Systemic Sclerosis Patients Experiencing Mindfulness-Based Stress Reduction Program: The Beneficial Effect on Their Psychological Status and Quality of Life
Abstract
1. Introduction
2. Materials and Methods
2.1. Universe of Participants
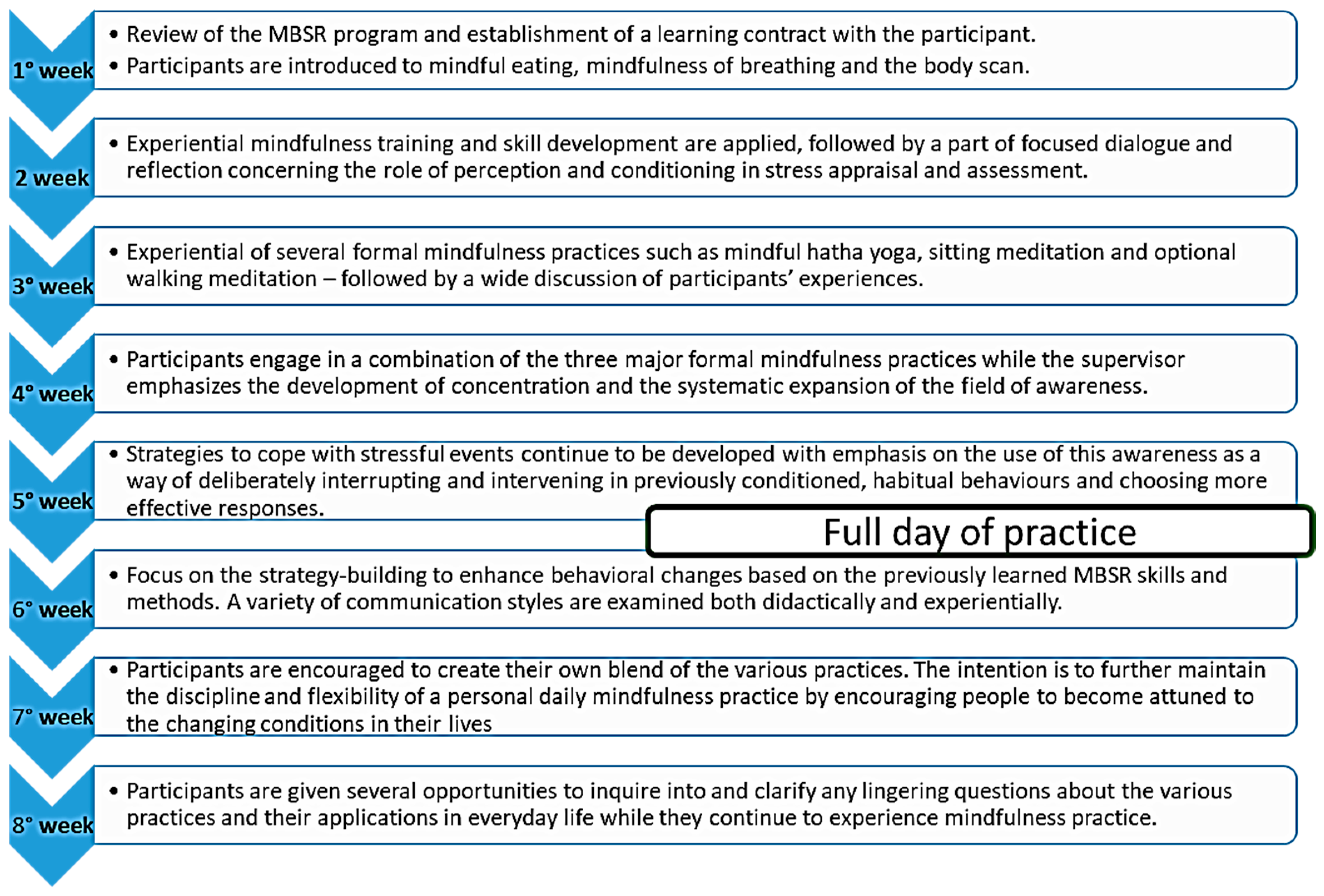
2.2. Mindfulness-Based Stress Reduction Program
2.3. Questionnaires Application and Outcome Measures
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gabrielli, A.; Avvedimento, E.V.; Krieg, T. Scleroderma. N. Engl. J. Med. 2009, 360, 1989–2003. [Google Scholar] [CrossRef] [PubMed]
- Leroy, E.C.; Black, C.; Fleischmajer, R.; Jablonska, S.; Krieg, T.; Medsger, T.A., Jr.; Rowell, N.; Wollheim, F. Scleroderma (systemic sclerosis): Classification, subsets and pathogenesis. J. Rheumatol. 1988, 15, 202–205. [Google Scholar] [PubMed]
- Haustein, U.-F. Systemic Sclerosis—An Update. Lab. Med. 2011, 42, 562–572. [Google Scholar] [CrossRef]
- Murgia, F.; Svegliati, S.; Poddighe, S.; Lussu, M.; Manzin, A.; Spadoni, T.; Fischetti, C.; Gabrielli, A.; Atzori, L. Metabolomic profile of systemic sclerosis patients. Sci. Rep. 2018, 8, 7626. [Google Scholar] [CrossRef] [PubMed]
- Evers, A.W.M.; Zautra, A.; Thieme, K. Stress and resilience in rheumatic diseases: A review and glimpse into the future. Nat. Rev. Rheumatol. 2011, 7, 409–415. [Google Scholar] [CrossRef]
- Wilson, I.B.; Cleary, P.D. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA 1995, 273, 59–65. [Google Scholar] [CrossRef]
- Richards, H.L.; Herrick, A.L.; Griffin, K.; Gwilliam, P.D.H.; Loukes, J.; Fortune, D.G. Systemic sclerosis: Patients’ perceptions of their condition. Arthritis Rheum. 2003, 49, 689–696. [Google Scholar] [CrossRef]
- Bradley, L.A.; Alberts, K.R. Psychological and behavioral approaches to pain management for patients with rheumatic disease. Rheum. Dis. Clin. N. Am. 1999, 25, 215–232. [Google Scholar] [CrossRef]
- Mozzetta, A.; Antinone, V.; Alfani, S.; Neri, P.; Bonda, P.F.; Pasquini, P.; Puddu, P.; Picardi, A. Mental health in patients with systemic sclerosis: A controlled investigation. J. Eur. Acad. Dermatol. Venereol. 2008, 22, 336–340. [Google Scholar] [CrossRef]
- Roca, R.P.; Wigley, F.M.; White, B. Depressive symptoms associated with scleroderma. Arthritis Rheum. 1996, 39, 1035–1040. [Google Scholar] [CrossRef]
- Kwakkenbos, L.; Delisle, V.C.; Fox, R.S.; Gholizadeh, S.; Jewett, L.R.; Levis, B.; Milette, K.; Mills, S.D.; Malcarne, V.L.; Thombs, B.D. Psychosocial Aspects of Scleroderma. Rheum. Dis. Clin. N. Am. 2015, 41, 519–528. [Google Scholar] [CrossRef] [PubMed]
- van Lankveld, W.G.; Vonk, M.C.; Teunissen, H.; van den Hoogen, F.H. Appearance self-esteem in systemic sclerosis–subjective experience of skin deformity and its relationship with physician-assessed skin involvement, disease status and psychological variables. Rheumatology 2007, 46, 872–876. [Google Scholar] [CrossRef] [PubMed]
