Towards an Understanding of Successes of the Psychiatric Nurses in Caring for Children with Mental Health Problems: An Appreciative Inquiry
Abstract
1. Introduction
2. Materials and Methods
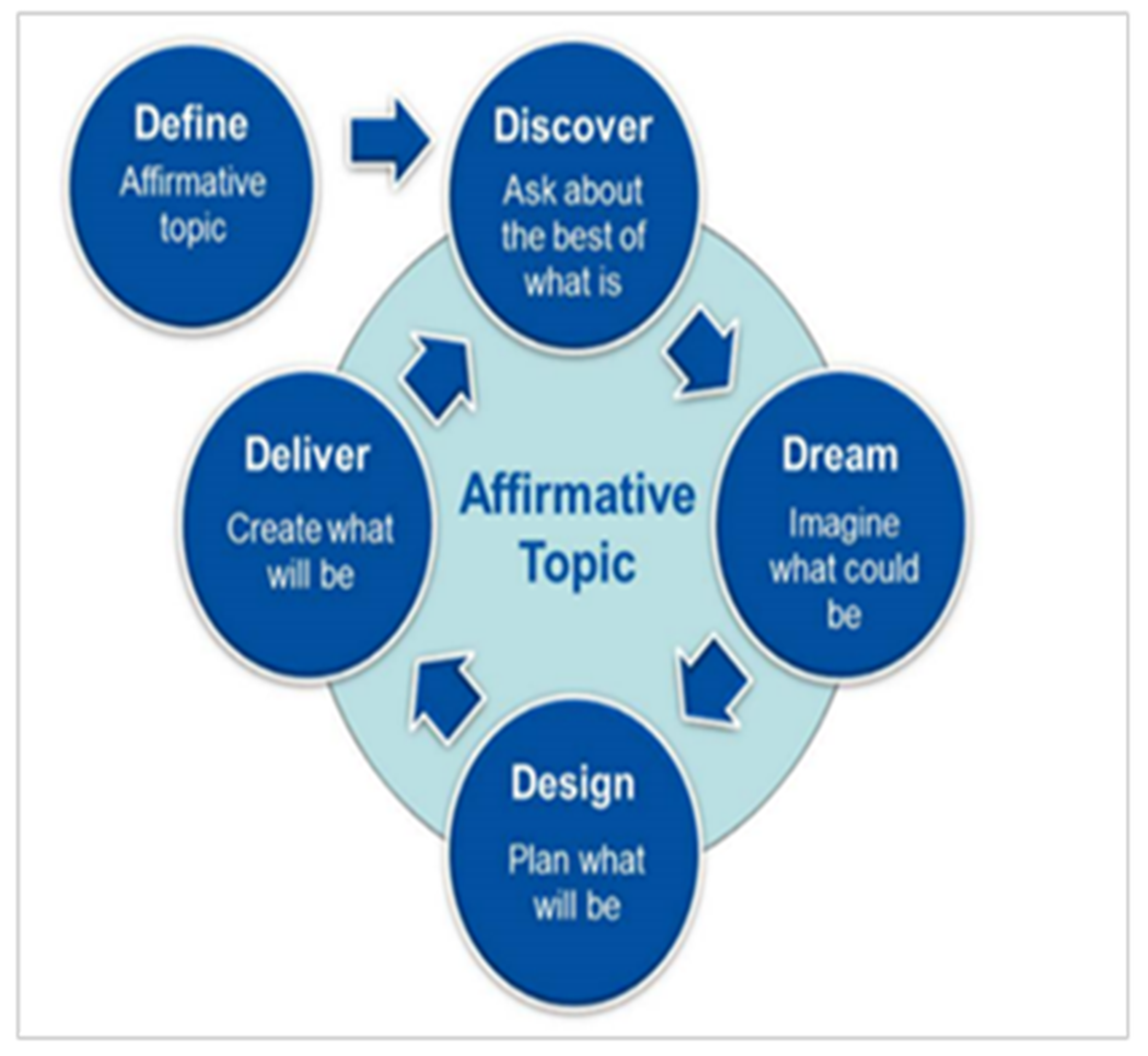
2.1. Study Design
2.2. Appreciative Inquiry (AI) Assumptions
2.3. Setting
2.4. Data Collection
2.5. Data Analysis
2.6. Ethical Approval
3. Results
3.1. Definition Phase
3.2. Discovery Phase
3.2.1. Staff Willingness, Enthusiasm, and Commitment
FG 3 Participant 1 ‘What is working is let’s say people are committed to come to work. You come and you are committed to do your best.’
