2022 [99]; McQuaid, 2021 [100]; Megalakaki, 2021 [101]; Orozco-Vargas, 2022 [104]; Owczarek, 2022 [106]; Rossi, 2020 [108]; Rufarakh, 2021 [109]; Stevens, 2021 [115]; Stickley, 2022 [116]; Torres, 2022 [119]; Vallières, 2022 [120]; Varma, 2021 [121]; Velotti, 2021 [122]; Wu, 2022 [84].
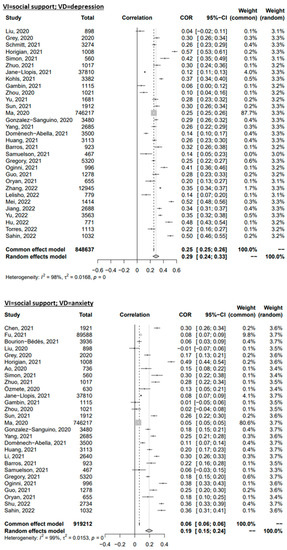
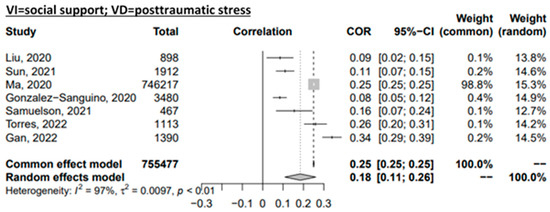
Figure 3.
Forest plot of the Omnibus Test for the correlations of social support with mental disorder symptoms. References: Ao, 2020 [55]; Barros, 2021 [57]; Bourion-Bédès, 2021 [58]; Chen, 2021 [62]; Domènech-Abella, 2021 [66]; Fu, 2021 [67]; Gambin, 2021 [68]; Gan, 2022 [69]; González-Sanguino, 2020 [72]; Gregory, 2021 [73]; Grey, 2020 [74]; Guo, 2021 [76]; Horigian, 2021 [81]; Hu, 2022 [82]; Huang, 2021 [83]; Jané-Llopis, 2021 [85]; Jiang, 2022 [86]; Kohls, 2021 [91]; Lelisho, 2022 [92]; Li, 2021 [93]; Liu, 2020 [4]; Ma, 2020 [97]; Mei, 2022 [102]; Oginni, 2021 [103]; Oryan, 2021 [105]; Özmete, 2020 [107]; Sahin, 2022 [110]; Samuelson, 2021 [111]; Schmitt, 2021 [112]; Shu, 2022 [113]; Simon, 2021 [114]; Sun, 2021 [117]; Yu, 2022 [118]; Torres, 2022 [119]; Yang, 2021 [123]; Yu, 2021 [96]; Zhang, 2022 [124]; Zhou, 2020 [125]; Zhuo, 2021 [126].
3.3. Moderator Analysis
The heterogeneous results were analysed with subgroup analyses. For each of the subgroups, the total effects and associated heterogeneity measures were calculated and the results are reported in Table 2 and Table 3.

Table 2.
Subgroup analysis for the associations between loneliness and mental disorder symptoms.

Table 3.
Subgroup analysis for the associations between social support and mental disorder symptoms.
Although, in many cases, the moderation effects could not be tested in the relationships with PTSS due to a low number of studies, in general we observed that the associations of social support and loneliness with mental disorder symptoms were stronger in samples with a lower proportion of females and COVID-19 stringency index, in those studies adequately using the PCL-5 (Blevins et al., 2015), and conducted in China, whereas those studies using the Patient Health Questionnaire (PHQ) [49] to measure depressive symptoms and the UCLA loneliness scale [48] to measure loneliness showed weaker associations. In the case of the relationship between loneliness and mental disorder symptoms, the associations were stronger when the interviews were carried between July and December 2020 in studies with high methodological quality and in those studies using the Generalized Anxiety Disorder (GAD) scale [50] to measure anxiety symptoms while in developing countries, these associations were weaker. Regarding the relationship between social support and mental disorder symptoms, the correlation values were lower in those studies carried in Europe and with an earlier collection date. In the case of the sample size, the results were discordant between the studied associations.
3.4. Publication Bias
Publication bias was assessed by constructing funnel plots (Figures S1 and S2) followed by Egger tests. The results indicated insignificant levels of publication bias for all relationships, except for the associations of social support and loneliness with anxiety (p < 0.05).
4. Discussion
This meta-analysis sought to explore the correlation of social support and loneliness with symptoms of depression, anxiety, and posttraumatic stress during the COVID-19 pandemic. The results show that social support had a weak association with mental disorder symptoms, whereas loneliness had a moderate association with symptoms of anxiety, posttraumatic stress, and, particularly, depression during the COVID-19 pandemic. If we compare the pooled correlations with guidelines for interpreting the magnitude of correlation coefficients [128], we observe the effect of the association between loneliness and mental health outcomes to be in the upper third distribution of correlation coefficients. In all cases, the results were characterized by a high level of heterogeneity.
In general, our results suggest that the effect sizes of the associations of social support and loneliness with symptoms of mental disorders are similar to pre-pandemic evidence. A previous meta-analysis reported almost the same effect size of loneliness on depression (r = 0.50) [129] as the one obtained in the present study, whereas another meta-analysis showed a weaker association between social support and depression (r = 0.17) [130]. A systematic review defined the association between loneliness and anxiety as moderate (r = 0.42), whereas the association between social support and anxiety was seen to be less clear [17]. Finally, the effect size of the association between social support and PTSS reported in the present meta-analysis was lower than that reported in a previous study with pre-pandemic data (r = 0.26) [131], which may be explained by the diversity of traumatic events considered. No reviews were found about the effect of loneliness on PTSS in the general population.
Therefore, the increase in mental health problems during the COVID-19 pandemic could be partially explained by an increase in the prevalence of loneliness and a decrease in social support [1,2] rather than by more robust associations between social relationships and mental health. The smaller effect size obtained in those associations where social support was the independent variable could be explained by (i) the fact that loneliness might mediate the relationship between social support and mental health [23,24] and (ii) the substantial overlap between these two constructs and the instruments used to measure them. Loneliness and social support are both strictly linked with an individual’s social system and are interconnected concepts that affect one another. They partially share some conceptual aspects but are distinguished by the theoretical interpretation and definition of the concepts, the individual’s experience, perceptions, and social exchanges, and its public connotations [132,133].
Most of the moderation effects detected in our analysis can be explained by previous literature. The stronger association of social support with mental disorder symptoms among younger individuals can be explained by the different relational needs that exist across age groups. Following the socioemotional selectivity theory [134], although social contact declines across adulthood, social goals change and the close and emotionally satisfying relationships prevail, and these may have remained more stable during the pandemic. In contrast, young people rely more on frequent and diverse social interactions, which might have been more greatly affected by social restrictions [134,135]. On the other hand, this pattern is not seen for the impact of loneliness, as subjective aspects of social relationships do not necessarily correspond with objective ones.
