Burnout, Resilience, Supervisory Support, and Quitting Intention among Healthcare Professionals in Saudi Arabia: A National Cross-Sectional Survey
Abstract
1. Introduction
Theoretical Framework
2. Methods
2.1. Study Design
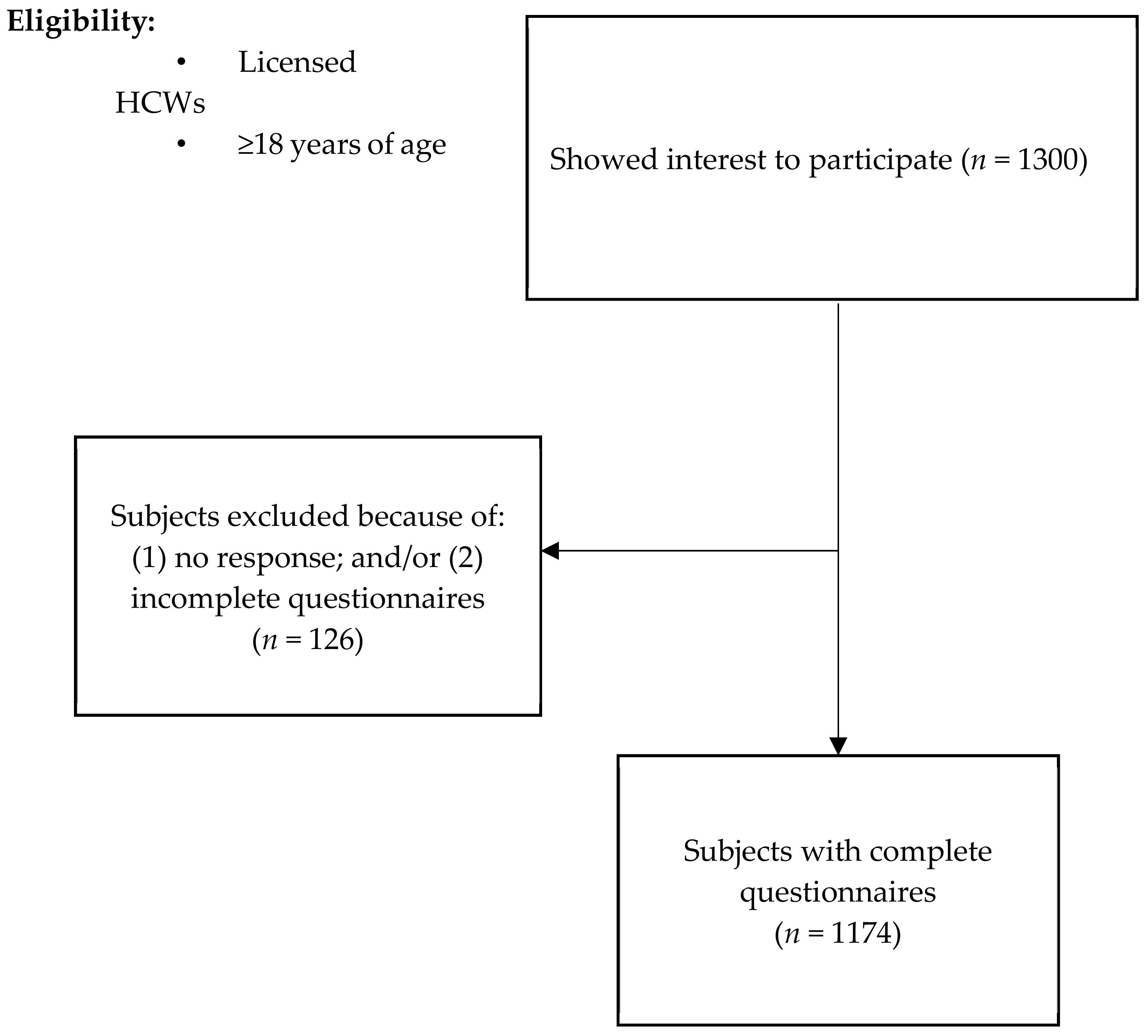
2.2. Participants, Sampling Strategy and Data Collection
2.3. Instruments
2.4. Burnout
2.5. Resilience
2.6. Perceived Supervisory Support Scale (PSS)
2.7. Ethical Consideration
2.8. Statistical Analysis
3. Results
3.1. Prevalence of Burnout
3.2. Factors Associated with Burnout among HCWs
3.3. Associations between Resilience, Burnout, and Intention to Quit
3.4. Associations between Burnout and its Subscales with Supervisory Support
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, W.; Laureys, S.; Di, H. Burnout syndrome in healthcare professionals who care for patients with prolonged disorders of consciousness: A cross-sectional survey. BMC Health Serv. Res. 2020, 20, 841. [Google Scholar] [CrossRef] [PubMed]
- Canadas-De la Fuente, G.A.; Vargas, C.; San Luis, C.; Garcia, I.; Canadas, G.R.; De la Fuente, E.I. Risk factors and prevalence of burnout syndrome in the nursing profession. Int. J. Nurs. Stud. 2015, 52, 240–249. [Google Scholar] [CrossRef]
- West, C.P.; Huschka, M.M.; Novotny, P.J.; Sloan, J.A.; Kolars, J.C.; Habermann, T.M.; Shanafelt, T.D. Association of perceived medical errors with resident distress and empathy: A prospective longitudinal study. JAMA 2006, 296, 1071–1078. [Google Scholar] [CrossRef] [PubMed]
- Panagioti, M.; Geraghty, K.; Johnson, J.; Zhou, A.; Panagopoulou, E.; Chew-Graham, C.; Esmail, A. Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2018, 178, 1317–1331. [Google Scholar] [CrossRef]
- Johnson, J.R.; Emmons, H.C.; Rivard, R.L.; Griffin, K.H.; Dusek, J.A. Resilience Training: A Pilot Study of a Mindfulness-Based Program with Depressed Healthcare Professionals. Explore 2015, 11, 433–444. [Google Scholar] [CrossRef]
- Maunz, S.; Steyrer, J. Burnout syndrome in nursing: Etiology, complications, prevention. Wien. Klin. Wochenschr. 2001, 113, 296–300. [Google Scholar]
- Algarni, S.S.; Algihab, A.A.; Bin Dahmash, H.A.; Alomaireni, A.S.; Alzahrani, R.A.; Alruwaili, A.H.; Alanazi, A.M. Burnout Among Respiratory Therapists in a tertiary hospital in Saudi Arabia. Respir. Care 2022. ahead of print. [Google Scholar] [CrossRef]
- Curtis, W.J.; Cicchetti, D. Moving research on resilience into the 21st century: Theoretical and methodological considerations in examining the biological contributors to resilience. Dev Psychopathol. 2003, 15, 773–810. [Google Scholar] [CrossRef]
