Relationship between Health Status and Daily Activities Based on Housing Type among Suburban Residents during COVID-19 Self-Isolation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey Area
2.2. Questionnaire Survey
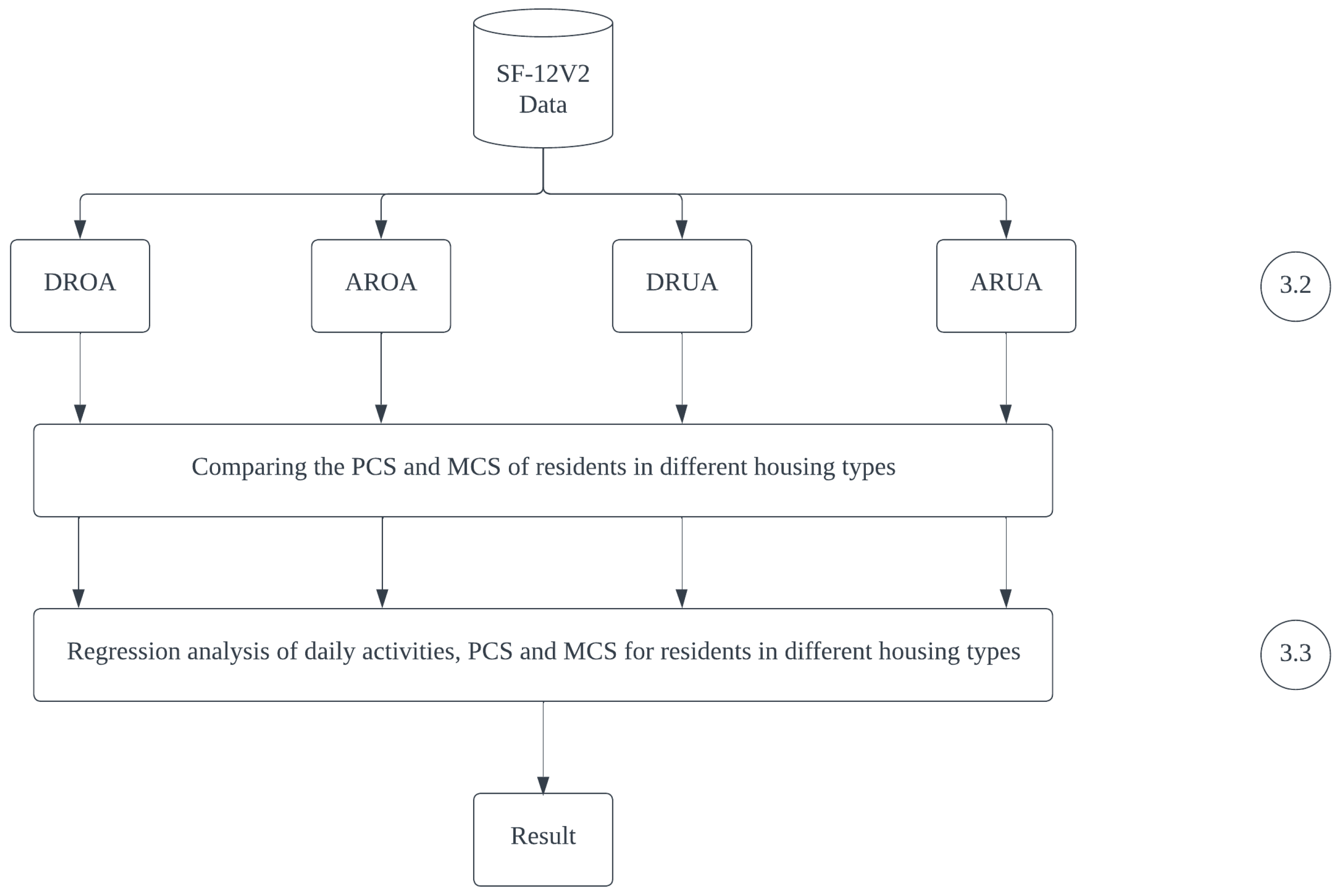
2.3. Sociodemographic Characteristics and Housing Types
2.4. Basic Survey on Social Life
2.5. Health Indicators
2.6. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Health Score
3.3. Relationship between Daily Activities and Health Status
3.3.1. Physical Health Score
3.3.2. Mental Health Scores
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Coronavirus (COVID-19) Dashboard: Situation by Country, Territory and Area. Available online: https://covid19.who.int/table (accessed on 20 August 2022).
