Learning Laparoscopic Radical Hysterectomy: Are We Facing an Emerging Situation?
Abstract
1. Introduction
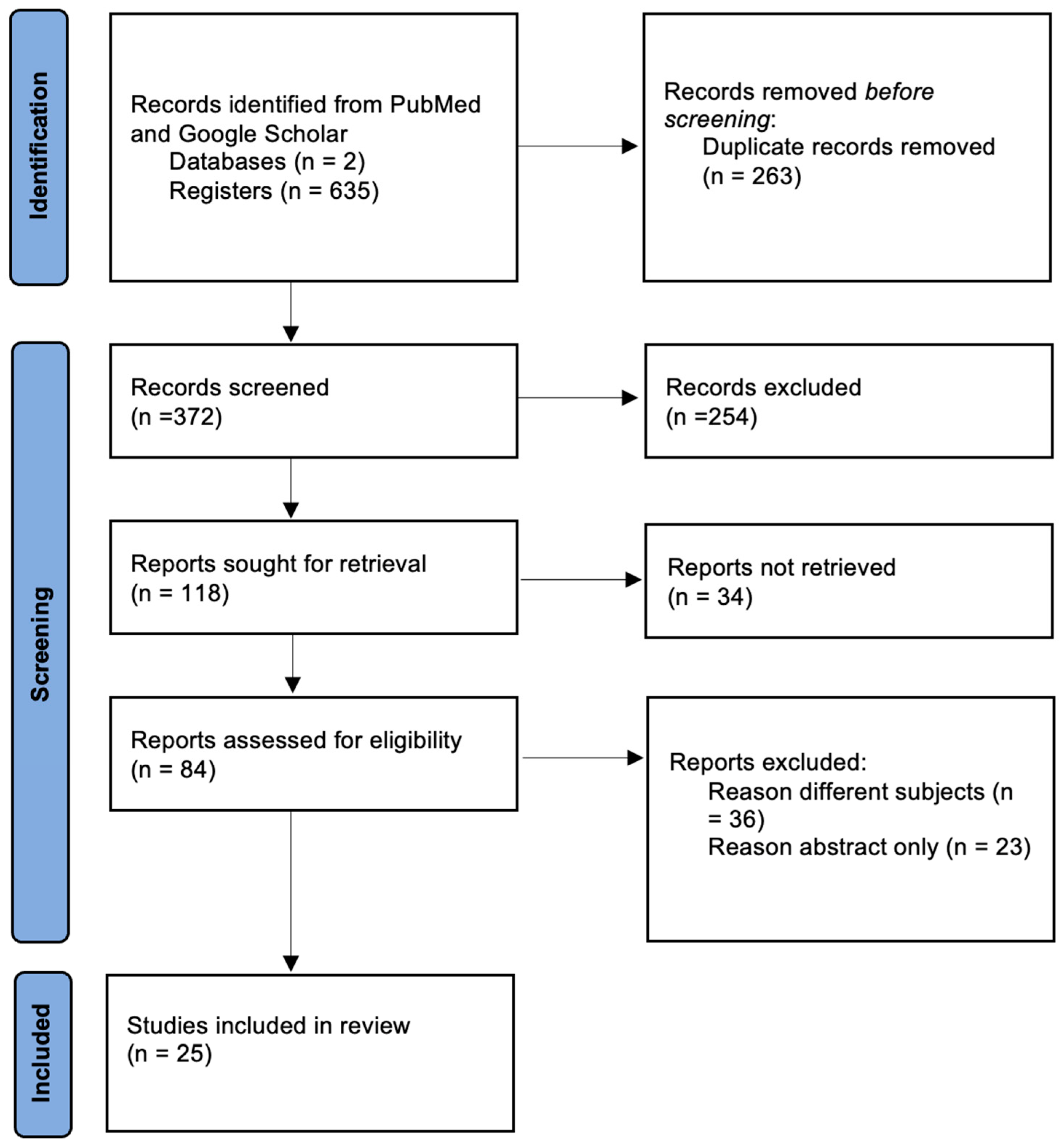
2. Materials and Methods
3. Radical Hysterectomy Learning Curve: In Numbers and Percentages
4. Is the Number of Radical Hysterectomies Performed Decreasing?
5. The LACC Trial: Did It Change Surgeons’ Attitude?
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, S.; Min, K.J.; Lee, S.; Hong, J.H.; Song, J.Y.; Lee, J.K.; Lee, N.W. Learning Curve Could Affect Oncologic Outcome of Minimally Invasive Radical Hysterectomy for Cervical Cancer. Asian J. Surg. 2021, 44, 174–180. [Google Scholar] [CrossRef]
- Schreuder, H.W.R.; Zweemer, R.P.; van Baal, W.M.; van de Lande, J.; Dijkstra, J.C.; Verheijen, R.H.M. From Open Radical Hysterectomy to Robot-Assisted Laparoscopic Radical Hysterectomy for Early Stage Cervical Cancer: Aspects of a Single Institution Learning Curve. Gynecol. Surg. 2010, 7, 253–258. [Google Scholar] [CrossRef]
- Zakashansky, K.; Bradley, W.H.; Nezhat, F.R. New Techniques in Radical Hysterectomy. Curr. Opin. Obs. Gynecol. 2008, 20, 14–19. [Google Scholar] [CrossRef]
- Yaribakht, S.; Guillemin, F.; Harter, V.; Malartic, C.; Marchal, F. New approach of learning curve for robotic-assisted gynecologic oncology surgery. Gynecol. Obs. Fertil. 2015, 43, 348–355. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Li, L.Y.; Wen, L.Y.; Park, S.H.; Nam, E.J.; Lee, J.Y.; Kim, S.; Kim, Y.T.; Kim, S.W. Impact of the Learning Curve on the Survival of Abdominal or Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer. Cancer Res. Treat. 2021, 53, 243–251. [Google Scholar] [CrossRef]
- Pedone Anchora, L.; Bizzarri, N.; Gallotta, V.; Chiantera, V.; Fanfani, F.; Fagotti, A.; Cosentino, F.; Vizzielli, G.; Carbone, V.; Ferrandina, G.; et al. Impact of Surgeon Learning Curve in Minimally Invasive Radical Hysterectomy on Early Stage Cervical Cancer Patient Survival. Facts Views Vis. Obgyn 2021, 13, 231–239. [Google Scholar] [CrossRef]
- Eoh, K.J.; Lee, J.-Y.; Nam, E.J.; Kim, S.; Kim, S.W.; Kim, Y.T. The Institutional Learning Curve Is Associated with Survival Outcomes of Robotic Radical Hysterectomy for Early-Stage Cervical Cancer-a Retrospective Study. BMC Cancer 2020, 20, 152. [Google Scholar] [CrossRef]
- Kong, T.-W.; Chang, S.-J.; Paek, J.; Park, H.; Kang, S.W.; Ryu, H.-S. Learning Curve Analysis of Laparoscopic Radical Hysterectomy for Gynecologic Oncologists without Open Counterpart Experience. Obs. Gynecol. Sci. 2015, 58, 377–384. [Google Scholar] [CrossRef]