- Epstein, R.M.; Krasner, M.S. Physician resilience: What it means, why it matters, and how to promote it. Acad. Med. 2013, 88, 301–303. [Google Scholar] [CrossRef]
- Herrman, H.; Stewart, D.E.; Diaz-Granados, N.; Berger, E.L.; Jackson, B.; Yuen, T. What is resilience? Can. J. Psychiatry 2011, 56, 258–265. [Google Scholar] [CrossRef]
- Nituica, C.; Bota, O.A.; Blebea, J.; Cheng, C.I.; Slotman, G.J. Factors influencing resilience and burnout among resident physicians—A National Survey. BMC Med. Educ. 2021, 21, 514. [Google Scholar] [CrossRef]
- Kutluturkan, S.; Sozeri, E.; Uysal, N.; Bay, F. Resilience and burnout status among nurses working in oncology. Ann. Gen. Psychiatry 2016, 15, 33. [Google Scholar] [CrossRef]
- Kalliath, T.; Morris, R. Job satisfaction among nurses: A predictor of burnout levels. J. Nurs. Adm. 2002, 32, 648–654. [Google Scholar] [CrossRef]
- Fukui, S.; Wu, W.; Salyers, M.P. Impact of Supervisory Support on Turnover Intention: The Mediating Role of Burnout and Job Satisfaction in a Longitudinal Study. Adm. Policy Ment. Health 2019, 46, 488–497. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The job demands-resources model of burnout. J. Appl. Psychol. 2001, 86, 499–512. [Google Scholar] [CrossRef]
- Hobfoll, S.E. Conservation of resources. A new attempt at conceptualizing stress. Am. Psychol. 1989, 44, 513–524. [Google Scholar] [CrossRef]
- Eisenberger, R.; Huntington, R.; Hutchison, S.; Sowa, D. Perceived organizational support. J. Appl. Psychol. 1986, 71, 500. [Google Scholar] [CrossRef]
- Maslach, C.; Schaufeli, W.B. Historical and conceptual development of burnout. In Professional Burnout: Recent Developments in Theory and Research; CRC Press: Boca Raton, FL, USA, 2018; pp. 1–16. [Google Scholar]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Campbell-Sills, L.; Stein, M.B. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J. Trauma Stress 2007, 20, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Elkudssiah Ismail, N.; Hui, W.M.; Goh, K.W.; Jimam, N.S.; Hermansyah, A.; Ming, L.C. Resilience among Malaysian Community Pharmacists and General Medical Practitioners Using the 10-Item Connor-Davidson Resilience Scale (CD-RISC): The First National Survey. Behav. Sci. 2022, 12, 272. [Google Scholar] [CrossRef]
