Risk Factors for Alcohol Consumption after Starting Assisted Reproductive Technology Treatment among Japanese Women: Japan-Female Employment and Mental Health in Assisted Reproductive Technology (J-FEMA) Study
Abstract
1. Introduction
2. Materials and Methods
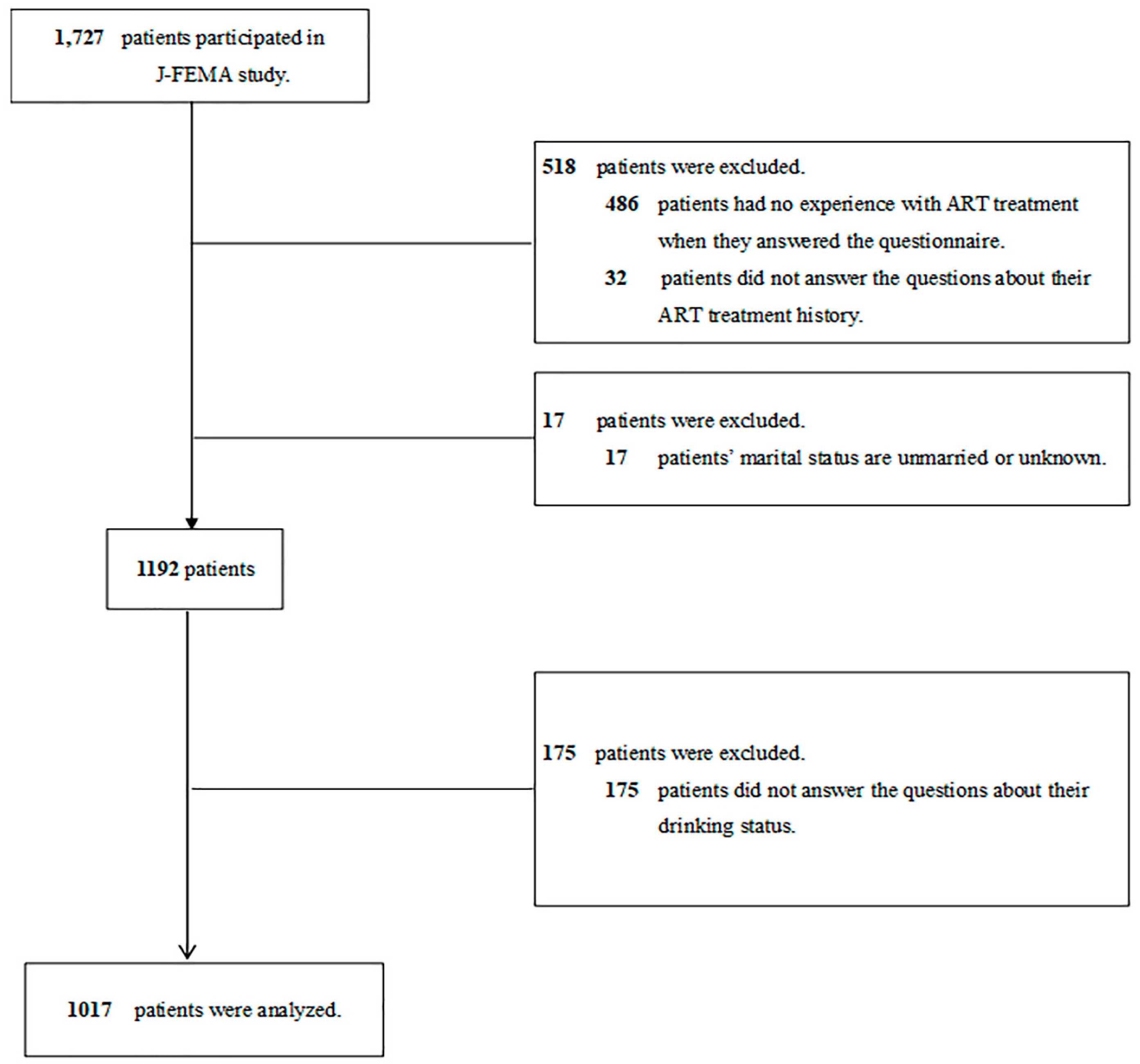
2.1. Patients
2.2. Questionnaire and Variables
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The World Bank. Fertility Rate, Total (Births per Woman). 2019. Available online: http://data.worldbank.org/indicator/SP.DYN.TFRT.IN (accessed on 4 December 2023).