- Nussbaumer-Streit, B.; Mayr, V.; Dobrescu, A.I.; Chapman, A.; Persad, E.; Klerings, I.; Wagner, G.; Siebert, U.; Christof, C.; Zachariah, C.; et al. Quarantine Alone or in Combination with Other Public Health Measures to Control COVID-19: A Rapid Review. Cochrane Database Syst. Rev. 2020, 9. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare: Basic Coping Policy for New Coronavirus Infection Control. Available online: https://www.mhlw.go.jp/content/10900000 (accessed on 5 April 2022).
- Kato, H.; Takizawa, A.; Matsushita, D. Impact of COVID-19 Pandemic on Home Range in a Suburban City in the Osaka Metropolitan Area. Sustainability 2021, 13, 8974. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sport Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Tamai, K.; Terai, H.; Takahashi, S.; Katsuda, H.; Shimada, N.; Habibi, H.; Nakamura, H. Decreased Daily Exercise since the COVID-19 pandemic and the Deterioration of Health-Related Quality of Life in the Elderly Population: A Population-Based Cross-Sectional Study. BMC Geriatr. 2022, 22, 678. [Google Scholar] [CrossRef]
- Yang, G.; Lin, X.; Fang, A.; Zhu, H. Eating Habits and Lifestyles during the Initial Stage of the COVID-19 Lockdown in China: A Cross-Sectional Study. Nutrients 2021, 13, 970. [Google Scholar] [CrossRef] [PubMed]
- Cheikh Ismail, L.; Osaili, T.M.; Mohamad, M.N.; al Marzouqi, A.; Jarrar, A.H.; Abu Jamous, D.O.; Magriplis, E.; Ali, H.I.; al Sabbah, H.; Hasan, H.; et al. Eating Habits and Lifestyle during COVID-19 Lockdown in the United Arab Emirates: A Cross-Sectional Study. Nutrients 2020, 12, 3314. [Google Scholar] [CrossRef]
- Barrea, L.; Pugliese, G.; Framondi, L.; di Matteo, R.; Laudisio, D.; Savastano, S.; Colao, A.; Muscogiuri, G. Does Sars-CoV-2 Threaten Our Dreams? Effect of Quarantine on Sleep Quality and Body Mass Index. J. Transl. Med. 2020, 18, 318. [Google Scholar] [CrossRef] [PubMed]
- Kolokotroni, O.; Mosquera, M.C.; Quattrocchi, A.; Heraclides, A.; Demetriou, C.; Philippou, E. Lifestyle Habits of Adults during the COVID-19 Pandemic Lockdown in Cyprus: Evidence from a Cross-Sectional Study. BMC Public Health 2021, 21, 786. [Google Scholar] [CrossRef]
- Wang, X.; Lei, S.M.; Le, S.; Yang, Y.; Zhang, B.; Yao, W.; Gao, Z.; Cheng, S. Bidirectional Influence of the COVID-19 Pandemic Lockdowns on Health Behaviors and Quality of Life among Chinese Adults. Int. J. Environ. Res. Public Health 2020, 17, 5575. [Google Scholar] [CrossRef]
- Casas, R.; Raidó-Quintana, B.; Ruiz-León, A.M.; Castro-Barquero, S.; Bertomeu, I.; Gonzalez-Juste, J.; Campolier, M.; Estruch, R. Changes in Spanish Lifestyle and Dietary Habits during the COVID-19 Lockdown. Eur. J. Nutr. 2022, 61, 2417–2434. [Google Scholar] [CrossRef] [PubMed]
- García, E.L.; Banegas, J.R.; Pérez-Regadera, A.G.; Cabrera, R.H.; Rodríguez-Artalejo, F. Social Network and Health-Related Quality of Life in Older Adults: A Population-Based Study in Spain. Qual. Life Res. 2005, 14, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Brindal, E.; Ryan, J.C.; Kakoschke, N.; Golley, S.; Zajac, I.T.; Wiggins, B. Individual Differences and Changes in Lifestyle Behaviours Predict Decreased Subjective Well-Being during COVID-19 Restrictions in an Australian Sample. J. Public Health 2022, 44, 450–456. [Google Scholar] [CrossRef] [PubMed]
- Drolet, M.; Godbout, A.; Mondor, M.; Béraud, G.; Drolet-Roy, L.; Lemieux-Mellouki, P.; Bureau, A.; Demers, É.; Boily, M.-C.; Sauvageau, C.; et al. Time Trends in Social Contacts before and during the COVID-19 Pandemic: The CONNECT Study. BMC Public Health 2022, 22, 1032. [Google Scholar] [CrossRef] [PubMed]
