Effectiveness of Social Inclusion Interventions for Anxiety and Depression among Adolescents: A Systematic Review
Abstract
1. Introduction
- What types of interventions are being delivered to prevent or treat adolescent depression and/or anxiety by promoting social inclusion?
- How effective are these interventions?
- Are there specific groups of adolescents for whom these interventions are most effective?
- What are the mechanisms through which these interventions reduce adolescent depression and anxiety?
2. Materials and Methods
2.1. Eligibility Criteria
2.1.1. Population
2.1.2. Interventions
- Networking and social support, including linking people to appropriate support networks in the community, for example, non-governmental organisations and self-help groups.
- Improving community attitudes by working with the media to promote positive images and role models of marginalised groups and making information on services available.
- Social and communication skill training, including therapeutic approaches used to improve interpersonal relations.
- Access to, and participation in, cultural programmes, arts, drama and theatres.
- Access to the legal system and justice.
2.1.3. Control Groups
2.1.4. Types of Studies
2.1.5. Setting
2.1.6. Outcomes
2.1.7. Information Sources
2.1.8. Search Strategy
- MEDLINE(R);
- Embase Classic + Embase;
- PsycINFO;
- CAB Global Health;
- CINAHL;
- ERIC;
- CENTRAL;
- Scopus;
- Web of Science (Social Sciences Citation Index);
- WHO Global Health Index.
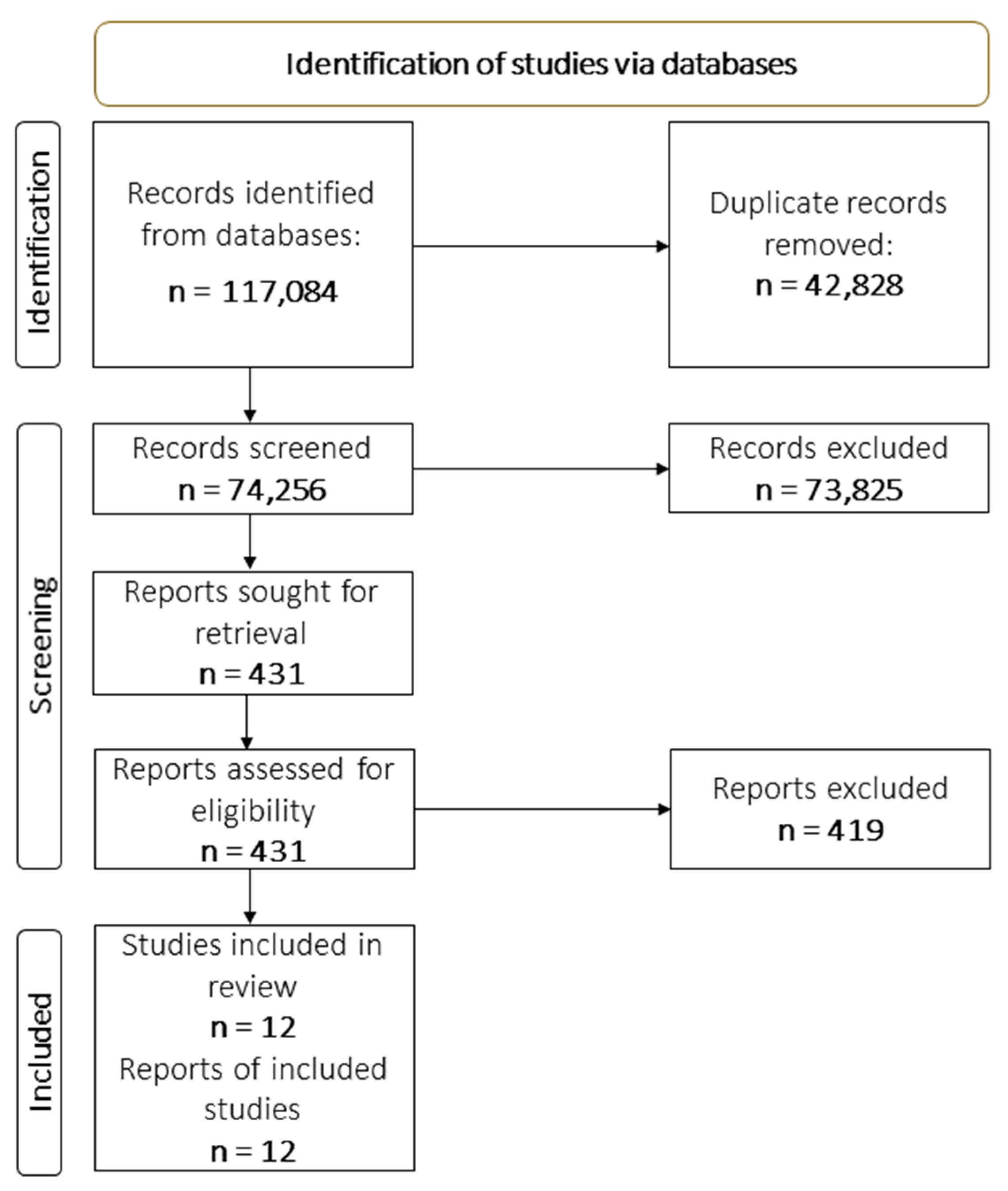
2.1.9. Selection Process
2.1.10. Data Collection Process and Data Items
2.1.11. Risk of Bias (Confidence in Study Findings) Assessment
- Study design (Potential confounders considered): impact evaluations need either a well-designed control group, preferably based on random assignment, or an estimation technique which controls for confounding and the associated possibility of selection bias.