Our results are also in line with previous evidence suggesting that the beneficial effects of social support on mental health are stronger in the most deprived regions and neighbourhoods (i.e., with lower socioeconomic conditions and social capital and higher poverty), where inhabitants would be more likely to establish reciprocity networks with neighbours due to the absence of other resources [136,137,138].
In addition, the stronger associations seen in those studies with a higher proportion of males in the sample could be explained by the cultural differences in the socialization process of men and women, as men might be more vulnerable to the negative consequences of loneliness and low social support on mental health since they have fewer relational resources due to different socialization processes between genders. Socialization among men tends to lead to an emotional independence from general social support, with men relying on their partners for social and emotional support, whereas socialization among women tends to lead to a more complex social and emotional life [139].
The differences among variable measurement instruments may be partially explained by the scales having been designed to measure different types of symptoms, the use of different terminology, and variations in recall time frames [140]. In the case of COVID-19 related (post) traumatic stress symptoms, the associations were stronger when the DSM-5 criteria had been strictly followed; nevertheless, we should be cautious when interpreting these results, due to the low number of studies that fit in the “PCL5” category.
Finally, the moderation effect of the collection date and the COVID-19 stringency index, which is based on the public health and social measures imposed by the governments, reflect the changing course of the pandemic and its stages, which have affected social relationships and mental health differently.
Strengths and Limitations
This is the first meta-analysis to focus on synthesizing correlational data of social support and loneliness with symptoms of depression, anxiety, and posttraumatic stress during the COVID-19 pandemic. A strength of the study is the exhaustive search of both published and unpublished data (i.e., multiple attempts to contact authors to obtain missing data) that it involved. However, the cross-sectional nature of the data from the included studies limited the possibility of examining causal relationships. It would have strengthened the meta-analysis to include prospective and longitudinal studies, but few studies used this design, and they used distinct follow-up periods, which impeded their inclusion. Second, the gathered data were based on self-reported questionnaires, which may have resulted in recall or reporting bias. In addition, self-reported measurements are related with the distorted perception of individuals with mental disorder symptoms and their mood state, which could have influenced some of the findings [141]. Third, although 22 out of the 73 included studies had a poor methodological quality, the exclusion of the poor quality studies did not have an impact on our overall results, as it can be seen in the subgroup analyses. Finally, the funnel plots revealed significant publication bias for the relationships with anxiety as the outcome. The asymmetry could be the result of publication and citation bias, as studies giving stronger results are more likely to be published and to be cited and, thus, are more likely to be included in meta-analyses [142,143]. However, no significant publication bias was detected in the remaining associations, although all of them reported a high level of heterogeneity (I2 > 95%). We explored methodological and theoretical factors moderating the correlation of the associations, but it is likely that other factors such as sociodemographic and socioeconomic characteristics of the study samples may have also contributed to the heterogeneity of the results. Therefore, we should cautiously interpret the findings of the present study, and future studies should try to identify further explanatory factors.
5. Conclusions
The current review shows that social support had a weak association, whereas loneliness had a moderate one, with mental disorders symptoms during the COVID-19 pandemic. Therefore, strategies focused on loneliness could be highly effective in reducing the impact of a pandemic on mental health. The synergy between objective aspects of social relationships, such as social support, and subjective aspects, such as loneliness, that configure the population’s mental health suggests that these interventions should be oriented both toward the individual and the community of social networks. These interventions directed towards people feeling loneliness should aim (i) to provide psychological assistance promoting changes in their social behaviour (i.e., targeting their maladaptive social perception and cognitive biases towards loneliness [144,145]) and (ii) to increase their chances of establishing satisfactory social contacts while considering the target population and the effects of moderator variables, such as gender, setting, and age.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20042765/s1. Supplementary Material File S1, Figure S1: Funnel plots representing the standard error by Fisher’s Z for the loneliness’ effect sizes showing the symmetry of the data in relation to publication bias; Figure S2: Funnel plots representing the standard error by Fisher’s Z for the social support effect sizes showing the symmetry of the data in relation to publication bias; Table S1: Overview of the search terms used in each database; Supplementary Material File S2: Adapted version of the Newcastle Ottawa Scale (NOS).
Author Contributions
A.G.-P.: Conceptualization, Methodology, Formal analysis, Investigation, Writing—Original Draft, Writing—Review & Editing. H.G.-M.: Methodology, Writing—Review & Editing. I.G.-V.: Methodology, Writing—Review & Editing. M.V.M.: Methodology, Writing—Review & Editing. A.K.: Conceptualization, Writing—Review & Editing, Supervision. J.M.H.: Conceptualization, Writing—Review & Editing, Supervision. J.D.-A.: Conceptualization, Methodology, Formal analysis, Investigation, Writing—Original Draft, Writing—Review & Editing, Supervision. All authors have read and agreed to the published version of the manuscript.
Funding
Aina Gabarrell-Pascuet’s work is supported by the Secretariat of Universities and Research of the Generalitat de Catalunya and the European Social Fund (2021 FI_B 00839). Joan Domènech-Abella has a “Juan de la Cierva” research contract awarded by the ‘Ministerio de Ciencia, Innovación y Universidades’ (FJC2019-038955-I). Helena García-Mieres has a “Margarita Salas” research contract awarded by the University of Barcelona and financed by the Plan de Recuperación, Transformación y Resiliencia 2021-2023 of the Spanish government (NextGeneration EU funds).
Institutional Review Board Statement
Ethical review and approval was waived for this study as it is based on previously published studies that had already been approved by their respective ethics committees.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data will be made available upon request made to the corresponding author.
Acknowledgments
The authors thank the translator Thomas Yohannan for the spell and grammar check and help in English language editing.