- Wilkie, S.; Townshend, T.; Thompson, E.; Ling, J. Restructuring the Built Environment to Change Adult Health Behaviors: A Scoping Review Integrated with Behavior Change Frameworks. Cities Health 2018, 2, 198–211. [Google Scholar] [CrossRef]
- Xiao, J.; Zhao, J.; Luo, Z.; Liu, F.; Greenwood, D. The Impact of Built Environment on Mental Health: A COVID-19 Lockdown Perspective. Health Place 2022, 77, 102889. [Google Scholar] [CrossRef]
- Koyama, Y.; Nawa, N.; Yamaoka, Y.; Nishimura, H.; Kuramochi, J.; Fujiwara, T. Association between Social Engagements and Stigmatization of COVID-19 Infection among Community Population in Japan. Int. J. Environ. Res. Public Health 2022, 19, 9050. [Google Scholar] [CrossRef]
- Ministry of Internal Affairs and Communications, Communication Usage Survey. Ministry of Internal Affairs and Communications. 2019. Available online: https://www.soumu.go.jp/johotsusintokei/statistics/data/200529_1.pdf (accessed on 1 August 2022).
- Sato, K.; Sakata, R.; Murayama, C.; Yamaguchi, M.; Matsuoka, Y.; Kondo, N. Changes in Work and Life Patterns Associated with Depressive Symptoms during the COVID-19 Pandemic: An Observational Study of Health App (CALO Mama) Users. Occup. Environ. Med. 2021, 78, 632–637. [Google Scholar] [CrossRef]
- Rubin, G.J.; Wessely, S. The Psychological Effects of Quarantining a City. BMJ 2020, 368, m313. [Google Scholar] [CrossRef]
- Amerio, A.; Brambilla, A.; Morganti, A.; Aguglia, A.; Bianchi, D.; Santi, F.; Costantini, L.; Odone, A.; Costanza, A.; Signorelli, C.; et al. COVID-19 Lockdown: Housing Built Environment’s Effects on Mental Health. Int. J. Environ. Res. Public Health 2020, 17, 5973. [Google Scholar] [CrossRef]
- Guo, Y.; Kato, H.; Matsushita, D. Relationship between living behavior and depressive trend among residents of suburban resi-dential areas during the covid 19 pandemic. J. Archit. Plan. (Trans. AIJ) 2022, 87, 587–595. [Google Scholar] [CrossRef]
- E-Stat. Stat Province City Town Village, Percentage of Owner-Occupied Houses in Each Prefecture. Available online: https://uub.jp/pdr/47/_p_pdr.cgi?D=h&H=home&T=4&P=27 (accessed on 8 August 2022).
- Ministry of Land, Infrastructure, Transport and Tourism, Land, Property and Construction, Nationwide List of New Towns. Available online: https://www.mlit.go.jp/totikensangyo/totikensangyo_tk2_000065.html (accessed on 18 January 2023).
- E-Stat. Japanese Census Data in 2020. Available online: https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00200521&tstat=000001136464&cycle=0&tclass1=000001136472&tclass2=000001159900&stat_infid=000032163495&tclass3val=0 (accessed on 8 August 2022).
- E-Stat. Tondabayasi City Government: Monthly Population Change. Available online: https://www.city.tondabayashi.lg.jp/soshiki/15/2073.html (accessed on 8 August 2022).
- Arghittu, A.; Deiana, G.; Castiglia, E.; Pacifico, A.; Brizzi, P.; Cossu, A.; Castiglia, P.; Dettori, M. Knowledge, Attitudes, and Behaviors towards Proper Nutrition and Lifestyles in Italian Diabetic Patients during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 11212. [Google Scholar] [CrossRef] [PubMed]
- Statistics Bureau, Ministry of Internal Affairs and Communications. Japan, Survey on Time Use and Leisure Activities. Available online: https://www.stat.go.jp/data/shakai/2021/gaiyou.html (accessed on 8 August 2022).