- The Ministry of Health Labor and Welfare in Japan. Overview of Vital Statistics in 2019. 2020. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/kakutei19/dl/15_all.pdf (accessed on 4 December 2023).
- Broekmans, F.J.; Soules, M.R.; Fauser, B.C. Ovarian aging: Mechanisms and clinical consequences. Endocr. Rev. 2009, 30, 465–493. [Google Scholar] [CrossRef] [PubMed]
- Te Velde, E.R.; Pearson, P.L. The variability of female reproductive ageing. Hum. Reprod. Update 2002, 8, 141–154. [Google Scholar] [CrossRef]
- Irahara, M.; Kuwahara, A.; Iwasa, T.; Ishikawa, T.; Ishihara, O.; Kugu, K.; Sawa, R.; Banno, K.; Saito, H. Assisted reproductive technology in Japan: A summary report of 1992–2014 by the Ethics Committee, Japan Society of Obstetrics and Gynecology. Reprod. Med. Biol. 2017, 16, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Katagiri, Y.; Jwa, S.C.; Kuwahara, A.; Iwasa, T.; Ono, M.; Kato, K.; Kishi, H.; Kuwabara, Y.; Harada, M.; Hamatani, T.; et al. Assisted reproductive technology in Japan: A summary report for 2020 by the ethics Committee of the Japan Society of obstetrics and gynecology. Reprod. Med. Biol. 2023, 22, e12494. [Google Scholar] [CrossRef] [PubMed]
- National Collaborating Centre for Women’s and Children’s Health (UK). Fertility: Assessment and Treatment for People with Fertility Problems; Royal College of Obstetricians & Gynaecologists: London, UK, 2013. [Google Scholar]
- Anderson, K.; Nisenblat, V.; Norman, R. Lifestyle factors in people seeking infertility treatment—A review. Aust. N. Z. J. Obstet. Gynaecol. 2010, 50, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Mattson, S.N.; Bernes, G.A.; Doyle, L.R. Fetal Alcohol Spectrum Disorders: A Review of the Neurobehavioral Deficits Associated with Prenatal Alcohol Exposure. Alcohol. Clin. Exp. Res. 2019, 43, 1046–1062. [Google Scholar] [CrossRef] [PubMed]
- Van Heertum, K.; Rossi, B. Alcohol and fertility: How much is too much? Fertil. Res. Pract. 2017, 3, 10. [Google Scholar] [CrossRef]
- Rossi, B.V.; Berry, K.F.; Hornstein, M.D.; Cramer, D.W.; Ehrlich, S.; Missmer, S.A. Effect of alcohol consumption on in vitro fertilization. Obstet. Gynecol. 2011, 117, 136–142. [Google Scholar] [CrossRef]
- Klonoff-Cohen, H.; Lam-Kruglick, P.; Gonzalez, C. Effects of maternal and paternal alcohol consumption on the success rates of in vitro fertilization and gamete intrafallopian transfer. Fertil. Steril. 2003, 79, 330–339. [Google Scholar] [CrossRef]
- Gormack, A.A.; Peek, J.C.; Derraik, J.G.; Gluckman, P.D.; Young, N.L.; Cutfield, W.S. Many women undergoing fertility treatment make poor lifestyle choices that may affect treatment outcome. Hum. Reprod. 2015, 30, 1617–1624. [Google Scholar] [CrossRef][Green Version]
- Wdowiak, A.; Sulima, M.; Sadowska, M.; Grzegorz, B.; Bojar, I. Alcohol consumption and quality of embryos obtained in programmes of in vitro fertilization. Ann. Agric. Environ. Med. 2014, 21, 450–453. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Braga, D.P.; Halpern, G.; Setti, A.S.; Figueira, R.C.; Iaconelli, A., Jr.; Borges, E., Jr. The impact of food intake and social habits on embryo quality and the likelihood of blastocyst formation. Reprod. Biomed. Online 2015, 31, 30–38. [Google Scholar] [CrossRef] [PubMed]
- International Alliance for Responsible Drinking (IARD). Drinking Guidelines for Pregnancy and Breastfeeding. 2019. Available online: https://iard.org/science-resources/detail/Drinking-Guidelines-for-Pregnancy-and-Breastfeedin (accessed on 4 December 2023).