- Masking (RCTs only, also known as blinding): masking helps limit the biases which can occur if study participants, data collectors or data analysts are aware of the assignment condition of individual participants.
- Loss to follow up: Attrition can be a major source of bias in studies, especially if these is differential attrition between the treatment and comparison group so that the two may no longer be balanced in pre-intervention characteristics. The US Institute of Education Sciences What Works Clearing House has developed standards for acceptable levels of attrition, in aggregate and the differential, which we applied.
- Clear definition of outcome measures: this is needed to aid interpretation and reliability of findings and comparability with other studies. Studies should clearly state the outcomes being used with a definition and the basis on which they are measured, preferably with reference to a widely used international standard.
- Baseline balance shows that the treatment and comparison groups are the same at baseline. Lack of balance can bias the results.
2.1.12. Effect Measures
2.1.13. Narrative Synthesis
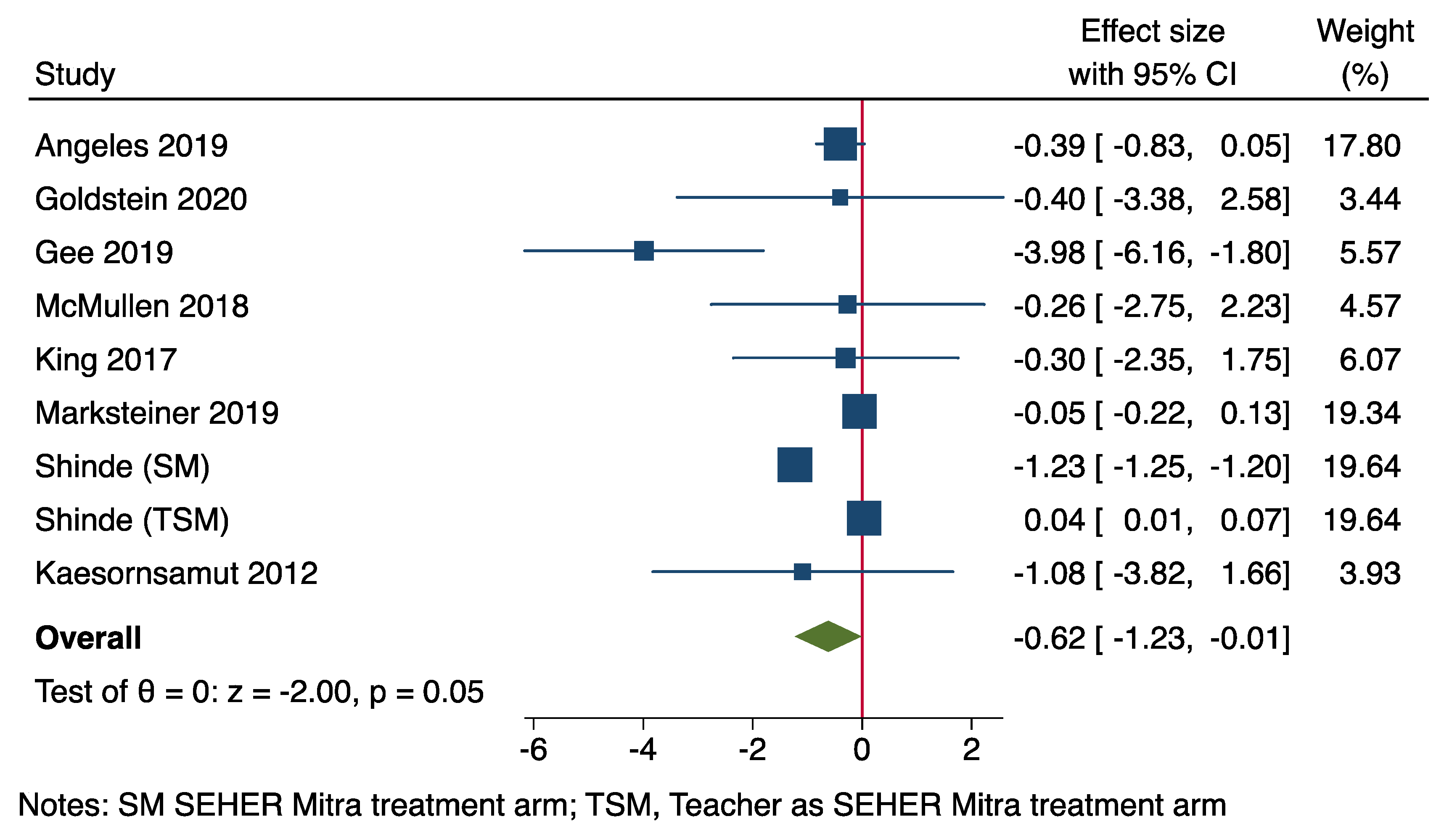
2.1.14. Forest Plot
3. Results
3.1. Risk of Bias (Confidence in Study Findings) Results
3.2. Forest Plot of Intervention Effects
3.3. Intervention Modalities and Mechanisms of Change
4. Discussion
5. Conclusions
Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Polanczyk, G.V.; Salum, G.A.; Sugaya, L.S.; Caye, A.; Rohde, L.A. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatry 2015, 56, 345–365. [Google Scholar] [CrossRef] [PubMed]
- Institute for Health Metrics and Evaluation. Global Health Data Exchange (GHDx). Available online: http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/d780dffbe8a381b25e1416884959e88b (accessed on 20 August 2022).
- Kessler, R.C.; Amminger, G.P.; Aguilar-Gaxiola, S.; Alonso, J.; Lee, S.; Ustun, T.B. Age of onset of mental disorders: A review of recent literature. Curr. Opin. Psychiatry 2007, 20, 359. [Google Scholar] [CrossRef] [PubMed]
- Lijster, J.M.d.; Dierckx, B.; Utens, E.M.; Verhulst, F.C.; Zieldorff, C.; Dieleman, G.C.; Legerstee, J.S. The age of onset of anxiety disorders: A meta-analysis. Can. J. Psychiatry 2017, 62, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Clayborne, Z.M.; Varin, M.; Colman, I. Systematic review and meta-analysis: Adolescent depression and long-term psychosocial outcomes. J. Am. Acad. Child Adolesc. Psychiatry 2019, 58, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Asselmann, E.; Wittchen, H.U.; Lieb, R.; Beesdo-Baum, K. Sociodemographic, clinical, and functional long-term outcomes in adolescents and young adults with mental disorders. Acta Psychiatr. Scand. 2018, 137, 6–17. [Google Scholar] [CrossRef]
- Johnson, D.; Dupuis, G.; Piche, J.; Clayborne, Z.; Colman, I. Adult mental health outcomes of adolescent depression: A systematic review. Depress. Anxiety 2018, 35, 700–716. [Google Scholar] [CrossRef]
- Naicker, K.; Galambos, N.L.; Zeng, Y.; Senthilselvan, A.; Colman, I. Social, demographic, and health outcomes in the 10 years following adolescent depression. J. Adolesc. Health 2013, 52, 533–538. [Google Scholar] [CrossRef]
