The Impact of the COVID-19 Pandemic and Lockdowns on Self-Poisoning and Suicide in Sri Lanka: An Interrupted Time Series Analysis
Abstract
1. Background
2. Methods
2.1. Setting
2.2. Self-Poisoning Hospital Data
2.3. Suicide Data
2.4. Data Management
2.5. Self-Poisoning Hospital Data
2.6. Suicide Data
2.7. Statistical Analyses
2.8. Ethical Approval
3. Results
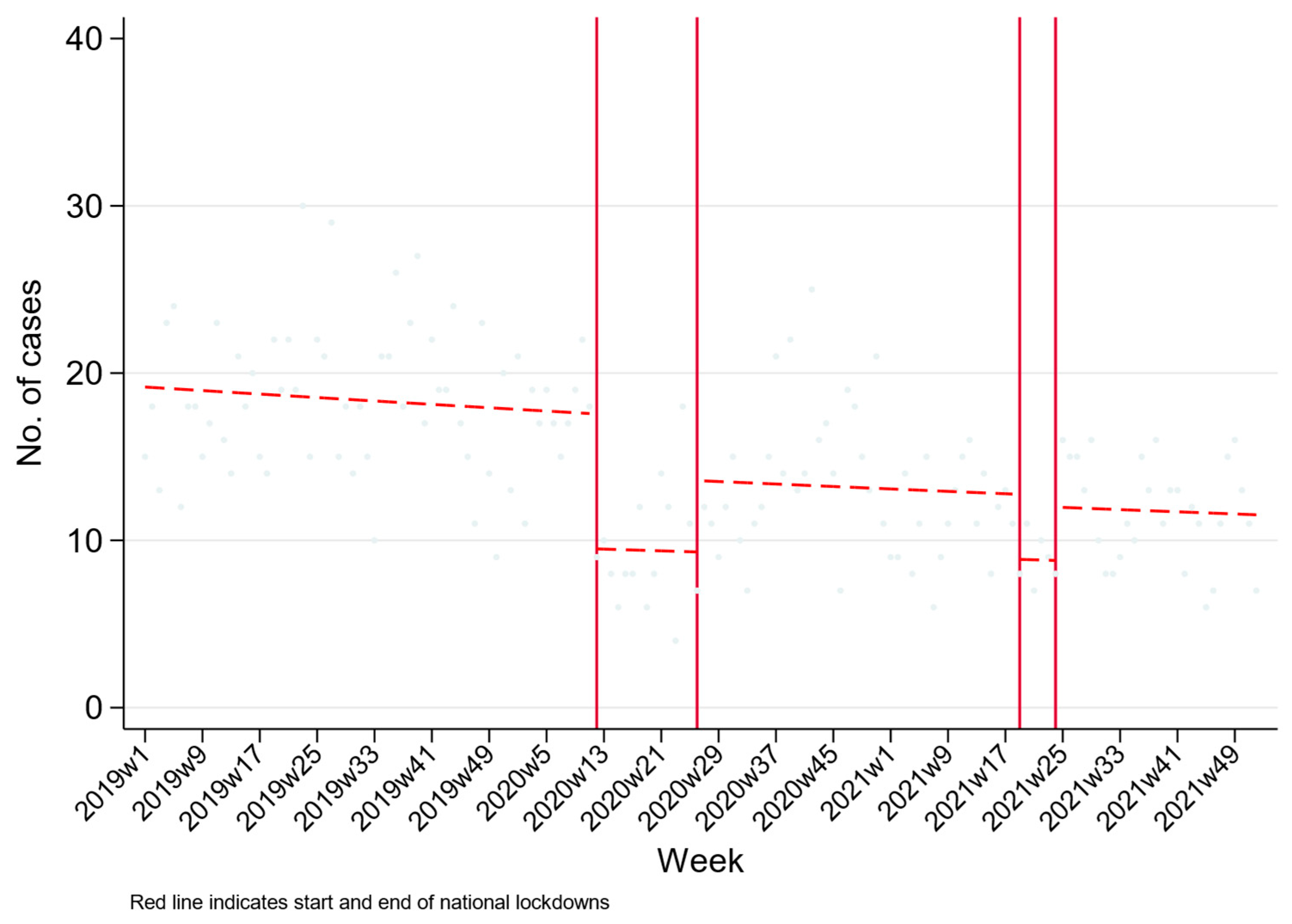
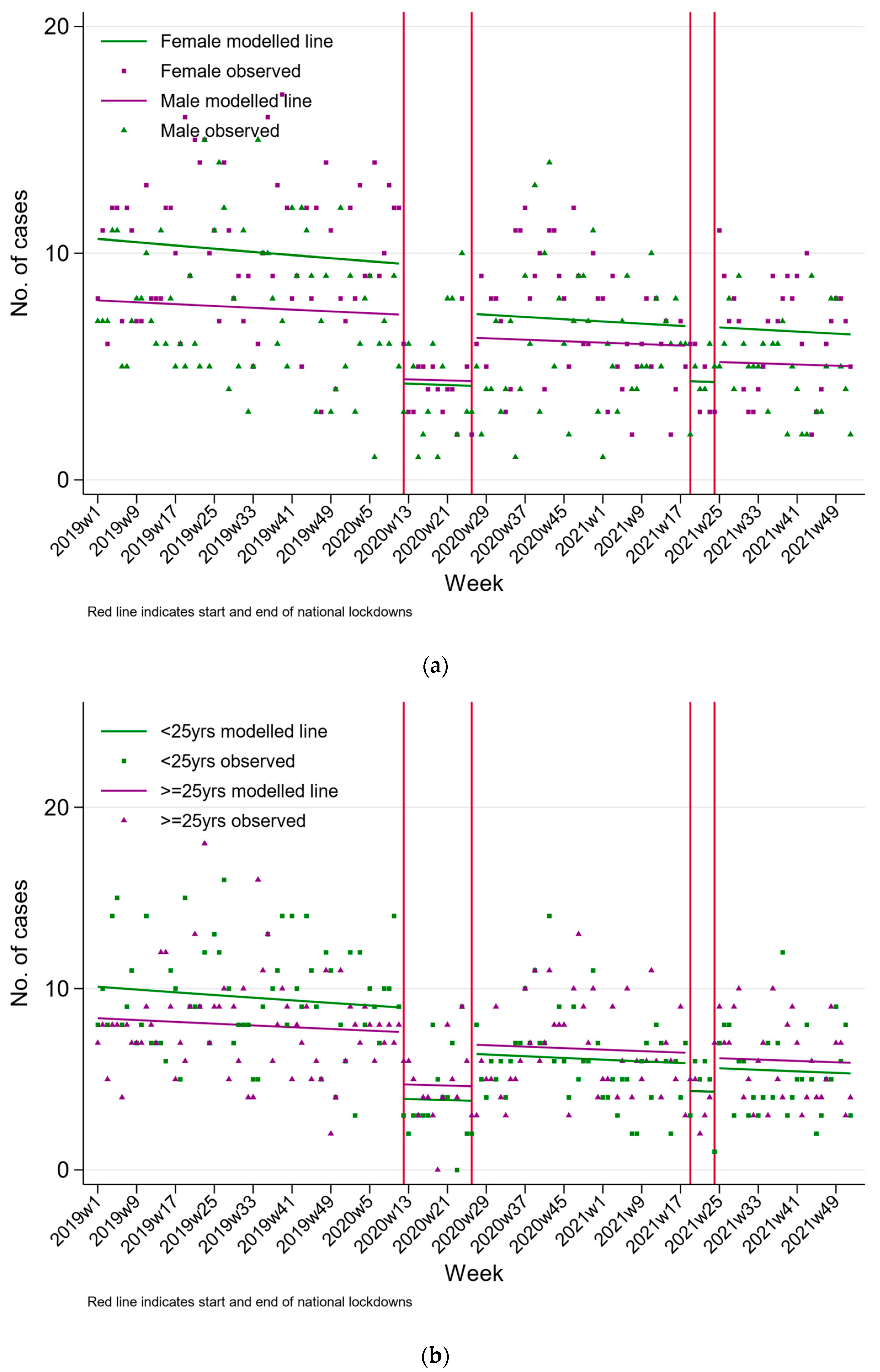
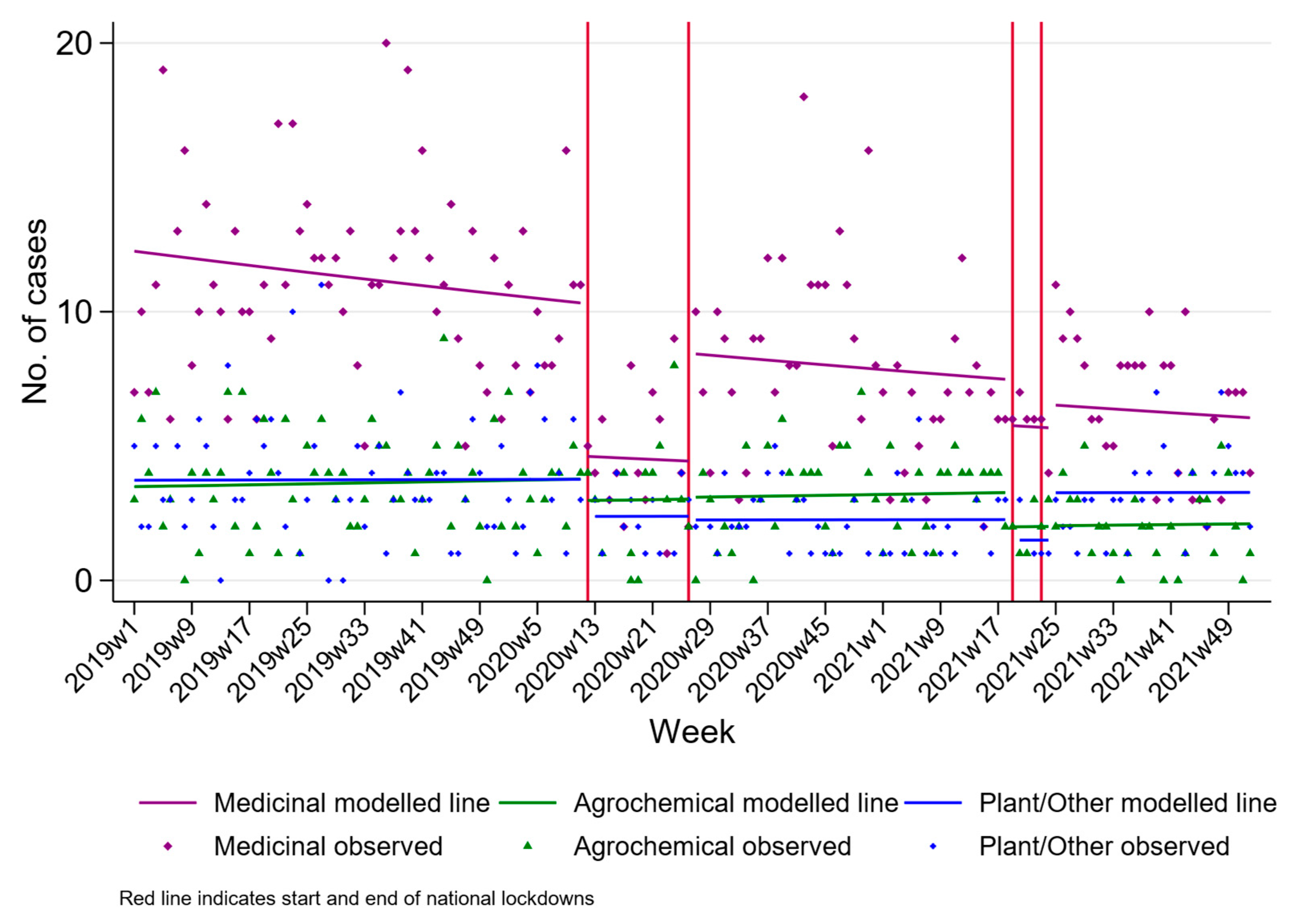
3.1. Hospital Admissions Due to Self-Poisoning, Peradeniya
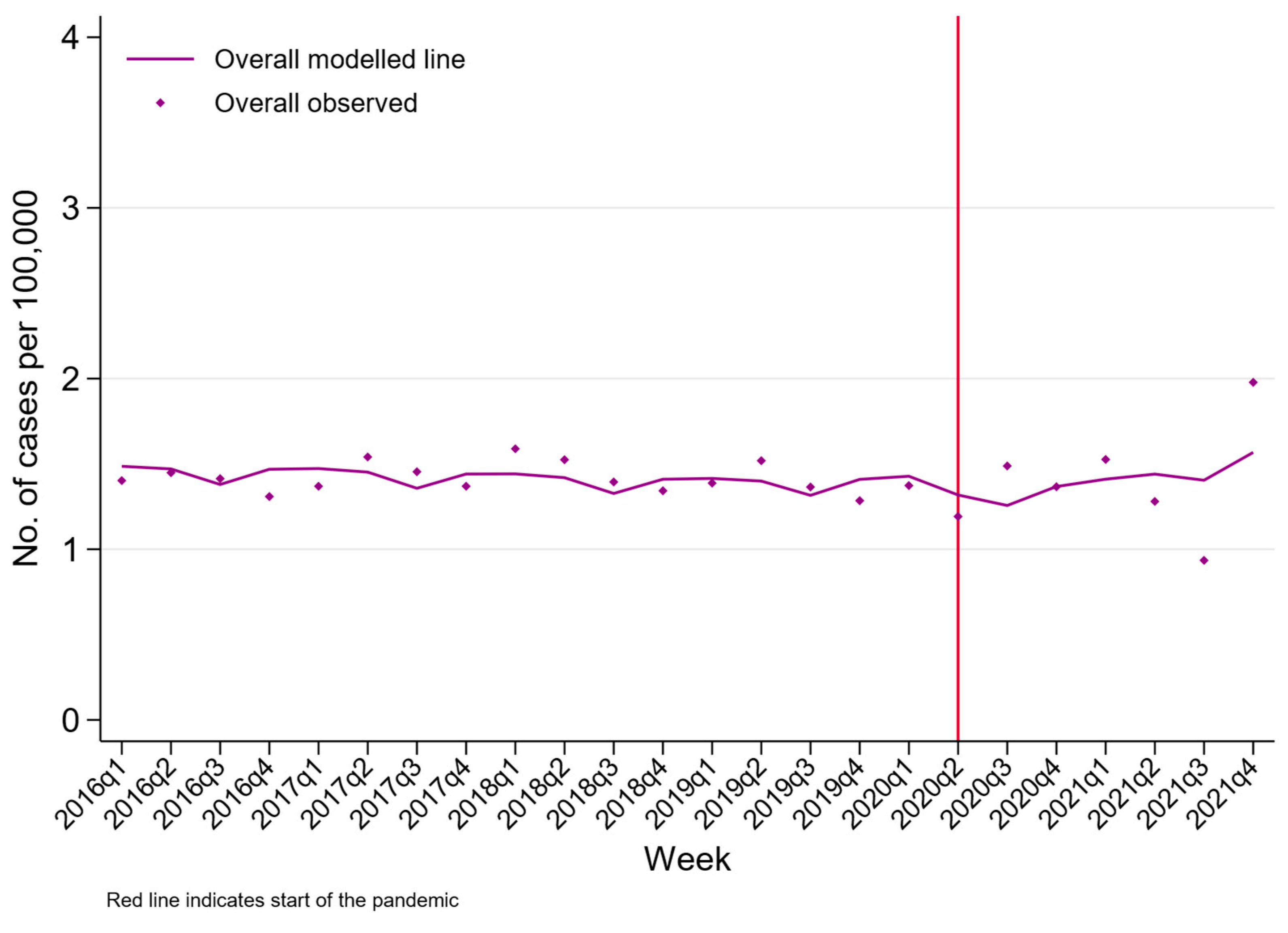
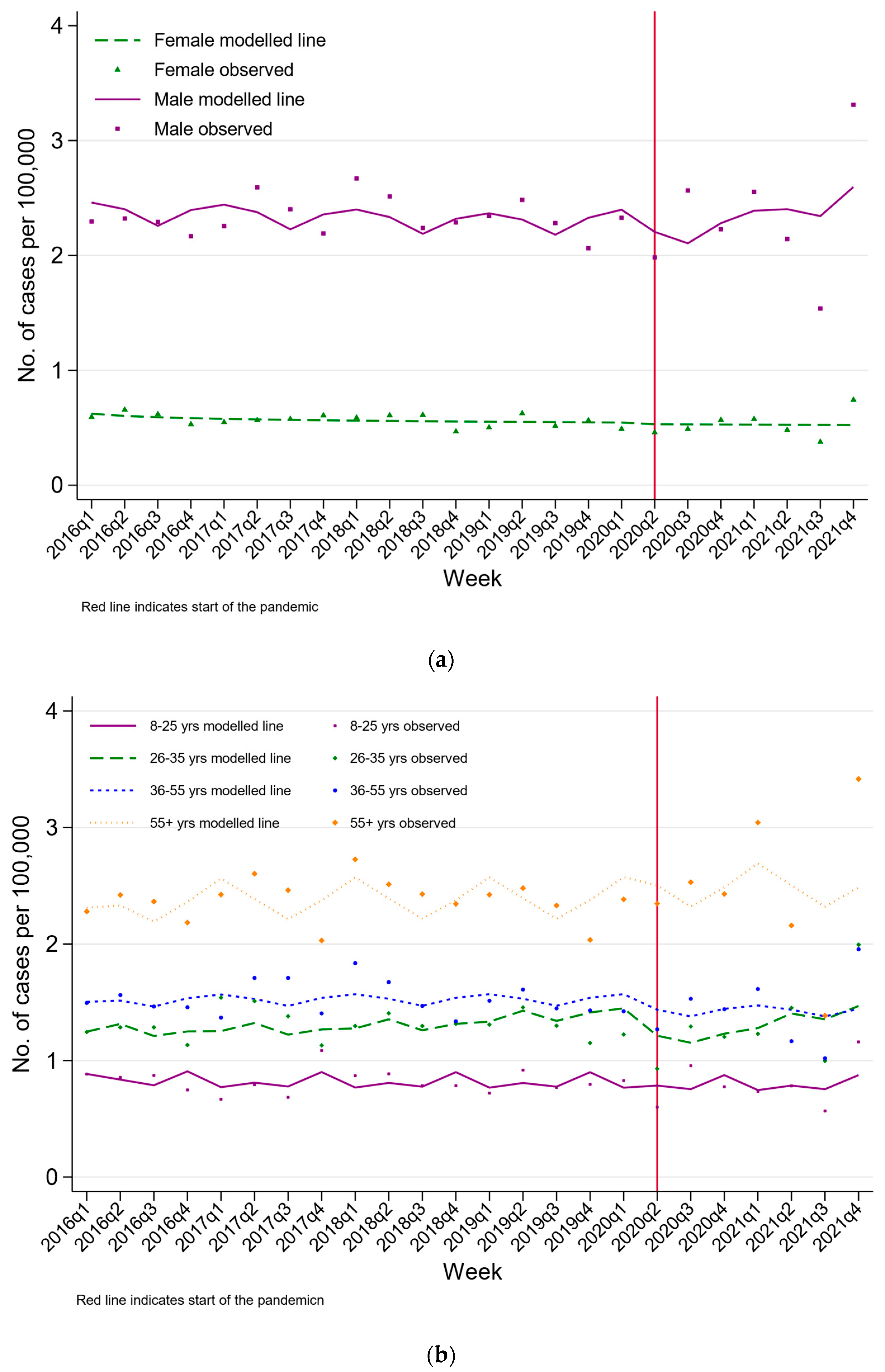
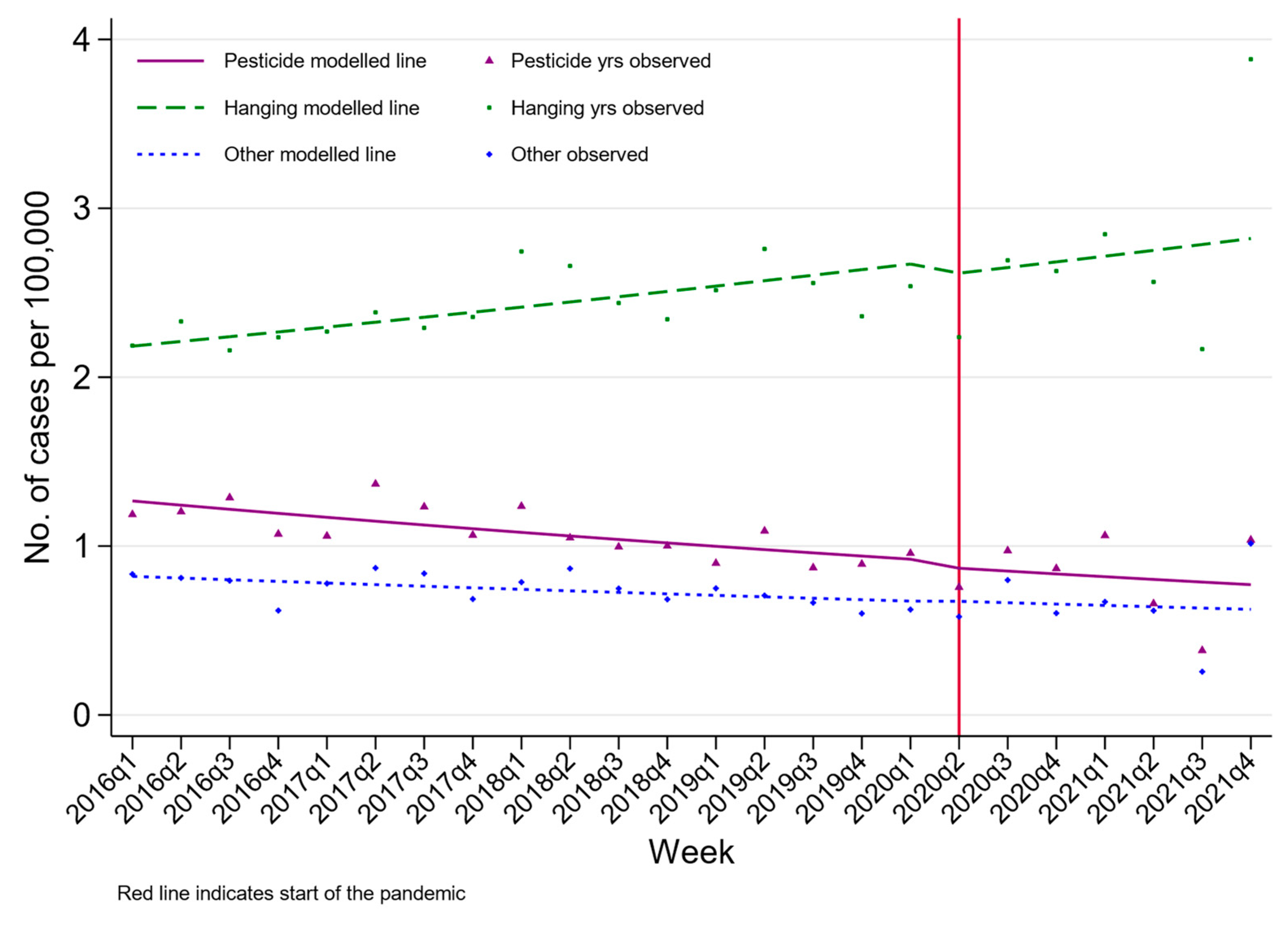
3.2. Suicide Numbers, Nationwide
4. Discussion
4.1. Hospital Presenting Self-Poisoning
4.2. Suicide
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Rothman, S.; Sher, L. Suicide prevention in the covid-19 era. Prev. Med. 2021, 152, 106547. [Google Scholar] [CrossRef]
- Elbogen, E.B.; Lanier, M.; Blakey, S.M.; Wagner, H.R.; Tsai, J. Suicidal ideation and thoughts of self-harm during the COVID-19 pandemic: The role of COVID-19-related stress, social isolation, and financial strain. Depress. Anxiety 2021, 38, 739–748. [Google Scholar] [CrossRef]