- Liu, Y.; Li, L.; Wu, M.; Ma, S.; Tan, X.; Zhong, S.; Lang, J. The Impact of the Surgical Routes and Learning Curve of Radical Hysterectomy on the Survival Outcomes in Stage IB Cervical Cancer: A Retrospective Cohort Study. Int. J. Surg. 2019, 68, 72–77. [Google Scholar] [CrossRef]
- Yim, G.W.; Kim, S.W.; Nam, E.J.; Kim, S.; Kim, Y.T. Learning Curve Analysis of Robot-Assisted Radical Hysterectomy for Cervical Cancer: Initial Experience at a Single Institution. J. Gynecol. Oncol. 2013, 24, 303–312. [Google Scholar] [CrossRef]
- Hwang, J.H.; Yoo, H.J.; Joo, J.; Kim, S.; Lim, M.C.; Song, Y.J.; Park, S.-Y. Learning Curve Analysis of Laparoscopic Radical Hysterectomy and Lymph Node Dissection in Early Cervical Cancer. Eur. J. Obs. Gynecol. Reprod. Biol. 2012, 163, 219–223. [Google Scholar] [CrossRef]
- Oladokun, A.; Morhason-Bello, I.O.; Bello, F.A.; Adewole, I.F. The Learning Curve of Radical Hysterectomy for Early Cervical Carcinoma. Afr. J. Med. Med. Sci. 2010, 39, 329–332. [Google Scholar]
- Chong, G.O.; Park, N.Y.; Hong, D.G.; Cho, Y.L.; Park, I.S.; Lee, Y.S. Learning Curve of Laparoscopic Radical Hysterectomy with Pelvic and/or Para-Aortic Lymphadenectomy in the Early and Locally Advanced Cervical Cancer: Comparison of the First 50 and Second 50 Cases. Int. J. Gynecol. Cancer 2009, 19, 1459–1464. [Google Scholar] [CrossRef]
- Heo, Y.J.; Kim, S.; Min, K.J.; Lee, S.; Hong, J.H.; Lee, J.K.; Lee, N.W.; Song, J.Y. The Comparison of Surgical Outcomes and Learning Curves of Radical Hysterectomy by Laparoscopy and Robotic System for Cervical Cancer: An Experience of a Single Surgeon. Obs. Gynecol. Sci. 2018, 61, 468–476. [Google Scholar] [CrossRef]
- Qin, M.; Siyi, L.; Huang, H.-F.; Li, Y.; Gu, Y.; Wang, W.; Shan, Y.; Yin, J.; Wang, Y.-X.; Cai, Y.; et al. A Comparison of Laparoscopies and Laparotomies for Radical Hysterectomy in Stage IA1-IB1 Cervical Cancer Patients: A Single Team With 18 Years of Experience. Front. Oncol. 2020, 10, 1738. [Google Scholar] [CrossRef]
- Kim, Y.B.; Suh, D.H.; Kim, K.; No, J.H. Case Selection Is a Fundamental Prerequisite to the Successful Surmounting of Learning Curve of Laparoscopic Radical Hysterectomy in Early-Stage Cervical Cancer: A Matched-Case Comparison in a Single Institution. J. Minim. Invasive Gynecol. 2015, 22, S97. [Google Scholar] [CrossRef]
- Lycke, K.D.; Kahlert, J.; Damgaard, R.; Mogensen, O.; Hammer, A. Trends in Hysterectomy Incidence Rates During 2000-2015 in Denmark: Shifting from Abdominal to Minimally Invasive Surgical Procedures. Clin. Epidemiol. 2021, 13, 407–416. [Google Scholar] [CrossRef]
- Reade, C.; Hauspy, J.; Schmuck, M.-L.; Moens, F. Characterizing the Learning Curve for Laparoscopic Radical Hysterectomy: Buddy Operating as a Technique for Accelerating Skill Acquisition. Int. J. Gynecol. Cancer 2011, 21, 930–935. [Google Scholar] [CrossRef]