- Orri, M.; Galera, C.; Turecki, G.; Forte, A.; Renaud, J.; Boivin, M.; Tremblay, R.E.; Côté, S.M.; Geoffroy, M.-C. Association of childhood irritability and depressive/anxious mood profiles with adolescent suicidal ideation and attempts. JAMA Psychiatry 2018, 75, 465–473. [Google Scholar] [CrossRef]
- Oud, M.; De Winter, L.; Vermeulen-Smit, E.; Bodden, D.; Nauta, M.; Stone, L.; Van Den Heuvel, M.; Al Taher, R.; De Graaf, I.; Kendall, T. Effectiveness of CBT for children and adolescents with depression: A systematic review and meta-regression analysis. Eur. Psychiatry 2019, 57, 33–45. [Google Scholar] [CrossRef]
- Rasing, S.; Creemers, D.H.; Janssens, J.M.; Scholte, R.H. Depression and anxiety prevention based on cognitive behavioral therapy for at-risk adolescents: A meta-analytic review. Front. Psychol. 2017, 8, 1066. [Google Scholar] [CrossRef]
- Sigurvinsdóttir, A.L.; Jensínudóttir, K.B.; Baldvinsdóttir, K.D.; Smárason, O.; Skarphedinsson, G. Effectiveness of cognitive behavioral therapy (CBT) for child and adolescent anxiety disorders across different CBT modalities and comparisons: A systematic review and meta-analysis. Nord. J. Psychiatry 2020, 74, 168–180. [Google Scholar] [CrossRef] [PubMed]
- Das, J.K.; Salam, R.A.; Lassi, Z.S.; Khan, M.N.; Mahmood, W.; Patel, V.; Bhutta, Z.A. Interventions for adolescent mental health: An overview of systematic reviews. J. Adolesc. Health 2016, 59, S49–S60. [Google Scholar] [CrossRef] [PubMed]
- Bennett, K.; Manassis, K.; Duda, S.; Bagnell, A.; Bernstein, G.A.; Garland, E.J.; Miller, L.D.; Newton, A.; Thabane, L.; Wilansky, P. Treating child and adolescent anxiety effectively: Overview of systematic reviews. Clin. Psychol. Rev. 2016, 50, 80–94. [Google Scholar] [CrossRef]
- Bennett, K.; Manassis, K.; Duda, S.; Bagnell, A.; Bernstein, G.A.; Garland, E.J.; Miller, L.D.; Newton, A.; Thabane, L.; Wilansky, P. Preventing child and adolescent anxiety disorders: Overview of systematic reviews. Depress. Anxiety 2015, 32, 909–918. [Google Scholar] [CrossRef] [PubMed]
- Keles, S.; Idsoe, T. A meta-analysis of group cognitive behavioral therapy (CBT) interventions for adolescents with depression. J. Adolesc. 2018, 67, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Strawn, J.R.; Welge, J.A.; Wehry, A.M.; Keeshin, B.; Rynn, M.A. Efficacy and tolerability of antidepressants in pediatric anxiety disorders: A systematic review and meta-analysis. Depress. Anxiety 2015, 32, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Cartwright-Hatton, S.; Roberts, C.; Chitsabesan, P.; Fothergill, C.; Harrington, R. Systematic review of the efficacy of cognitive behaviour therapies for childhood and adolescent anxiety disorders. Br. J. Clin. Psychol. 2004, 43, 421–436. [Google Scholar] [CrossRef]
- Allen, J.; Balfour, R.; Bell, R.; Marmot, M. Social determinants of mental health. Int. Rev. Psychiatry 2014, 26, 392–407. [Google Scholar] [CrossRef]
- Carod-Artal, F.J. Social determinants of mental health. In Global Mental Health; Springer: Cham, Switzerland, 2017; pp. 33–46. [Google Scholar]