FG 1 Participant 1 ‘Where we are working, our staff are committed despite them not having the speciality of mental health in children. But they are committed at any point or whatever. At the end of the day, we are managing these children.’
3.2.2. Functional Multidisciplinary Team (MDT)
FG 5 Participant 2 ‘We have a full Multidisciplinary Team.’
FG 3 Participant 1 ‘For me what works is multidisciplinary team collaboration. So, on Wednesdays we have what we call child clinic. So, if we have a difficult or complicated case, we get to call the family and the child as well. And then our specialist, the psychiatrist actually does the interview while the child is there. She does the assessment. So, I feel like that is working.’
3.2.3. Involvement of Family Members in the Management and Treatment Plan
FG 3 Participant 3 ‘I think maybe to educate the parents of the patients.’
FG 2 Participant 3 ‘Active involvement of family members is crucial in the care, treatment and rehabilitation of children who have been diagnosed with mental illness.’
3.3. Dream Phase
3.3.1. Acceptable Times: Children’s Clinic for Mental Health
FG 5 Participant 1 ‘The clinic to run Monday to Friday without limitations till 4 p.m.’
3.3.2. Improvement of Outreach Programs
FG 1 Participant 8 ‘Even if you can understand how to work with children, children come from different homes and from different families, where they don’t really understand when the child is having a problem. So may be strengthening mental health services at the community also needs to be attended to.’
FG 2 Participant 2 ‘With the community there is always a need for education, which I think NW has... should I say zero because a lot of people actually do not know. If it was not for pre-school teachers and primary school teachers, then a lot of parents would be with these children and not aware that their child is sick. They would just see the child as naughty, as different from the others, but they don’t acknowledge it as a mental problem that needs to be attended to. Hence most of the time if the child does not attend preschool, she gets to be seen in primary school. So, I think what need to be done the whole province is education. Whether that is via media, via pamphlets, whether is …you know, more focus should be taken back to mental illness not only the normal mental illness—the adult mental illness, but we are now looking at kids. Because a lot of families need it, if any one of us can get a slot on YOU FM and talk about ADHD. I am sure the following week we will be full in the clinic.’
3.4. Design Phase
FG 5 Participant 4 ‘Come with money and build the hospital with staff.’
FG 2 Participant 1 ‘Build us a hospital. Well equipped. May be a twenty (20) bed hospital dedicated just for kids. Because that really is what they need. Like a playroom even though it is a positive thing that we do have a child clinic, the set up sometimes is disadvantageous to the kids because there is no one way mirror.’
3.4.1. Training and Development of Multi-Disciplinary Team Members in Child Psychiatry
FG 1 Participant 3 ‘There must be a psychiatrist, a psychologist that will be able to assist with the child. A multidisciplinary team. We need a psychiatrist who is trained with children or a psychologist who is trained specifically with children because all other professions have got that.’
FG1 Participant 6 ‘I would like to specialize: Training and development on mental needs especially with children. We must have more training for nurses on child mental health.’
FG 2 Participant 3 ‘Even other things like integrating mental health into the school health program or services. Also having more training for nurses on child mental health and adult psyche. And the support and understanding of management. Because sometimes even if they can be trained you find that the managers don’t have skills and understanding. It will be just a fruitless exercise. They must have an understanding on mental health and child psychiatry.’
3.4.2. Investment in Infrastructure
FG 2 Participant 2 ‘And a child friendly clinic as well. Because some children still make it as an outpatient client. But they would need…Even our psychologist I think they are doing their best right now but, they could actually do better if they could have play therapy equipment, a playroom, you know like a garden outside to play and see how they respond.’
FG 1 Participant 4 ‘If they can build psychiatric hospitals in rural areas.’
3.5. Destiny Phase
Availability and Upgrading of Infrastructure
FG 1 Participant 4 ‘If they can make a ward and a child mental health specialized one, the one which specializes with kids. And for MDT to take place as well.’
FG 2 Participant 1 ‘If it was a fantasy world, where we could have a 20-bedded, dedicated child unit, then obviously it would be best to separate them so that you go in depth.’
FG 1 Participant 6 ‘Even if [it means] we can have a child psychiatric clinic in each village where it becomes easier to communicate.’
FG 2 Participant 3 ‘Even if they build this small hospitals or psychiatric clinic. It will help.’