- World Health Organization. Global Status Report on Alcohol and Health 2014; World Health Organization: Geneva, Switzerland, 2014; Available online: https://www.who.int/publications/i/item/global-status-report-on-alcohol-and-health-2014 (accessed on 4 December 2023).
- World Health Organization. Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2018; Available online: https://apps.who.int/iris/handle/10665/274603 (accessed on 4 December 2023).
- The Ministry of Health Labor and Welfare in Japan. National Health and Nutrition Survey 1994. 1995. Available online: https://www.mhlw.go.jp/toukei/kouhyo/indexkk_14_1.html (accessed on 4 December 2023).
- The Ministry of Health Labor and Welfare in Japan. National Health and Nutrition Survey 2019. 2020. Available online: https://www.e-stat.go.jp/dbview?sid=0003223919 (accessed on 4 December 2023).
- Imai, Y.; Endo, M.; Kuroda, K.; Tomooka, K.; Ikemoto, Y.; Sato, S.; Mitsui, K.; Ueda, Y.; Deshpande, G.A.; Tanaka, A.; et al. Risk factors for resignation from work after starting infertility treatment among Japanese women: Japan-Female Employment and Mental health in Assisted reproductive technology (J-FEMA) study. Occup. Environ. Med. 2020, 78, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.J.; Sung, H.Y.; Max, W.; Shi, Y.; Ong, M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int. J. Methods Psychiatr. Res. 2012, 21, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Munezawa, T.; Morin, C.M.; Inoue, Y.; Nedate, K. Development of the Japanese version of the Insomnia Severity Index (ISI-J). Jpn. J. Psychiatr. Treat. 2009, 24, 219–225. (In Japanese) [Google Scholar]
- The Ministry of Health Labor and Welfare in Japan. National Health and Nutrition Survey 2018. 2019. Available online: https://www.mhlw.go.jp/content/000615345.pdf (accessed on 4 December 2023).
- Agarwal, D.P.; Harada, S.; Goedde, H.W. Racial differences in biological sensitivity to ethanol: The role of alcohol dehydrogenase and aldehyde dehydrogenase isozymes. Alcohol. Clin. Exp. Res. 1981, 5, 12–16. [Google Scholar] [CrossRef]
- Yin, S.J. Alcohol dehydrogenase: Enzymology and metabolism. Alcohol Alcohol. Suppl. 1994, 2, 113–119. [Google Scholar] [PubMed]
- Ishitsuka, K.; Hanada-Yamamoto, K.; Mezawa, H.; Saito-Abe, M.; Konishi, M.; Ohya, Y.; Japan Environment and Children’s Study Group. Determinants of Alcohol Consumption in Women Before and After Awareness of Conception. Matern. Child. Health J. 2020, 24, 165–176. [Google Scholar] [CrossRef]
- Gosdin, L.K.; Deputy, N.P.; Kim, S.Y.; Dang, E.P.; Denny, C.H. Alcohol Consumption and Binge Drinking During Pregnancy Among Adults Aged 18–49 Years—United States, 2018–2020. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 10–13, Correction in MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 156. [Google Scholar] [CrossRef]
- The Ministry of Health Labor and Welfare in Japan. National Health and Nutrition Survey 2019. 2020. Available online: https://www.mhlw.go.jp/content/10900000/000687163.pdf (accessed on 4 December 2023).
