Potential Clinical Applications of Ozone Therapy in Dental Specialties—A Literature Review, Supported by Own Observations
Abstract
1. Introduction
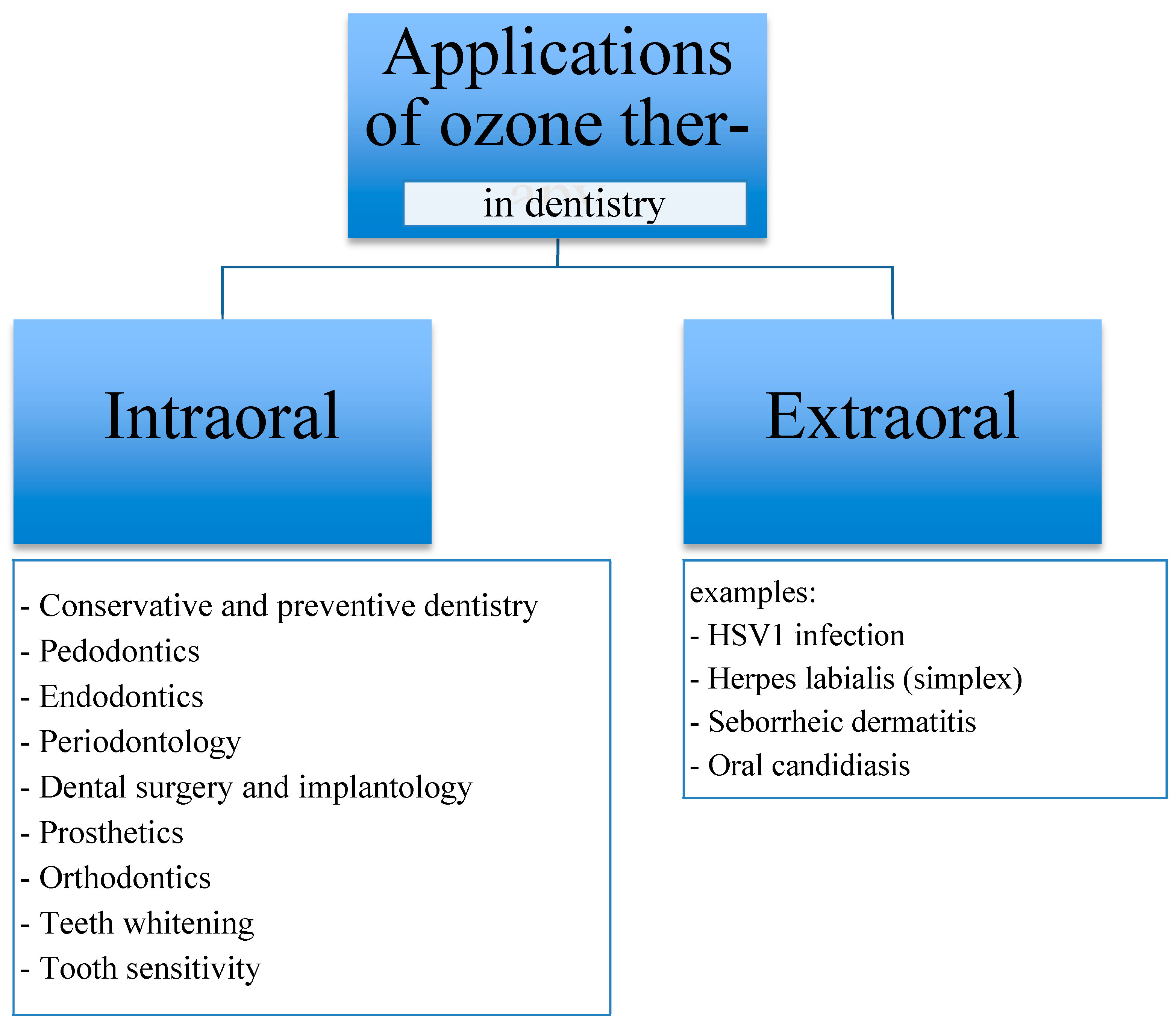
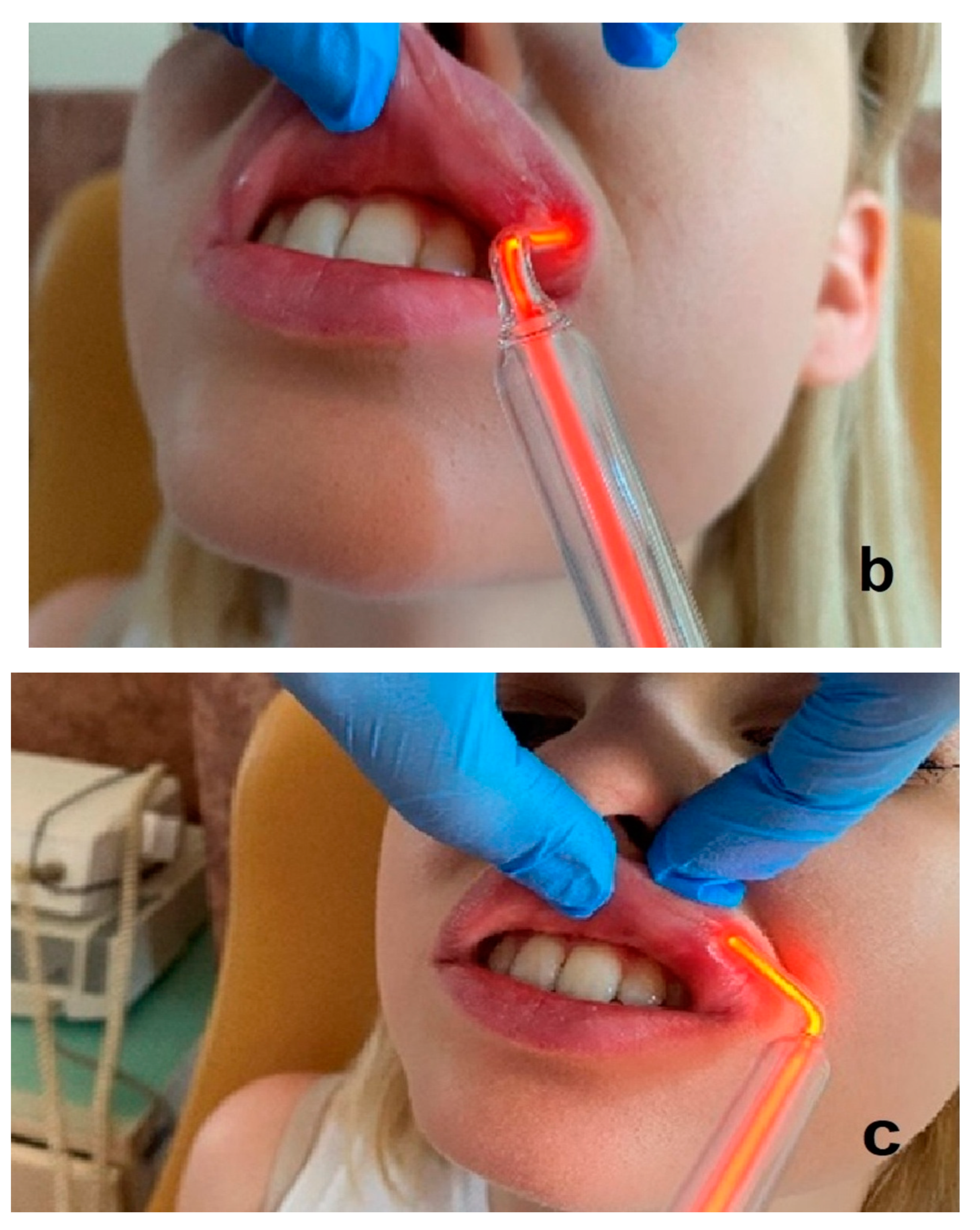
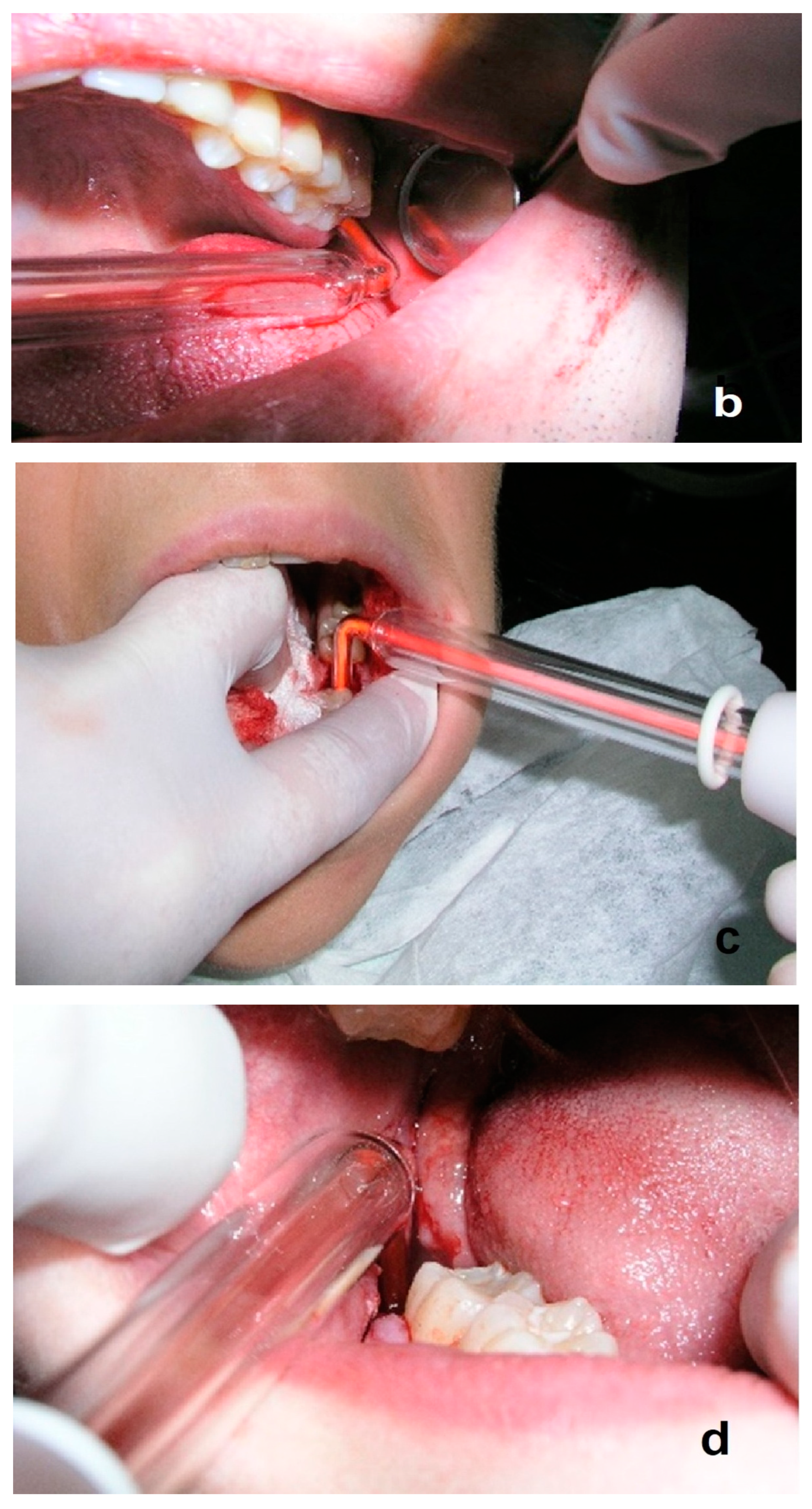
2. Ozone Therapy in Dentistry
3. Ozone Therapy Modalities Used in Dentistry
4. Aim of the Study
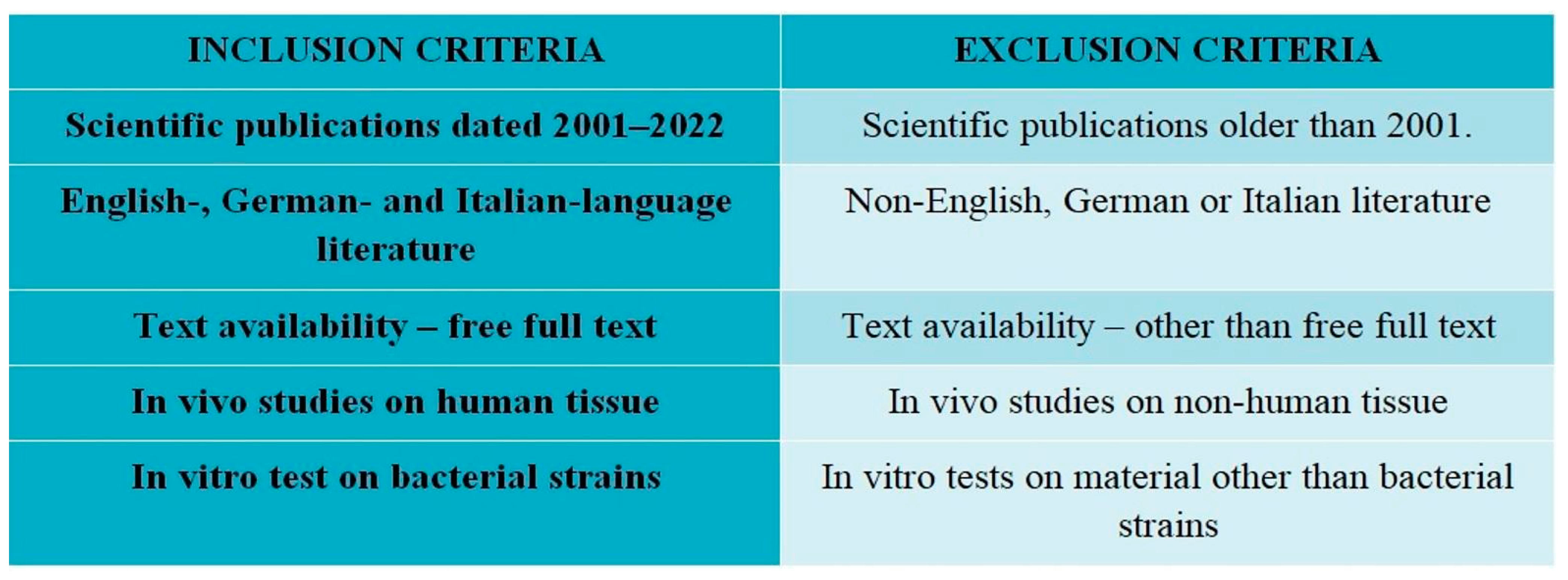
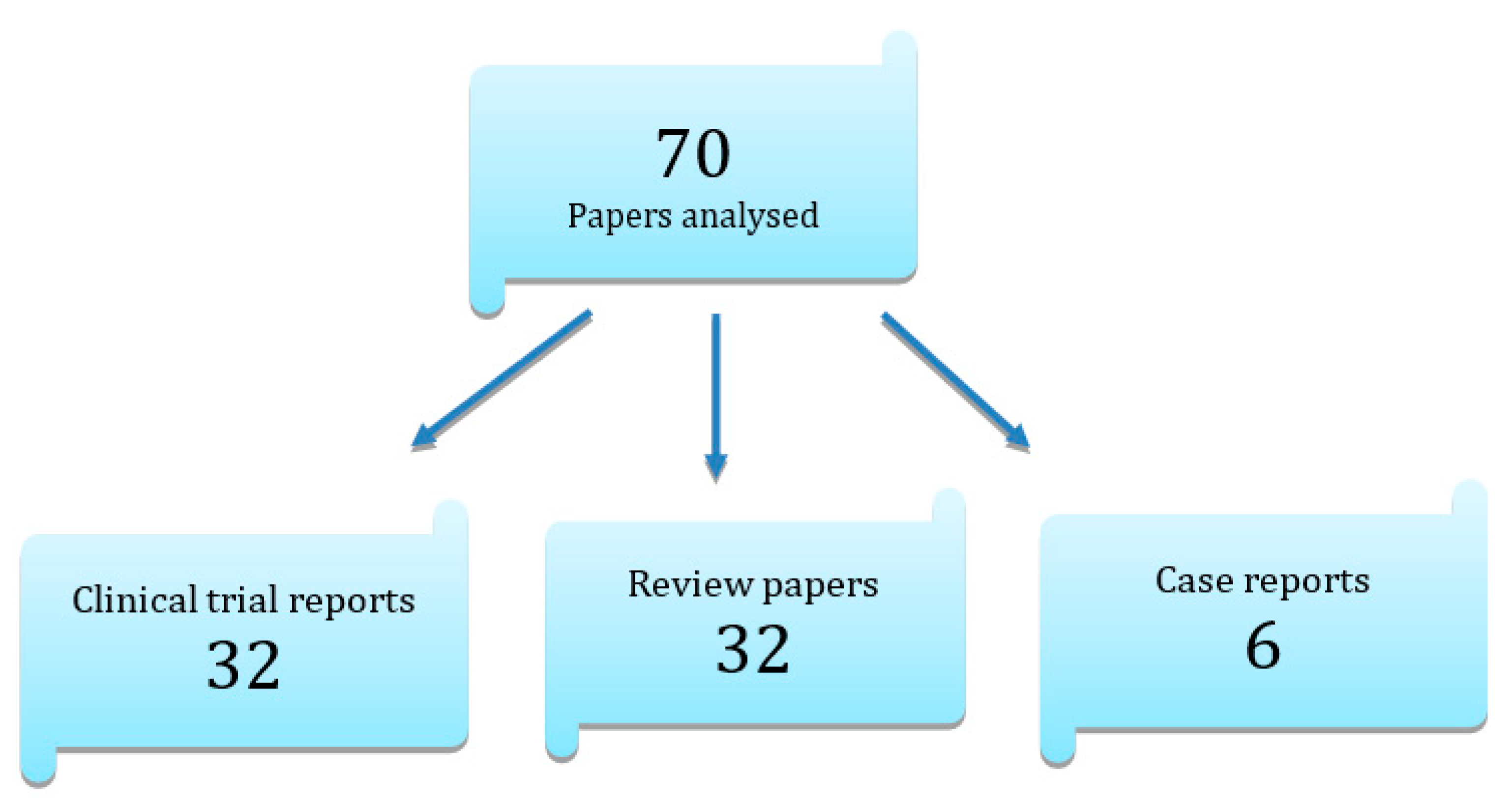
5. Material and Methods
6. Main Issue
6.1. Conservative Dentistry
6.2. Pedodontics
6.3. Teeth Whitening
6.4. Endodontics
6.5. Periodontology
6.6. Tooth Sensitivity
6.7. Dental Surgery and Implantology
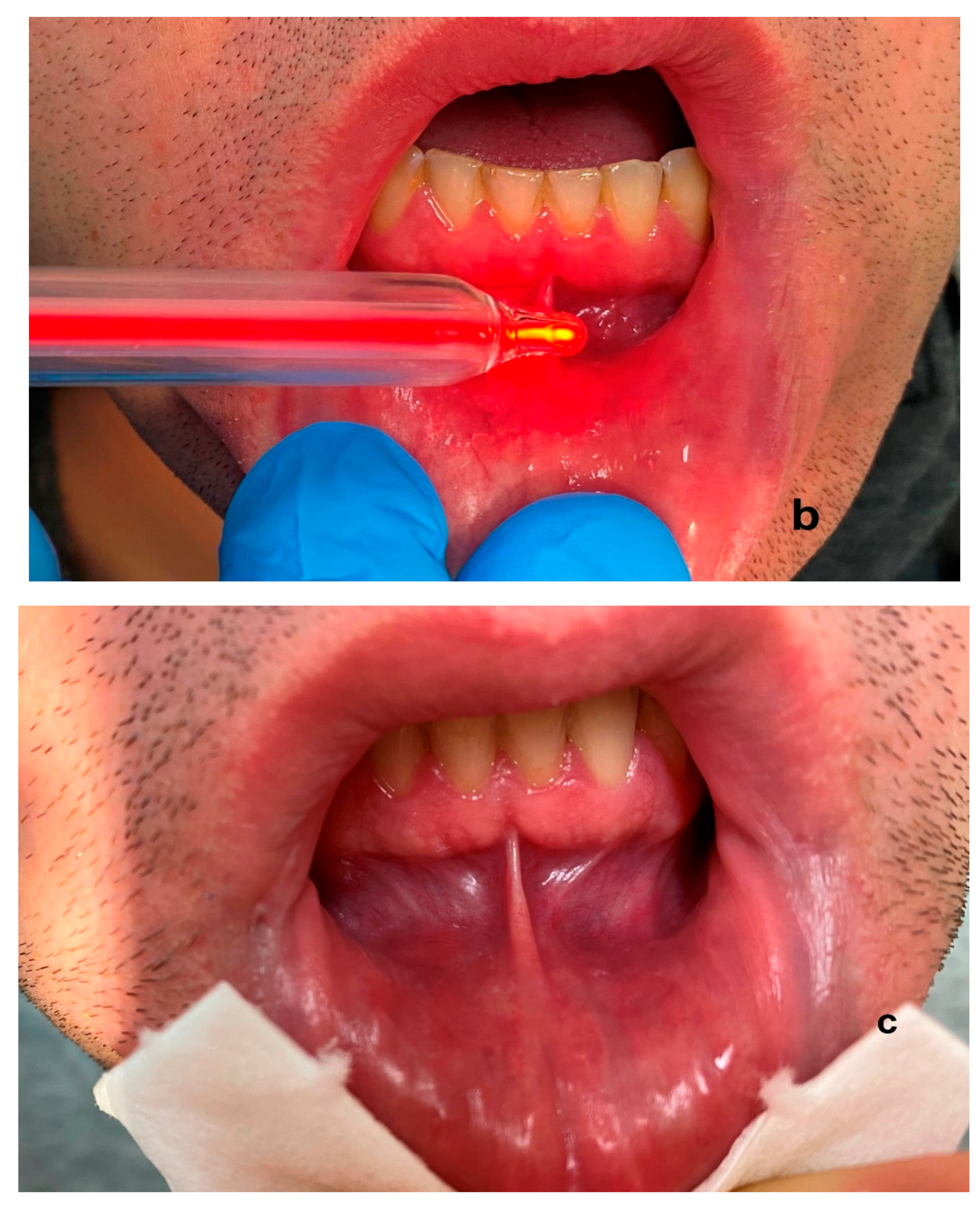
6.8. Temporomandibular Joint Disorders
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Saini, R. Ozone therapy in dentistry: A strategic review. J. Nat. Sci. Biol. Med. 2011, 2, 151–153. [Google Scholar] [CrossRef] [PubMed]
- Nogales, C.G.; Ferrari, P.H.; Kantorovich, E.O.; Lage-Marques, J.L. Ozone therapy in medicine and dentistry. J. Contemp. Dent. Pract. 2008, 9, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Elvis, A.M.; Ekta, J.S. Ozone therapy: A clinical review. J. Nat. Sci. Biol. Med. 2011, 2, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Aydogan, S.; Artis, A.S. How Ozone Treatment Affects Erythrocytes. In Haemodynamics-New Diagnostic and Therapeutic Approaches; Artis, A.S., Ed.; In Tech: Rijeka, Croatia, 2012; pp. 69–84. [Google Scholar]
- Borrelli, E.; Monte, A.; Bocci, V. ReseArch. article oxygen ozone therapy in the integrated treatment of chronic ulcer: A case series report. Int. J. Rec. Sci. Res. 2015, 6, 4132–4136. [Google Scholar]
- Suh, Y.; Patel, S.; Kaitlyn, R.; Gandhi, J.; Joshi, G.; Smith, N.L.; Khan, S.A. Clinical utility of ozone therapy in dental and oral medicine. Med. Gas Res. 2019, 9, 163–167. [Google Scholar]
- Oldoini, G.; Frabattista, G.R.; Saragoni, M.; Cosola, S.; Giammarinaro, E.; Genovesi, A.M.; Marconcini, S. Ozone Therapy for Oral Palatal Ulcer in a Leukaemic Patient. Eur. J. Case Rep. Intern. Med. 2020, 7, 001406. [Google Scholar]
- Louw, A.; Diener, I.; Butler, D.S.; Puentedura, E.J. The Effect of Neuroscience Education on Pain, Disability, Anxiety, and Stress in Chronic Musculoskeletal Pain. Arch. Phys. Med. Rehabil. 2011, 92, 2041–2056. [Google Scholar] [CrossRef]
- Apkarian, A.V.; Baliki, M.N.; Geha, P.Y. Towards a theory of chronic pain. Prog. Neurobiol. 2009, 87, 81–97. [Google Scholar] [CrossRef]
- Devon, I.; Rubin, M.D. Epidemiology and Risk Factors for Spine Pain. Neurol. Clin. 2007, 25, 353–371. [Google Scholar]
- Braidy, N.; Izadi, M.; Sureda, A.; Jonaidi-Jafari, N.; Banki, A.; Nabavi, S.F.; Nabavi, S.M. Therapeutic relevance of ozone therapy in degenerative diseases: Focus on diabetes and spinal pain. Cell. Physiol. 2018, 233, 2705–2714. [Google Scholar] [CrossRef]