- Pirkis, J.; John, A.; Shin, S.; DelPozo-Banos, M.; Arya, V.; Analuisa-Aguilar, P.; Appleby, L.; Arensman, E.; Bantjes, J.; Baran, A.; et al. Suicide trends in the early months of the COVID-19 pandemic: An interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry 2021, 8, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Liem, A.; Prawira, B.; Magdalena, S.; Siandita, M.J.; Hudiyana, J. Predicting self-harm and suicide ideation during the COVID-19 pandemic in Indonesia: A nationwide survey report. BMC Psychiatry 2022, 22, 304. [Google Scholar] [CrossRef] [PubMed]
- Salman, M.; Shehzadi, N.; Mustafa, Z.U.; Mallhi, T.H.; Khan, Y.H.; Khan, T.M.; Hussain, K. Self-harm and suicidal ideation in Pakistani youth amid COVID-19 pandemic: Findings of a large, cross-sectional study. Psychol. Health Med. 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Knipe, D.; John, A.; Padmanathan, P.; Eyles, E.; Dekel, D.; Higgins, J.P.T.; Bantjes, J.; Dandona, R.; Macleod-Hall, C.; McGuinness, L.A.; et al. Suicide and self-harm in low- and middle- income countries during the COVID-19 pandemic: A systematic review. PLOS Glob. Public Health 2022, 2, e0000282. [Google Scholar] [CrossRef]