- Leonard, K.E.; Eiden, R.D. Marital and family processes in the context of alcohol use and alcohol disorders. Annu. Rev. Clin. Psychol. 2007, 3, 285–310. [Google Scholar] [CrossRef]
- Yamamoto, Y.; Kaneita, Y.; Yokoyama, E.; Sone, T.; Takemura, S.; Suzuki, K.; Kaneko, A.; Ohida, T. Alcohol consumption and abstention among pregnant Japanese women. J. Epidemiol. 2008, 18, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, A.; Kawachi, I.; Iso, H.; Inoue, M.; Tsugane, S.; JPHC Study Group. Gender difference in the association between social support and metabolic syndrome in Japan: The ‘enkai’ effect? J. Epidemiol. Community Health 2011, 65, 71–77. [Google Scholar] [CrossRef]
- Kinjo, A.; Kuwabara, Y.; Minobe, R.; Maezato, H.; Kimura, M.; Higuchi, S.; Matsumoto, H.; Yuzuriha, T.; Horie, Y.; Kanda, H.; et al. Different socioeconomic backgrounds between hazardous drinking and heavy episodic drinking: Prevalence by sociodemographic factors in a Japanese general sample. Drug Alcohol Depend. 2018, 193, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Keyes, K.M.; Li, G.; Hasin, D.S. Birth cohort effects and gender differences in alcohol epidemiology: A review and synthesis. Alcohol. Clin. Exp. Res. 2011, 35, 2101–2112. [Google Scholar] [CrossRef] [PubMed]
- van der Wulp, N.Y.; Hoving, C.; de Vries, H. Partner’s influences and other correlates of prenatal alcohol use. Matern. Child Health J. 2015, 19, 908–916. [Google Scholar] [CrossRef]
- Leonard, K.E.; Das Eiden, R. Husband’s and wife’s drinking: Unilateral or bilateral influences among newlyweds in a general population sample. J. Stud. Alcohol Suppl. 1999, 13, 130–138. [Google Scholar] [CrossRef]
- Castillo-Carniglia, A.; Keyes, K.M.; Hasin, D.S.; Cerdá, M. Psychiatric comorbidities in alcohol use disorder. Lancet Psychiatry 2019, 6, 1068–1080. [Google Scholar] [CrossRef]
- Osaki, Y.; Kinjo, A.; Higuchi, S.; Matsumoto, H.; Yuzuriha, T.; Horie, Y.; Kimura, M.; Kanda, H.; Yoshimoto, H. Prevalence and Trends in Alcohol Dependence and Alcohol Use Disorders in Japanese Adults; Results from Periodical Nationwide Surveys. Alcohol Alcohol. 2016, 51, 465–473. [Google Scholar] [CrossRef]
- de Angelis, C.; Nardone, A.; Garifalos, F.; Pivonello, C.; Sansone, A.; Conforti, A.; Di Dato, C.; Sirico, F.; Alviggi, C.; Isidori, A.; et al. Smoke, alcohol and drug addiction and female fertility. Reprod. Biol. Endocrinol. 2020, 18, 21. [Google Scholar] [CrossRef]
| Variables Categories | Number (%) | Habitual Drinking Rate (%) | p Value ** | |||||
|---|---|---|---|---|---|---|---|---|
| Total | Not Habitual Drinking | Habitual Drinking | ||||||
| N | 1017 | 859 | (84.5) | 158 | (15.5) | 15.5 | ||
| Age (years) | ||||||||
| <35 | 197 | (19.6) | 179 | (21.1) | 18 | (11.6) | 9.1 | 0.01 |
| ≥35 | 806 | (80.4) | 669 | (78.9) | 137 | (88.3) | 17.0 | |
| Educational background * | ||||||||
| Higher | 528 | (52.2) | 434 | (50.8) | 94 | (59.9) | 17.8 | <0.01 |
| Lower | 483 | (47.8) | 420 | (49.2) | 63 | (40.1) | 13.0 | |
| Partner’s drinking status | ||||||||
| Not drinking | 291 | (28.8) | 280 | (32.8) | 11 | (7.0) | 3.8 | <0.01 |
| Drinking | 720 | (71.2) | 573 | (67.2) | 147 | (93.0) | 20.4 | |
| Duration of infertility (year) | ||||||||
| <2 | 250 | (25.2) | 213 | (25.4) | 37 | (23.6) | 14.8 | 0.62 |
| ≥2 | 744 | (74.8) | 624 | (74.6) | 120 | (76.4) | 16.1 | |
| IVF cycle | ||||||||
| <6 | 644 | (76.2) | 545 | (75.8) | 99 | (78.6) | 15.4 | 0.50 |
| ≥6 | 201 | (23.8) | 174 | (24.2) | 27 | (21.4) | 13.4 | |
| History of childbirth | ||||||||