- Bocci, V.; Pogni, R. Oxygen-ozone in Orthopaedics: EPR Detection of Hydroxyl Free Radicals in Ozone-Treated ‘NucleusPulposus’ Material. Riv. Neuroradiol. 2001, 14, 55–59. [Google Scholar] [CrossRef]
- Legier, L. Treatment of chronic low back pain incorporating active patient participation and chiropractic: A retrospective case report. J. Chiropr. Med. 2005, 4, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-Tallón, F.J.; Torres-Morera, L.M.; Baeza-Noci, J.; Carrillo-Izquierdo, M.D.; Pinto-Bonilla, R. Updated Review on Ozone Therapy in Pain Medicine. Front. Physiol. 2022, 13, 840623. [Google Scholar] [CrossRef]
- Ma, L.; Yao, M. Safety and Efficacy of CT-Guided Pulsed Radiofrequency Combined with Steroid and Ozone Injection-Treated Cervical 3-8 Herpes Zoster Neuralgia Using a Posterior and Upper Quarter of the Cervical Foramina Puncture Approach. J. Pain Res. 2022, 15, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Sagai, M.; Bocci, V. Mechanisms of Action Involved in Ozone Therapy: Is healing induced via a mild oxidative stress? Med. Gas Res. 2011, 1, 29. [Google Scholar] [CrossRef]
- Bocci, V.; Borrelli, E.; Zanardi, I.; Travagli, V. The usefulness of ozone treatment in spinal pain. Drug Des. Dev. Ther. 2015, 9, 2677–2685. [Google Scholar]
- Steppan, J.; Meaders, T.; Muto, M.; Murphy, K.J. A Meta-analysis of the Effectiveness and Safety of Ozone Treatments for Herniated Lumbar Discs. J. Vasc. Interv. Radiol. 2010, 21, 534–548. [Google Scholar] [CrossRef]
- Hidalgo-Tallón, F.J.; Torres, L.M. Ozonoterapia en medicina del dolor. Revisión. Rev. Soc. Esp. Dolor 2013, 20, 291–300. [Google Scholar] [CrossRef]
- Tsochatzis, E.; Bosch, J.; Burroughs, A. Liver cirrhosis. Lancet 2014, 383, 1749–1761. [Google Scholar] [CrossRef]
- Bocci, V. Visual Improvement Following Ozonetherapy in Dry Age Related Macular Degeneration; a Review. Med. Hypothesis Discov. Innov. Ophthalmol. 2013, 2, 47–51. [Google Scholar]
- Bocci, V.; Diadori, A. Linee guida per alcune pathologie oculari. Riv. Ital. Ossigeno-Ozonoterapia 2003, 2, 59–61. [Google Scholar]
- Borrelli, E.; Diadori, A.; Zalaffi, A.; Bocci, V. Effects of major ozonated autohemotherapy in the treatment of dry age related macular degeneration: A randomized controlled clinical study. Int. J. Ophthalmol. 2012, 5, 708–713. [Google Scholar]
- Bocci, V.A. Scientific and medical aspects of ozone therapy. State of the art. A review. Arch. Med. Res. 2006, 37, 425–435. [Google Scholar] [CrossRef]
- Leroy, P.; Tham, A.; Wong, H.; Tenney, R.; Chen, C.; Stiner, R.; Balmes, J.R.; Paquet, A.C.; Arjomandi, M. Inflammatory and repair pathways induced in human bronchoalveolar lavage cells with ozone inhalation. PLoS ONE 2015, 10, e0127283. [Google Scholar] [CrossRef] [PubMed]