Conflicts of Interest
The authors declare that they have no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
References
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of Stress, Anxiety, Depression among the General Population during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Global. Health 2020, 16, 57. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, R.; Burns, A.; Leavey, G.; Leroi, I.; Burholt, V.; Lubben, J.; Holt-Lunstad, J.; Victor, C.; Lawlor, B.; Vilar-Compte, M.; et al. Impact of the COVID-19 Pandemic on Loneliness and Social Isolation: A Multi-Country Study. Int. J. Environ. Res. Public Health 2021, 18, 9982. [Google Scholar] [CrossRef]
- Palgi, Y.; Shrira, A.; Ring, L.; Bodner, E.; Avidor, S.; Bergman, Y.; Cohen-Fridel, S.; Keisari, S.; Hoffman, Y. The Loneliness Pandemic: Loneliness and Other Concomitants of Depression, Anxiety and Their Comorbidity during the COVID-19 Outbreak. J. Affect. Disord. 2020, 275, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S.; Hahm, H. “Chris” Factors Associated with Depression, Anxiety, and PTSD Symptomatology during the COVID-19 Pandemic: Clinical Implications for U.S. Young Adult Mental Health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.G.; Mukunzi, J.N.; McIntee, S.E.; Dalexis, R.D.; Goulet, M.A.; Labelle, R.P. Prevalence of Symptoms of Depression, Anxiety, Insomnia, Posttraumatic Stress Disorder, and Psychological Distress among Populations Affected by the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Psychiatry Res. 2021, 295, 113599. [Google Scholar] [CrossRef]
- Necho, M.; Tsehay, M.; Birkie, M.; Biset, G.; Tadesse, E. Prevalence of Anxiety, Depression, and Psychological Distress among the General Population during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Int. J. Soc. Psychiatry 2021, 67, 892–906. [Google Scholar] [CrossRef]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of Mental Health Problems during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. J. Affect. Disord. 2021, 281, 91. [Google Scholar] [CrossRef]
- Yunitri, N.; Chu, H.; Kang, X.L.; Jen, H.J.; Pien, L.C.; Tsai, H.T.; Kamil, A.R.; Chou, K.R. Global Prevalence and Associated Risk Factors of Posttraumatic Stress Disorder during COVID-19 Pandemic: A Meta-Analysis. Int. J. Nurs. Stud. 2022, 126, 104136. [Google Scholar] [CrossRef]
- Arora, T.; Grey, I.; Östlundh, L.; Lam, K.B.H.; Omar, O.M.; Arnone, D. The Prevalence of Psychological Consequences of COVID-19: A Systematic Review and Meta-Analysis of Observational Studies. J. Health Psychol. 2022, 27, 805–824. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Lara, E.; Rubio-Valera, M.; Olaya, B.; Moneta, M.V.; Rico-Uribe, L.A.; Ayuso-Mateos, J.L.; Mundó, J.; Haro, J.M. Loneliness and Depression in the Elderly: The Role of Social Network. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 381–390. [Google Scholar] [CrossRef]
- Santini, Z.I.; Fiori, K.L.; Feeney, J.; Tyrovolas, S.; Haro, J.M.; Koyanagi, A. Social Relationships, Loneliness, and Mental Health among Older Men and Women in Ireland: A Prospective Community-Based Study. J. Affect. Disord. 2016, 204, 59–69. [Google Scholar] [CrossRef]
- Santini, Z.I.; Koyanagi, A.; Tyrovolas, S.; Mason, C.; Haro, J.M. The Association between Social Relationships and Depression: A Systematic Review. J. Affect. Disord. 2015, 175, 53–65. [Google Scholar] [CrossRef]
- Cornwell, E.Y.; Waite, L.J. Social Disconnectedness, Perceived Isolation, and Health among Older Adults. J. Health Soc. Behav. 2009, 50, 31–48. [Google Scholar] [CrossRef]
- Cohen, S. Social Relationships and Health. Am. Psychol. 2004, 59, 676–684. [Google Scholar] [CrossRef]
- Perlman, D.; Peplau, L. Toward a Social Psychology of Loneliness. Pers. Relatsh. 1981, 3, 31–55. [Google Scholar] [CrossRef]
- Wang, J.; Mann, F.; Lloyd-Evans, B.; Ma, R.; Johnson, S. Associations between Loneliness and Perceived Social Support and Outcomes of Mental Health Problems: A Systematic Review. BMC Psychiatry 2018, 18, 156. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Mundó, J.; Haro, J.M.; Rubio-Valera, M. Anxiety, Depression, Loneliness and Social Network in the Elderly: Longitudinal Associations from The Irish Longitudinal Study on Ageing (TILDA). J. Affect. Disord. 2019, 246, 82–88. [Google Scholar] [CrossRef]
- Clifton, K.; Gao, F.; Jabbari, J.; van Aman, M.; Dulle, P.; Hanson, J.; Wildes, T.M. Loneliness, Social Isolation, and Social Support in Older Adults with Active Cancer during the COVID-19 Pandemic. J. Geriatr. Oncol. 2022, 13, 1879–4068. [Google Scholar] [CrossRef]
- Kan, Z.; Søegaard, E.G.I.; Siqveland, J.; Hussain, A.; Hanssen-Bauer, K.; Jensen, P.; Heiervang, K.S.; Ringen, P.A.; Ekeberg, Ø.; Hem, E.; et al. Coping, Social Support and Loneliness during the COVID-19 Pandemic and Their Effect on Depression and Anxiety: Patients’ Experiences in Community Mental Health Centers in Norway. Healthcare 2022, 10, 875. [Google Scholar] [CrossRef]
- Perlman, D.; Peplau, L.A. Toward a Social Psychology of Loneliness. In Personal Relationships in Disorder; Duck, S., Gimour, R., Eds.; Academic Press: London, UK, 1981; Volume 3, pp. 31–56. [Google Scholar]
- Labrague, L.J.; de los Santos, J.A.A.; Falguera, C.C. Social and Emotional Loneliness among College Students during the COVID-19 Pandemic: The Predictive Role of Coping Behaviors, Social Support, and Personal Resilience. Perspect. Psychiatr. Care 2021, 57, 1578–1584. [Google Scholar] [CrossRef]
- Gabarrell-Pascuet, A.; Moneta, M.V.; Ayuso-Mateos, J.L.; Miret, M.; Lara, E.; Haro, J.M.; Olaya, B.; Domènech-Abella, J. The Effect of Loneliness and Social Support on the Course of Major Depressive Disorder among Adults Aged 50 Years and Older: A Longitudinal Study. Depress. Anxiety 2022, 39, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Santini, Z.I.; Jose, P.E.; York Cornwell, E.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social Disconnectedness, Perceived Isolation, and Symptoms of Depression and Anxiety among Older Americans (NSHAP): A Longitudinal Mediation Analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef] [PubMed]
- Pineda, C.N.; Naz, M.P.; Ortiz, A.; Ouano, E.L.; Padua, N.P.; Paronable, J.J.; Pelayo, J.M.; Regalado, M.C.; Torres, G.C.S. Resilience, Social Support, Loneliness and Quality of Life during COVID-19 Pandemic: A Structural Equation Model. Nurse Educ. Pract. 2022, 64, 103419. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. The Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 Pandemic and Mental Health Consequences: Systematic Review of the Current Evidence. Brain Behav. Immun. 2020, 89, 531. [Google Scholar] [CrossRef]
- Bryant-Genevier, J.; Rao, C.Y.; Lopes-Cardozo, B.; Kone, A.; Rose, C.; Thomas, I.; Orquiola, D.; Lynfield, R.; Shah, D.; Freeman, L.; et al. Symptoms of Depression, Anxiety, Post-Traumatic Stress Disorder, and Suicidal Ideation among State, Tribal, Local, and Territorial Public Health Workers during the COVID-19 Pandemic—United States, March–April 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 947. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Waraich, P.; Goldner, E.M.; Somers, J.M.; Hsu, L. Prevalence and Incidence Studies of Mood Disorders: A Systematic Review of the Literature. Can. J. Psychiatry 2004, 49, 124–138. [Google Scholar] [CrossRef]
- Kieling, C.; Rohde, L.A. Going Global: Epidemiology of Child and Adolescent Psychopathology. J. Am. Acad. Child. Adolesc. Psychiatry 2012, 51, 1236–1237. [Google Scholar] [CrossRef]
- Luppa, M.; Sikorski, C.; Luck, T.; Ehreke, L.; Konnopka, A.; Wiese, B.; Weyerer, S.; König, H.H.; Riedel-Heller, S.G. Age- and Gender-Specific Prevalence of Depression in Latest-Life—Systematic Review and Meta-Analysis. J. Affect. Disord. 2012, 136, 212–221. [Google Scholar] [CrossRef]
- Steel, Z.; Marnane, C.; Iranpour, C.; Chey, T.; Jackson, J.W.; Patel, V.; Silove, D. The Global Prevalence of Common Mental Disorders: A Systematic Review and Meta-Analysis 1980-2013. Int. J. Epidemiol. 2014, 43, 476–493. [Google Scholar] [CrossRef]
- Somers, J.M.; Goldner, E.M.; Waraich, P.; Hsu, L. Prevalence and Incidence Studies of Anxiety Disorders: A Systematic Review of the Literature. Can. J. Psychiatry 2006, 51, 100–113. [Google Scholar] [CrossRef]
- Dekkers, O.M.; Vandenbroucke, J.P.; Cevallos, M.; Renehan, A.G.; Altman, D.G.; Egger, M. COSMOS-E: Guidance on Conducting Systematic Reviews and Meta-Analyses of Observational Studies of Etiology. PLoS Med. 2019, 16, e1002742. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 25 March 2022).