- Eisenberger, R.; Stinglhamber, F.; Vandenberghe, C.; Sucharski, I.L.; Rhoades, L. Perceived supervisor support: Contributions to perceived organizational support and employee retention. J. Appl. Psychol. 2002, 87, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Chemali, Z.; Ezzeddine, F.L.; Gelaye, B.; Dossett, M.L.; Salameh, J.; Bizri, M.; Fricchione, G. Burnout among healthcare providers in the complex environment of the Middle East: A systematic review. BMC Public Health 2019, 19, 1337. [Google Scholar] [CrossRef]
- Linzer, M.; Harwood, E. Gendered Expectations: Do They Contribute to High Burnout Among Female Physicians? J. Gen. Intern. Med. 2018, 33, 963–965. [Google Scholar] [CrossRef]
- Lou, N.M.; Montreuil, T.; Feldman, L.S.; Fried, G.M.; Lavoie-Tremblay, M.; Bhanji, F.; Harley, J.M. Evaluations of Healthcare Providers’ Perceived Support from Personal, Hospital, and System Resources: Implications for Well-Being and Management in Healthcare in Montreal, Quebec, During COVID-19. Eval. Health Prof. 2021, 44, 319–322. [Google Scholar] [CrossRef]
- Hu, D.; Kong, Y.; Li, W.; Han, Q.; Zhang, X.; Zhu, L.X.; Zhu, J. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. EClinicalMedicine 2020, 24, 100424. [Google Scholar] [CrossRef] [PubMed]
- Barr, P. Personality Traits, State Positive and Negative Affect, and Professional Quality of Life in Neonatal Nurses. J. Obstet. Gynecol. Neonatal Nurs. 2018, 47, 771–782. [Google Scholar] [CrossRef]
- Galván, M.E.; Vassallo, J.C.; Rodríguez, S.P.; Otero, P.; Montonati, M.M.; Cardigni, G.; Sarli, M. Professional burnout in pediatric intensive care units in Argentina. Arch. Argent. Pediatr. 2012, 110, 466–473. [Google Scholar] [CrossRef]
- Sasso, L.; Bagnasco, A.; Catania, G.; Zanini, M.; Aleo, G.; Watson, R. Push and pull factors of nurses’ intention to leave. J. Nurs. Manag. 2019, 27, 946–954. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Ball, J.; Reinius, M.; Griffiths, P. Burnout in nursing: A theoretical review. Hum. Resour. Health 2020, 18, 41. [Google Scholar] [CrossRef]
- Buchbinder, S.B.; Wilson, M.; Melick, C.F.; Powe, N.R. Primary care physician job satisfaction and turnover. Am. J. Manag. Care 2001, 7, 701–713. [Google Scholar] [PubMed]
- Hann, M.; Reeves, D.; Sibbald, B. Relationships between job satisfaction, intentions to leave family practice and actually leaving among family physicians in England. Eur. J. Public Health 2011, 21, 499–503. [Google Scholar] [CrossRef]
- Wong, A.V.-K.; Olusanya, O. Burnout and resilience in anaesthesia and intensive care medicine. BJA Educ. 2017, 17, 334–340. [Google Scholar] [CrossRef]