- Smith, N.L.; Wilson, A.L.; Gandhi, J.; Vatsia, S.; Khan, S.A. Ozone therapy: An overview of pharmacodynamics, current research, and clinical utility. Med. Gas Res. 2017, 7, 212–219. [Google Scholar]
- Bocci, V. The case for oxygen-ozonetherapy. Br. J. BioMed. Sci. 2007, 64, 44–49. [Google Scholar] [CrossRef] [PubMed]
- De Sire, A.; Agostini, F.; Lippi, L.; Mangone, M.; Marchese, S.; Cisari, C.; Bernetti, A.; Invernizzi, M. Oxygen-Ozone Therapy in the Rehabilitation Field:State of the Art on Mechanisms of Action, Safety andEffectiveness in Patients with Musculoskeletal Disorders. Biomolecules 2021, 11, 356. [Google Scholar] [CrossRef] [PubMed]
- Bocci, V. OZONE A New Medical Drug; Springer: Berlin/Heidelberg, Germany, 2005; ISBN 9781402031403. [Google Scholar]
- Żukowski, P.; Maciejczyk, M.; Waszkiel, D. Sources of free radicals and oxidative stress in the oral cavity. Arch. Oral Biol. 2018, 92, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Di Mauro, R.; Cantarella, G.; Bernardini, R.; Di Rosa, M.; Barbagallo, I.; Distefano, A.; Longhitano, L.; Vicario, N.; Nicolosi, D.; Lazzarino, G.; et al. The Biochemical and Pharmacological Properties of Ozone: The Smell of Protection in Acute and Chronic Diseases. Int. J. Mol. Sci. 2019, 20, 634. [Google Scholar] [CrossRef]
- Brusselle, G.G.; Koppelman, G.H. Biologic Therapies for Severe Asthma. N. Engl. J. Med. 2022, 386, 157–171. [Google Scholar] [CrossRef]
- Tonnel, A.B.; Gosset, P.; Tillie-Leblond, I. Characteristics of the Inflammatory Response in Bronchial Lavage Fluids from Patients with Status asthmaticus. Int. Arch. Allergy Immunol. 2001, 124, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Noh, S.U.; Han, Y.W.; Kim, K.M.; Kang, H.; Kim, H.O.; Park, Y.M. Therapeutic effects of topical application of ozone on acute cutaneous wound healing. J. Korean Med. Sci. 2009, 24, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Al-Dalain, S.M.; Martinez, G.; Candelario-Jalil, E.; Menendez, S.; Re, L.; Giuliani, A.; Leon, O.S. Ozone treatment reduces markers of oxidative and endothelial damage in an experimental diabetes model in rats. Pharm. Res. 2001, 44, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Uruno, A.; Yagishita, Y.; Yamamoto, M. The Keap1-Nrf2 system and diabetes mellitus. Arch. Biochem. Biophys. 2015, 566, 76–84. [Google Scholar] [CrossRef]
- Lim, A.K.H. Diabetic nephropathy—Complications and treatment. Int. J. Nephrol. Renovasc. Dis. 2014, 7, 361–381. [Google Scholar] [CrossRef]
- Janic, B.; Umstead, T.M.; Phelps, D.S.; Floros, J. Modulatory effects of ozone on thp-1 cells in response to sp-a stimulation. Am. J. Physiol. Lung. Cell. Mol. Physiol. 2005, 288, L317–L325. [Google Scholar] [CrossRef]