4. Discussion
4.1. Basic Belief and Values
4.2. Changing Operational Practices
4.3. Strategy and Tasks
4.4. Leadership and Decision-Making Processes
4.5. Implications for Practice
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gustin, L.W. Being mutually involved in recovery. A hermeneutic exploration of nurses’ experiences of patient participation in psychiatric care. Int. J. Qual. Stud. Health Well-Being 2021, 16, 1–13. [Google Scholar]
- Phoenix, B.J. The Current Psychiatric Mental Health Registered Nurse Workforce. J. Am. Psychiatr. Nurses Assoc. 2019, 25, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Bruce, J.C. Nursing in the 21st Century—Challenging its values and roles. Prof. Nurs. Today 2018, 22, 44–48. [Google Scholar]
- Onyibo, E. Understanding the True Meaning of Success. The Guardian Newspaper, 18 March 2016; 1. [Google Scholar]
- Bushel, H.; Stuart, L.; Keppich-Arnold, S.; Anderson, S.; Batu, G.; Hopkins, L. How Do Mental Health Nurses Define Success? A Comparative Study of Bed-Based and Community-Based Services. Issues Ment. Health Nurs. 2021, 42, 836–844. [Google Scholar] [CrossRef] [PubMed]
- Joubert, P.; Bhagwan, R. An empirical study of the challenging roles of psychiatric nurses at in-patient psychiatric facilities and its implications for nursing education. Int. J. Afr. Nurs. Sci. 2018, 9, 49–56. [Google Scholar] [CrossRef]
- World Health Organization. Standards for Improving the Quality of Care for Children and Young Adolescents in Health Facilities; World Health Organization: Geneva, Switzerland, 2020.
- Zheng, Y. Child psychiatry in China: Present situation and future prospects. Pediatr. Investig. 2020, 4, 79–83. [Google Scholar] [CrossRef]
- Frissora, K.M.; Ranz, J.A. Community Psychiatry Nurse Practitioner Fellowship: Preparing Nurse Practitioners for Mental Health Workforce Expansion. Psychiatr. Serv. 2021, 72, 91–93. [Google Scholar] [CrossRef]
- Peterlin, J.; Praničević, D. Perceived trends in viewing the future by Croatian and Slovenian business students: Implications for managerial education. Manag.-J. Contemp. Manag. Issues 2019, 24, 103–120. [Google Scholar] [CrossRef]
- Hung, L.; Lee, P.A.; Au-Yeung, A.T.; Kucherova, I.; Harrigan, M. Adopting a clinical assessment framework in older adult mental health. J. Psychosoc. Nurs. Ment. Health Serv. 2016, 54, 26–41. [Google Scholar] [CrossRef]
- Boy, N.M.; Bright, D.S. Appreciative Inquiry as mode of Action Research for community psychology. J. Community Psychol. 2007, 35, 1019–1036. [Google Scholar]
- Iriarte, C.; Bayona, S. IT projects success factors: A literature review. Int. J. Inf. Syst. Proj. Manag. 2020, 8, 49–78. [Google Scholar] [CrossRef]
- Chauke, M.E.; Van Der Wal, D.; Botha, A. Using appreciative inquiry to transform student nurses’ image of nursing. Curationis 2015, 38, 1–8. [Google Scholar] [CrossRef]
- Hung, L.; Phinney, A.; Habib, C.; Rodney, P.; Tabamo, J.; Bohl, D. Appreciative Inquiry: Bridging Research and Practice in a Hospital Setting. Int. J. Qual. Methods 2018, 17, 1–10. [Google Scholar] [CrossRef]
- Curtis, K.; Gallagher, A.; Ramage, C.; Montgomery, J.; Martin, C.; Leng, J.; Holah, J. Using appreciative inquiry to develop, implement and evaluate a multiorganization “Cultivating Compassion” programme for health professionals and support staff. J. Res. Nurs. 2017, 22, 150–165. [Google Scholar] [CrossRef]
- Scerri, A.; Innes, A.; Scerri, C. Using appreciative inquiry to implement person-centred dementia care in hospital wards. Dementia 2019, 18, 190–209. [Google Scholar] [CrossRef]
- Watkins, S.; Dewar, B.; Kennedy, C. Appreciative Inquiry as an intervention to change nursing practice in in-patient settings: An integrative review. Int. J. Nurs. Stud. 2016, 60, 179–190. [Google Scholar] [CrossRef]