- Maruish, M.E. User’s Manual for the SF-36v2® Health Survey, 3rd ed.; QualityMetric Incorporated: Lincoln, RI, USA, 2011. [Google Scholar]
- Ware, J.; Kosinski, M.; Dewey, J. How to Score Version 2 of the SF-36® Health Survey; Quality Metric Incorporated: Lincoln, RI, USA, 2000. [Google Scholar]
- Ware, J.E.; Ware, J. SF-36 Physical and Mental Health Summary Scales: A User’s Manual Estimation of Medical Care Total Expenditures View Project; Health Assessment Lab.: San Diego, CA, USA, 1993. [Google Scholar]
- Schoofs, M.C.A.; Bakker, E.A.; de Vries, F.; Hartman, Y.A.W.; Spoelder, M.; Thijssen, D.H.J.; Eijsvogels, T.M.H.; Buffart, L.M.; Hopman, M.T.E. Impact of Dutch COVID-19 Restrictive Policy Measures on Physical Activity Behavior and Identification of Correlates of Physical Activity Changes: A Cohort Study. BMC Public Health 2022, 22, 147. [Google Scholar] [CrossRef]
- Browne, R.A.V.; Cabral, L.L.P.; Freire, Y.A.; Macêdo, G.A.D.; Oliveira, G.T.A.; Vivas, A.; Elsangedy, H.M.; Fontes, E.B.; Costa, E.C. Housing Type Is Associated with Objectively Measured Changes in Movement Behavior during the COVID-19 Pandemic in Older Adults with Hypertension: An Exploratory Study. Arch. Gerontol. Geriatr. 2021, 94, 104354. [Google Scholar] [CrossRef] [PubMed]
- McKee, G.; Kearney, P.M.; Kenny, R.A. The Factors Associated with Self-Reported Physical Activity in Older Adults Living in the Community. Age Ageing 2015, 44, 586–592. [Google Scholar] [CrossRef]
- Cerin, E.; van Dyck, D.; Zhang, C.J.P.; van Cauwenberg, J.; Lai, P.; Barnett, A. Urban Environments and Objectively-Assessed Physical Activity and Sedentary Time in Older Belgian and Chinese Community Dwellers: Potential Pathways of Influence and the Moderating Role of Physical Function. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 73. [Google Scholar] [CrossRef]
- Yomoda, K.; Kurita, S. Influence of Social Distancing during the COVID-19 Pandemic on Physical Activity in Children: A Scoping Review of the Literature. J. Exerc. Sci. Fit. 2021, 19, 195–203. [Google Scholar] [CrossRef]
- Nurul Habib, K.; El-Assi, W.; Hasnine, M.S.; Lamers, J. Daily Activity-Travel Scheduling Behaviour of Non-Workers in the National Capital Region (NCR) of Canada. Transp. Res. Part A Policy Pract. 2017, 97, 1–16. [Google Scholar] [CrossRef]
- Dettori, M.; Altea, L.; Fracasso, D.; Trogu, F.; Azara, A.; Piana, A.; Arghittu, A.; Saderi, L.; Sotgiu, G.; Castiglia, P. Housing Demand in Urban Areas and Sanitary Requirements of Dwellings in Italy. J. Environ. Public Health 2020, 2020, 7642658. [Google Scholar] [CrossRef]
- Psomas, T.; Teli, D.; Langer, S.; Wahlgren, P.; Wargocki, P. Indoor Humidity of Dwellings and Association with Building Characteristics, Behaviors and Health in a Northern Climate. Build. Environ. 2021, 198, 107885. [Google Scholar] [CrossRef]
- Newton, D.; Lucock, M.; Armitage, R.; Monchuk, L.; Brown, P. Understanding the Mental Health Impacts of Poor Quality Private-Rented Housing during the UK’s First COVID-19 Lockdown. Health Place 2022, 78, 102898. [Google Scholar] [CrossRef] [PubMed]