- Valacchi, G.; van der Vliet, A.; Schock, B.C.; Okamoto, T.; Obermuller-Jevic, U.; Cross, C.E.; Packer, L. Ozone exposure activates oxidative stress responses in murine skin. Toxicology 2002, 179, 163–170. [Google Scholar] [CrossRef]
- Kushmakov, R.; Gandhi, J.; Seyam, O.; Jiang, W.; Joshi, G.; Smith, N.L.; Khan, S.A. Ozone therapy for diabetic foot. Med. Gas Res. 2018, 8, 111–115. [Google Scholar]
- Bocci, V.; Borrelli, E.; Travagli, V.; Zanardi, I. The ozone paradox: Ozone is a strong oxidant as well as a medical drug. Med. Res. Rev. 2009, 29, 646–682. [Google Scholar] [CrossRef]
- Jordan, L.; Beaver, K.; Foy, S. Ozone treatment for radiotherapy skin reactions: Is there an evidence base for practice? Eur. J. Oncol. Nurs. 2002, 6, 220–227. [Google Scholar] [CrossRef]
- Domb, W.C. Ozone Therapy in Dentistry. Interv. Neuroradiol. 2014, 20, 632–636. [Google Scholar] [CrossRef] [PubMed]
- Naik, S.V.; Rajeshwari, K.; Kohli, S.; Zohabhasan, S.; Bhatia, S. Ozone- A Biological Therapy in Dentistry- Reality or Myth? Open Dent. J. 2016, 10, 196–206. [Google Scholar] [CrossRef] [PubMed]
- Gupta, G.; Mansi, B. Ozone therapy in periodontics. J. Med. Life. 2012, 5, 59–67. [Google Scholar] [PubMed]
- Song, M.; Zeng, Q.; Xiang, Y.; Gao, L.; Huang, J.; Huang, J.; Wu, K.; Lu, J. The antibacterial effect of topical ozone on the treatment of MRSA skin infection. Mol. Med. Rep. 2018, 17, 2449–2455. [Google Scholar] [CrossRef] [PubMed]
- Longbottom, C.; Ekstrand, K.; Zero, D.; Kambara, M. Novel preventive treatment options. Monogr. Oral Sci. 2009, 21, 156–163. [Google Scholar] [PubMed]
- Gaines, S.; Serota, K.S. The new frontier: Minimally invasive dentistry and ozone aerotheraphy. Oral Health 2005, 95, 47–78. [Google Scholar]
- Liu, J.; Zhang, P.; Tian, J.; Li, L.; Li, J.; Tian, J.H.; Yang, K. Ozone therapy for treating foot ulcers in people with diabetes. Cochrane Database Syst. Rev. 2015, 10, Cd008474. [Google Scholar] [CrossRef]
- Reddy, S.; Reddy, N.; Dinapadu, S.; Reddy, M.; Pasari, S. Role of Ozone Therapy in Minimal Intervention Dentistry and Endodontics—A Review. J. Int. Oral Health 2013, 5, 102–108. [Google Scholar]
- Seydanur Dengizek, E.; Serkan, D.; Abubekir, E.; Aysun Bay, K.; Onder, O.; Arife, C. Evaluating clinical and laboratory effects of ozone in non-surgical periodontal treatment: A randomized controlled trial. J. Appl. Oral Sci. 2019, 27, e20180108. [Google Scholar] [CrossRef]
- Onder, C.; Kurgan, Ş.; Altıngöz, S.M.; Bağış, N.; Uyanık, M.; Serdar, M.A.; Kantarcı, A.; Günhan, M. Impact of non-surgical periodontal therapy on saliva and serum levels of markers of oxidative stress. Clin. Oral Investig. 2017, 21, 1961–1969. [Google Scholar] [CrossRef]