- Hunter, B.; Warren, L. Midwives’ experiences of workplace resilience. Midwifery 2014, 30, 926–934. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E.; Euwema, M.C. Job resources buffer the impact of job demands on burnout. J. Occup. Health Psychol. 2005, 10, 170–180. [Google Scholar] [CrossRef]
| Variable | |
|---|---|
| Age, years (mean (SD)) | 31 (6.2) |
| Gender (male %) | 639 (54.4%) |
| Profession, n (%) | |
| Physicians | 314 (26.7%) |
| Nurse | 444 (37.8%) |
| Respiratory Therapists | 315 (26.8%) |
| Others | 101 (8.7%) |
| Working Hospital, n (%) | |
| Medical City | 361 (30.8%) |
| Military Hospital | 207 (17.6%) |
| Primary Care Clinic | 100 (8.5%) |
| Specialized Hospital | 160 (13.6%) |
| University Hospital | 70 (6%) |
| General Hospital | 228 (19.4%) |
| Psychiatry Hospital | 48 (4.1%) |
| Sector, n (%) | |
| Governmental | 1027 (87.5%) |
| Private | 147 (12.5%) |
| Geographical Region, n (%) | |
| Eastern | 109 (9.3%) |
| Central | 226 (19.2%) |
| Western | 298 (25.4%) |
| Southern | 393 (33.5%) |
| Northern | 148 (12.6%) |
| Working Settings, n (%) | |
| General Wards | 258 (22%) |
| ER | 105 (9%) |
| ICUs | 317 (27%) |
| OR | 151 (13%) |
| Recovery/Post-op | 129 (11%) |
| Rehabilitation Center | 70 (8%) |
| General Clinic | 46 (4%) |
| Specialized Clinic | 35 (3%) |
| Training Center | 23 (2%) |
| Others | 11 (1%) |
| Years of clinical experience, n (%) | |
| <1 year | 203 (17.3%) |
| 1–4 years | 447 (40.6%) |
| 5–10 years | 133 (11.3%) |
| >10 years | 203 (17.3%) |
| Living arrangements, n (%) | |
| Living alone | 183 (24%) |
| Living with family | 784 (66.8%) |
| Living elsewhere | 107 (9.2%) |
| Marital status, n (%) | |
| Single | 497 (42.3%) |
| Married | 636 (54.2%) |
| Divorced/Separated/Widowed | 41 (3.5%) |
| Monthly income in SR, n (%) | |
| <12,000 | 446 (38%) |
| 12,000–20,000 | 662 (53%) |
| >20,000 | 106 (9%) |
| Current shift work, n (%) | |
| Day | 76 (40%) |
| Night | 114 (60%) |
| Intention to leave the job, n (%) | |
| Yes | 390 (33.2%) |
| No | 784 (66.8%) |
| Burnout | |
| High | 909 (77.4%) |
| Moderate | 111 (9.5%) |
| low | 154 (13.1%) |
| Burnout subscale | |
| Emotional exhaustion | |
| High | 686 (58.4%) |
| Moderate | 251 (21.4%) |
| Low | 237 (20.2%) |
| Depersonalization | |
| High | 850 (72.4%) |
| Moderate | 124 (10.6%) |
| Low | 200 (17%) |
| Personal accomplishment | |
| Low | 775 (66%) |
| Moderate | 193 (16.4%) |
| High | 206 (17.6%) |
| Variables | OR Burnout | 95% CI |