- Yunus, R.M.; Hairi, N.N.; Choo, W.Y. Consequences of Elder Abuse and Neglect: A Systematic Review of Observational Studies. Trauma Violence Abus. 2017, 20, 197–213. [Google Scholar] [CrossRef]
- Mohd, T.A.M.T.; Yunus, R.M.; Hairi, F.; Hairi, N.N.; Choo, W.Y. Social Support and Depression among Community Dwelling Older Adults in Asia: A Systematic Review. BMJ Open 2019, 9, 26667. [Google Scholar] [CrossRef]
- Schwarzer, G.; Carpenter, J.R.; Rücker, G. Meta-Analysis with R; Use R! Springer International Publishing: Cham, Switzerland, 2015; ISBN 978-3-319-21415-3. [Google Scholar]
- R Core Team. A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. 2022. Available online: https://www.r-project.org/ (accessed on 25 March 2022).
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. Part 2: Effect Size and Precision. In Introduction to Meta-Analysis; Wiley: New York, NY, USA, 2009; pp. 45–49. ISBN 9780470743386. [Google Scholar]
- Ruscio, J. A Probability-Based Measure of Effect Size: Robustness to Base Rates and Other Factors. Psychol. Methods 2008, 13, 19–30. [Google Scholar] [CrossRef]
- Sánchez-Meca, J.; Marín-Martínez, F.; Chacón-Moscoso, S. Effect-Size Indices for Dichotomized Outcomes in Meta-Analysis. Psychol. Methods 2003, 8, 448–467. [Google Scholar] [CrossRef]
- Allen, L.; Jones, C.; Fox, A.; Copello, A.; Jones, N.; Meiser-Stedman, R. The Correlation between Social Support and Post-Traumatic Stress Disorder in Children and Adolescents: A Meta-Analysis. J. Affect. Disord. 2021, 294, 543–557. [Google Scholar] [CrossRef]
- Langan, D.; Higgins, J.P.T.; Simmonds, M. An Empirical Comparison of Heterogeneity Variance Estimators in 12 894 Meta-Analyses. Res. Synth. Methods 2015, 6, 195–205. [Google Scholar] [CrossRef]
- Higgins, J.; Thompson, S.; Deeks, J.; Altman, D. Measuring Inconsistency in Meta-Analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A Global Panel Database of Pandemic Policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Russell, D.W. UCLA Loneliness Scale (Version 3): Reliability, Validity, and Factor Structure. J. Personal. Assess. 2010, 66, 20–40. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Personal. Assess. 2010, 52, 30–41. [Google Scholar] [CrossRef]
- Asmundson, G.J.G.; Taylor, S. Garbage in, Garbage out: The Tenuous State of Research on PTSD in the Context of the COVID-19 Pandemic and Infodemic. J. Anxiety Disord. 2021, 78, 102368. [Google Scholar] [CrossRef]
- American Psychiatric Association APA—Diagnostic and Statistical Manual of Mental Disorders DSM-5 Fifth Edition; American Psychiatric Association: Washington, DC, USA, 2013.