- Huth, K.C.; Quirling, M.; Lenzke, S.; Paschos, E.; Kamereck, K.; Brand, K.; Hickel, R.; Ilie, M. Effectiveness of ozone against periodontal pathogenic microorganisms. Eur. J. Oral Sci. 2011, 119, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Isler, S.C.; Unsal, B.; Soysal, F.; Ozcan, G.; Peker, E.; Karaca, I.R. The effects of ozone therapy as an adjunct to the surgical treatment of peri-implantitis. J. Periodontal Implant. Sci. 2018, 48, 136–151. [Google Scholar] [CrossRef] [PubMed]
- Batinjan, G.; Zore, I.F.; Vuletić, M.; Rupić, I. The use of ozone in the prevention of osteoradionecrosis of the jaw. Saudi Med. J. 2014, 35, 1260–1263. [Google Scholar] [PubMed]
- Jacobson, A.S.; Buchbinder, D.; Hu, K.; Urken, M.L. Paradigm shifts in the management of osteoradionecrosis of the mandible. Oral Oncol. 2010, 46, 795–801. [Google Scholar] [CrossRef] [PubMed]
- Rickard, G.D.; Richardson, R.; Johnson, T.; McColl, D.; Hooper, L. Ozone therapy for the treatment of dental caries. Cochrane Database Syst. Rev. 2004, 3, CD004153. [Google Scholar]
- Nagayoshi, M.; Fukuizumi, T.; Kitamura, C.; Yano, J.; Terashita, M.; Nishihara, T. Efficacy of ozone on survival and permeability of oral microorganisms. Oral Microbiol. Immunol. 2004, 19, 240–246. [Google Scholar] [CrossRef]
- Rumbaugh, K.P.; Sauer, K. Biofilm dispersion. Nat. Rev. Microbiol. 2020, 18, 571–586. [Google Scholar] [CrossRef]
- Baysan, A.; Lynch, E. Effect of ozone on the oral microbiota and clinical severity of primary root caries. Am. J. Dent. 2004, 17, 56–60. [Google Scholar]
- Zanjani, V.; Ghasemi, A.; Torabzadeh, H.; Jamali, M.; Razmavar, S. Bleaching effect of ozone on pigmented teeth. Dent. Res. J. 2015, 12, 20–24. [Google Scholar]
- Azarpazhooh, A.; Limeback, H. The application of ozone in dentistry: A systematic review of literature. J. Dent. 2008, 36, 104–116. [Google Scholar] [CrossRef]
- Bengel, W.M. Digital photography and the assessment of therapeutic results after bleaching procedures. J. Esthet. Restor. Dent. 2003, 15 (Suppl. S1), S21–S32. [Google Scholar] [CrossRef] [PubMed]
- AL-Omiri, K.; Al Nazeh, A.; KIelbassa, A.; Lynch, E. Randomized controlled clinical trial on bleaching sensitivity and whitening efficacy of hydrogen peroxide versus combinations of hydrogen peroxide and ozone. Sci. Rep. 2018, 8, 2407. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, M.G.; de Oliveira, L.D.; Koga-Ito, C.Y.; Jorge, A.O.C. Effectiveness of ozonated water on Candida albicans, Enterococcus faecalis, and endotoxins in root canals. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2008, 105, e85–e91. [Google Scholar] [CrossRef]
- Lynch, E. Comment on “The application of Ozone in dentistry: A systematic review of the literature”. J. Dent. 2009, 37, 406–410. [Google Scholar] [CrossRef]
- Elkarim, I.; Kennedy, J.; Hussey, D. The antimicrobial effects of root canal irrigation and medication. Oral Surg. Oral Med. Oral Pathol. 2007, 103, 560–569. [Google Scholar] [CrossRef]