- Kwakkenbos, L.; van Lankveld, W.G.; Vonk, M.C.; Becker, E.S.; Hoogen, F.H.V.D.; Ende, C.H.V.D. Disease-related and psychosocial factors associated with depressive symptoms in patients with systemic sclerosis, including fear of progression and appearance self-esteem. J. Psychosom. Res. 2012, 72, 199–204. [Google Scholar] [CrossRef]
- Benrud-Larson, L.M.; Heinberg, L.J.; Boling, C.; Reed, J.; White, B.; Wigley, F.M.; Haythornthwaite, J.A. Body image dissatisfaction among women with scleroderma: Extent and relationship to psychosocial function. Health Psychol. 2003, 22, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Amin, K.; Clarke, A.; Sivakumar, B.; Puri, A.; Fox, Z.; Brough, V.; Denton, C.; Peter, E.; Butler, M. The psychological impact of facial changes in scleroderma. Psychol. Health. Med. 2011, 16, 304–312, Erratum in Psychol. Health Med. 2011, 16, 492. [Google Scholar] [CrossRef] [PubMed]
- Hudson, M.; Thombs, B.D.; Steele, R.; Panopalis, P.; Newton, E.; Baron, M. Canadian Scleroderma Research Group Health-related quality of life in systemic sclerosis: A systematic review. Arthritis Rheum. 2009, 61, 1112–1120. [Google Scholar] [CrossRef]
- Del Rosso, A.; Boldrini, M.; D’Agostino, D.; Placidi, G.P.; Scarpato, A.; Pignone, A.; Generini, S.; Konttinen, Y.; Zoppi, M.; Vlak, T.; et al. Health-related quality of life in systemic sclerosis as measured by the Short Form 36, relationship with clinical and biologic markers. Arthritis Rheum. 2004, 51, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Georges, C.; Chassany, O.; Toledano, C.; Mouthon, L.; Tiev, K.; Meyer, O.; Ilie, D.; Rambeloarisoa, J.; Marjanovic, Z.; Cabane, J.; et al. Impact of pain in health related quality of life of patients with systemic sclerosis. Rheumatology 2006, 45, 1298–1302. [Google Scholar] [CrossRef] [PubMed]
- Hudson, M.; Thombs, B.D.; Steele, R.; Panopalis, P.; Newton, E.; Baron, M.; for the Canadian Scleroderma Research Group. Quality of Life in Patients with Systemic Sclerosis Compared to the General Population and Patients with Other Chronic Conditions. J. Rheumatol. 2009, 36, 768–772. [Google Scholar] [CrossRef]
- Hyphantis, T.N.; Tsifetaki, N.; Siafaka, V.; Voulgari, P.V.; Pappa, C.; Bai, M.; Palieraki, K.; Venetsanopoulou, A.; Mavreas, V.; Drosos, A.A. The Impact of Psychological Functioning upon Systemic Sclerosis Patients’ Quality of Life. Semin. Arthritis Rheum. 2007, 37, 81–92. [Google Scholar] [CrossRef]