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Ao, Y.; Zhu, H.; Meng, F.; Wang, Y.; Ye, G.; Yang, L.; Dong, N.; Martek, I. The Impact of Social Support on Public Anxiety amidst the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health 2020, 17, 97. [Google Scholar] [CrossRef]
- Banik, R.; Islam, M.S.; Ahmed, M.; Koly, K.N.; Mubarak, M.; Rahman, M.; Zhai, Z.W.; Sikder, M.T.; Potenza, M.N. General Psychiatric Symptoms among Bangladeshi People Approximately One Year after the Onset of the COVID-19 Pandemic. BMC Psychiatry 2022, 22, 615. [Google Scholar] [CrossRef]
- Barros, C.; Sacau-Fontenla, A. New Insights on the Mediating Role of Emotional Intelligence and Social Support on University Students’ Mental Health during COVID-19 Pandemic: Gender Matters. Int. J. Environ. Res. Public Health 2021, 18, 2935. [Google Scholar] [CrossRef]
- Bourion-Bédès, S.; Tarquinio, C.; Batt, M.; Tarquinio, P.; Lebreuilly, R.; Sorsana, C.; Legrand, K.; Rousseau, H.; Baumann, C. Psychological Impact of the COVID-19 Outbreak on Students in a French Region Severely Affected by the Disease: Results of the PIMS-CoV 19 Study. Psychiatry Res. 2021, 295, 113559. [Google Scholar] [CrossRef]
- Boursier, V.; Gioia, F.; Musetti, A.; Schimmenti, A. Facing Loneliness and Anxiety During the COVID-19 Isolation: The Role of Excessive Social Media Use in a Sample of Italian Adults. Front. Psychiatry 2020, 11, 586222. [Google Scholar] [CrossRef]
- Boyraz, G.; Legros, D.N.; Tigershtrom, A. COVID-19 and Traumatic Stress: The Role of Perceived Vulnerability, COVID-19-Related Worries, and Social Isolation. J. Anxiety Disord. 2020, 76, 102307. [Google Scholar] [CrossRef]
- Bulut, N.S.; Yorguner, N.; Akvardar, Y. Impact of COVID-19 on the Life of Higher-Education Students in İstanbul: Relationship between Social Support, Health-Risk Behaviors, and Mental/Academic Well-Being. Alpha Psychiatry 2021, 22, 291–300. [Google Scholar] [CrossRef]
- Chen, H.; Zhao, X.; Zeng, M.; Li, J.; Ren, X.; Zhang, M.; Liu, Y.; Yang, J. Collective Self-Esteem and Perceived Stress among the Non-Infected General Public in China during the 2019 Coronavirus Pandemic: A Multiple Mediation Model. Pers. Individ. Dif. 2021, 168, 110308. [Google Scholar] [CrossRef]
- Ciccarelli, M.; Nigro, G.; D’Olimpio, F.; Griffiths, M.D.; Sacco, M.; Pizzini, B.; Cosenza, M. The Associations between Loneliness, Anxiety, and Problematic Gaming Behavior during the COVID-19 Pandemic: The Mediating Role of Mentalization. Mediterr. J. Clin. Psychol. 2022, 10. [Google Scholar] [CrossRef]
- Cordaro, M.; Grigsby, T.J.; Howard, J.T.; Deason, R.G.; Haskard-Zolnierek, K.; Howard, K. Pandemic-Specific Factors Related to Generalized Anxiety Disorder during the Initial COVID-19 Protocols in the United States. Issues Ment. Health Nurs. 2021, 42, 747–757. [Google Scholar] [CrossRef]
- Deimel, D.; Köhler, T.; Dyba, J.; Graf, N.; Firk, C. Mental Health of COVID-19 Risk Groups during the First COVID-19 Lockdown in Germany: A Cross-Sectional Study. BMC Public Health 2022, 22, 1187. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Gabarrell-Pascuet, A.; Faris, L.H.; Cristóbal-Narváez, P.; Félez-Nobrega, M.; Mortier, P.; Vilagut, G.; Olaya, B.; Alonso, J.; Haro, J.M. The Association of Detachment with Affective Disorder Symptoms during the COVID-19 Lockdown: The Role of Living Situation and Social Support. J. Affect. Disord. 2021, 292, 464–470. [Google Scholar] [CrossRef]
- Fu, W.; Yan, S.; Zong, Q.; Anderson-Luxford, D.; Song, X.; Lv, Z.; Lv, C. Mental Health of College Students during the COVID-19 Epidemic in China. J. Affect. Disord. 2021, 280, 7–10. [Google Scholar] [CrossRef]
- Gambin, M.; Sękowski, M.; Woźniak-Prus, M.; Wnuk, A.; Oleksy, T.; Cudo, A.; Hansen, K.; Huflejt-Łukasik, M.; Kubicka, K.; Łyś, A.E.; et al. Generalized Anxiety and Depressive Symptoms in Various Age Groups during the COVID-19 Lockdown in Poland. Specific Predictors and Differences in Symptoms Severity. Compr. Psychiatry 2021, 105, 152222. [Google Scholar] [CrossRef] [PubMed]
- Gan, Y.; Ma, J.; Wu, J.; Chen, Y.; Zhu, H.; Hall, B.J. Immediate and Delayed Psychological Effects of Province-Wide Lockdown and Personal Quarantine during the COVID-19 Outbreak in China. Psychol. Med. 2022, 52, 1321–1332. [Google Scholar] [CrossRef] [PubMed]
- Gilbar, O.; Gelkopf, M.; Berger, R.; Greene, T. Risk Factors for Depression and Anxiety during COVID-19 in Israel: A Two-Wave Study before and during the Pandemic. Stress Health 2022, 38, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, A.P.; Zuanazzi, A.C.; Salvador, A.P.; Jaloto, A.; Pianowski, G.; de Francisco Carvalho, L. Preliminary Findings on the Associations between Mental Health Indicators and Social Isolation during the COVID-19 Pandemic. Arch. Psychiatry Psychother. 2020, 22, 10–19. [Google Scholar] [CrossRef]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental Health Consequences during the Initial Stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef]
- Gregory, M.A.; Legg, N.K.; Senay, Z.; Barden, J.L.; Phiri, P.; Rathod, S.; Turner, B.J.; Paterson, T.S.E. Mental Health and Social Connectedness across the Adult Lifespan in the Context of the COVID-19 Pandemic. Can. J. Aging 2021, 40, 554–569. [Google Scholar] [CrossRef]
- Grey, I.; Arora, T.; Thomas, J.; Saneh, A.; Tomhe, P.; Abi-Habib, R. The Role of Perceived Social Support on Depression and Sleep during the COVID-19 Pandemic. Psychiatry Res. 2020, 293, 113452. [Google Scholar] [CrossRef]
- Groarke, J.M.; McGlinchey, E.; McKenna-Plumley, P.E.; Berry, E.; Graham-Wisener, L.; Armour, C. Examining Temporal Interactions between Loneliness and Depressive Symptoms and the Mediating Role of Emotion Regulation Difficulties among UK Residents during the COVID-19 Lockdown: Longitudinal Results from the COVID-19 Psychological Wellbeing Study. J. Affect. Disord. 2021, 285, 1–9. [Google Scholar] [CrossRef]