- Bachanek, T.; Bieżanek, T.; Strycharz, M.; Chałas, R.; Paluch-Oleś, J. Ozone influence on elimination of bacteria from the root canals—Preliminary observations. Pol. J. Environ. Stud. 2008, 17, 316–319. [Google Scholar]
- Estrela, C.; Estrela, C.R.A.; Decurcio, D.; Hollanda, A.; Silva, J. Antimicrobial efficacy of ozonated water, gaseous ozone, sodium hypochlorite and chlorhexidine in infected human root canals. Int. Endod. J. 2007, 40, 85–93. [Google Scholar] [CrossRef]
- Huth, K.C.; Quirling, M.; Maier, S.; Kamereck, K.; Alkhayer, M.; Paschos, E.; Welsch, U.; Miethke, T.; Brand, K.; Hickel, R. Effectiveness of ozone against endodontopathogenic microorganisms in a root canal biofilm model. Int. Endod. J. 2009, 42, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Baysan, A.; Lynch, E. The use of ozone in dentistry and medicine. Prim. Dent. Care 2005, 12, 47–52. [Google Scholar] [CrossRef]
- Lubojanski, A.; Dobrzynski, M.; Nowak, N.; Rewak-Soroczynska, J.; Sztyler, K.; Zakrzewski, W.; Dobrzynski, W.; Szymonowicz, M.; Rybak, Z.; Wiglusz, K.; et al. Application of Selected Nanomaterials and Ozone in Modern Clinical Dentistry. Nanomaterials 2021, 11, 259. [Google Scholar] [CrossRef]
- Eick, S.; Tigan, M.; Sculean, A. Effect of ozone on periodontopathogenic species--an in vitro study. Clin. Oral Investig. 2012, 16, 537–544. [Google Scholar] [CrossRef]
- Kronenberg, O.; Lussi, A.; Ruf, S. Preventive effect of ozone on the development of white spot lesions during multibracket appliance therapy. Angle Orthod. 2009, 79, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Dai, Z.; Liu, M.; Ma, Y.; Cao, L.; Xu, H.H.; Zhang, K.; Bai, Y. Effects of Fluoride and Calcium Phosphate Materials on Remineralization of Mild and Severe White Spot Lesions. BioMed. Res. Int. 2019, 2019, 1271523. [Google Scholar] [CrossRef] [PubMed]
- Almaz, M.E.; Sönmez, I.Ş. Ozone therapy in the management and prevention of caries. J. Formos. Med. Assoc. 2015, 114, 3–11. [Google Scholar] [CrossRef]
- Ozdemir, H.; Toker, H.; Balcı, H.; Ozer, H. Effect of ozone therapy on autogenous bone graft healing in calvarial defects: A histologic and histometric study in rats. J. Periodontal Res. 2013, 48, 722–726. [Google Scholar] [CrossRef]
- Jan, A.; Sandor, G.K.; Brkovic, B.B.; Peel, S.; Evans, A.W.; Clokie, C.M. Effect of hyper- baric oxygen on grafted and nongrafted calvarial critical-sized defects. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 157–163. [Google Scholar] [CrossRef] [PubMed]
- McKenna, D.F.; Borzabadi-Farahani, A.; Lynch, E. The effect of subgingival ozone and/or hydrogen peroxide on the development of peri-implant mucositis: A double-blind randomized controlled trial. Int. J. Oral Maxillofac Implant. 2013, 28, 1483–1489. [Google Scholar] [CrossRef]