- Lund, C.; Stansfeld, S.; De Silva, M. Social determinants of mental health. Glob. Ment. Health: Princ. Pract. 2014, 116–136. [Google Scholar]
- Vargas, S.M.; Huey Jr, S.J.; Miranda, J. A critical review of current evidence on multiple types of discrimination and mental health. Am. J. Orthopsychiatr. 2020, 90, 374. [Google Scholar] [CrossRef]
- Respress, B.N.; Morris, D.L.; Gary, F.A.; Lewin, L.C.; Francis, S.A. Social determinants of adolescent depression: An examination of racial differences. Issues Ment. Health Nurs. 2013, 34, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Butler, A.C. Poverty and adolescent depressive symptoms. Am. J. Orthopsychiatr. 2014, 84, 82. [Google Scholar] [CrossRef] [PubMed]
- Dashiff, C.; DiMicco, W.; Myers, B.; Sheppard, K. Poverty and adolescent mental health. J. Child Adolesc. Psychiatr. Nurs. 2009, 22, 23–32. [Google Scholar] [CrossRef]
- Elliott, K.J.; Stacciarini, J.-M.R.; Jimenez, I.A.; Rangel, A.P.; Fanfan, D. A Review of Psychosocial Protective and Risk Factors for the Mental Well-Being of Rural LGBTQ+ Adolescents. Youth Soc. 2021, 54, 312–341. [Google Scholar] [CrossRef]
- Sapiro, B.; Ward, A. Marginalized youth, mental health, and connection with others: A review of the literature. Child Adolesc. Soc. Work J. 2020, 37, 343–357. [Google Scholar] [CrossRef]
- Priest, N.; Kavanagh, A.; Bécares, L.; King, T. Cumulative effects of bullying and racial discrimination on adolescent health in Australia. J. Health Soc. Behav. 2019, 60, 344–361. [Google Scholar] [CrossRef] [PubMed]
- Rawal, N. Social inclusion and exclusion: A review. Dhaulagiri J. Sociol. Anthropol. 2008, 2, 161–180. [Google Scholar] [CrossRef]
- Department of Economic and Social Affairs of the United Nations. Leaving No One Behind: The Imperative of Inclusive Development; United Nations: New York, NY, USA, 2016; pp. 17–32. [Google Scholar]
- Byrne, D. Social Exclusion; McGraw-Hill Education: London, UK, 2005. [Google Scholar]
- Burchardt, T.; Le Grand, J.; Piachaud, D. Social exclusion in Britain 1991–1995. Soc. Policy Adm. 1999, 33, 227–244. [Google Scholar] [CrossRef]
- Rodgers, G.; Gore, C.; Figueiredo, J.B. Social Exclusion: Rhetoric, Reality, Responses; International Institute for Labour Studies: Geneva, Switzerland, 1995. [Google Scholar]
- O’Reilly, D. Social inclusion: A philosophical anthropology. Politics 2005, 25, 80–88. [Google Scholar] [CrossRef]
- Peace, R. Social exclusion: A concept in need of definition? Soc. Policy J. N. Z. 2001, 5, 17–36. [Google Scholar]
- Peace, R. Surface Tension: Place/Poverty/Policy—From “Poverty” to Social Exclusion: Implications of Discursive Shifts in European Union Poverty Policy 1975–1999. Ph.D. Thesis, University of Waikato, Hamilton, New Zealand, 1999. [Google Scholar]
- Percy-Smith, J. Policy Responses to Social Exclusion: Towards Inclusion? Mcgraw-Hill Education: London, UK, 2000. [Google Scholar]
- Labonté, R.; Hadi, A.; Kauffmann, X.E. Indicators of Social Exclusion and Inclusion: A Critical and Comparative Analysis of the Literature; É/Exchange Working Paper Series; Population Health Improvement Research Network: Toronto, ON, Canada, 2011; Volume 2, Issue 8. [Google Scholar]