- Knipe, D.; Silva, T.; Aroos, A.; Senarathna, L.; Hettiarachchi, N.M.; Galappaththi, S.R.; Spittal, M.J.; Gunnell, D.; Metcalfe, C.; Rajapakse, T. Hospital presentations for self-poisoning during COVID-19 in Sri Lanka: An interrupted time-series analysis. Lancet Psychiatry 2021, 8, 892–900. [Google Scholar] [CrossRef] [PubMed]
- Steeg, S.; John, A.; Gunnell, D.J.; Kapur, N.; Dekel, D.; Schmidt, L.; Knipe, D.; Arensman, E.; Hawton, K.; Higgins, J.P.T.; et al. The impact of the COVID-19 pandemic on presentations to health services following self-harm: Systematic review. Br. J. Psychiatry 2022, 221, 603–612. [Google Scholar] [CrossRef] [PubMed]
- Gunnell, D.; Fernando, R.; Hewagama, M.; Priyangika, W.D.D.; Konradsen, F.; Eddleston, M. The impact of pesticide regulations on suicide in Sri Lanka. Int. J. Epidemiol. 2007, 36, 1235–1242. [Google Scholar] [CrossRef]
- Knipe, D.W.; Gunnell, D.; Eddleston, M. Preventing deaths from pesticide self-poisoning: Learning from Sri Lanka’s success. Lancet Glob. Health 2017, 5, e651–e652. [Google Scholar] [CrossRef]