- Megighian, G.D. The clinical experience in private general dental practice in Italy. In Ozone: The Revolution in Dentistry; Lynch, E., Ed.; Quintessence: Copenhagen, Denmark, 2004; pp. 243–256. [Google Scholar]
- Dukić, W.; Dukić, O.L.; Milardović, S. The influence of Healozone on micro leakage and fissure penetration of different sealing materials. Coll. Antropol. 2009, 33, 157–162. [Google Scholar]
- Maiya, A. Applications of Ozone in Dentistry. Int. J. Clin. Dent. Sci. 2011, 2, 1–5. [Google Scholar]
- Martínez-Sánchez, G.; Saied, M.; Al-Dalain Menéndez, S.; Re, L.; Giuliani, A.; Candelario-Jalil, E.; Álvarez, H.; Fernández-Montequín, J.I.; León, O.S. Therapeutic efficacy of ozone in patients with diabetic foot. Eur. J. Pharmacol. 2005, 523, 151–161. [Google Scholar] [CrossRef]
- Malik, T.; Kaura, S.; Kakria, P. Dental ozone: A boon for dentistry. Indian J. Dent. Sci. 2020, 12, 49–52. [Google Scholar] [CrossRef]
- Bhateja, S. The miraculous healing therapy “Ozone therapy” in dentistry. Indian J. Dent. 2012, 3, 150–155. [Google Scholar] [CrossRef]
- Maiorana, C.; Grossi, G.B.; Garramone, R.A.; Manfredini, R.; Santoro, F. Do ultrasonic dental scalers interfere with implantable cardioverter defibrillators? An in vivo investigation. J. Dent. 2013, 41, 955–959. [Google Scholar] [CrossRef] [PubMed]
- Bin-Shuwaish, M.S. Effects and Effectiveness of Cavity Disinfectants in Operative Dentistry: A Literature Review. J. Contemp. Dent. Pract. 2016, 17, 867–879. [Google Scholar] [CrossRef] [PubMed]
- Stübinger, S.; Sader, R.; Filippi, A. The use of ozone in dentistry and maxillofacial surgery: A review. Quintessence Int. 2006, 37, 353–359. [Google Scholar] [PubMed]
- Ahmedi, J.; Ahmedi, E.; Sejfija, O.; Agani, Z.; Hamiti, V. Efficiency of gaseous ozone in reducing the development of dry socket following surgical third molar extraction. Eur. J. Dent. 2016, 10, 381–385. [Google Scholar] [CrossRef]
- Boch, T.; Tennert, C.; Vach, K.; Al Ahmad, A.; Hellwig, E.; Polydorou, O. Effect of gaseous ozone on Enterococcus faecalis biofilm an in vitro study. Clin. Oral Investig. 2016, 20, 1733–1739. [Google Scholar] [CrossRef]
- Loncar, B.; Mravak Stipetic, M.; Matosevic, D.; Tarle, Z. Ozone application in dentistry. Arch. Med. Res. 2009, 40, 136–137. [Google Scholar] [CrossRef]
- Agapov, V.S.; Shulakov, V.V.; Fomchenkov, N.A. Ozone therapy of chronic mandibular osteomyelitis. Stomatologiia 2001, 80, 14–17. [Google Scholar]
- Moezizaden, M. Future of dentistry, nanodentistry, ozone therapy and tissue engineering. J. Dev. Biol. Tissue Eng. 2013, 5, 1–6. [Google Scholar]
- Meghan, K.; MacBarb, R.F.; Wong, M.E.; Athanasiou, K.A. Temporomandibular JoInt. Disorders: A Review of Etiology. Clinical Management and Tissue Engineering Strategies. J. Oral Maxillofac Implant. 2013, 28, 393–414. [Google Scholar]