- Merriel, A.; Wilson, A.; Decker, E.; Hussein, J.; Larkin, M.; Barnard, K.; O’Dair, M.; Costello, A.; Malata, A.; Coomarasamy, A. Systematic review and narrative synthesis of the impact of Appreciative Inquiry in healthcare. BMJ Open Qual. 2022, 11, 1–11. [Google Scholar] [CrossRef]
- Ogude, N.A.; Meyer, I.J.; Mwambakana, J.; Mthethwa, N.E. Can extended curriculum programmes be improved through engagement with students using appreciative inquiry? S. Afr. J. High. Educ. 2019, 33, 219–236. [Google Scholar] [CrossRef]
- Arieli, S.; Sagiv, L.; Roccas, S. Values at Work: The Impact of Personal Values in Organisations. Appl. Psychol. 2020, 69, 230–275. [Google Scholar] [CrossRef]
- Sibandze, B.; Scafide, K. Among nurses, how does education level impact professional values? A systematic review. Int. Nurs. Rev. 2018, 65, 65–77. [Google Scholar] [CrossRef]
- Van Der Ende, P.; Korevaar, E.; Nicholson; Van Busschbach, J.; Van Weeghel, J. Strategies for parenting by mothers and fathers with mental illness. J. Psychiatr. Ment. Health Nurs. 2016, 23, 86–97. [Google Scholar] [CrossRef] [PubMed]
- Kruk, M.E.; Lewis, T.; Arsenault, C.; Bhutta, Z.A.; Irimu, G.; Jeong, J.; Lassi, Z.S.; Sawyer, S.M.; Vaivada, T.; Waiswa, P.; et al. Improving health and social systems for all children in LMICs: Structural innovations to deliver high quality services. Lancet 2022, 399, 1830–1844. [Google Scholar] [CrossRef] [PubMed]
- Stadnick, N.; Martinez, K.; Aarons, G.; Lee, D.; Van Cleave, J.; Brookman-Frazee, L. Paediatric primary care perspectives on integrated mental health care for autism. Acad. Pediatr. 2020, 20, 1140–1147. [Google Scholar] [CrossRef] [PubMed]
- Bonham, E.; Kwasky, A. Caring for the Mental Health of Youth and Families. Clin. Nurse Spec. 2021, 35, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Kearney, B.; Hoskinsd, K.; Iyengarc, A. The role of psychiatric mental health nurse practitioners in improving mental and behavioural health care delivery for children and adolescents in multiple settings. Arch. Psychiatr. Nurs. 2020, 34, 275–280. [Google Scholar] [CrossRef]
- Blanchard, K. The power of Empowerment. Manag. Today 2007, 33, 14–19. [Google Scholar]
- Wu, B.; Yun, Z.; Xu, D.; Wang, Y.; Niu, N.; Zhang, M.; Zhi, X.; Zhu, P.; Meng, A. Factors associated with nurses’ willingness to participate in care of patients with COVID-19: A survey in China. J. Nurs. Manag. 2020, 28, 1704–1712. [Google Scholar] [CrossRef]
- Unroe, K.T.; Evan, S.R.; Weaver, L.; Rusyniak, D.; Blackburn, J. Willingness of Long-Term Care Staff to Receive a COVID-19Vaccine: Single State Survey. J. Am. Geriatr. Soc. 2021, 69, 593–599. [Google Scholar] [CrossRef]
- Van Rensburg, J. Following on from the Life Esidimeni incident—Access to care for people living with severe mental disability, according to national policy. S Afr. J. Bioeth. Law 2017, 10, 48–50. [Google Scholar] [CrossRef]
- Kapologwe, N.A.; Meara, J.G.; Kengia, J.T.; Sonda, Y.; Gwajima, D.; Alidina, S.; Kalolo, A. Development and upgrading of public primary healthcare facilities with essential surgical services infrastructure: A strategy towards achieving universal health coverage in Tanzania. BMC Health Serv. Res. Open Access 2020, 20, 218. [Google Scholar] [CrossRef]
- Butala, N.M.; Van Rooyen, M.J.; Patel, R.B. Improved health outcomes in urban slums through infrastructure upgrading. Soc. Sci. Med. 2010, 71, 935–940. [Google Scholar] [CrossRef]
- Odeyemi, C.; Morrissey, J.; Donohue, G. Factors affecting mental health nurses working with clients with first- episode psychosis: A qualitative study. J. Psychiatr. Ment. Health Nurs. 2018, 25, 423–431. [Google Scholar] [CrossRef]
- Menta Health Care Act, Act 17 of 2002, 449; Government Gazzette Republic of South Africa: Pretoria, South Africa, 2002.