- Undurraga, M.; Loubeyre, P.; Dubuisson, J.-B.; Schneider, D.; Petignat, P. Early-Stage Cervical Cancer: Is Surgery Better than Radiotherapy? Expert Rev. Anticancer Ther. 2010, 10, 451–460. [Google Scholar] [CrossRef]
- Pecorino, B.; D’Agate, M.G.; Scibilia, G.; Scollo, P.; Giannini, A.; Di Donna, M.C.; Chiantera, V.; Laganà, A.S. Evaluation of Surgical Outcomes of Abdominal Radical Hysterectomy and Total Laparoscopic Radical Hysterectomy for Cervical Cancer: A Retrospective Analysis of Data Collected before the LACC Trial. Int. J. Environ. Res. Public Health 2022, 19, 13176. [Google Scholar] [CrossRef]
- Di Donna, M.C.; Giallombardo, V.; Lo Balbo, G.; Cucinella, G.; Sozzi, G.; Capozzi, V.A.; Abbate, A.; Laganà, A.S.; Garzon, S.; Chiantera, V. Conventional Laparoscopy versus Robotic-Assisted Aortic Lymph-Nodal Staging for Locally Advanced Cervical Cancer: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 3332. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.I.; Choi, B.R.; Kim, H.S.; Chung, H.H.; Kim, J.-W.; Park, N.H.; Song, Y.-S.; Choi, C.H.; Lee, M. Cervical Conization before Primary Radical Hysterectomy Has a Protective Effect on Disease Recurrence in Early Cervical Cancer: A Two-Center Matched Cohort Study According to Surgical Approach. Gynecol. Oncol. 2022, 164, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, P.T.; Frumovitz, M.; Pareja, R.; Lopez, A.; Vieira, M.; Ribeiro, R.; Buda, A.; Yan, X.; Shuzhong, Y.; Chetty, N.; et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N. Engl. J. Med. 2018, 379, 1895–1904. [Google Scholar] [CrossRef] [PubMed]
- Schaafsma, M.; Plante, M.; Mom, C.H.; van Trommel, N.E. Is Less More in the Surgical Treatment of Early-Stage Cervical Cancer? Curr. Opin. Oncol. 2022, 34, 473–489. [Google Scholar] [CrossRef] [PubMed]
- Lewicki, P.J.; Basourakos, S.P.; Qiu, Y.; Hu, J.C.; Sheyn, D.; Hijaz, A.; Shoag, J.E. Effect of a Randomized, Controlled Trial on Surgery for Cervical Cancer. N. Engl. J. Med. 2021, 384, 1669–1671. [Google Scholar] [CrossRef]
- Valenti, G.; Vitale, S.G.; Tropea, A.; Biondi, A.; Laganà, A.S. Tumor Markers of Uterine Cervical Cancer: A New Scenario to Guide Surgical Practice? Updat. Surg. 2017, 69, 441–449. [Google Scholar] [CrossRef]
- Laganà, A.S.; Gavagni, V.; Musubao, J.V.; Pizzo, A. The Prevalence of Sexually Transmitted Infections among Migrant Female Patients in Italy. Int. J. Gynaecol. Obs. 2015, 128, 165–168. [Google Scholar] [CrossRef]
- Shepherd, J.H.; Milliken, D.A. Conservative Surgery for Carcinoma of the Cervix. Clin. Oncol. 2008, 20, 395–400. [Google Scholar] [CrossRef]