- Knipe, D.W.; Metcalfe, C.; Fernando, R.; Pearson, M.; Konradsen, F.; Eddleston, M.; Gunnell, D. Suicide in Sri Lanka 1975-2012: Age, period and cohort analysis of police and hospital data. BMC Public Health 2014, 14, 839. [Google Scholar] [CrossRef] [PubMed]
- Hanwella, R.; Senanayake, S.M.; De Silva, V. Geographical variation in admissions due to poisoning in Sri Lanka: A time series analysis. Ceylon Med. J. 2012, 57, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Amnesty International UK. Sri Lanka: Economic Crisis Has Had ‘Devastating Consequences’ on Healthcare and Food Supplies—New Report. Available online: https://www.amnesty.org.uk/press-releases/sri-lanka-economic-crisis-has-had-devastating-consequences-healthcare-and-food#:~:text=Root%20of%20the%20economic%20crisis,from%20overseas%20workers%20also%20dropped (accessed on 14 December 2022).
- World Bank. The World Bank In Sri Lanka. Available online: https://www.worldbank.org/en/country/srilanka/overview (accessed on 14 December 2022).
- Boafo, G.; Spooner, M. Ghana’s Economic Crisis: Expert Insights into How Things Got So Bad—And What the Fixes Are. Available online: https://theconversation.com/ghanas-economic-crisis-expert-insights-into-how-things-got-so-bad-and-what-the-fixes-are-193153 (accessed on 14 December 2022).
- Knipe, D.; Rajapakse, T. Self-Poisoning and Suicide in Sri Lanka—COVID19 (Analysis Plan); Center for Open Science: Charlottesville, VA, USA, 2021. [Google Scholar] [CrossRef]
- Bernal, J.L.; Cummins, S.; Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Int. J. Epidemiol. 2017, 46, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Rajapakse, T.; Christensen, H.; Cotton, S.; Griffiths, K.M. Non-fatal self-poisoning across age groups, in Sri Lanka. Asian J. Psychiatry 2016, 19, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Fernando, K.; Jayamanna, S.; Weerasinghe, M.; Priyadarshana, C.; Ratnayake, R.; Pearson, M.; Gunnell, D.; Dawson, A.; Hawton, K.; Konradsen, F.; et al. Risk factors for deliberate self-harm in young people in rural Sri Lanka: A prospective cohort study of 22,000 individuals. Ceylon Med. J. 2021, 66, 87–95. [Google Scholar] [CrossRef]
- Haw, C.; Hawton, K. Life problems and deliberate self-harm: Associations with gender, age, suicidal intent and psychiatric and personality disorder. J. Affect. Disord. 2008, 109, 139–148. [Google Scholar] [CrossRef]