- Reibel, D.K.; Greeson, J.M.; Brainard, G.C.; Rosenzweig, S. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. Gen. Hosp. Psychiatry 2001, 23, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Grossman, P.; Niemann, L.; Schmidt, S.; Walach, H. Mindfulness-based stress reduction and health benefits: A meta-analysis. J. Psychosom. Res. 2004, 57, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen. Hosp. Psychiatry 1982, 4, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J.; Lipworth, L.; Burney, R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J. Behav. Med. 1985, 8, 163–190. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Bringing mindfulness to medicine. Interview by Karolyn A. Gazella. Altern. Ther. Health. Med. 2005, 11, 56–64. [Google Scholar]
- Slagter, L.; Demyttenaere, K.; Verschueren, P.; De Cock, D. The Effect of Meditation, Mindfulness, and Yoga in Patients with Rheumatoid Arthritis. J. Pers. Med. 2022, 12, 1905. [Google Scholar] [CrossRef]
- Gordon, S.; Brown, R.; Hogan, M.; Menzies, V. Mindfulness as a Symptom Management Strategy for Fibromyalgia: An Integrative Review. J. Holist. Nurs. 2022. [Google Scholar] [CrossRef]
- Leça, S.; Tavares, I. Research in Mindfulness Interventions for Patients with Fibromyalgia: A Critical Review. Front. Integr. Neurosci. 2022, 16, 920271. [Google Scholar] [CrossRef]
- van den Hoogen, F.; Khanna, D.; Fransen, J.; Johnson, S.R.; Baron, M.; Tyndall, A.; Matucci-Cerinic, M.; Naden, R.P.; Medsger, T.A., Jr.; Carreira, P.E.; et al. 2013 classification criteria for systemic sclerosis: An American college of rheumatology/European league against rheumatism collaborative initiative. Ann. Rheum. Dis. 2013, 72, 1747–1755. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Kabat-Zinn, J. Mindfulness Based Stress Reduction (MBSR). Constr. Hum. Sci. 2003, 8, 73–83. [Google Scholar]
- Spielberger, C.D. Manual for the State-Trait Anger Expression Inventory-2; Psychological Assessment Resources: Odessa, FL, USA, 1999. [Google Scholar]
- Spielberger, C. Manual for the State-Trait Anxiety Inventory, Revised ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Radloff, L.S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Thombs, B.D.; Hudson, M.; Schieir, O.; Taillefer, S.S.; Baron, M.; The Canadian Scleroderma Research Group. Reliability and validity of the center for epidemiologic studies depression scale in patients with systemic sclerosis. Arthritis Rheum. 2008, 59, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The measurement of pessimism: The Hopelessness Scale. J. Consult. Clin. Psychol. 1974, 42, 861–865. [Google Scholar] [CrossRef] [PubMed]
- Feldman, G.; Hayes, A.; Kumar, S.; Greeson, J.; Laurenceau, J.-P. Mindfulness and Emotion Regulation: The Development and Initial Validation of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R). J. Psychopathol. Behav. Assess. 2006, 29, 177–190. [Google Scholar] [CrossRef]