- Scioscia, M.; Noventa, M.; Palomba, S.; Laganà, A.S. Effect of the COVID-19 Pandemic on Oncology Screenings: It Is Time to Change Course. BJOG 2021, 128, 2213–2214. [Google Scholar] [CrossRef]
- NIHR Global Health Unit on Global Surgery; COVIDSurg Collaborative. Elective Surgery System Strengthening: Development, Measurement, and Validation of the Surgical Preparedness Index across 1632 Hospitals in 119 Countries. Lancet 2022, 400, 1607–1617. [Google Scholar] [CrossRef] [PubMed]
- Lukanović, D.; Laganà, A.S. The Impact of COVID-19 on Simulation-Based Learning of Gynecology and Obstetrics Skills. Minim. Invasive Ther. Allied Technol. 2022, 31, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Vitale, S.G.; La Rosa, V.L.; Rapisarda, A.M.C.; Laganà, A.S. Fertility Preservation in Women with Gynaecologic Cancer: The Impact on Quality of Life and Psychological Well-Being. Hum. Fertil. 2018, 21, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Vitale, S.G.; La Rosa, V.L.; Rapisarda, A.M.C.; Laganà, A.S. The Importance of Fertility Preservation Counseling in Patients with Gynecologic Cancer. J. Reprod. Infertil. 2017, 18, 261–263. [Google Scholar]
- Giannini, A.; D’Oria, O.; Chiantera, V.; Margioula-Siarkou, C.; Di Donna, M.C.; Terzic, S.; Sleiman, Z.; Laganà, A.S. Minimally Invasive Surgery for Cervical Cancer: Should We Look beyond Squamous Cell Carcinoma? J. Investig. Surg. 2022, 35, 1602–1603. [Google Scholar] [CrossRef]
- Casarin, J.; Bogani, G.; Papadia, A.; Ditto, A.; Pinelli, C.; Garzon, S.; Donadello, N.; Laganà, A.S.; Cromi, A.; Mueller, M.; et al. Preoperative Conization and Risk of Recurrence in Patients Undergoing Laparoscopic Radical Hysterectomy for Early Stage Cervical Cancer: A Multicenter Study. J. Minim. Invasive Gynecol. 2021, 28, 117–123. [Google Scholar] [CrossRef]
- Allahqoli, L.; Laganà, A.S.; Mazidimoradi, A.; Salehiniya, H.; Günther, V.; Chiantera, V.; Karimi Goghari, S.; Ghiasvand, M.M.; Rahmani, A.; Momenimovahed, Z.; et al. Diagnosis of Cervical Cancer and Pre-Cancerous Lesions by Artificial Intelligence: A Systematic Review. Diagnostics 2022, 12, 2771. [Google Scholar] [CrossRef]
- D’Oria, O.; Corrado, G.; Laganà, A.S.; Chiantera, V.; Vizza, E.; Giannini, A. New Advances in Cervical Cancer: From Bench to Bedside. Int. J. Environ. Res. Public Health 2022, 19, 7094. [Google Scholar] [CrossRef]
| Authors, Year | Patients | Open or Minimally Invasive | Oncological Outcome | Morbidity for the Early Years of the Learning Curve | Morbidity for the Late Years of the Learning Curve |
|---|---|---|---|---|---|