- Pirkis, J.; Gunnell, D.; Shin, S.; Del Pozo-Banos, M.; Arya, V.; Aguilar, P.A.; Appleby, L.; Arafat, S.M.Y.; Arensman, E.; Ayuso-Mateos, J.L.; et al. Suicide numbers during the first 9-15 months of the COVID-19 pandemic compared with pre-existing trends: An interrupted time series analysis in 33 countries. eClinicalMedicine 2022, 51, 101573. [Google Scholar] [CrossRef]
- Moscicki, E.K. Epidemiology of completed and attempted suicide: Toward a framework for prevention. Clin. Neurosci. Res. 2001, 1, 310–323. [Google Scholar] [CrossRef]
- Abeyasinghe, R.; Gunnell, D. Psychological autopsy study of suicide in three rural and semi-rural districts of Sri Lanka. Soc. Psychiatr Psychiatr Epidemiol. 2008, 43, 280–285. [Google Scholar] [CrossRef]
- Centre for Pesticide Suicide Prevention. Why Sri Lanka’s Current Crisis Shouldn’t Overshadow Its Success in Suicide Prevention. 2022, Volume 2023. Available online: https://centrepsp.org/media/blog/why-sri-lankas-current-crisis-shouldnt-overshadow-its-success-in-suicide-prevention/ (accessed on 14 December 2022).