- Natomi, K.; Kato, H.; Matsushita, D. Work-Related Stress of Work from Home with Housemates Based on Residential Types. Int. J. Environ. Res. Public Health 2022, 19, 3060. [Google Scholar] [CrossRef] [PubMed]
- Midway, S.R.; Lynch, A.J.; Peoples, B.K.; Dance, M.; Caffey, R. COVID-19 Influences on US Recreational Angler Behavior. PLoS ONE 2021, 16, e0254652. [Google Scholar] [CrossRef] [PubMed]
- Eklund, R.; Bondjers, K.; Hensler, I.; Bragesjö, M.; Johannesson, K.B.; Arnberg, F.K.; Sveen, J. Daily Uplifts during the COVID-19 Pandemic: What Is Considered Helpful in Everyday Life? BMC Public Health 2022, 22, 85. [Google Scholar] [CrossRef] [PubMed]
- Morse, K.F.; Fine, P.A.; Friedlander, K.J. Creativity and Leisure During COVID-19: Examining the Relationship Between Leisure Activities, Motivations, and Psychological Well-Being. Front. Psychol. 2021, 12, 609967. [Google Scholar] [CrossRef] [PubMed]
- Alhofaian, A.; Alharazi, R.; Alaamri, M.; Sofar, S.M.; Tunsi, A.; Elhady, M.M.; Almutary, H.; Sallam, L.; Asiri, S. The Effect of Social Isolation Types on Quality of Life during the Coronavirus Disease 2019 Pandemic in Saudi Arabia: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 6808. [Google Scholar] [CrossRef] [PubMed]
- Hawash, M.M.; Alhazmi, A.H.; Wafik, W.; Muzammil, K.; Mushfiq, S.; Ahmed, H.A. The Association of COVID-19 Pandemic Stress with Health-Related Quality of Life in the Kingdom of Saudi Arabia: A Cross-Sectional Analytical Study. Front. Public Health 2021, 9, 600330. [Google Scholar] [CrossRef]

| Number of questionnaires distributed | 1308 |
| Number of questionnaires collected | 476 |
| Research location | Kongodanchi Teraikeidai, Tondabayashi, Osaka, Japan |
| Method of investigation | Exhaustive questionnaire |
| Research period | 16 March 2022–15 April 2022 |
| Number of valid questionnaires | 427 |
| Valid availability ratio | 32.6% |
| Respondents’ age distribution | Under 65 years: 200 (46.84%) Over 65 years: 227 (53.16%) |
| Respondents’ sex distribution | Male: 153 (35.83%) Female: 246 (57.61%) Non-respondents: 28 (6.56%) |
| DRUA | ARUA | DROA | AROA | |
|---|---|---|---|---|
| Gender | ||||
| Male | 73 (17.10%) | 19 (4.45%) | 42 (9.84%) | 19 (4.45%) |
| Female | 85 (19.91%) | 32 (7.49%) | 96 (22.48%) | 33 (7.73%) |
| Unknown | 12 (2.81%) | 6 (1.26%) | 7 (1.64%) | 3 (0.7%) |
| Family structure | ||||
| Living alone | 29 (6.79%) | 12 (2.81%) | 1 (0.23%) | 2 (0.47%) |
| Couple | 95 (22.25%) | 26 (6.09%) | 28 (6.56%) | 8 (1.87%) |
| Nuclear family generations | 35 (8.2%) | 17 (3.98%) | 100 (23.42%) | 41 (9.6%) |
| Three generations | 4 (0.94%) | 1 (0.23%) | 11 (2.58%) | 1 (0.23%) |
| Other | 7 (1.64%) | 1 (0.23%) | 5 (1.17%) | 3 (0.7%) |
| Occupation | ||||
| Company employees and civil servants | 10 (2.34%) | 2 (0.47%) | 66 (15.46%) | 23 (5.39%) |
| Self-employed profession | 15 (3.51%) | 2 (0.47%) | 13 (3.04%) | 5 (1.17%) |
| Household chores | 67 (15.69%) | 18 (4.22%) | 26 (6.09%) | 9 (2.11%) |
| Student | 0 | 0 | 2 (0.47%) | 0 |
| Part-time job | 9 (2.11%) | 5 (1.17%) | 30 (7.03%) | 9 (2.11%) |
| Fixed year retirees | 55 (12.88%) | 23 (5.39%) | 4 (0.94%) | 1 (0.23%) |
| Other | 14 (3.28%) | 6 (1.41%) | 4 (0.94%) | 8 (1.87%) |
| Unknown | 0 | 1 (0.23%) | 0 | 0 |