| Kim et al., 2021 [1] | 89 | Open, robotic-assisted, and minimally invasive | Surgical proficiency could significantly affect oncological outcome | Poorer progression-free survival | Improved progression free survival and survival rates |
| Li et al., 2021 [6] | 280 | Open and minimally invasive | 5 year disease-free and overall survival rates | NA | NA |
| Pedone Anchora et al., 2021 [7] | 243 | Minimally invasive | 3-year disease-free survival | 75.4% | 91.6% |
| Eoh et al., 2020 [8] | 310 | Robotic-assisted and open techniques | Progression-free survival and overall survival | NA | Operation year decreased morbidity in the late years of the learning curve |
| Kong et al., 2015 [9] | 84 | Minimally invasive | Operating time | Longer operating time | Shorter operating time |
| Liu et al., 2019 [10] | 406 | Open and minimally invasive | 5-year disease-free survival | NA | 5-year disease-free survival increased with years |
| Yim et al., 2013 [11] | 65 | Minimally invasive | Blood loss and early post operative complications | 225 mL blood loss, 28% postop complications | 100 mL blood loss, 8.1% postop complications |
| Hwang et al., 2012 [12] | 70 | Minimally invasive | Mean operating time, complication rate | 307 min, N = 9 | 266 min, N = 1 |
| Oladokun et al., 2010 [13] | 10 | Abdominal | Operative time and blood loss | Linear reduction in surgical blood loss and operative time | |
| Chong et al., 2009 [14] | 100 | Minimally invasive | Operative time, length of hospital stay, transfusion rate | Significant decrease in operative time, length of hospital stay, and transfusion rate | |
| Schreuder et al., 2010 [2] | 28 | Abdominal and robotic assisted | Operative time | 9 h | 4 h |
| Heo et al., 2018 [15] | 41 | Robotic-assisted and laparoscopic | Average operation time | Longer | Shorter |
| Qin et al., 2020 [16] | 256 | Abdominal and minimally invasive | Progression-free survival and overall survival | Similar rates | Similar rates |
| Yaribakht et al., 2015 [4] | 72 | Robotic-assisted | Surgeon console time | Increased surgeon’s console time | Decreased surgeon’s console time |
| Zakashansky et al., 2008 [3] | NA | Abdominal, laparoscopic-assisted, and robotic-assisted | Safety profile, blood loss, hospital stay | NA | Improved safety profile and blood loss with laparoscopic surgery |
| Kim et al., 2015 [17] | 161 | Laparoscopic-assisted | Surgical and survival outcomes | Longer operating time, more intraoperative ureter injury | Lesser blood loss and shorter post op hospital stay |
| Lycke et al., 2021 [18] | 98,484 | Abdominal and minimally invasive surgery | NA | NA | NA |