- Filia, K.; Jackson, H.; Cotton, S.; Killackey, E. Understanding what it means to be socially included for people with a lived experience of mental illness. Int. J. Soc. Psychiatry 2019, 65, 413–424. [Google Scholar] [CrossRef] [PubMed]
- Gardner, A.; Filia, K.; Killackey, E.; Cotton, S. The social inclusion of young people with serious mental illness: A narrative review of the literature and suggested future directions. Aust. N. Z. J. Psychiatry 2019, 53, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Pascoe, E.A.; Smart Richman, L. Perceived discrimination and health: A meta-analytic review. Psychol. Bull. 2009, 135, 531. [Google Scholar] [CrossRef]
- Berry, C.; Hodgekins, J.; Michelson, D.; Chapman, L.; Chelidoni, O.; Crowter, L.; Sacadura, C.; Fowler, D. A systematic review and lived-experience panel analysis of hopefulness in youth depression treatment. Adolesc. Res. Rev. 2021, 7, 235–266. [Google Scholar] [CrossRef] [PubMed]
- Beames, J.R.; Kikas, K.; O’Gradey-Lee, M.; Gale, N.; Werner-Seidler, A.; Boydell, K.M.; Hudson, J.L. A new normal: Integrating lived experience into scientific data syntheses. Front. Psychiatry 2021, 12, 763005. [Google Scholar] [CrossRef] [PubMed]
- Hunt, X.; Abdurahman, H.; Omobowale, O.; Afolayan, A.; Munetsi, E.; Dzapasi, L.; Mokaya, N.; Koroma, A.; Barrie, I.; Ogunmola, O. Interventions for adolescents and adults with psychosis in Africa: A systematic review and narrative synthesis. Glob. Ment. Health 2022, 9, 223–240. [Google Scholar] [CrossRef] [PubMed]
- Saran, A.; Hunt, X.; White, H.; Kuper, H. PROTOCOL: Effectiveness of interventions for improving social inclusion outcomes for people with disabilities in low-and middle-income countries: A systematic review. Campbell Syst. Rev. 2021, 17, e1191. [Google Scholar] [CrossRef]
- Saran, A.; White, H.; Kuper, H. Evidence and gap map of studies assessing the effectiveness of interventions for people with disabilities in low-and middle-income countries. Campbell Syst. Rev. 2020, 16, e1070. [Google Scholar] [CrossRef]
- Riley, R.D.; Higgins, J.P.T.; Deeks, J.J. Interpretation of random effects meta-analyses. BMJ 2011, 342, d549. [Google Scholar] [CrossRef]
- Shinde, S.; Weiss, H.A.; Khandeparkar, P.; Pereira, B.; Sharma, A.; Gupta, R.; Ross, D.A.; Patton, G.; Patel, V. A multicomponent secondary school health promotion intervention and adolescent health: An extension of the SEHER cluster randomised controlled trial in Bihar, India. PLoS Med. 2020, 17, e1003021. [Google Scholar] [CrossRef]
- Angeles, G.; de Hoop, J.; Handa, S.; Kilburn, K.; Milazzo, A.; Peterman, A.; Malawi Social Cash Transfer Evaluation, T. Government of Malawi’s unconditional cash transfer improves youth mental health. Soc. Sci. Med. 2019, 225, 108–119. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, M.R.; Lewin, R.K.; Allen, J.J.B. Improvements in well-being and cardiac metrics of stress following a yogic breathing workshop: Randomized controlled trial with active comparison. J. Am. Coll. Health 2020, 70, 918–928. [Google Scholar] [CrossRef] [PubMed]