- Apolone, G.; Mosconi, P. The Italian SF-36 Health Survey: Translation, Validation and Norming. J. Clin. Epidemiol. 1998, 51, 1025–1036. [Google Scholar] [CrossRef]
- Kirwan, J.R.; Reeback, J.S. Stanford Health Assessment Questionnaire modified to assess disability in British patients with rheumatoid arthritis. Br. J. Rheumatol. 1986, 25, 206–209. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Aranda, A.; Feliu-Soler, A.; Montero-Marín, J.; García-Campayo, J.; Andrés-Rodríguez, L.; Borràs, X.; Rozadilla-Sacanell, A.; Peñarrubia-Maria, M.T.; Angarita-Osorio, N.; McCracken, L.M.; et al. A randomized controlled efficacy trial of mindfulness-based stress reduction compared with an active control group and usual care for fibromyalgia: The EUDAIMON study. Pain 2019, 160, 2508–2523. [Google Scholar] [CrossRef]
- Haugmark, T.; Hagen, K.B.; Smedslund, G.; Zangi, H.A. Mindfulness- and acceptance-based interventions for patients with fibromyalgia—A systematic review and meta-analyses. PLoS ONE 2019, 14, e0221897. [Google Scholar] [CrossRef]
- Andrés-Rodríguez, L.; Borràs, X.; Feliu-Soler, A.; Pérez-Aranda, A.; Rozadilla-Sacanell, A.; Montero-Marin, J.; Maes, M.; Luciano, J.V. Immune-inflammatory pathways and clinical changes in fibromyalgia patients treated with Mindfulness-Based Stress Reduction (MBSR): A randomized, controlled clinical trial. Brain Behav. Immun. 2019, 80, 109–119. [Google Scholar] [CrossRef]
- Fogarty, F.A.; Booth, R.J.; Gamble, G.D.; Dalbeth, N.; Consedine, N.S. The effect of mindfulness-based stress reduction on disease activity in people with rheumatoid arthritis: A randomised controlled trial. Ann. Rheum. Dis. 2015, 74, 472–474. [Google Scholar] [CrossRef]
- Maddali-Bongi, S.; Orlandi, M.; Pollina, A.; El Aoufy, K. Mindfulness Program in Sjögren’s Syndrome and Non-Sjögren’s Sicca Syndrome Patients: A Pilot Study on Quality of Life and Psychological Distress. Altern. Complement. Ther. 2019, 25, 241–247. [Google Scholar] [CrossRef]
- Grossman, P.; Deuring, G.; Walach, H.; Schwarzer, B.; Schmidt, S. Mindfulness-Based Intervention Does Not Influence Cardiac Autonomic Control or the Pattern of Physical Activity in Fibromyalgia During Daily Life: An Ambulatory, Multimeasure Randomized Controlled Trial. Clin. J. Pain. 2017, 33, 385–394. [Google Scholar] [CrossRef]
- Straub, R.H.; Cutolo, M. Psychoneuroimmunology—Developments in stress research. Wien. Med. Wochenschr. 2018, 168, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Graninger, M. Verhaltenstraining als zusätzlicher Therapieansatz bei rheumatoider Arthritis (Behavioral training as additional therapy approach for rheumatoid arthritis). Z. Rheumatol. 2015, 74, 579–583. (In German) [Google Scholar] [CrossRef]