| Yes | 202 | (38.4) | 179 | (41.1) | 23 | (25.6) | 11.4 | 0.01 |
| No | 324 | (61.6) | 257 | (58.9) | 67 | (74.4) | 20.7 | |
| K6 | ||||||||
| <13 | 940 | (93.8) | 791 | (93.4) | 149 | (96.1) | 15.9 | 0.19 |
| ≥13 | 62 | (6.2) | 56 | (6.6) | 6 | (3.9) | 9.7 | |
| ISI-J | ||||||||
| <10 | 791 | (78.7) | 664 | (78.4) | 127 | (80.4) | 16.1 | 0.58 |
| ≥10 | 214 | (21.3) | 183 | (21.6) | 31 | (19.6) | 14.5 | |
| Employment type | ||||||||
| Non-worker | 273 | (27.1) | 249 | (29.3) | 24 | (15.3) | 8.8 | <0.01 |
| Worker | 735 | (72.9) | 602 | (70.7) | 133 | (84.7) | 18.1 | |
| Company size (employees) | ||||||||
| <50 | 232 | (32.3) | 193 | (32.8) | 39 | (29.8) | 16.8 | 0.20 |
| 50–999 | 249 | (34.6) | 209 | (35.5) | 40 | (30.5) | 16.1 | |
| ≥1000 | 238 | (33.1) | 186 | (31.6) | 52 | (39.7) | 21.8 | |
| Variables Categories | Crude OR (95% CI) | p Value *** | Multivariate OR ** (95% CI) | p Value *** |
|---|---|---|---|---|
| Age (years) | ||||
| <35 | 1.00 | 1.00 | ||
| ≥35 | 2.04 (1.21–3.42) | 0.01 | 2.27 (0.99–5.21) | 0.053 |
| Educational background * | ||||
| Higher | 1.00 | 1.00 | ||
| Lower | 0.69 (0.49–0.98) | 0.04 | 0.78 (0.48–1.28) | 0.33 |
| Partner’s drinking status | ||||
| Not drinking | 1.00 | 1.00 | ||
| Drinking | 6.53 (3.48–12.25) | <0.01 | 4.26 (1.98–9.16) | <0.01 |
| History of childbirth | ||||
| Yes | 1.00 | 1.00 | ||
| No | 2.03 (1.22–3.38) | 0.01 | 1.84 (1.08–3.12) | 0.02 |
| Employment type | ||||
| Non-worker | 1.00 | 1.00 | ||
| Worker | 2.29 (1.45–3.63) | <0.01 | 1.77 (1.00–3.14) | 0.050 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sato, M.; Endo, M.; Tomooka, K.; Kuroda, K.; Ueda, Y.; Sato, S.; Ikemoto, Y.; Imai, Y.; Mitsui, K.; Tanaka, A.; et al. Risk Factors for Alcohol Consumption after Starting Assisted Reproductive Technology Treatment among Japanese Women: Japan-Female Employment and Mental Health in Assisted Reproductive Technology (J-FEMA) Study. Int. J. Environ. Res. Public Health 2023, 20, 7152. https://doi.org/10.3390/ijerph20247152
Sato M, Endo M, Tomooka K, Kuroda K, Ueda Y, Sato S, Ikemoto Y, Imai Y, Mitsui K, Tanaka A, et al. Risk Factors for Alcohol Consumption after Starting Assisted Reproductive Technology Treatment among Japanese Women: Japan-Female Employment and Mental Health in Assisted Reproductive Technology (J-FEMA) Study. International Journal of Environmental Research and Public Health. 2023; 20(24):7152. https://doi.org/10.3390/ijerph20247152
Chicago/Turabian StyleSato, Mamiko, Motoki Endo, Kiyohide Tomooka, Keiji Kuroda, Yuito Ueda, Setsuko Sato, Yuko Ikemoto, Yuya Imai, Kiyomi Mitsui, Atsushi Tanaka, and et al. 2023. "Risk Factors for Alcohol Consumption after Starting Assisted Reproductive Technology Treatment among Japanese Women: Japan-Female Employment and Mental Health in Assisted Reproductive Technology (J-FEMA) Study" International Journal of Environmental Research and Public Health 20, no. 24: 7152. https://doi.org/10.3390/ijerph20247152
APA StyleSato, M., Endo, M., Tomooka, K., Kuroda, K., Ueda, Y., Sato, S., Ikemoto, Y., Imai, Y., Mitsui, K., Tanaka, A., Sugiyama, R., Nakagawa, K., Sato, Y., Kuribayashi, Y., Kitade, M., Itakura, A., Takeda, S., & Tanigawa, T. (2023). Risk Factors for Alcohol Consumption after Starting Assisted Reproductive Technology Treatment among Japanese Women: Japan-Female Employment and Mental Health in Assisted Reproductive Technology (J-FEMA) Study. International Journal of Environmental Research and Public Health, 20(24), 7152. https://doi.org/10.3390/ijerph20247152