- Curtis, S.V.; Wodarski, J.S. The East Tennessee assertive adolescent family treatment program: A three-year evaluation. Soc. Work Public Health 2015, 30, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Gee, K.A.; Hawes, V.; Cox, N.A. Blue Notes: Using Songwriting to Improve Student Mental Health and Wellbeing. A Pilot Randomised Controlled Trial. Front. Psychol. 2019, 10, 423. [Google Scholar] [CrossRef]
- Hughes, S.; Rondeau, M.; Shannon, S.; Sharp, J.; Ivins, G.; Lee, J.; Taylor, I.; Bendixsen, B. A Holistic Self-learning Approach for Young Adult Depression and Anxiety Compared to Medication-Based Treatment-As-Usual. Community Ment. Health J. 2021, 57, 392–402. [Google Scholar] [CrossRef]
- McMullen, J.D.; McMullen, N. Evaluation of a teacher-led, life-skills intervention for secondary school students in Uganda. Soc. Sci. Med. 2018, 217, 10–17. [Google Scholar] [CrossRef]
- Travis, R.; Gann, E.; Crooke, A.H.; Jenkins, S.M. Hip Hop, empowerment, and therapeutic beat-making: Potential solutions for summer learning loss, depression, and anxiety in youth. J. Hum. Behav. Soc. Environ. 2019, 29, 744–765. [Google Scholar] [CrossRef]
- King, C.A.; Gipson, P.Y.; Arango, A.; Foster, C.E.; Clark, M.; Ghaziuddin, N.; Stone, D. LET’s CONNECT community mentorship program for youths with peer social problems: Preliminary findings from a randomized effectiveness trial. J. Community Psychol. 2018, 46, 885–902. [Google Scholar] [CrossRef]
- Marksteiner, T.; Janke, S.; Dickhäuser, O. Effects of a brief psychological intervention on students’ sense of belonging and educational outcomes: The role of students’ migration and educational background. J. Sch. Psychol. 2019, 75, 41–57. [Google Scholar] [CrossRef]
- Kaesornsamut, P.; Sitthimongkol, Y.; Williams, R.A.; Sangon, S.; Rohitsuk, W.; Vorapongsathorn, T. Effectiveness of the BAND intervention program on Thai adolescents’ sense of belonging, negative thinking and depressive symptoms. Pac. Rim Int. J. Nurs. Res. 2012, 16, 29–47. [Google Scholar]
- Hill, T.L.; Gray, S.A.O.; Baker, C.N.; Boggs, K.; Carey, E.; Johnson, C.; Kamps, J.L.; Varela, R.E. A Pilot Study Examining the Effectiveness of the PEERS Program on Social Skills and Anxiety in Adolescents with Autism Spectrum Disorder. J. Dev. Phys. Disabil. 2017, 29, 797–808. [Google Scholar] [CrossRef] [PubMed]
- Gohar, S.M.; Hamdi, E.; Lamis, A.; Horan, W.P.; Green, M.F. Adapting and evaluating a social cognitive remediation program for schizophrenia in Arabic. Schizophr. Res. 2013, 148, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Rami, H.; Hussien, H.; Rabie, M.; Sabry, W.; Missiry, M.E.; Ghamry, R.E. Evaluating the effectiveness of a culturally adapted behavioral family psycho-educational program for Egyptian patients with schizophrenia. Transcult. Psychiatry 2018, 55, 601–622. [Google Scholar] [CrossRef] [PubMed]
- Gureje, O.; Appiah-Poku, J.; Bello, T.; Kola, L.; Araya, R.; Chisholm, D.; Esan, O.; Harris, B.; Makanjuola, V.; Othieno, C. Effect of collaborative care between traditional and faith healers and primary health-care workers on psychosis outcomes in Nigeria and Ghana (COSIMPO): A cluster randomised controlled trial. Lancet 2020, 396, 612–622. [Google Scholar] [CrossRef] [PubMed]