- Malakoutikhah, A.; Zakeri, M.A.; Dehghan, M. A Comparison between the Relaxation/Meditation/Mindfulness Tracker t Inventory and the Freiburg Mindfulness Inventory for Predicting General Health, Anxiety, and Anger in Adult General Population. Front. Psychol. 2022, 13, 810383. [Google Scholar] [CrossRef] [PubMed]
- Hirano, M.; Yukawa, S. The impact of mindfulness meditation on anger. Shinrigaku Kenkyu 2013, 84, 93–102. (In Japanese) [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Wang, H.; Luo, J.; Guo, Y.; Xie, Y.; Lei, B.; Wiley, J.; Whittemore, R. Factors influencing the effect of mindfulness-based interventions on diabetes distress: A meta-analysis. BMJ Open Diabetes Res. Care 2019, 7, e000757. [Google Scholar] [CrossRef] [PubMed]
- Carmody, J.; Baer, R.A. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J. Behav. Med. 2008, 31, 23–33. [Google Scholar] [CrossRef]
- Horesh, D.; Glick, I.; Taub, R.; Agmon-Levin, N.; Shoenfeld, Y. Mindfulness-based group therapy for systemic lupus erythematosus: A first exploration of a promising mind-body intervention. Complement. Ther. Clin. Pract. 2017, 26, 73–75. [Google Scholar] [CrossRef]
| MBSR Group (n = 16) % or M ± SD | Control Group (n = 16) % or M ± SD | p-Value | |
|---|---|---|---|
| Age (years) | 61.9 ± 12.9 | 54.5 ± 12.9 | 0.12 |
| Years of SSc diagnosis (months) | 80.3 ± 65.2 | 122.9 ± 86.4 | 0.15 |
| Years of education | 11.8 ± 3.3 | 12.06 ± 3.3 | 0.86 |
| Education NO | 18.75% | 0% | 0.25 |
| Education media | 18.75% | 31.25% | |
| Education college | 37.5% | 56.25% | |
| Education University | 25% | 12.5% | |
| No occupation | 25% | 50% | 0.13 |
| Yes occupation | 18.75% | 31.25% | |
| Retired | 56.25% | 18.75% | |
| Comorbidity YES | 56.25% | 37.5% | 0.47 |
| Comorbidity NO | 43.75% | 62.5% | |
| Physical Functionality (HAQ-DI) | 0.51 ± 0.59 | 0.21 ± 0.33 | 0.07 |
| State Anxiety (STAIY1) | 43.7 ± 12.8 | 46.1 ± 12.1 | 0.60 |
| Trait Anxiety (STAIY2) | 49.2 ± 12.9 | 45.09 ± 13.9 | 0.51 |
| Mindfulness (CAMS) | 72.6 ± 0.7 | 2.6 ± 0.7 | 0.96 |
| Hopelessness (BHS) | 6.4 ± 4.4 | 8.6 ± 6.0 | 0.26 |
| Depression (CESD) | 15.3 ± 8.2 | 19.7 ± 17.6 | 0.97 |
| Physical Health Status (SF36-SPI) | 39.7 ± 10.9 | 42.9 ± 10.6 | 0.27 |
| Mental Health status (SF3-SMI) | 44.3 ± 10.8 | 40.7 ± 13.1 | 0.41 |
| State Anger (STAXI_RS) | 18.4 ± 5.5 | 21.1 ± 12.3 | 0.92 |
| Trait Anger (STAXI_ RT) | 18.0 ± 4.5 | 19.5 ± 6.3 | 0.47 |
| Anger Expression outside (STAXI EROut) | 12.8 ± 2.6 | 13.1 ± 3.4 | 0.81 |
| MBSR Group (n = 16) M ± SD | Control Group (n = 16) M ± SD | p-Value | |
|---|---|---|---|
| Physical Functionality (HAQ-DI) | 0.46 ± 0.52 | 0.16 ± 0.40 | 0.08 |