- Guo, K.; Zhang, X.; Bai, S.; Minhat, H.S.; Nazan, A.I.N.M.; Feng, J.; Li, X.; Luo, G.; Zhang, X.; Feng, J.; et al. Assessing Social Support Impact on Depression, Anxiety, and Stress among Undergraduate Students in Shaanxi Province during the COVID-19 Pandemic of China. PLoS ONE 2021, 16, e0253891. [Google Scholar] [CrossRef]
- Hajduk, M.; Dancik, D.; Januska, J.; Strakova, A.; Turcek, M.; Heretik, A.; Pecenak, J. Depression and Anxiety among College Students in Slovakia-Comparison of the Year 2018 and during COVID-19 Pandemic. Bratisl. Med. J. 2022, 123, 44–49. [Google Scholar] [CrossRef]
- Hesse, C.; Mikkelson, A.; Tian, X. Affection Deprivation during the COVID-19 Pandemic: A Panel Study. J. Soc. Pers. Relat. 2021, 38, 2965–2984. [Google Scholar] [CrossRef]
- Hettich, N.; Beutel, M.E.; Ernst, M.; Schliessler, C.; Kampling, H.; Kruse, J.; Braehler, E. Conspiracy Endorsement and Its Associations with Personality Functioning, Anxiety, Loneliness, and Sociodemographic Characteristics during the COVID-19 Pandemic in a Representative Sample of the German Population. PLoS ONE 2022, 17, e0263301. [Google Scholar] [CrossRef]
- Hoffart, A.; Johnson, S.U.; Ebrahimi, O.V. Loneliness and Social Distancing during the COVID-19 Pandemic: Risk Factors and Associations with Psychopathology. Front. Psychiatry 2020, 11, 589127. [Google Scholar] [CrossRef]
- Horigian, V.E.; Schmidt, R.D.; Feaster, D.J. Loneliness, Mental Health, and Substance Use among US Young Adults during COVID-19. J. Psychoactive Drugs 2021, 53, 1–9. [Google Scholar] [CrossRef]
- Hu, J.; Huang, Y.; Liu, J.; Zheng, Z.; Xu, X.; Zhou, Y.; Wang, J. COVID-19 Related Stress and Mental Health Outcomes 1 Year After the Peak of the Pandemic Outbreak in China: The Mediating Effect of Resilience and Social Support. Front. Psychiatry 2022, 13, 828379. [Google Scholar] [CrossRef]
- Huang, Y.; Su, X.; Si, M.; Xiao, W.; Wang, H.; Wang, W.; Gu, X.; Ma, L.; Li, J.; Zhang, S.; et al. The Impacts of Coping Style and Perceived Social Support on the Mental Health of Undergraduate Students during the Early Phases of the COVID-19 Pandemic in China: A Multicenter Survey. BMC Psychiatry 2021, 21, 530. [Google Scholar] [CrossRef]
- Wu, J.; Wu, Y.; Tian, Y. Temporal Associations among Loneliness, Anxiety, and Depression during the COVID-19 Pandemic Period. Stress Health 2022, 38, 90–101. [Google Scholar] [CrossRef]
- Jané-Llopis, E.; Anderson, P.; Segura, L.; Zabaleta, E.; Muñoz, R.; Ruiz, G.; Rehm, J.; Cabezas, C.; Colom, J. Mental Ill-Health during COVID-19 Confinement. BMC Psychiatry 2021, 21, 194. [Google Scholar] [CrossRef]
- Jiang, M.; Zhao, Y.; Wang, J.; Hua, L.; Chen, Y.; Yao, Y.; Jin, Y. Serial Multiple Mediation of the Correlation Between Internet Addiction and Depression by Social Support and Sleep Quality of College Students During the COVID-19 Epidemic. Psychiatry Investig. 2022, 19, 9–15. [Google Scholar] [CrossRef]
- Kiernan, F.; Chmiel, A.; Garrido, S.; Hickey, M.; Davidson, J.W. The Role of Artistic Creative Activities in Navigating the COVID-19 Pandemic in Australia. Front. Psychol 2021, 12, 696202. [Google Scholar] [CrossRef]
- Kim, S.W.; Park, I.H.; Kim, M.; Park, A.-L.; Jhon, M.; Kim, J.W.; Kang, H.J.; Ryu, S.; Lee, J.Y.; Kim, J.M. Risk and Protective Factors of Depression in the General Population during the COVID-19 Epidemic in Korea. BMC Psychiatry 2021, 21, 445. [Google Scholar] [CrossRef] [PubMed]
- Kobos, E.; Knoff, B.; Dziedzic, B.; Maci, R.; Idzik, A. Original Research: Loneliness and Mental Well-Being in the Polish Population during the COVID-19 Pandemic: A Cross-Sectional Study. BMJ Open 2022, 12, 56368. [Google Scholar] [CrossRef] [PubMed]
- Kochel, K.P.; Bagwell, C.L.; Abrash, R.W. Empirically Derived Psychological Profiles of College Students: Differential Associations With COVID-19 Impact and Social Adjustment. Emerg. Adulthood 2022, 10, 1299–1311. [Google Scholar] [CrossRef]
- Kohls, E.; Baldofski, S.; Moeller, R.; Klemm, S.L.; Rummel-Kluge, C. Mental Health, Social and Emotional Well-Being, and Perceived Burdens of University Students during COVID-19 Pandemic Lockdown in Germany. Front. Psychiatry 2021, 12, 643957. [Google Scholar] [CrossRef]
- Lelisho, M.E.; Tareke, S.A. Prevalence and Associated Factors of Depressive Symptoms Among Mizan-Tepi University Students During the COVID-19 Pandemic. J. Racial Ethn. Health Disparities 2022, 1–11. [Google Scholar] [CrossRef]
- Li, Y.; Peng, J. Does Social Support Matter? The Mediating Links with Coping Strategy and Anxiety among Chinese College Students in a Cross-Sectional Study of COVID-19 Pandemic. BMC Public Health 2021, 21, 1298. [Google Scholar] [CrossRef]
- Lim, M.H.; Qualter, P.; Thurston, L.; Eres, R.; Hennessey, A.; Holt-Lunstad, J.; Lambert, G.W. A Global Longitudinal Study Examining Social Restrictions Severity on Loneliness, Social Anxiety, and Depression. Front. Psychiatry 2022, 13, 818030. [Google Scholar] [CrossRef]
- Lv, F.; Yu, M.; Li, J.; Tan, J.; Ye, Z.; Xiao, M.; Zhu, Y.; Guo, S.; Liu, Y.; Gao, D. Young Adults’ Loneliness and Depression During the COVID-19 Pandemic: A Moderated Mediation Model. Front. Psychol. 2022, 13, 3132. [Google Scholar] [CrossRef]
- Yu, M.; Tian, F.; Cui, Q.; Wu, H. Prevalence and Its Associated Factors of Depressive Symptoms among Chinese College Students during the COVID-19 Pandemic. BMC Psychiatry 2021, 21, 66. [Google Scholar] [CrossRef]
- Ma, Z.; Zhao, J.; Li, Y.; Chen, D.; Wang, T.; Zhang, Z.; Chen, Z.; Yu, Q.; Jiang, J.; Fan, F.; et al. Mental Health Problems and Correlates among 746 217 College Students during the Coronavirus Disease 2019 Outbreak in China. Epidemiol. Psychiatr. Sci. 2020, 29, e181. [Google Scholar] [CrossRef]