- Thomas, I.F.; Lawani, A.O.; James, B.O. Effect of Short Message Service Reminders on Clinic Attendance Among Outpatients with Psychosis at a Psychiatric Hospital in Nigeria. Psychiatr. Serv. 2017, 68, 75–80. [Google Scholar] [CrossRef]
- Engelbrecht, R.; Plastow, N.; Botha, U.; Niehaus, D.; Koen, L. The effect of an occupational therapy mental health day treatment centre on the use of inpatient services in the Western Cape, South Africa. Disabil. Rehabil. 2019, 41, 1974–1980. [Google Scholar] [CrossRef]
- Botha, U.A.; Koen, L.; Joska, J.A.; Hering, L.M.; Oosthuizen, P.P. Assessing the efficacy of a modified assertive community-based treatment programme in a developing country. BMC Psychiatry 2010, 10, 73. [Google Scholar] [CrossRef]
- De Menil, V.; Knapp, M.; McDaid, D.; Raja, S.; Kingori, J.; Waruguru, M.; Wood, S.; Mannarath, S.; Lund, C. Cost-effectiveness of the Mental Health and Development model for schizophrenia-spectrum and bipolar disorders in rural Kenya. Psychol. Med. 2015, 45, 2747–2756. [Google Scholar] [CrossRef]
- Sorketti, E.A.; Zainal, N.Z.; Habil, M.H. The treatment outcome of psychotic disorders by traditional healers in central Sudan. Int. J. Soc. Psychiatry 2013, 59, 365–376. [Google Scholar] [CrossRef]
- Brooke-Sumner, C.; Selohilwe, O.; Mazibuko, M.S.; Petersen, I. Process evaluation of a pilot intervention for psychosocial rehabilitation for service users with schizophrenia in North West Province, South Africa. Community Ment. Health J. 2018, 54, 1089–1096. [Google Scholar] [CrossRef]
- Sibeko, G.; Temmingh, H.; Mall, S.; Williams-Ashman, P.; Thornicroft, G.; Susser, E.S.; Lund, C.; Stein, D.J.; Milligan, P.D. Improving adherence in mental health service users with severe mental illness in South Africa: A pilot randomized controlled trial of a treatment partner and text message intervention vs. treatment as usual. BMC Res. Notes 2017, 10, 584. [Google Scholar] [CrossRef] [PubMed]
- Asher, L.; Hanlon, C.; Birhane, R.; Habtamu, A.; Eaton, J.; Weiss, H.A.; Patel, V.; Fekadu, A.; De Silva, M. Community-based rehabilitation intervention for people with schizophrenia in Ethiopia (RISE): A 12 month mixed methods pilot study. BMC Psychiatry 2018, 18, 250. [Google Scholar] [CrossRef] [PubMed]
- Hanlon, C.; Medhin, G.; Selamu, M.; Birhane, R.; Dewey, M.; Tirfessa, K.; Garman, E.; Asher, L.; Thornicroft, G.; Patel, V. Impact of integrated district level mental health care on clinical and social outcomes of people with severe mental illness in rural Ethiopia: An intervention cohort study. Epidemiol. Psychiatr. Sci. 2020, 29, E45. [Google Scholar] [CrossRef] [PubMed]
| Angeles 2019 [49] | Goldstein 2020 [50] | Curtis 2018 [51] | Gee 2019 [52] | Hughes 2021 [53] | McMullen 2018 [54] | Travis 2019 [55] | King 2017 [56] | Marksteiner 2019 [57] | Shinde 2020 [48] | Kaesornsamut 2012 [58] | Hill 2017 [59] | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size | 2099 | 69 | 107 | 13 | 39 | 170 | 35 | 218 | 106 | 7824 | 60 | 5 | |
| Level | Universal | x | x | x | x | x | |||||||
| Targeted | x | x | x | ||||||||||
| Indicated | x | x | x | x | |||||||||