| State Anxiety (STAIY1) | 37.1 ± 10.7 | 36.5 ± 23.1 | 0.92 |
| Trait Anxiety (STAIY2) | 41.5 ± 10.8 | 37.5 ± 23.8 | 0.56 |
| Mindfulness (CAMS) | 2.9 ± 0.5 | 2.2 ± 1.2 | 0.13 |
| Hopelessness (BHS) | 5.5 ± 3.1 | 8.1 ± 7.2 | 0.53 |
| Depression (CESD) | 12.7 ± 9.7 | 15.1 ± 15.6 | 0.96 |
| Physical Health Status (SF36-SPI) | 38.4 ± 10.4 | 42.8 ± 10.6 | 0.28 |
| Mental Health status (SF36-SMI) | 49.1 ± 9.8 | 40.8 ± 13.3 | 0.07 |
| State Anger (STAXI_RS) | 16.9 ± 3.7 | 17.6 ± 12.2 | 0.65 |
| Trait Anger (STAXI_ RT) | 17.1 ± 5.0 | 15.0 ± 9.9 | 0.45 |
| Anger Expression outside (STAXI EROut) | 13.1 ± 2.7 | 10.6 ± 6.0 | 0.50 |
| Anger Expression inside (STAXI ERin) | 16.9 ± 4.9 | 14.9 ± 9.0 | 0.45 |
| Anger Control outside (STAXI CROut) | 22.1 ± 3.7 | 16.1 ± 9.2 | 0.045 |
| Anger Control outside (STAXI CRin) | 25.3 ± 4.9 | 16.9 ± 9.9 | 0.009 |
| Anger Expression Index (STAXI ER Index) | 30.5 ± 11.3 | 40.3 ± 9.2 | 0.014 |
| Perceived Stress (PSS) | 18.6 ± 4.4 | 18.7 ± 4.9 | 0.97 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El Aoufy, K.; Pezzutto, A.; Pollina, A.; Rasero, L.; Bambi, S.; Bellando-Randone, S.; Guiducci, S.; Maddali-Bongi, S.; Matucci Cerinic, M. Systemic Sclerosis Patients Experiencing Mindfulness-Based Stress Reduction Program: The Beneficial Effect on Their Psychological Status and Quality of Life. Int. J. Environ. Res. Public Health 2023, 20, 2512. https://doi.org/10.3390/ijerph20032512
El Aoufy K, Pezzutto A, Pollina A, Rasero L, Bambi S, Bellando-Randone S, Guiducci S, Maddali-Bongi S, Matucci Cerinic M. Systemic Sclerosis Patients Experiencing Mindfulness-Based Stress Reduction Program: The Beneficial Effect on Their Psychological Status and Quality of Life. International Journal of Environmental Research and Public Health. 2023; 20(3):2512. https://doi.org/10.3390/ijerph20032512
Chicago/Turabian StyleEl Aoufy, Khadija, Arianna Pezzutto, Alessandra Pollina, Laura Rasero, Stefano Bambi, Silvia Bellando-Randone, Serena Guiducci, Susanna Maddali-Bongi, and Marco Matucci Cerinic. 2023. "Systemic Sclerosis Patients Experiencing Mindfulness-Based Stress Reduction Program: The Beneficial Effect on Their Psychological Status and Quality of Life" International Journal of Environmental Research and Public Health 20, no. 3: 2512. https://doi.org/10.3390/ijerph20032512
APA StyleEl Aoufy, K., Pezzutto, A., Pollina, A., Rasero, L., Bambi, S., Bellando-Randone, S., Guiducci, S., Maddali-Bongi, S., & Matucci Cerinic, M. (2023). Systemic Sclerosis Patients Experiencing Mindfulness-Based Stress Reduction Program: The Beneficial Effect on Their Psychological Status and Quality of Life. International Journal of Environmental Research and Public Health, 20(3), 2512. https://doi.org/10.3390/ijerph20032512