- Seeley, J. What is Planning? Definition and Strategy. J. Am. Inst. Plan. 2008, 28, 91–97. [Google Scholar] [CrossRef]
- Troxel, J.P. Appreciative Inquiry. An Action Research Method for Organizational Transformation and Its Implications for the Practice of Group Process Facilitation; Millennia Consulting: Chicago, IL, USA, 2002; pp. 1–18. [Google Scholar]
- Alexandrova, E.; Shapekova, N.L.; Bilal, A.K.; Özcanaslan, F.; Turan, N. Health Sciences Research in the Globalizing World; St. Kliment Ohridski University Press: Sofia, Bulgaria, 2018. [Google Scholar]
- Rasheed, S.P.; Younas, A.; Sundus, A. Self-awareness in nursing: A scoping review. J. Clin. Nurs. 2018, 28, 762–774. [Google Scholar] [CrossRef]
- Sinclair, S.; Kondejewski, J.; Raffin-Bouchal, S.; King-Shier, K.M.; Singh, P. Can Self-Compassion Promote Healthcare Provider Well-Being and Compassionate Care to Others? Results of a Systematic Review. Appl. Psychol. Health Well-Being 2017, 9, 168–206. [Google Scholar] [CrossRef]
- Yoo, Y.J.; Kim, J.H.; Kim, J.S.; Kim, H.L.; Ki, J.S. Clinical nurses’ beliefs, knowledge, organizational readiness and level of implementation of evidence-based practice: The first step to creating an evidence-based practice culture. PLoS ONE 2019, 14, e0226742. [Google Scholar] [CrossRef]
- Carroll, N.; Conboy, K. Normalising the “new normal”: Changing tech-driven work practices under pandemic time pressure. Int. J. Inf. Manag. 2020, 55, 102186. [Google Scholar] [CrossRef]
- Farrell, M. Leadership Reflections. J. Libr. Adm. 2017, 57, 674–682. [Google Scholar] [CrossRef]
- Oates, J.; Burrell, C.; Ebrahim, S.; Taylor, J.; Veitch, P.; Brandon, T. Responsibility as professional leadership and decision making: Interviews with non-medical Responsible Clinicians. Int. J. Law Psychiatry 2020, 71, 101575. [Google Scholar] [CrossRef]
- O’Reilly, M.; Svirydzenka, N.; Adams, S.; Dogra, N. Review of mental health promotion interventions in schools. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 647–662. [Google Scholar] [CrossRef]
- World Health Organization. The WHO Special Initiative for Mental Health (2019–2023): Universal Health Coverage for Mental Health; World Health Organization: Geneva, Switzerland, 2018.
| Research Question | Themes | |
|---|---|---|
| Definition phase | None | Not applicable |
| Discovery phase | What works for you in caring for children with mental health problems? | Staff willingness, enthusiasm and commitment Functional multi-disciplinary team (MDT) Involvement of family members in the management and treatment plan |
| Dream phase | Where do you want to see the care of children with mental health problem in NW province? | Acceptable times for children’s clinic for mental health Improved outreach programs |
| Design phase | What can be done to maximize the potential in the care of children with mental health problems? | Training and development of MDT members in child psychiatry Attention to infrastructural issues and staff shortage |
| Destiny phase | How can we help in caring for children with mental health problems? | Upgrading of infrastructure |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Machailo, R.M.; Koen, D.; Matsipane, M. Towards an Understanding of Successes of the Psychiatric Nurses in Caring for Children with Mental Health Problems: An Appreciative Inquiry. Int. J. Environ. Res. Public Health 2023, 20, 1725. https://doi.org/10.3390/ijerph20031725
Machailo RM, Koen D, Matsipane M. Towards an Understanding of Successes of the Psychiatric Nurses in Caring for Children with Mental Health Problems: An Appreciative Inquiry. International Journal of Environmental Research and Public Health. 2023; 20(3):1725. https://doi.org/10.3390/ijerph20031725
Chicago/Turabian StyleMachailo, Rorisang Mary, Daleen Koen, and Molekodi Matsipane. 2023. "Towards an Understanding of Successes of the Psychiatric Nurses in Caring for Children with Mental Health Problems: An Appreciative Inquiry" International Journal of Environmental Research and Public Health 20, no. 3: 1725. https://doi.org/10.3390/ijerph20031725
APA StyleMachailo, R. M., Koen, D., & Matsipane, M. (2023). Towards an Understanding of Successes of the Psychiatric Nurses in Caring for Children with Mental Health Problems: An Appreciative Inquiry. International Journal of Environmental Research and Public Health, 20(3), 1725. https://doi.org/10.3390/ijerph20031725