| Age Range | 13–19 years | 18–35 years | 12–17 years | 18–31 years | 18–25 years | 13–18 years | 11–15 years | 12–15 years | 19.8 years * | 13–15 years | 16–18 years | 13–15 years | |
| Gender | Female Only | x | |||||||||||
| Male and Female | x | x | x | x | x | x | x | x | x | x | x | ||
| Country | Malawi | USA | USA | UK | USA | Uganda | Australia | USA | Germany | India | Thailand | USA | |
| Outcome | Depression | x | x | x | x | x | x | x | x | x | x | x | |
| Anxiety | x | x | x | x | x | x | x |
| Angeles 2019 [49] | Goldstein 2020 [50] | Curtis 2018 [51] | Gee 2019 [52] | Hughes 2021 [53] | McMullen 2018 [54] | Travis 2019 [55] | King 2017 [56] | Marksteiner 2019 [57] | Shinde 2020 [48] | Kaesornsamut 2012 [58] | Hill 2017 [59] | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study Design | Low | x | x | x | x | ||||||||
| Medium | x | ||||||||||||
| High | x | x | x | x | x | x | x | ||||||
| Loss to Follow Up | Low | x | x | x | x | ||||||||
| Medium | x | x | x | x | |||||||||
| High | x | x | x | x | |||||||||
| Masking | Low | x | x | N/A | x | N/A | N/A | N/A | x | x | N/A | N/A | |
| Medium | |||||||||||||
| High | x | ||||||||||||
| MH Outcome Measure | Low | ||||||||||||
| Medium | x | ||||||||||||
| High | x | x | x | x | x | x | x | x | x | x | |||
| Baseline Balance | Low | N/A | x | x | N/A | ||||||||
| Medium | x | x | x | ||||||||||
| High | x | x | x | x | x | ||||||||
| Overall score | Low | x | x | x | x | x | x | x | x | x | x | x | |
| Medium | |||||||||||||
| High | x |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hunt, X.; Shakespeare, T.; Vilyte, G.; Melendez-Torres, G.J.; Henry, J.; Bradshaw, M.; Naidoo, S.; Mbuyamba, R.; Aljassem, S.; Suubi, E.; et al. Effectiveness of Social Inclusion Interventions for Anxiety and Depression among Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 1895. https://doi.org/10.3390/ijerph20031895
Hunt X, Shakespeare T, Vilyte G, Melendez-Torres GJ, Henry J, Bradshaw M, Naidoo S, Mbuyamba R, Aljassem S, Suubi E, et al. Effectiveness of Social Inclusion Interventions for Anxiety and Depression among Adolescents: A Systematic Review. International Journal of Environmental Research and Public Health. 2023; 20(3):1895. https://doi.org/10.3390/ijerph20031895
Chicago/Turabian StyleHunt, Xanthe, Tom Shakespeare, Gabriele Vilyte, G. J. Melendez-Torres, Junita Henry, Melissa Bradshaw, Selvan Naidoo, Rachel Mbuyamba, Shahd Aljassem, Esta Suubi, and et al. 2023. "Effectiveness of Social Inclusion Interventions for Anxiety and Depression among Adolescents: A Systematic Review" International Journal of Environmental Research and Public Health 20, no. 3: 1895. https://doi.org/10.3390/ijerph20031895
APA StyleHunt, X., Shakespeare, T., Vilyte, G., Melendez-Torres, G. J., Henry, J., Bradshaw, M., Naidoo, S., Mbuyamba, R., Aljassem, S., Suubi, E., Aljasem, N., Makhetha, M., & Bantjes, J. (2023). Effectiveness of Social Inclusion Interventions for Anxiety and Depression among Adolescents: A Systematic Review. International Journal of Environmental Research and Public Health, 20(3), 1895. https://doi.org/10.3390/ijerph20031895