- Ajdacic-Gross, V.; Weiss, M.G.; Ring, M.; Hepp, U.; Bopp, M.; Gutzwiller, F.; Rössler, W. Methods of suicide: International suicide patterns derived from the WHO mortality database. Bull. World Health Organ. 2008, 86, 726–732. [Google Scholar] [CrossRef]
- Milner, A.; Page, A.; LaMontagne, A.D. Long-term unemployment and suicide: A systematic review and meta-analysis. PLoS ONE 2013, 8, e51333. [Google Scholar] [CrossRef] [PubMed]
- Oyesanya, M.; Lopez-Morinigo, J.; Dutta, R. Systematic review of suicide in economic recession. World Psychiatry 2015, 5, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Frasquilho, D.; Matos, M.G.; Salonna, F.; Guerreiro, D.; Storti, C.C.; Gaspar, T.; Caldas-de-Almeida, J.M. Mental health outcomes in times of economic recession: A systematic literature review. BMC Public Health 2016, 16, 115. [Google Scholar] [CrossRef]
- Kerr, W.C.; Kaplan, M.S.; Huguet, N.; Caetano, R.; Giesbrecht, N.; McFarland, B.H. Economic Recession, Alcohol, and Suicide Rates: Comparative Effects of Poverty, Foreclosure, and Job Loss. Am. J. Prev. Med. 2017, 52, 469–475. [Google Scholar] [CrossRef]
- Haw, C.; Hawton, K.; Gunnell, D.; Platt, S. Economic recession and suicidal behaviour: Possible mechanisms and ameliorating factors. Int. J. Soc. Psychiatry 2015, 61, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Menon, V.; Cherian, A.V.; Vijayakumar, L. Rising incidence and changing demographics of suicide in India: Time to recalibrate prevention policies? Asian J. Psychiatr. 2021, 25, 102983. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Lee, Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry 2020, 19, 250–251. [Google Scholar] [CrossRef]
| Pandemic Lockdown Period * n (%) | |||||
|---|---|---|---|---|---|
| Pre- | During 1st | Post-1st | During 2nd | Post-2nd | |
| Number of presentations | 1157 | 141 | 579 | 53 | 329 |
| Mean number of presentations/week | 18 | 9 | 13 | 9 | 12 |
| Patients with BHT data, n (%) | 1115 (96.4) | 131 (92.9) | 576 (99.5) | 53 (100) | 323 (98.2) |
| Age in years–Median (IQI) | 23 (18, 34) | 26 (19, 39) | 26 (19, 38) | 24 (19, 31) | 25 (19, 38) |
| Sex | |||||
| Male | 479 (41.4) | 66 (46.8) | 268 (46.3) | 26 (49.1) | 143 (43.5) |
| Female | 635 (54.9) | 63 (44.7) | 310 (53.5) | 26 (49.1) | 184 (55.9) |
| Missing | 43 (3.7) | 12 (8.5) | 1 (0.2) | 1 (1.9) | 2 (0.6) |
| Time of attendance | |||||
| 00:00–07:59 | 130 (11.2) | 11 (7.8) | 62 (10.7) | 2 (3.8) | 28 (8.5) |
| 08:00–15:59 | 354 (30.6) | 55 (39.0) | 227 (39.2) | 22 (41.5) | 140 (42.6) |
| 16:00–23:59 | 628 (54.3) | 64 (45.4) | 285 (49.2) | 28 (52.8) | 158 (48) |
| Missing | 45 (3.9) | 11 (7.8) | 5 (0.9) | 1 (1.9) | 3 (0.9) |
| Psychiatric assessment conducted | |||||
| Yes | 1035 (89.5) | 125 (88.7) | 546 (94.3) | 52 (98.1) | 304 (92.4) |
| No | 56 (4.8) | 6 (4.3) | 25 (4.3) | 0 (0) | 22 (6.7) |
| Unknown | 66 (5.7) | 10 (7.1) | 8 (1.4) | 1 (1.9) | 3 (0.9) |
| Assessment performed by | |||||
| No assessment | 56 (4.8) | 6 (4.3) | 52 (9.0) | 3 (5.7) | 23 (7.0) |
| Consultant | 42 (3.6) | 11 (7.8) | 58 (10.0) | 2 (3.8) | 7 (2.1) |
| Registrar | 403 (34.8) | 57 (40.4) | 302 (52.2) | 34 (64.2) | 165 (50.2) |
| Senior registrar | 60 (5.2) | 12 (8.5) | 9 (1.6) | 0 (0) | 2 (0.6) |
| Medical Officer | 501 (43.3) | 45 (31.9) | 148 (25.6) | 11 (20.8) | 123 (37.4) |
| Unknown | 95 (8.2) | 10 (7.1) | 10 (1.7) | 3 (5.7) | 9 (2.7) |
| Current psychiatric diagnosis | |||||
| Yes | 533 (46.1) | 69 (48.9) | 201 (34.7) | 18 (34) | 119 (36.2) |
| No | 480 (41.5) | 53 (37.6) | 274 (47.3) | 29 (54.7) | 155 (47.1) |