- MacDonald, J.J.; Baxter-King, R.; Vavreck, L.; Naeim, A.; Wenger, N.; Sepucha, K.; Stanton, A.L. Depressive Symptoms and Anxiety During the COVID-19 Pandemic: Large, Longitudinal, Cross-Sectional Survey. JMIR Ment. Health 2022, 9, e33585. [Google Scholar] [CrossRef]
- Mann, L.M.; Walker, B.R. The Role of Equanimity in Mediating the Relationship between Psychological Distress and Social Isolation during COVID-19. J. Affect. Disord. 2022, 296, 370. [Google Scholar] [CrossRef]
- McQuaid, R.J.; Cox, S.M.L.; Ogunlana, A.; Jaworska, N. The Burden of Loneliness: Implications of the Social Determinants of Health during COVID-19. Psychiatry Res. 2021, 296, 113648. [Google Scholar] [CrossRef]
- Megalakaki, O.; Kokou-Kpolou, C.K. Effects of Biopsychosocial Factors on the Association between Loneliness and Mental Health Risks during the COVID-19 Lockdown. Curr. Psychol. 2021, 41, 8224–8235. [Google Scholar] [CrossRef]
- Mei, S.; Meng, C.; Hu, Y.; Guo, X.; Lv, J.; Qin, Z.; Liang, L.; Li, C.; Fei, J.; Cao, R.; et al. Relationships Between Depressive Symptoms, Interpersonal Sensitivity and Social Support of Employees Before and During the COVID-19 Epidemic: A Cross-Lag Study. Front. Psychol. 2022, 13, 587. [Google Scholar] [CrossRef]
- Oginni, O.A.; Oloniniyi, I.O.; Ibigbami, O.; Ugo, V.; Amiola, A.; Ogunbajo, A.; Esan, O.; Adelola, A.; Daropale, O.; Ebuka, M.; et al. Depressive and Anxiety Symptoms and COVID-19-Related Factors among Men and Women in Nigeria. PLoS ONE 2021, 16, e0256690. [Google Scholar] [CrossRef]
- Orozco-Vargas, A.E. Soledad y Ansiedad Durante El Confinamiento Por COVID-19. El Efecto Mediador de La Regulación Emocional. Interdisciplinaria 2022, 39, 335–354. [Google Scholar] [CrossRef]
- Oryan, Z.; Avinir, A.; Levy, S.; Kodesh, E.; Elkana, O. Risk and Protective Factors for Psychological Distress during COVID-19 in Israel. Curr. Psychol. 2021, 1–12. [Google Scholar] [CrossRef]
- Owczarek, M.; Nolan, E.; Shevlin, M.; Butter, S.; Karatzias, T.; McBride, O.; Murphy, J.; Vallieres, F.; Bentall, R.; Martinez, A.; et al. How Is Loneliness Related to Anxiety and Depression: A Population-Based Network Analysis in the Early Lockdown Period. Int. J. Psychol. 2022, 57, 585–596. [Google Scholar] [CrossRef]
- Özmete, E.; Pak, M. The Relationship between Anxiety Levels and Perceived Social Support during the Pandemic of COVID-19 in Turkey. Soc. Work Public Health 2020, 35, 603–616. [Google Scholar] [CrossRef]
- Rossi, A.; Panzeri, A.; Pietrabissa, G.; Manzoni, G.M.; Castelnuovo, G.; Mannarini, S. The Anxiety-Buffer Hypothesis in the Time of COVID-19: When Self-Esteem Protects from the Impact of Loneliness and Fear on Anxiety and Depression. Front. Psychol. 2020, 11, 2177. [Google Scholar] [CrossRef] [PubMed]
- Rufarakh, A.; Majeed, S.; Jahangir, A.; Jabeen Khan, M.; Farooq, Z.; Mohammad, A. Effect of Loneliness and Sleep Disturbances on Mental Health Problems among Young Adults during COVID-19 Pandemic: Moderating Role of Resilience—BiblioMed.Org—Deposit for Medical Articles. Rawal Med. J. 2021, 46, 776–779. [Google Scholar]
- Sahin, F.; Karadag, F.; Kucukkarapinar, M. A Cross-Sectional Study Investigating Mental Health Among Turkish Citizens During The COVID-19 Pandemic: The Importance of Perceived Social Support. Psychiatry Behav. Sci. 2022, 12, 14. [Google Scholar] [CrossRef]
- Samuelson, K.W.; Dixon, K.; Jordan, J.T.; Powers, T.; Sonderman, S.; Brickman, S. Mental Health and Resilience during the Coronavirus Pandemic: A Machine Learning Approach. J. Clin. Psychol. 2021, 78, 821–846. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, A.A.; Brenner, A.M.; Primo de Carvalho Alves, L.; Claudino, F.C.d.A.; Fleck, M.P.d.A.; Rocha, N.S. Potential Predictors of Depressive Symptoms during the Initial Stage of the COVID-19 Outbreak among Brazilian Adults. J. Affect. Disord. 2021, 282, 1090–1095. [Google Scholar] [CrossRef]
- Shu, Y.; Lin, W.; Yang, J.; Huang, P.; Li, B.; Zhang, X. How Social Support Predicts Anxiety among University Students during COVID-19 Control Phase: Mediating Roles of Self-Esteem and Resilience. Anal. Soc. Issues Public Policy 2022, 22, 490–505. [Google Scholar] [CrossRef]
- Simon, J.; Helter, T.M.; White, R.G.; van der Boor, C.; Łaszewska, A. Impacts of the COVID-19 Lockdown and Relevant Vulnerabilities on Capability Well-Being, Mental Health and Social Support: An Austrian Survey Study. BMC Public Health 2021, 21, 314. [Google Scholar] [CrossRef]
- Stevens, M.; Lieschke, J.; Cruwys, T.; Cárdenas, D.; Platow, M.J.; Reynolds, K.J. Better Together: How Group-Based Physical Activity Protects against Depression. Soc. Sci. Med. 2021, 286, 114337. [Google Scholar] [CrossRef]
- Stickley, A.; Ueda, M. Loneliness in Japan during the COVID-19 Pandemic: Prevalence, Correlates and Association with Mental Health. Psychiatry Res. 2022, 307, 114318. [Google Scholar] [CrossRef]
- Sun, S.; Goldberg, S.B.; Lin, D.; Qiao, S.; Operario, D. Psychiatric Symptoms, Risk, and Protective Factors among University Students in Quarantine during the COVID-19 Pandemic in China. Global. Health 2021, 17, 15. [Google Scholar] [CrossRef]
- Yu, T.; Hu, J. Extraversion and Neuroticism on College Freshmen’s Depressive Symptoms During the COVID-19 Pandemic: The Mediating Role of Social Support. Front. Psychiatry 2022, 13, 822699. [Google Scholar] [CrossRef]
- Torres, A.; Palomin, A.; Morales, F.; Sevilla-Matos, M.; Colunga-Rodríguez, C.; Ángel-González, M.; Sarabia-López, L.E.; Dávalos-Picazo, G.; Delgado-García, D.; Duclos-Bastías, D.; et al. A Cross-Sectional Study of the Mental Health Symptoms of Latin American, US Hispanic, and Spanish College Students Amid the COVID-19 Pandemic. Int. J. Ment. Health Addict. 2022, 1–20. [Google Scholar] [CrossRef]