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin AC, S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; Mendes de Souza, B.D. Prevalence of temporomandibular joInt. disorders: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef]
- Goncalves, D.A.; Fabbro, A.L.; Campos, J.A.; Bigal, M.E.; Speciali, J.G. Symptoms of temporomandibular disorders in the population: An epidemiological study. J. Orofac. Pain. 2010, 24, 270–278. [Google Scholar] [PubMed]
- Klasser, G.D.; Greene, C.S. Oral appliances in the management of temporomandibular disorders. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 212–223. [Google Scholar] [CrossRef] [PubMed]
- Daif, E.T. Role of intra-articular ozone gas injection in the management of internal derangement of the temporomandibular joint. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 113, e10–e14. [Google Scholar] [CrossRef]
- Bocci, V. Ozone as Janus: This controversial gas can be either toxic or medically useful. Mediat. Inflamm. 2004, 13, 3–11. [Google Scholar] [CrossRef]
- Larheim, T.A. Role of Magnetic Resonance Imaging in the Clinical Diagnosis of the Temporomandibular Joint. Cells Tissues Organs 2005, 180, 6–21. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barczyk, I.; Masłyk, D.; Walczuk, N.; Kijak, K.; Skomro, P.; Gronwald, H.; Pawlak, M.; Rusińska, A.; Sadowska, N.; Gronwald, B.; et al. Potential Clinical Applications of Ozone Therapy in Dental Specialties—A Literature Review, Supported by Own Observations. Int. J. Environ. Res. Public Health 2023, 20, 2048. https://doi.org/10.3390/ijerph20032048
Barczyk I, Masłyk D, Walczuk N, Kijak K, Skomro P, Gronwald H, Pawlak M, Rusińska A, Sadowska N, Gronwald B, et al. Potential Clinical Applications of Ozone Therapy in Dental Specialties—A Literature Review, Supported by Own Observations. International Journal of Environmental Research and Public Health. 2023; 20(3):2048. https://doi.org/10.3390/ijerph20032048
Chicago/Turabian StyleBarczyk, Izabela, Diana Masłyk, Natalia Walczuk, Karina Kijak, Piotr Skomro, Helena Gronwald, Maria Pawlak, Angelika Rusińska, Natalia Sadowska, Barbara Gronwald, and et al. 2023. "Potential Clinical Applications of Ozone Therapy in Dental Specialties—A Literature Review, Supported by Own Observations" International Journal of Environmental Research and Public Health 20, no. 3: 2048. https://doi.org/10.3390/ijerph20032048
APA StyleBarczyk, I., Masłyk, D., Walczuk, N., Kijak, K., Skomro, P., Gronwald, H., Pawlak, M., Rusińska, A., Sadowska, N., Gronwald, B., Garstka, A. A., & Lietz-Kijak, D. (2023). Potential Clinical Applications of Ozone Therapy in Dental Specialties—A Literature Review, Supported by Own Observations. International Journal of Environmental Research and Public Health, 20(3), 2048. https://doi.org/10.3390/ijerph20032048