| Reade et al., 2011 [19] | 45 | Laparoscopic-assisted | Operative time, estimated blood loss, number of lymph nodes removed, hospital stay | 201 min, 355 mL, N = 11.5, 1.57 days | 176 min, 196 mL, N = 15.3, 0.14 days |
| Undurraga et al., 2010 [20] | NA | Laparoscopy | Complication rate, quality of life | NA | NA |
| Pecorino et al., 2022 [21] | 196 | Abdominal and laparoscopic-assisted | Operative time, estimated blood loss, hospital stay, transfusions | NA | NA |
| Di Donna et al., 2022 [22] | 1200 | Laparoscopic and robotic-assisted | Estimated blood loss, hospital stay | NA | Estimated blood loss was higher in laparoscopy compared with robotic surgery, and hospital stay was longer in robotic assisted surgery compared with laparoscopic surgery |
| Kim et al., 2022 [23] | 578 | Abdominal and laparoscopic-assisted | Disease-free survival | NA | NA |
| Ramirez et al., 2018 [24] | 631 | Abdominal and minimally invasive surgery | Disease-free survival and overall survival | NA | NA |
| Schaafsma et al., 2022 [25] | NA | Abdominal and minimally invasive surgery | NA | NA | NA |
| Lewicki et al., 2021 [26] | 2437 | Abdominal and minimally invasive surgery | Number of minimally invasive surgeries performed after LACC trial was published | NA | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moufawad, G.; Laganà, A.S.; Habib, N.; Chiantera, V.; Giannini, A.; Ferrari, F.; Vitagliano, A.; Della Corte, L.; Bifulco, G.; Sleiman, Z. Learning Laparoscopic Radical Hysterectomy: Are We Facing an Emerging Situation? Int. J. Environ. Res. Public Health 2023, 20, 2053. https://doi.org/10.3390/ijerph20032053
Moufawad G, Laganà AS, Habib N, Chiantera V, Giannini A, Ferrari F, Vitagliano A, Della Corte L, Bifulco G, Sleiman Z. Learning Laparoscopic Radical Hysterectomy: Are We Facing an Emerging Situation? International Journal of Environmental Research and Public Health. 2023; 20(3):2053. https://doi.org/10.3390/ijerph20032053
Chicago/Turabian StyleMoufawad, Graziella, Antonio Simone Laganà, Nassir Habib, Vito Chiantera, Andrea Giannini, Federico Ferrari, Amerigo Vitagliano, Luigi Della Corte, Giuseppe Bifulco, and Zaki Sleiman. 2023. "Learning Laparoscopic Radical Hysterectomy: Are We Facing an Emerging Situation?" International Journal of Environmental Research and Public Health 20, no. 3: 2053. https://doi.org/10.3390/ijerph20032053
APA StyleMoufawad, G., Laganà, A. S., Habib, N., Chiantera, V., Giannini, A., Ferrari, F., Vitagliano, A., Della Corte, L., Bifulco, G., & Sleiman, Z. (2023). Learning Laparoscopic Radical Hysterectomy: Are We Facing an Emerging Situation? International Journal of Environmental Research and Public Health, 20(3), 2053. https://doi.org/10.3390/ijerph20032053