| B | Bate | SE | t | p | 95%CI | VIF | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| DROA | (Constant) | 27.17 | 0 | 4.84 | 5.62 | 0.0001 ** | 17.59 | 36.75 | |
| Meals | 1.74 | 0.10 | 1.50 | 1.16 | 0.25 | −1.22 | 4.70 | 1.04 | |
| Work | 1.69 | 0.24 | 0.59 | 2.86 | 0.0049 ** | 0.52 | 2.86 | 1.07 | |
| Recreational hobbies | 3.04 | 0.25 | 1.09 | 2.80 | 0.0059 ** | 0.89 | 5.19 | 1.23 | |
| Sports | 2.48 | 0.21 | 1.02 | 2.43 | 0.0167 * | 0.46 | 4.51 | 1.17 | |
| AROA | (Constant) | 41.26 | 0 | 4.94 | 8.36 | 0.0001 ** | 31.33 | 51.20 | |
| Exchange socializing | 4.50 | 0.37 | 1.58 | 2.85 | 0.0065 ** | 1.32 | 7.68 | 1.00 | |
| Medical treatment | −3.4 | −0.23 | 1.98 | −1.72 | 0.09 | −7.40 | 0.57 | 1.00 | |
| DRUA | (Constant) | 56.91 | 0 | 2.04 | 27.84 | 0.001 ** | 52.86 | 60.95 | |
| Sports | 2.17 | 0.22 | 0.82 | 2.66 | 0.0088 ** | 0.56 | 3.80 | 1.06 | |
| Social participation activities | −2.49 | −0.18 | 1.18 | −2.11 | 0.0369 | −4.82 | −0.15 | 1.09 | |
| Medical treatment | −3.24 | −0.24 | −1.11 | −2.93 | 0.0040 ** | −5.43 | −1.05 | 1.05 | |
| ARUA | (Constant) | 56.27 | 0 | 3.02 | 18.66 | 0.0001 ** | 50.21 | 62.33 | |
| Medical treatment | −5.64 | −0.41 | 1.88 | −3.00 | 0.0043 ** | −9.43 | −1.86 | 1.03 | |
| B | Bate | SE | t | p | 95%CI | VIF | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| AROA | (Constant) | 39.48 | 0 | 2.90 | 13.62 | 0.0001 ** | 33.66 | 45.29 | |
| Exchange socializing | 4.53 | 0.39 | 1.49 | 3.03 | 0.0038 ** | 1.53 | 7.52 | 1.00 | |
| DRUA | (Constant) | 44.43 | 0 | 1.97 | 22.50 | 0.0001 ** | 40.53 | 48.34 | |
| Sports | 2.53 | 0.17 | 1.21 | 2.09 | 0.038 * | 0.14 | 4.90 | 1.00 | |
| ARUA | (Constant) | 40.03 | 0 | 3.98 | 10.06 | 0.0001 ** | 32.04 | 48.02 | |
| Recreational hobbies | 3.42 | 0.34 | 1.46 | 2.34 | 0.0235 * | 0.48 | 6.36 | 1.13 | |
| Exchange socializing | −2.37 | −0.18 | 1.89 | −1.25 | 0.2163 | −6.18 | 1.44 | 1.13 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gu, Y.; Kato, H.; Matsushita, D. Relationship between Health Status and Daily Activities Based on Housing Type among Suburban Residents during COVID-19 Self-Isolation. Int. J. Environ. Res. Public Health 2023, 20, 2639. https://doi.org/10.3390/ijerph20032639
Gu Y, Kato H, Matsushita D. Relationship between Health Status and Daily Activities Based on Housing Type among Suburban Residents during COVID-19 Self-Isolation. International Journal of Environmental Research and Public Health. 2023; 20(3):2639. https://doi.org/10.3390/ijerph20032639
Chicago/Turabian StyleGu, Yangcheng, Haruka Kato, and Daisuke Matsushita. 2023. "Relationship between Health Status and Daily Activities Based on Housing Type among Suburban Residents during COVID-19 Self-Isolation" International Journal of Environmental Research and Public Health 20, no. 3: 2639. https://doi.org/10.3390/ijerph20032639
APA StyleGu, Y., Kato, H., & Matsushita, D. (2023). Relationship between Health Status and Daily Activities Based on Housing Type among Suburban Residents during COVID-19 Self-Isolation. International Journal of Environmental Research and Public Health, 20(3), 2639. https://doi.org/10.3390/ijerph20032639