|---|---|---|
| Gender | ||
| Male | Reference | Reference |
| Female | 1.47 | 1.04–2.06 |
| Marital status | ||
| Single | Reference | Reference |
| Married | 0.28 | 0.13–0.58 |
| Divorced/widowed | 0.71 | 0.49–1.02 |
| Years of clinical experience | ||
| <1 year | References | References |
| 1–4 years | 1.2 | 0.65–2.26 |
| 5–9 years | 0.91 | 0. 54–1.5 |
| >10 years | 0.17 | 0.10–0.30 |
| Monthly income (SR) | ||
| <20,000 SR | Reference | Reference |
| >20,000 SR | 0.90 | 0.51–1.41 |
| PSS, mean (SD) PSS levels, n (%) High (5.1–7.0) Medium (3.0–5.0) Low (0.1–2.9) | 2.81 (0.68) 144 (12.3%) 473 (40.3%) 556 (47.4%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siraj, R.A.; Alhaykan, A.E.; Alrajeh, A.M.; Aldhahir, A.M.; Alqahtani, J.S.; Bakhadlq, S.; Alghamdi, S.M.; Alqarni, A.A.; Alqarni, M.M.; Alanazi, T.M.; et al. Burnout, Resilience, Supervisory Support, and Quitting Intention among Healthcare Professionals in Saudi Arabia: A National Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2023, 20, 2407. https://doi.org/10.3390/ijerph20032407
Siraj RA, Alhaykan AE, Alrajeh AM, Aldhahir AM, Alqahtani JS, Bakhadlq S, Alghamdi SM, Alqarni AA, Alqarni MM, Alanazi TM, et al. Burnout, Resilience, Supervisory Support, and Quitting Intention among Healthcare Professionals in Saudi Arabia: A National Cross-Sectional Survey. International Journal of Environmental Research and Public Health. 2023; 20(3):2407. https://doi.org/10.3390/ijerph20032407
Chicago/Turabian StyleSiraj, Rayan A., Ahmed E. Alhaykan, Ahmed M. Alrajeh, Abdulelah M. Aldhahir, Jaber S. Alqahtani, Samah Bakhadlq, Saeed M. Alghamdi, Abdullah A. Alqarni, Manal M. Alqarni, Turki M. Alanazi, and et al. 2023. "Burnout, Resilience, Supervisory Support, and Quitting Intention among Healthcare Professionals in Saudi Arabia: A National Cross-Sectional Survey" International Journal of Environmental Research and Public Health 20, no. 3: 2407. https://doi.org/10.3390/ijerph20032407
APA StyleSiraj, R. A., Alhaykan, A. E., Alrajeh, A. M., Aldhahir, A. M., Alqahtani, J. S., Bakhadlq, S., Alghamdi, S. M., Alqarni, A. A., Alqarni, M. M., Alanazi, T. M., Alruwaili, A., Algarni, S. S., Alahmadi, F. H., Alahmari, M., & Alahmadi, R. H. (2023). Burnout, Resilience, Supervisory Support, and Quitting Intention among Healthcare Professionals in Saudi Arabia: A National Cross-Sectional Survey. International Journal of Environmental Research and Public Health, 20(3), 2407. https://doi.org/10.3390/ijerph20032407