- Vallières, F.; Murphy, J.; McBride, O.; Shevlin, M.; Gilmore, B.; Travers, Á.; Nolan, A.; Butter, S.; Karatzias, T.; Bentall, R.; et al. The Role of Psychosocial Factors in Explaining Sex Differences in Major Depression and Generalized Anxiety during the COVID-19 Pandemic. BMC Public Health 2022, 22, 1563. [Google Scholar] [CrossRef]
- Varma, P.; Junge, M.; Meaklim, H.; Jackson, M.L. Younger People Are More Vulnerable to Stress, Anxiety and Depression during COVID-19 Pandemic: A Global Cross-Sectional Survey. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 109, 110236. [Google Scholar] [CrossRef]
- Velotti, P.; Rogier, G.; Beomonte Zobel, S.; Castellano, R.; Tambelli, R. Loneliness, Emotion Dysregulation, and Internalizing Symptoms during Coronavirus Disease 2019: A Structural Equation Modeling Approach. Front. Psychiatry 2021, 11, 581494. [Google Scholar] [CrossRef]
- Yang, Q.; Wu, Z.; Xie, Y.; Xiao, X.; Wu, J.; Sang, T.; Zhang, K.; Song, H.; Wu, X.; Xu, X. The Impact of Health Education Videos on General Public’s Mental Health and Behavior during COVID-19. Glob. Health Res. Policy 2021, 6, 37. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, X.; Mi, Y.; Wang, W.; Xu, H. Resilience and Depressive Symptoms Mediated Pathways from Social Support to Suicidal Ideation Among Undergraduates During the COVID-19 Campus Lockdown in China. Psychol. Res. Behav. Manag. 2022, 15, 2291–2301. [Google Scholar] [CrossRef]
- Zhou, Y.; Macgeorge, E.L.; Myrick, J.G. Mental Health and Its Predictors during the Early Months of the COVID-19 Pandemic Experience in the United States. Int. J. Environ. Res. Public Health 2020, 17, 6315. [Google Scholar] [CrossRef]
- Zhuo, L.; Wu, Q.; Le, H.; Li, H.; Zheng, L.; Ma, G.; Tao, H. COVID-19-Related Intolerance of Uncertainty and Mental Health among Back-to-School Students in Wuhan: The Moderation Effect of Social Support. Int. J. Environ. Res. Public Health 2021, 18, 981. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Hillsdale, N.J., Ed.; Lawrence Erlbaum Associates, Publishers: Mahwah, NJ, USA, 1988; pp. 77–81. [Google Scholar] [CrossRef]
- Hemphill, J.F. Interpreting the Magnitudes of Correlation Coefficients. Am. Psychol. 2003, 58, 78–79. [Google Scholar] [CrossRef]
- Erzen, E.; Çikrikci, Ö. The Effect of Loneliness on Depression: A Meta-Analysis. Int. J. Soc. Psychiatry 2018, 64, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Gariépy, G.; Honkaniemi, H.; Quesnel-Vallée, A. Social Support and Protection from Depression: Systematic Review of Current Findings in Western Countries. Br. J. Psychiatry 2016, 209, 284–293. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chung, M.C.; Wang, N.; Yu, X.; Kenardy, J. Social Support and Posttraumatic Stress Disorder: A Meta-Analysis of Longitudinal Studies. Clin. Psychol. Rev. 2021, 85, 101998. [Google Scholar] [CrossRef] [PubMed]
- Rook, K. Loneliness and Lack of Social Support: Same or Different Phenomena? In Proceedings of the 92nd Annual Convention of the American Psychological Association, Toronto, ON, Canada, 24–28 August 1984. [Google Scholar]
- Newcomb, M.D.; Bentler, P.M. Loneliness and Social Support: A confirmatory hierarchical analysis. Personal. Soc. Psychol. Bull. 1986, 12, 520–535. [Google Scholar] [CrossRef]
- Carstensen, L.L. Motivation for Social Contact across the Life Span: A Theory of Socioemotional Selectivity; University of Nebraska Press: Lincoln, Nebraska, 1993. [Google Scholar]
- Nicolaisen, M.; Thorsen, K. What Are Friends for? Friendships and Loneliness over the Lifespan—From 18 to 79 Years. Int. J. Aging Hum. Dev. 2017, 84, 126–158. [Google Scholar] [CrossRef]
- Silva, M.; Loureiro, A.; Cardoso, G. Social Determinants of Mental Health: A Review of the Evidence. Eur. J. Psychiatry 2016, 30, 259–292. [Google Scholar]
- Chang, Q.; Peng, C.; Guo, Y.; Cai, Z.; Yip, P.S.F. Mechanisms Connecting Objective and Subjective Poverty to Mental Health: Serial Mediation Roles of Negative Life Events and Social Support. Soc. Sci. Med. 2020, 265, 113308. [Google Scholar] [CrossRef]
- Singh, A.; Aitken, Z.; Baker, E.; Bentley, R. Do Financial Hardship and Social Support Mediate the Effect of Unaffordable Housing on Mental Health? Soc. Psychiatry Psychiatr. Epidemiol. 2020, 55, 705–713. [Google Scholar] [CrossRef]
- Gierveld, J.d.J.; van Tilburg, T.G.; Dykstra, P.A. New Ways of Theorizing and Conducting Research in the Field of Loneliness and Social Isolation; Cambridge University Press: Cambridge, UK, 2018; pp. 391–404. [Google Scholar]
- Peters, L.; Peters, A.; Andreopoulos, E.; Pollock, N.; Pande, R.L.; Mochari-Greenberger, H. Comparison of DASS-21, PHQ-8, and GAD-7 in a Virtual Behavioral Health Care Setting. Heliyon 2021, 7, e06473. [Google Scholar] [CrossRef]
- Amann, G. Social Network and Social Support Deficits in Depressed Patients: A Result of Distorted Perception? Eur. Arch. Psychiatry Clin. Neurosci. 1991, 241, 49–56. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Harbord, R.M. Funnel Plots in Meta-Analysis. Stata J. 2004, 4, 127–141. [Google Scholar] [CrossRef]
- Hoffman, J. Basic Biostatistics for Medical and Biomedical Practitioners, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2019; ISBN 9780128170847. [Google Scholar]
- Veronese, N.; Galvano, D.; D’Antiga, F.; Vecchiato, C.; Furegon, E.; Allocco, R.; Smith, L.; Gelmini, G.; Gareri, P.; Solmi, M.; et al. Interventions for Reducing Loneliness: An Umbrella Review of Intervention Studies. Health Soc. Care Community 2021, 29, e89–e96. [Google Scholar] [CrossRef]
- Hickin, N.; Käll, A.; Shafran, R.; Sutcliffe, S.; Manzotti, G.; Langan, D. The Effectiveness of Psychological Interventions for Loneliness: A Systematic Review and Meta-Analysis. Clin. Psychol. Rev. 2021, 88, 102066. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).