| Unknown | 144 (12.4) | 19 (13.5) | 104 (18.0) | 6 (11.3) | 55 (16.7) |
| Method | |||||
| Medicine | 696 (60.2) | 68 (48.2) | 351 (60.6) | 35 (66) | 186 (56.5) |
| Agrochemical/pesticide/insecticide | 225 (19.4) | 42 (29.8) | 140 (24.2) | 12 (22.6) | 58 (17.6) |
| Plant/other | 194 (16.8) | 21 (14.9) | 86 (14.9) | 6 (11.3) | 84 (25.5) |
| Missing | 42 (3.6) | 10 (7.1) | 2 (0.3) | 0 (0) | 1 (0.3) |
| Lockdown Periods *—Step Change IRR (95% CI) | ||||
|---|---|---|---|---|
| During 1st | Post-1st | During 2nd | Post-2nd | |
| Overall | 0.54 (0.44, 0.67) | 0.79 (0.63, 0.99) | 0.55 (0.37, 0.81) | 0.75 (0.53, 1.05) |
| Sex | ||||
| Female | 0.45 (0.34, 0.59) | 0.79 (0.60, 1.04) | 0.51 (0.31, 0.84) | 0.79 (0.52, 1.21) |
| Male | 0.61 (0.43, 0.86) | 0.88 (0.61, 1.27) | 0.65 (0.34, 1.21) | 0.78 (0.44, 1.37) |
| Age group in years | ||||
| <25 | 0.44 (0.32, 0.60) | 0.74 (0.54, 1.00) | 0.54 (0.32, 0.93) | 0.71 (0.44, 1.13) |
| 25+ | 0.62 (0.46, 0.83) | 0.93 (0.68, 1.27) | 0.63 (0.36, 1.08) | 0.90 (0.55, 1.45) |
| Methods | ||||
| Medicinal | 0.45 (0.32, 0.62) | 0.85 (0.63, 1.16) | 0.66 (0.38, 1.15) | 0.76 (0.47, 1.23) |
| Agrochemical | 0.79 (0.53, 1.18) | 0.81 (0.51, 1.28) | 0.49 (0.22, 1.10) | 0.50 (0.24, 1.03) |
| Plant/other | 0.63 (0.40, 0.99) | 0.60 (0.37, 0.96) | 0.40 (0.15, 1.06) | 0.86 (0.43, 1.72) |
| Pandemic Period n (%) | |||
|---|---|---|---|
| Pre- | During | IRR (95% CI) | |
| Overall | 13,405 | 5574 | 0.9 (0.68, 1.19) |
| Sex | |||
| Female | 2797 (20.9) | 1093 (19.6) | 0.98 (0.84, 1.14) |
| Male | 10,608 (79.1) | 4481 (80.4) | 0.89 (0.69, 1.16) |
| Age group in years | |||
| 8–25 | 2563 (19.1) | 1057 (19) | 0.97 (0.83, 1.13) |
| 26–35 | 2237 (16.7) | 936 (16.8) | 0.77 (0.56, 1.06) |
| 36–55 | 4281 (31.9) | 1689 (30.3) | 0.94 (0.82, 1.07) |
| 55+ | 4324 (32.3) | 1892 (33.9) | 1.05 (0.91, 1.21) |
| Methods | |||
| Hanging | 3421 (25.5) | 1091 (19.6) | 0.96 (0.75, 1.23) |
| Poisoning | 7636 (57) | 3619 (64.9) | 0.97 (0.82, 1.15) |
| Other | 2348 (17.5) | 864 (15.5) | 1.01 (0.75, 1.36) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rajapakse, T.; Silva, T.; Hettiarachchi, N.M.; Gunnell, D.; Metcalfe, C.; Spittal, M.J.; Knipe, D. The Impact of the COVID-19 Pandemic and Lockdowns on Self-Poisoning and Suicide in Sri Lanka: An Interrupted Time Series Analysis. Int. J. Environ. Res. Public Health 2023, 20, 1833. https://doi.org/10.3390/ijerph20031833
Rajapakse T, Silva T, Hettiarachchi NM, Gunnell D, Metcalfe C, Spittal MJ, Knipe D. The Impact of the COVID-19 Pandemic and Lockdowns on Self-Poisoning and Suicide in Sri Lanka: An Interrupted Time Series Analysis. International Journal of Environmental Research and Public Health. 2023; 20(3):1833. https://doi.org/10.3390/ijerph20031833
Chicago/Turabian StyleRajapakse, Thilini, Tharuka Silva, Nirosha Madhuwanthi Hettiarachchi, David Gunnell, Chris Metcalfe, Matthew J. Spittal, and Duleeka Knipe. 2023. "The Impact of the COVID-19 Pandemic and Lockdowns on Self-Poisoning and Suicide in Sri Lanka: An Interrupted Time Series Analysis" International Journal of Environmental Research and Public Health 20, no. 3: 1833. https://doi.org/10.3390/ijerph20031833
APA StyleRajapakse, T., Silva, T., Hettiarachchi, N. M., Gunnell, D., Metcalfe, C., Spittal, M. J., & Knipe, D. (2023). The Impact of the COVID-19 Pandemic and Lockdowns on Self-Poisoning and Suicide in Sri Lanka: An Interrupted Time Series Analysis. International Journal of Environmental Research and Public Health, 20(3), 1833. https://doi.org/10.3390/ijerph20031833






